Abstract
Crohn’s disease (CD) is an idiopathic inflammatory bowel disease that can involve any part of the gastrointestinal tract. Esophageal involvement is rarely seen in adults, especially at the initial diagnosis of CD. Esophageal symptoms as primary manifestations of the disease are extremely rare. We report a case of a CD with esophageal involvement at the time of her initial diagnosis of CD.
Introduction
Crohn’s disease (CD) can involve any segment of the gastrointestinal tract frequently involving the colon or small bowel. Esophageal involvement is very rare with most patients being diagnosed with extraesophageal CD 3 years on average before their diagnosis of esophageal CD.1 In a Mayo Clinic study, only 0.2% of Crohn’s patients were identified with esophageal involvement with a mean age of 31 at diagnosis.2
Case Report
A 64-year-old white woman with past medical history of hypertension and osteoarthritis presented to the hospital with a 13.6-kg weight loss and fatigue for several months. She reported postprandial epigastric pain and odynophagia. She had an oral ulcer almost 1 month before this admission. She had no dysphagia or melena. She also noted a change in her stool size and frequency (small and 2-3 times daily). She did not smoke or drink alcohol. She had no history of diverticulitis. Her mother died from complications of CD. On physical examination, she was afebrile and normotensive, with a weight of 51.6 kg and a calculated body mass index of 19 kg/m2. Her oropharynx was normal. Abdomen was soft and nondistended but tender to palpation in the left lower quadrant.
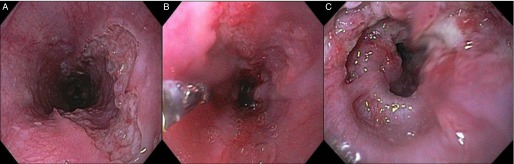
Abdominal and pelvic computed tomography showed severe wall thickening and pericolonic inflammation in the sigmoid colon. Chest computed tomography demonstrated distal esophagus wall thickening concerning for ulcer. An upper endoscopy showed a 10-cm length of ulceration and friable tissue with nodularity in the mid to distal esophagus with a normal appearing stomach and duodenum (Figure 1). Colonoscopy demonstrated deep ulcers with friable tissue in rectum around 2 cm in length extending into anal canal. The sigmoid colon was significantly narrowed preventing the scope from advancing further. Biopsies from the esophagus and colon showed granulation tissue with reactive epithelial changes with evidence of chronicity and no granulomas. There was no evidence of dysplasia or malignancy, and stains were negative for cytomegalovirus and herpes. C-reactive protein was 55 mg/L and erythrocyte sedimentation rate was 27 mm/hr. Considering the sigmoid and rectal ulcers, family history, and histologic findings, esophageal CD was suspected.
Figure 1.
(A-C) Esophageal ulcers before treatment.
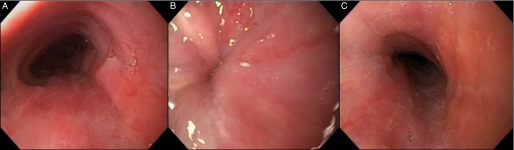
Because of concerns for absorption, she was started on intravenous solumedrol and was transitioned to oral prednisone. She was also started on a proton pump inhibitor. At a 2-week follow-up, her stool was more formed, and the abdominal pain and odynophagia had resolved. A follow-up upper endoscopy 4 weeks later showed resolution of the esophageal ulcers (Figure 2). During follow-up sigmoidoscopy at 4 and 12 weeks the scope could not be advanced beyond the sigmoid colon. She was not initially started on anti-tumor necrosis factor (anti-TNF) therapy due to patient reluctance, and surgery was not initially performed due to her poor nutritional and overall debilitated state. At 16 weeks, she developed a colovaginal fistula. Resection of the 16-cm sigmoid stricture with colostomy was performed, and pathology was negative for malignancy. She had a small bowel follow-through at the time of her surgery, which did not reveal any small intestinal disease. Follow-up endoscopy through her ostomy did not demonstrate any small intestinal involvement. Colonoscopy after her surgery revealed only mild ascending colon colitis. She was started on ant-TNF therapy and did well.
Figure 2.
(A-C) Esophageal ulcers after steroid therapy at 4-week follow-up.
Discussion
Esophageal involvement is one of the rare complications of CD. In a retrospective review only 20/9900 patients were diagnosed with CD involving the esophagus (0.2%), with a median age of 31 at diagnosis.2 The prevalence of endoscopic esophageal CD in the pediatric population is higher. One study showed endoscopic findings of esophageal CD in 7.6% of children with CD, with 17.6% showing histologic evidence of esophageal CD.3 These numbers may be underestimating the true extent in adults, as there is no standard of performing an upper endoscopy in asymptomatic CD patients, which is commonly performed in the pediatric population. The mid and distal esophagus is more commonly affected.1,2
Most common presenting symptoms are odynophagia, dysphagia, heartburn, chest pain, and aphthous ulcers. Rarely patients may present with fistulizing disease involving the bronchus, stomach, or mediastinum. Patients with advanced disease may also present with an esophageal stricture. Most often patients will have extraesophageal involvement.2 Esophageal CD at time of CD diagnosis is rare, and the median interval between the diagnosis of extraesophageal CD and CD involving the esophagus was 1-3 years. Upper endoscopy with multiple biopsies is required to establish the diagnosis. Common endoscopic findings include aphthous ulcers, serpiginous ulcers, nodules, pseudopolyps, and skip lesions.4,5 Biopsies are not only important to diagnose CD but are important to rule out a neoplasm. Esophageal lesions must be differentiated from reflux esophagitis, infectious esophagitis (cytomegalovirus, herpes simplex virus), pill esophagitis, tuberculosis, sarcoidosis, Behcet’s disease, and malignancy.
The most common histological findings are nonspecific chronic inflammation, and granulomas are rare. A lymphocytic infiltrate in the lamina propria is commonly seen.2 The findings of noncaseating granulomas are neither sensitive nor specific as they are present in only 7%-9% of esophageal CD patients.6 The clinical diagnosis of esophageal CD can be difficult and is made through a combination of historical, endoscopic, and pathologic findings.
There are no treatment guidelines specific for esophageal CD. D'Haens et al followed 14 patients for 83 patient years, and 9 out of 12 patients responded well to steroid treatment.7 Various treatments include proton pump inhibitors, oral steroids, antimetabolites, and anti-TNF agents.8 Strictures may require dilation for symptomatic management. Our patient responded very well to corticosteroid therapy followed by initiation of adalimumab.
Disclosures
Author contributions: G. Kasarala is the article guarantor. G. Kasarala, G. Harvin, and S. Durrett wrote the manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.De Felice KM, Katzka DA, Raffals LE. Crohn's disease of the esophagus: Clinical features and treatment outcomes in the biologic era. Inflamm Bowel Dis. 2015; 21(9):2106–13. [DOI] [PubMed] [Google Scholar]
- 2.Decker GA, Loftus EV Jr, Pasha TM, Tremaine WJ, Sandborn WJ. Crohn's disease of the esophagus: Clinical features and outcomes. Inflamm Bowel Dis. 2001; 7(2):113–9. [DOI] [PubMed] [Google Scholar]
- 3.Ramaswamy K, Jacobson K, Jevon G, Israel D. Esophageal Crohn disease in children: A clinical spectrum. J Pediatr Gastroenterol Nutr. 2003; 36(4):454–8. [DOI] [PubMed] [Google Scholar]
- 4.Geboes K, Janssens J, Rutgeerts P, Vantrappen G. Crohn's disease of the esophagus. J Clin Gastroenterol. 1986; 8(1):31–7. [DOI] [PubMed] [Google Scholar]
- 5.Jevon GP, Madhur R. Endoscopic and histologic findings in pediatric inflammatory bowel disease. Gastroenterol Hepatol (NY). 2010; 6(3):174–80. [PMC free article] [PubMed] [Google Scholar]
- 6.Howden FM, Mills LRt, Rubin JW. Crohn's disease of the esophagus. Am Surg. 1994; 60(9):656–60. [PubMed] [Google Scholar]
- 7.D'Haens G, Rutgeerts P, Geboes K, Vantrappen G. The natural history of esophageal Crohn's disease: Three patterns of evolution. Gastrointest Endosc. 1994; 40(3):296–300. [DOI] [PubMed] [Google Scholar]
- 8.Isaacs KL. Crohn's disease of the esophagus. Curr Treat Options Gastroenterol. 2007; 10(1):61–70. [DOI] [PubMed] [Google Scholar]