Abstract
Aims
To examine the efficacy and safety of once‐weekly dulaglutide 0.75 mg monotherapy compared with once‐daily liraglutide 0.9 mg in Japanese patients with type 2 diabetes (T2D) for 52 weeks.
Methods
We conducted a phase III, randomized, 52‐week (26‐week primary endpoint), active‐ and placebo‐controlled trial comparing 492 Japanese patients (dulaglutide, n = 281; liraglutide, n = 141; and placebo, n = 70). Participants and investigators were blinded to treatment assignment for dulaglutide and placebo but not for liraglutide (open‐label comparator); after 26 weeks, patients randomized to placebo were switched to once‐weekly dulaglutide 0.75 mg (open‐label). The present paper reports results for patients treated with dulaglutide and patients treated with liraglutide for 52 weeks.
Results
At week 52, dulaglutide decreased HbA1c significantly from baseline compared with liraglutide [least squares mean difference: −0.20; 95% confidence interval (CI) −0.39, −0.01; p = 0.04]. At week 52 (last observation carried forward), dulaglutide significantly decreased pre‐ and post‐dinner blood glucose (BG) levels, the mean of seven‐point self‐monitored BG profiles, the mean of all postprandial BG levels and circadian variation compared with liraglutide. Body weight was generally stable in both groups through 52 weeks. The most frequently reported adverse events were nasopharyngitis, constipation, nausea and diarrhoea. Eight dulaglutide‐treated (2.9%) and four liraglutide‐treated (2.9%) patients reported hypoglycaemia, with no event being severe.
Conclusions
Monotherapy with once‐weekly dulaglutide 0.75 mg was effective and safe in Japanese patients with T2D, with better glycaemic control compared with once‐daily liraglutide 0.9 mg.
Keywords: dulaglutide, GLP‐1 receptor agonist, liraglutide, type 2 diabetes
Introduction
The initiation of incretin‐related therapy by dipeptidyl peptidase‐4 (DPP‐4) inhibitor and glucagon‐like peptide‐1 (GLP‐1) receptor agonists has changed the treatment strategy for type 2 diabetes (T2D) over the past 5 years. Native GLP‐1 is released from intestinal L‐cells in response to the ingestion of food, and mediates glucose metabolism by stimulating glucose‐dependent insulin secretion, inhibiting glucagon secretion and slowing gastric emptying. DPP‐4 inhibitors increase native GLP‐1 by inhibiting degradation; however, GLP‐1 receptor agonists directly stimulate GLP‐1 receptors, which results in a different treatment profile (e.g. less weight gain, less hypoglycaemia and occurrence of gastrointestinal adverse events) from those of other diabetic treatment options such as sulphonylureas and insulin. In addition to the conventional treatments, GLP‐1 receptor agonists have been established as one of the optimum injectable therapies for patients with T2D. GLP‐1 receptor agonists may be categorized as short‐acting (twice‐daily exenatide 1 and lixisenatide 2) or long‐acting (liraglutide 3, exenatide once‐weekly 4, albiglutide 5 and dulaglutide 6, 7, 8). Short‐ and long‐acting GLP‐1 receptor agonists have different profiles and allow clinicians to provide optimum treatment in response to individual patients' diabetic profiles 9. In addition, the different pharmacokinetic profiles among the GLP‐1 receptor agonists influence the frequency and dosage of administration, which allow further options for customization to patients' adherence and preferences 10, 11.
Among short‐acting GLP‐1 receptor agonists, a recent head‐to‐head study of once‐daily lixisenatide versus twice‐daily exenatide found no statistically significant differences in glycated haemoglobin (HbA1c) reduction over 24 weeks, despite the different dosing regimens 12; however, exenatide twice‐daily has not shown non‐inferiority to once‐daily liraglutide, a long‐acting GLP‐1 receptor agonist 13. Among the long‐acting receptor agonists, exenatide once‐weekly and albiglutide were also not non‐inferior to liraglutide 14, 15. Dulaglutide is a once‐weekly GLP‐1 receptor agonist; in global phase III trials in patients with T2D, dulaglutide 1.5 mg once‐weekly resulted in a statistically significant reduction in HbA1c from baseline compared with metformin, sitagliptin, insulin glargine and exenatide twice‐daily, with sustained effects on fasting and postprandial blood glucose (BG) levels 16, 17, 18, 19. Dulaglutide 1.5 mg was also non‐inferior to liraglutide 1.8 mg at 26 weeks in the AWARD‐6 study, which was the first study to show non‐inferiority of any GLP‐1 receptor agonist comparator to liraglutide 20.
In the primary results of this study at 26 weeks, dulaglutide 0.75 mg was non‐inferior to liraglutide 0.9 mg and superior to placebo in HbA1c reduction [least squares (LS) mean differences for dulaglutide – liraglutide and for dulaglutide – placebo were −0.10 and −1.57%, respectively], and 71% of dulaglutide‐treated patients achieved the HbA1c target of <7.0% 21. The dulaglutide dosage in Japan was half of the maximum dose approved in the USA and the European Union 6, 7, 8 and the liraglutide dosage in Japan (0.9 mg) was also half of the maximum dose approved in the USA and the European Union (1.8 mg) 3. In a randomized, double‐blind study of once‐weekly dulaglutide 0.75 mg versus once‐daily insulin glargine in Japanese patients with T2D treated with sulphonylureas and/or biguanides, dulaglutide was superior to insulin glargine at 26 weeks (LS mean difference in HbA1c, −0.54%), and 71% of dulaglutide‐treated patients achieved the HbA1c target of <7.0% 22.
This study assessed the efficacy and safety of once‐weekly dulaglutide 0.75 mg for 52 weeks compared with once‐daily liraglutide 0.9 mg, the highest available liraglutide dose in Japan, both as monotherapy. This was the first study of dulaglutide compared with liraglutide for 52 weeks.
Materials and Methods
Study Design and Patients
This was a phase III, randomized, 52‐week (26‐week primary endpoint), active‐ and placebo‐controlled trial examining the efficacy and safety of once‐weekly dulaglutide monotherapy in Japanese patients with T2D who had discontinued oral antidiabetic medication (OAM) monotherapy or were OAM‐naïve. This study was a registration trial that was conducted in accordance with the Guideline for Clinical Evaluation of Oral Hypoglycemic Agents in Japan 23. This guideline states that 24 weeks is the ideal length of treatment for a phase III, randomized, double‐blind, monotherapy study comparing a new OAM under development with a marketed comparator (control); therefore, 26 weeks was chosen as the primary evaluation time point for this study. An additional 26 weeks of treatment was added to the study to collect further safety and efficacy data. During the first 26 weeks of the study, participants and investigators were blinded to treatment assignment for dulaglutide and placebo but not for liraglutide (open‐label comparator). At 26 weeks, patients in the placebo group were switched to once‐weekly dulaglutide for the remainder of the 52‐week controlled study. In this paper, ‘dulaglutide‐treated patients’ or ‘the dulaglutide group’ refer only to patients randomized to dulaglutide treatment for the entire 52‐week treatment period. At the completion of participation or early discontinuation, all patients were required to participate in a 30‐day safety follow‐up period.
Data were collected at 33 Japanese sites from April 2012 to May 2014. During the 2‐week screening period, patients were screened for eligibility and then entered a 2‐week lead‐in period for OAM‐naïve patients or an 8‐week wash‐out period for patients on OAM monotherapy. The study was registered at ClinicalTrials.gov (NCT01558271).
The trial design and study population details have been previously reported 21. Eligible Japanese patients were men or women aged ≥20 years who were OAM‐naïve (diet and exercise only) or had discontinued OAM monotherapy (excluding thiazolidinedione). Furthermore, eligible patients had a body mass index (BMI) between 18.5 and 35.0 kg/m2 and HbA1c levels between 7.0 and 10.0%, confirmed at randomization.
Subcutaneous dulaglutide injections were initiated at the full dose. Subcutaneous liraglutide injections were uptitrated from 0.3 mg/day during week 1 to 0.6 mg/day during week 2 and 0.9 mg/day starting at week 3, according to the Japanese label. Patients not tolerating study treatment were to be discontinued from the study drug but remain in the study to collect safety data.
A common protocol was approved at each site by an institutional review board, and the study was performed in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice 24. Each patient provided written informed consent before participation.
Study Endpoints and Assessments
The primary objective of the study was to demonstrate superiority of once‐weekly dulaglutide versus placebo on HbA1c change from baseline at 26 weeks, as previously reported 21. Secondary objectives at 52 weeks evaluated change from baseline in HbA1c, the proportions of patients who achieved HbA1c targets (<7.0 or ≤6.5%), changes in fasting serum glucose (FSG) from baseline, changes in seven‐point self‐monitored BG (SMBG) profiles from baseline, changes in body weight from baseline, updated homoeostasis model assessment of β‐cell function (HOMA2‐%β) and updated homoeostasis model assessment of insulin sensitivity (HOMA2‐%S). SMBG profiles were collected over 2 non‐consecutive days within 2 weeks of baseline and at weeks 14, 26 and 52. Safety assessments included adverse events, hypoglycaemia, vital signs (pulse rate and blood pressure), ECGs, laboratory variables and dulaglutide antidrug antibodies. All patients were tested for the development of dulaglutide antidrug antibodies. Hypoglycaemia was defined as a BG concentration of ≤3.9 mmol/l and/or symptoms and/or signs attributable to hypoglycaemia. Severe hypoglycaemia was defined as an episode requiring the assistance of another person to actively administer therapy 25. Patients were allowed to initiate rescue therapy for severe, persistent hyperglycaemia according to predefined thresholds for fasting BG for at least 2 weeks with no readily identifiable cause.
Cardiovascular adverse events and pancreatitis were adjudicated by separate independent, external committees, using prespecified criteria, study evidence and clinical knowledge and experience.
This paper presents results through the full 52 weeks of treatment for only the dulaglutide and liraglutide treatment groups, with the addition of relevant safety findings in patients receiving placebo/dulaglutide.
Statistical Analyses
The definitions of the analysis populations (full analysis set and safety analysis set) were previously reported 21. The sample size of the study was calculated based on the comparisons at week 26 21. The sample size of at least 490 randomized patients was selected to provide > 99% power to demonstrate superiority of dulaglutide to placebo. This assumed a true mean difference in HbA1c change from baseline between dulaglutide and placebo of 0.8%, a common standard deviation of 1.1%, a one‐sided significance level of 0.025, and a 9% drop‐out rate between randomization and week 26. Moreover, assuming no difference between dulaglutide and liraglutide, the given sample size provided at least 90% power to confirm non‐inferiority of dulaglutide to liraglutide with a margin of 0.4%. Analyses at the 52‐week endpoint compared only dulaglutide with liraglutide. The primary efficacy analysis of the study was the comparison at week 26, and no adjustments for multiplicity were performed for the results at week 52.
Analyses for continuous variables such as HbA1c used a mixed model for repeated measures. Seven‐point SMBG profiles and vital signs were analysed using an analysis of covariance (ancova) model. The mixed model for repeated measures and ancova models used at week 52 were the same as previously reported 21. For categorical measurements such as the proportions of patients with HbA1c <7.0 or ≤6.5% at week 52 (LOCF), Cochran–Mantel–Haenszel tests stratified by prestudy therapy and baseline BMI were performed. For other categorical measurements, such as treatment‐emergent adverse events, Fisher's exact tests were performed.
Results
Patients
Figure 1 summarizes study disposition: 281 and 141 patients were randomized to treatment with dulaglutide or liraglutide, respectively; of these, 280 and 137 patients were treated with dulaglutide or liraglutide, respectively. Of the patients randomized to dulaglutide or liraglutide, a total of 387 patients (263 in the dulaglutide group, 124 in the liraglutide group) remained in the study for 52 weeks. A total of 18 patients (6.4%) randomized to dulaglutide and 17 patients (12.1%) randomized to liraglutide discontinued the study, with withdrawal by subject being the most common reason [dulaglutide, 10 patients (3.6%), liraglutide, 12 patients (8.5%)]. Patient demographics and baseline characteristics were similar in the two groups (Table 1).
Figure 1.
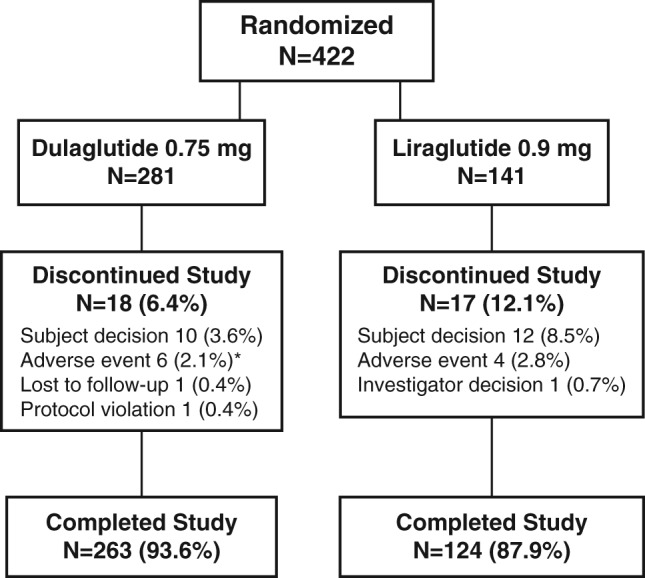
Study disposition. Patients were randomized to dulaglutide or liraglutide in a 2 : 1 ratio. N, number of patients. *Includes a patient who was discontinued from the study because of a serious adverse event, rectal cancer, which was diagnosed after treatment was interrupted. Because the event began after treatment ended it is not included in the serious adverse events in Table 2 or listed in Table S2.
Table 1.
Baseline demographics and characteristics.
| Variable | Dulaglutide 0.75 mg (N = 280) | Liraglutide 0.9 mg (N = 137) |
|---|---|---|
| Sex, n (%) | ||
| Men | 228 (81) | 113 (83) |
| Women | 52 (19) | 24 (18) |
| Mean (s.d.) age, years | 57.2 (9.6) | 57.9 (10.4) |
| Age ≥65 years, n (%) | 68 (24%) | 39 (29%) |
| Mean (s.d.) weight, kg | 71.3 (12.5) | 70.2 (12.5) |
| Mean (s.d.) BMI, kg/m2 | 25.6 (3.6) | 25.5 (3.5) |
| Mean (s.d.) diabetes duration, years | 6.8 (5.6) | 6.3 (6.0) |
| Mean (s.d.) HbA1c, % | 8.15 (0.77) | 8.08 (0.89) |
| HbA1c >8.5%, n (%) | 89 (32%) | 42 (31%) |
| Mean (s.d.) FSG, mmol/l | 9.4 (1.9) | 9.0 (1.9) |
| Prestudy OAM therapy, n (%) | 94 (34%) | 48 (35%) |
| OAM‐naïve, n (%) | 186 (66%) | 89 (65%) |
| Mean (s.d.) HOMA2‐%β (fasting insulin) | 34.5 (19.4) | 36.9 (20.3) |
| Mean (s.d.) HOMA2‐%S (fasting insulin) | 99.3 (53.8) | 100.7 (52.8) |
All patients were from Japan. BMI, body mass index; FSG, fasting serum glucose; HbA1c, glycated haemoglobin; HOMA2‐%β, updated homoeostasis model assessment of β‐cell function; HOMA2‐%S, updated homoeostasis model assessment of insulin sensitivity; N, number of patients in full analysis set; OAM, oral antidiabetic medication; s.d., standard deviation.
Efficacy
In both treatment groups, HbA1c was significantly reduced from baseline from weeks 4 to 52 (Figure 2A). The LS mean (standard error [s.e.]) changes from baseline to week 52 in HbA1c were −1.39% (0.06) and −1.19% (0.08) for dulaglutide and liraglutide, respectively. Dulaglutide significantly reduced HbA1c compared with liraglutide: the LS mean treatment difference (dulaglutide − liraglutide) and 95% confidence interval (CI) were −0.20% (−0.39, −0.01%); p = 0.04 (Figure 3A). In OAM‐naïve patients (previously on diet therapy only), the LS mean (s.e.) changes from baseline in HbA1c at week 52 were −1.45% (0.07) in the dulaglutide group (n = 186) and −1.21% (0.10) in the liraglutide group (n = 88). In patients previously treated with OAM, the LS mean (s.e.) changes from baseline in HbA1c were −1.35% (0.09) in the dulaglutide group (n = 94) and −1.26% (0.13) in the liraglutide group (n = 47).
Figure 2.

Glycated haemoglobin (HbA1c), fasting serum glucose (FSG), and body weight up to week 52. (A) Mean [standard error (s.e.)] HbA1c (%) from baseline to week 52. *p = 0.04 for between‐group difference; p < 0.001 for all within‐group changes from baseline for both treatment groups. (B) Mean (s.e.) FSG (mmol/l) from baseline to week 52. (C) Mean (s.e.) changes from baseline in body weight (kg) from baseline to week 52. LS, least squares.
Figure 3.
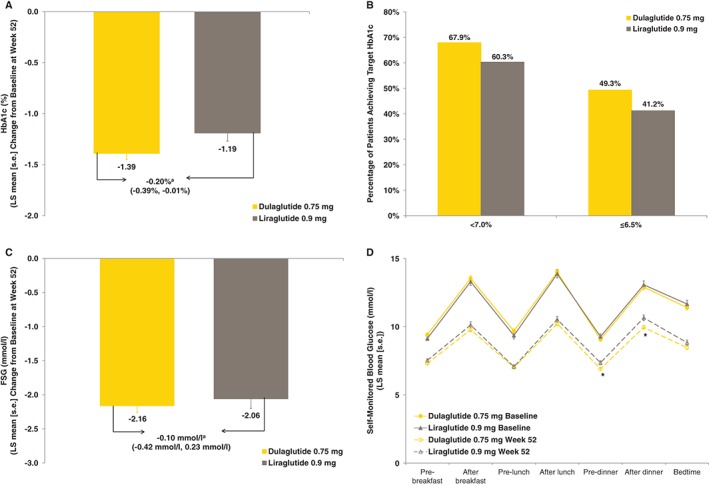
Glycated haemoglobin (HbA1c) changes from baseline, HbA1c targets, fasting serum glucose (FSG) and self‐monitored blood glucose (SMBG). (A) Mean (s.e.) changes from baseline to week 52 in HbA1c (%). (B) Proportions of patients achieving predefined HbA1c targets at week 52 (LOCF). (C) Mean (s.e.) changes from baseline to week 52 in FSG (mmol/l). (D) Mean (s.e.) seven‐point SMBG profiles (mmol/l) at baseline and week 52 (LOCF). aLeast squares (LS) mean difference (95% confidence interval): treatment difference calculated as dulaglutide 0.75 mg – liraglutide 0.9 mg. *Reduction from baseline in the dulaglutide 0.75 mg group was significantly greater than reduction in the liraglutide 0.9 mg group (p < 0.05).
The percentages of patients who achieved HbA1c <7.0 and ≤6.5% were similar between dulaglutide and liraglutide at week 52 (LOCF): 190/280 patients (67.9%) versus 82/136 patients (60.3%) and 138/280 patients (49.3%) versus 56/136 patients (41.2%), respectively (Figure 3B).
Reductions from baseline in FSG were similar in both treatment groups at week 52 (Figure 2B). The LS mean (s.e.) changes from baseline in FSG at week 52 were −2.16 mmol/l (0.10) and −2.06 mmol/l (0.14) for dulaglutide and liraglutide, respectively (Figure 3C). Treatment with dulaglutide significantly decreased the following seven‐point SMBG profile values from baseline at week 52 (LOCF) compared with liraglutide: pre‐ and post‐dinner BG levels, mean of the seven‐point SMBG profiles, mean of all postprandial BG levels, and circadian variation (daily circadian variation was calculated as the difference between maximum and minimum BG values collected on a particular day; Table S1). Figure 3D plots mean (s.e.) seven‐point SMBG profiles at baseline and week 52 (LOCF).
No clinically significant changes from baseline in body weight were observed in either treatment group (Figure 2C). At week 52, the LS mean changes were −0.17 and −0.13 kg for dulaglutide and liraglutide, respectively, and the treatment difference was not statistically significant.
Treatment in both groups significantly increased HOMA2‐%β (based on fasting insulin) from baseline to week 52 (LOCF; p < 0.001); the treatment difference was not significant (Figure S1A). Treatment with dulaglutide significantly decreased HOMA2‐%S (based on fasting insulin) from baseline to week 52 (LOCF; p < 0.001); the treatment difference was not significant (Figure S1B).
Safety
Table 2 summarizes treatment‐emergent adverse events, including the most frequently reported treatment‐emergent adverse events. No deaths were reported during the treatment period. The incidences of serious adverse events and treatment‐emergent adverse events were similar between the groups (Tables 2 and S2). Of the events occurring in ≥ 5% of patients in either group, only decreased appetite was significantly different between the dulaglutide and liraglutide groups [dulaglutide, two patients (0.7%); liraglutide, eight patients (5.8%); p = 0.003]. One patient, in the dulaglutide group, reported severe constipation; all other treatment‐emergent gastrointestinal adverse events were considered of mild or moderate intensity. The percentages of patients in each group who discontinued the study because of an adverse event were 1.8 and 2.9% for dulaglutide and liraglutide, respectively (Table 2). One dulaglutide‐treated and four liraglutide‐treated patients discontinued the study drug because of treatment‐emergent gastrointestinal adverse events.
Table 2.
Safety assessments up to week 52.
| Dulaglutide 0.75 mg (N = 280) | Liraglutide 0.9 mg (N = 137) | p | |
|---|---|---|---|
| Deaths | 0 | 0 | NA |
| Serious adverse events* | 9 (3.2) | 7 (5.1) | 0.416 |
| Patients with at least one treatment‐emergent adverse event | 185 (66.1) | 94 (68.6) | 0.658 |
| Treatment‐emergent adverse events (≥5% in either group) | |||
| Nasopharyngitis | 52 (18.6) | 24 (17.5) | 0.893 |
| Decreased appetite | 2 (0.7) | 8 (5.8) | 0.003 |
| Gastrointestinal disorders | 76 (27.1) | 51 (37.2) | 0.041 |
| Constipation | 22 (7.9) | 11 (8.0) | >0.999 |
| Diarrhoea | 20 (7.1) | 6 (4.4) | 0.388 |
| Nausea | 17 (6.1) | 11 (8.0) | 0.532 |
| Abdominal distension | 12 (4.3) | 7 (5.1) | 0.803 |
| Patients who discontinued study because of an adverse event | 5 (1.8) | 4 (2.9) | 0.484 |
| Seated vital signs, mean change from baseline (s.e.)†, ‡ | |||
| Systolic blood pressure, mmHg | 1.45 (0.64) | −1.58 (0.92) | 0.007 |
| Diastolic blood pressure, mmHg | 1.56 (0.40) | 1.27 (0.58) | 0.680 |
| Pulse rate, bpm | 3.45 (0.42) | 4.99 (0.60) | 0.036 |
| ECG PR interval: mean change from baseline (s.e.), ms;† | 2.81 (0.82) | 3.71 (1.03) | 0.398 |
| Pancreatic enzymes (median change, Q1, Q3) | |||
| Total amylase, U/l‡ | 7.0 (1.0, 14.0)** | 6.0 (1.0, 11.0)** | 0.206 |
| Lipase, U/l‡ | 6.0 (1.0, 12.0)** | 9.0 (3.0, 19.0)** | <0.001 |
| Patients with treatment‐emergent abnormal change in pancreatic enzymes (>ULN)§ | |||
| Total amylase | 19/261 (7.3) | 9/124 (7.3) | 1.000 |
| Lipase | 67/254 (26.4) | 44/121 (36.4) | 0.053 |
| Patients with pancreatic enzyme concentration >3 × ULN | |||
| Total amylase | 1 (0.4) | 0 | 1.000 |
| Lipase | 5 (1.8) | 2 (1.5) | 1.000 |
| Treatment‐emergent dulaglutide antidrug antibodies¶ | |||
| Dulaglutide antidrug antibodies | 3 (1.1) | 0 | NA |
| Dulaglutide neutralizing antidrug antibodies | 2 (0.7) | 0 | NA |
| nsGLP‐1 cross‐reactive antibodies | 2 (0.7) | 0 | NA |
| nsGLP‐1 neutralizing antibodies | 0 | 0 | NA |
| Both nsGLP‐1 neutralizing and cross‐reactive antibodies | 0 | 0 | NA |
p < 0.001 within‐group.
Data are n (%) unless otherwise specified. MedDRA, Medical Dictionary for Regulatory Activities (version 17.0); N, number of patients in safety analysis set; NA, not applicable; nsGLP‐1, native sequence glucagon‐like peptide‐1; Q1, first quartile; Q3, third quartile; s.e., standard error; ULN, upper limit of normal.
Reported serious adverse events are listed in Table S2.
Data are least‐squares mean change (s.e.).
Data are last observation carried forward.
Denominator is patients with enzyme level ≤ ULN at baseline and a postbaseline measurement.
These values include all postbaseline observations including the safety follow‐up.
Eight dulaglutide‐treated (2.9%) and four liraglutide‐treated (2.9%) patients experienced at least one episode of hypoglycaemia; no cases of severe hypoglycaemia were reported. A total of three patients [dulaglutide, two patients (0.7%); liraglutide, one patient (0.7%)] experienced nocturnal hypoglycaemia.
Pancreatic enzymes (amylase and lipase) at week 52 are summarized in Table 2. Treatment with liraglutide significantly increased lipase compared with dulaglutide (median increases 9.0 U/l vs 6.0 U/l, respectively; p < 0.001). Changes from baseline in amylase were not significantly different between the treatments. In both treatment groups, 7.3% of patients had treatment‐emergent postbaseline amylase values above the upper limit of normal (ULN). The percentages of patients with treatment‐emergent postbaseline lipase values above the ULN were dulaglutide, 26.4% and liraglutide, 36.4%. One dulaglutide‐treated patient and no liraglutide‐treated patients experienced amylase values >3 × ULN. Five dulaglutide‐treated patients and two liraglutide‐treated patients, as well as one patient who received placebo for 26 weeks and dulaglutide for 26 weeks, experienced a lipase value >3 × ULN. No cases of pancreatitis were confirmed by adjudication. Two patients were diagnosed with pancreatic carcinoma: a 65‐year‐old man who was treated with placebo and dulaglutide for a total of 52 weeks (diagnosis occurred during the follow‐up period after completion of the treatment period) and a 67‐year‐old woman who was treated with liraglutide for approximately 15 weeks.
All patients had calcitonin values within normal limits.
No confirmed adjudicated cardiovascular events were observed. The mean changes from baseline in seated vital signs and ECG PR interval are shown in Table 2. Treatment with liraglutide resulted in a mean decrease from baseline in seated systolic blood pressure at 52 weeks (LOCF), whereas treatment with dulaglutide resulted in a mean increase from baseline, and the difference was significant (p = 0.007). Liraglutide significantly increased seated pulse rate from baseline at week 52 (LOCF) compared with dulaglutide (p = 0.036). ECG PR interval increases from baseline were similar in both groups (dulaglutide, 2.81 ms; liraglutide, 3.71 ms).
At 52 weeks, renal marker urine albumin/creatinine ratio was decreased from baseline in both treatment groups; the difference was not statistically significant (Table S3). Treatment with dulaglutide statistically significantly decreased serum total cholesterol and triglycerides from baseline at 52 weeks; treatment with liraglutide also significantly decreased total cholesterol, and the differences between dulaglutide and liraglutide were not statistically significant for either variable (Table S4).
Three dulaglutide‐ and no liraglutide‐treated patients had treatment‐emergent dulaglutide antidrug antibodies (Table 2). HbA1c values at baseline and week 52 in the three patients who developed dulaglutide antidrug antibodies during the study were 8.0 and 7.0%, 7.8 and 6.7%, and 7.6 and 6.4%, respectively, and no adverse events of clinical interest were observed in these patients. Based on these results, it did not appear that the development of antidrug antibodies during dulaglutide treatment affected efficacy or safety. Few patients experienced injection site reactions (dulaglutide, 4.6%; liraglutide, 5.1%) or allergic and hypersensitivity reactions (dulaglutide, 0.4%; liraglutide, 2.2%).
Discussion
It was previously reported that dulaglutide was non‐inferior to liraglutide at 26 weeks in this study: LS mean (s.e.) changes from baseline in HbA1c at 26 weeks were dulaglutide, −1.43% (0.05) and liraglutide, −1.33% (0.07); the LS mean difference was −0.10%, and the 95% CI for the difference was (−0.27, 0.07%) 21. At 52 weeks, dulaglutide statistically significantly reduced HbA1c from baseline compared with liraglutide: LS mean (s.e.) changes were −1.39% (0.06) for dulaglutide and −1.19% (0.08) for liraglutide, and the LS mean difference (95% CI) for the difference was −0.20% (−0.39, −0.01%); p = 0.040. This was the first study of a GLP‐1 receptor agonist to show a statistically significant improvement in HbA1c compared with liraglutide. The reduction curves of HbA1c for dulaglutide and liraglutide were similar up to 26 weeks; from 26 to 52 weeks, mean HbA1c values in the dulaglutide group were stable, whereas those in the liraglutide group slightly increased. There was no interaction effect of treatment (dulaglutide or liraglutide) and previous OAM treatment (yes or no) on HbA1c reduction in this study; dulaglutide and liraglutide were equally effective regardless of previous OAM usage. Liraglutide was also equally effective regardless of previous OAM usage in a previous phase III study of liraglutide monotherapy in Japan 26. There were no statistically significant differences between dulaglutide and liraglutide in reductions from baseline in FSG at any time point (weeks 14, 26, 38 or 52); however, the LS mean decrease from baseline in the mean of the seven‐point SMBG profiles with dulaglutide was significantly greater than that with liraglutide at week 52 (LOCF). In addition, dulaglutide significantly lowered the mean of all postprandial BG levels and the pre‐ and post‐dinner BG levels compared with liraglutide at week 52 (LOCF). The LS mean decrease in the circadian variation from the seven‐point SMBG profiles in the dulaglutide group was also significantly greater compared with the liraglutide group. Taken together, these results indicate that dulaglutide may have a more sustained, less fluctuating, and more desirable effect on BG control, with reduction of postprandial BG levels compared with liraglutide.
Mean body weight at 52 weeks was largely unchanged from baseline in the dulaglutide and liraglutide groups, and the treatment difference was not statistically significant. Also, based on another phase III dulaglutide study in Japan, body weight changes with dulaglutide may be dependent on concomitant therapies; biguanides and α‐glucosidase inhibitors with dulaglutide may tend to reduce body weight, whereas concomitant therapy with thiazolidinediones, sulphonylureas or glinides may result in stable body weight or body weight gain 27.
In the present study, long‐term once‐weekly administration of dulaglutide 0.75 mg in Japanese patients with T2D was generally well tolerated. The incidence of treatment‐emergent adverse events up to 52 weeks was also not significantly different between dulaglutide and liraglutide. Gastrointestinal adverse events were among the most commonly reported treatment‐emergent adverse events in both groups and occurred at similar rates in both groups. Nausea was mainly observed in the first 2 weeks after starting dulaglutide (data not shown). The incidence of decreased appetite through 52 weeks in the dulaglutide group was significantly lower than in the liraglutide group.
The incidence of hypoglycaemia through 52 weeks was low in both treatment groups, consistent with monotherapy in the GLP‐1 receptor agonist class 26, 28. No severe hypoglycaemia was observed in either treatment group during the treatment period.
In a 26‐week study of dulaglutide using ambulatory blood pressure monitoring, treatment with dulaglutide 0.75 mg resulted in a mean reduction of 1.6 mmHg in 24‐h systolic blood pressure 29; however, in this study, small mean increases from baseline in seated systolic blood pressure were observed in the dulaglutide group at 26 and 52 weeks (0.62 and 1.45 mmHg, respectively) 21. These results also differ slightly from other studies of GLP‐1 receptor agonists in Japan, which showed no changes or decreases from baseline in systolic blood pressure 26, 30. Changes in seated systolic blood pressure in previous studies of dulaglutide 0.75 mg in Japan have varied. In a 26‐week study in combination with sulphonylureas and/or biguanides the mean change was 0.4 mmHg 22, and in a 52‐week study in combination with a single OAM, mean changes across the five treatment groups ranged from −2.1 to 1.0 mmHg 27. In this study, a statistically significant increase in pulse rate was observed in the liraglutide group at 52 weeks compared with the dulaglutide group. There were no clinically significant safety concerns in ECG PR interval in either group.
At week 52 (LOCF), statistically significant increases from baseline were observed in serum amylase and lipase levels in both treatment groups. The median increase in lipase in the dulaglutide group was significantly smaller than the increase in the liraglutide group; this result was similar to that seen in the global phase III AWARD‐6 study 20. The timing of increased lipase values varied and did not appear predictable; furthermore, increases in lipase were not sustained (data not shown) and did not predict pancreatitis. There were no confirmed cases of pancreatitis.
Although dulaglutide and placebo were blinded during the first 26 weeks of this study, the open‐label administration of liraglutide (necessary because placebo for liraglutide was not commercially available) during the entire 52‐week study and of dulaglutide during the extension phase may have affected physicians' and patients' behaviour. The dulaglutide and liraglutide treatment groups in study AWARD‐6 were also unblinded 20.
The length of the present study was relatively short in view of the required chronic treatment of patients with T2D; however, this is the longest study to date comparing liraglutide and a once‐weekly GLP‐1 receptor agonist.
In conclusion, monotherapy with once‐weekly dulaglutide 0.75 mg was effective and well tolerated in Japanese patients with T2D, with better glycaemic control compared with once‐daily liraglutide 0.9 mg over 52 weeks.
Conflict of Interest
M. O. has received grants from Eli Lilly, Novo Nordisk, and Sanofi; advisory panel fees from Eli Lilly, Novo Nordisk, and Sanofi; research support from Eli Lilly, Novo Nordisk, and Sanofi; and speaker's bureau fees from Eli Lilly, Novo Nordisk, and Sanofi. J. M. has received a grant from Boehringer Ingelheim and Eli Lilly and research support from Astra Zeneca, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly, Kowa Pharmaceutical, Novartis Pharma, Ono Pharmaceutical, and Sanwa Kagaku Kenkusho. T. T. has received a grant from Eli Lilly and speaker's bureau fees from Eli Lilly and Novo Nordisk. N. I., Y. T. and T. I. are employees of Eli Lilly Japan K.K., and T. I. has the company stock option.
M. O., J. M. and T. T. were trial investigators and participated in data collection. N. I., Y. T. and T. I. prepared the first draft of the manuscript. Y. T. was responsible for the statistical considerations in the analysis and trial design. N. I. and T. I. were responsible for trial design and medical oversight during the trial. All authors participated in reviewing and interpreting the data and providing comments and revisions to the manuscript. All authors approved the final version of the manuscript and take full responsibility for the content.
Supporting information
Figure S1. Updated homoeostasis model assessment changes from baseline at week 52 (LOCF).
Table S1. Summary of least squares (±standard error) mean changes from baseline in self‐monitored blood glucose (mmol/l) values (LOCF at week 52).
Table S2. Summary of serious adverse events by preferred term and treatment for the treatment period from baseline to 52 weeks.
Table S3. Summary and analysis of renal analytes: median baseline values and median changes from baseline to 52 weeks (LOCF).
Table S4. Summary and analysis of lipid profiles: median baseline values and median absolute and percent changes from baseline to 52 weeks (LOCF).
Acknowledgements
The trial was sponsored by Eli Lilly Japan K.K. (Kobe, Japan). We thank the study investigators, staff, and participants for their needed contributions. The authors would like to thank Mary Re (inVentiv Health Clinical) and Akiko Matsui, PhD (Eli Lilly Japan K.K) for medical writing contributions. We would also like to thank Miwa Sakaridani (Eli Lilly Japan K.K.) for clinical trial management of the study.
References
- 1. Byetta ([exenatide] injection) [prescribing information]. Wilmington, DE: AstraZeneca Pharmaceuticals LP; 2015. Available from URL: http://www.azpicentral.com/byetta/pi_byetta.pdf. Accessed 10 July 2015.
- 2. Sanofi‐Aventis Deutschland GmbH Lixisenatide (Lyxumia) . Summary of product characteristics. EMA website. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Product_Information/human/002445/WC500140401.pdf. Accessed 10 July 2015.
- 3. Victoza® (liraglutide [rDNA origin] injection, solution for subcutaneous use) [prescribing information]. Bagsvaerd, Denmark: Novo Nordisk A/S; 2015. Available from URL: http://www.novo‐pi.com/victoza.pdf. Accessed 10 July 2015.
- 4. Bydureon® ([exenatide extended‐release] for injectable suspension) [prescribing information]. Wilmington, DE: AstraZeneca Pharmaceuticals LP; 2015. Available from URL: http://www.azpicentral.com/bydureon/pi_bydureon.pdf Accessed 10 July 2015.
- 5. Tanzeum ([albiglutide] for injection, for subcutaneous use) [prescribing information]. Wilmington, DE: GlaxoSmithKline LLC; 2015. Available from URL: https://gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Tanzeum/pdf/TANZEUM‐PI‐MG‐IFU‐COMBINED.PDF. Accessed 10 July 2015.
- 6. Trulicity® ([dulaglutide] injection, for subcutaneous use) [prescribing information]. Indianapolis, IN: Eli Lilly and Company; 2015. Available from URL: http://pi.lilly.com/us/trulicity‐uspi.pdf. Accessed 10 July 2015.
- 7. Trulicity® [Summary of product characteristics]. Houten, The Netherlands: Eli Lilly and Company; 2015. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Product_Information/human/002825/WC500179470.pdf. Accessed 10 July 2015.
- 8. Trulicity® Ateos® (dulaglutide [gene recombination] injection) [Japan package insert]. Hyogo, Japan: Eli Lilly Japan K.K.; 2015. Available from URL: http://www.info.pmda.go.jp/downfiles/ph/PDF/530471_2499416G1029_1_03.pdf (in Japanese). Accessed 13 October 2015.
- 9. Meier JJ. GLP‐1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol 2012; 8: 728–742. [DOI] [PubMed] [Google Scholar]
- 10. Johnston SS, Nguyen H, Felber E et al. Retrospective study of adherence to glucagon‐like peptide‐1 receptor agonist therapy in patients with type 2 diabetes mellitus in the United States. Adv Ther 2014; 31: 1119–1133. [DOI] [PubMed] [Google Scholar]
- 11. Aroda VR, DeYoung MB. Clinical implications of exenatide as a twice‐daily or once‐weekly therapy for type 2 diabetes. Postgrad Med 2011; 123: 228–238. [DOI] [PubMed] [Google Scholar]
- 12. Rosenstock J, Raccah D, Koranyi L et al. Efficacy and safety of lixisenatide once daily versus exenatide twice daily in type 2 diabetes inadequately controlled on metformin: a 24‐week, randomized, open‐label, active‐controlled study (GetGoal‐X). Diabetes Care 2013; 36: 2945–2951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Buse JB, Rosenstock J, Sesti G et al. LEAD‐6 Study Group. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26‐week randomised, parallel‐group, multinational, open‐label trial (LEAD‐6). Lancet 2009; 374: 39–47. [DOI] [PubMed] [Google Scholar]
- 14. Buse JB, Nauck M, Forst T et al. Exenatide once‐weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION‐6): a randomised, open‐label study. Lancet 2013; 381: 117–124. [DOI] [PubMed] [Google Scholar]
- 15. Pratley RE, Nauck MA, Barnett AH et al. Once‐weekly albiglutide versus once‐daily liraglutide in patients with type 2 diabetes inadequately controlled on oral drugs (HARMONY 7): a randomised, open‐label, multicentre, non‐inferiority phase 3 study. Lancet Diabetes Endocrinol 2014; 2: 289–297. [DOI] [PubMed] [Google Scholar]
- 16. Wysham C, Blevins T, Arakaki R et al. Efficacy and safety of dulaglutide added on to pioglitazone and metformin versus exenatide in type 2 diabetes in a randomized controlled trial (AWARD‐1). [Erratum appears in Diabetes Care 2014; 37: 2895]. Diabetes Care 2014; 37: 2159–2167. [DOI] [PubMed] [Google Scholar]
- 17. Umpierrez G, Tofé Povedano S, Pérez Manghi F, Shurzinske L, Pechtner V. Efficacy and safety of dulaglutide monotherapy versus metformin in type 2 diabetes in a randomized controlled trial (AWARD‐3). Diabetes Care 2014; 37: 2168–2176. [DOI] [PubMed] [Google Scholar]
- 18. Nauck M, Weinstock RS, Umpierrez GE, Guerci B, Skrivanek Z, Milicevic Z. Efficacy and safety of dulaglutide versus sitagliptin after 52 weeks in type 2 diabetes in a randomized controlled trial (AWARD‐5). Diabetes Care 2014; 37: 2149–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Giorgino F, Benroubi M, Sun JH, Zimmermann AG, Pechtner V. Efficacy and safety of once‐weekly dulaglutide versus insulin glargine in patients with type 2 diabetes on metformin and glimepiride (AWARD‐2). Diabetes Care 2015; 38: 2241–2249. [DOI] [PubMed] [Google Scholar]
- 20. Dungan KM, Povedano ST, Forst T et al. Once‐weekly dulaglutide versus once‐daily liraglutide in metformin‐treated patients with type 2 diabetes (AWARD‐6): a randomised, open‐label, phase 3, non‐inferiority trial. [Erratum appears in Lancet 2014; 384: 1348]. Lancet 2014; 384: 1349–1357. [DOI] [PubMed] [Google Scholar]
- 21. Miyagawa J, Odawara M, Takamura T, Iwamoto N, Takita Y, Imaoka T. Once‐weekly glucagon‐like peptide‐1 receptor agonist dulaglutide is non‐inferior to once daily liraglutide and superior to placebo in Japanese patients with type 2 diabetes: a 26‐week randomized phase III study. Diabetes Obes Metab 2015; 17: 974–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Araki E, Inagaki N, Tanizawa Y, Oura T, Takeuchi M, Imaoka T. Efficacy and safety of once‐weekly dulaglutide in combination with sulphonylurea and/or biguanide compared with once daily insulin glargine in Japanese patients with type 2 diabetes: a randomized, open‐label, phase III, non‐inferiority study. Diabetes Obes Metab 2015; 17: 994–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ministry of Health, Labour and Welfare ; 2010. On release of the guideline for clinical evaluation of oral hypoglycemic agents. Available from URL: https://www.pmda.go.jp/files/000208194.pdf. Accessed 22 September 2015.
- 24. World Medical Association. Declaration of Helsinki . Recommendations guiding physicians in biomedical research involving human subjects. JAMA 1997; 277: 925–926. [PubMed] [Google Scholar]
- 25. American Diabetes Association Workgroup on Hypoglycemia . Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care 2005; 28: 1245–1249. [DOI] [PubMed] [Google Scholar]
- 26. Seino Y, Rasmussen MF, Nishida T, Kaku K. Efficacy and safety of the once‐daily human GLP‐1 analogue, liraglutide, vs glibenclamide monotherapy in Japanese patients with type 2 diabetes. Curr Med Res Opin 2010; 26: 1013–1022. [DOI] [PubMed] [Google Scholar]
- 27. Emoto M, Terauchi Y, Ozeki A, Oura T, Takeuchi M, Imaoka T. A 1‐year safety study of dulaglutide in Japanese patients with type 2 diabetes on a single oral hypoglycemic agent: an open‐label, nonrandomized, phase 3 trial. Endocrine J 2015; 62: 1101–1114. [DOI] [PubMed] [Google Scholar]
- 28. Russell‐Jones D, Cuddihy RM, Hanefeld M et al. Efficacy and safety of exenatide once weekly versus metformin, pioglitazone, and sitagliptin used as monotherapy in drug‐naïve patients with type 2 diabetes (DURATION‐4): a 26‐week double‐blind study. Diabetes Care 2012; 35: 252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ferdinand KC, White WB, Calhoun DA et al. Effects of the once‐weekly glucagon‐like peptide‐1 receptor agonist dulaglutide on ambulatory blood pressure and heart rate in patients with type 2 diabetes mellitus. Hypertension 2014; 64: 731–737. [DOI] [PubMed] [Google Scholar]
- 30. Kaku K, Rasmussen MF, Clauson P, Seino Y. Improved glycaemic control with minimal hypoglycaemia and no weight change with the once‐daily human glucagon‐like peptide‐1 analogue liraglutide as add‐on to sulphonylurea in Japanese patients with type 2 diabetes. Diabetes Obes Metab 2010; 12: 341–347. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Updated homoeostasis model assessment changes from baseline at week 52 (LOCF).
Table S1. Summary of least squares (±standard error) mean changes from baseline in self‐monitored blood glucose (mmol/l) values (LOCF at week 52).
Table S2. Summary of serious adverse events by preferred term and treatment for the treatment period from baseline to 52 weeks.
Table S3. Summary and analysis of renal analytes: median baseline values and median changes from baseline to 52 weeks (LOCF).
Table S4. Summary and analysis of lipid profiles: median baseline values and median absolute and percent changes from baseline to 52 weeks (LOCF).


