Abstract
The Social ABCs is a parent‐mediated intervention for toddlers with suspected or confirmed autism spectrum disorder (ASD). We undertook a multi‐site pilot study to evaluate feasibility and acceptability, and to identify trends in child and parent behavior to inform future research using a larger sample and a rigorous research design. The program involved 12 weeks of parent coaching, followed by 12 weeks' implementation, and 3‐month follow‐up assessment for 20 parent‐toddler dyads (age range: 12–32 months). Parents successfully learned the techniques and rated the intervention as highly acceptable. Paired samples t‐tests revealed significant gains in children's functional communication (responsivity, initiations), and language gains (age‐equivalents on standardized measures) commensurate with typical developmental rates. Significant increases in shared smiling and social orienting also emerged, but were attenuated at follow‐up. Parents' fidelity was positively associated with child responsivity. Training parents as mediators is a feasible and highly acceptable approach that provides a potentially cost‐effective opportunity for intensive intervention at a very young age at the first signs of ASD risk. Child and parent gains in several key variables demonstrate the promise of this intervention. Autism Res 2016, 9: 899–912. © 2015 The Authors Autism Research published by Wiley Periodicals, Inc. on behalf of International Society for Autism Research
Keywords: autism spectrum disorder, toddlers, high‐risk, early intervention, parent‐mediated, caregiver‐mediated, pivotal response treatment, communication, smiling
As prevalence estimates increase and early identification efforts improve, the need for feasible, cost‐effective interventions for infants and toddlers with autism spectrum disorder (ASD) has become critical. ASD is a neurodevelopmental disorder characterized by impaired social‐communication and restricted repetitive interests and patterns of behavior [American Psychiatric Association, 2013], with recent prevalence estimates >1% [i.e., 1/68; Centers for Disease Control and Prevention, 2014]. The past decade has yielded substantial advances in earlier detection, often within the first two years of life, particularly in high‐risk samples [e.g., younger siblings of children with ASD; see Jones, Gliga, Bedford, Charman, & Johnson, 2014, for a review]. Converging evidence on the nature and timing of the emergence of ASD has informed the development of novel intervention approaches that are sensitive to both the earliest manifestations of ASD and the developmental needs of infants and toddlers. Evidence continues to support the efficacy of interventions based on applied behavior analytic (ABA) principles, typically with intensive therapist‐delivered programming. Despite compelling evidence of efficacy, resource requirements may limit uptake in many regions and thus the need remains for less resource‐intensive interventions. This is particularly relevant when policy makers may be willing to provide resources for directed intervention in the face of risk for ASD (e.g., familial risk, emerging “red flags”), rather than waiting for confirmed diagnoses.
The most prominent comprehensive intervention models in use and under investigation for toddlers with ASD favor a naturalistic approach that is both behaviorally and developmentally informed (i.e., “Naturalistic, Developmental, Behavioral Interventions;” NDBIs; Schreibman et al., 2015), and a recent emphasis has been placed on adapting programs specifically for use with infants and toddlers. Pivotal Response Treatment [PRT; Koegel & Koegel, 2006], an established naturalistic ABA‐based intervention, stands out as particularly appealing for this younger age group, given its emphasis on naturally occurring, child‐focused, play‐based interactions. The strategies and principles that form the basis of PRT have been applied to a variety of service delivery models, with evidence of improved child responding, generalization, and increased positive affect [Mohammadzaheri, Koegel, Rezaee, & Rafiee, 2014; Ventola et al., 2014], as well as collateral effects on nontargeted skills [Koegel, Carter, & Koegel, 2003; Smith et al., 2010; Smith, Flanagan, Garon, & Bryson 2015; Koegel, Singh, Koegel, Hollingsworth, & Bradshaw, 2014], and increased self‐initiated (vs. prompt‐dependent) behavior [e.g., Koegel & Koegel, 2006]. Evidence of efficacy comes from relatively comprehensive programs [e.g., Smith et al., 2010] and briefer models [e.g., 3–4 months in duration; Mohammadzaheri et al., 2014; Ventola et al., 2014]. PRT techniques have shown promise when applied to infants and toddlers using lower‐intensity approaches to directly target the core social impairments in ASD [e.g., Koegel, Vernon, & Koegel, 2009; Steiner, Genoux, Klin, & Chawarska, 2013; Koegel et al., 2014].
Strong evidence to support the efficacy of intervention in toddlers with ASD has come from the early start Denver model [ESDM; Dawson, Rogers, Munson, & Smith, 2010], an intensive (20 hr/week), comprehensive, ABA‐based intervention specifically adapted for use with toddlers. ESDM incorporates a developmentally sequenced curriculum into a play‐based model, integrated with PRT techniques. A randomized control trial (RCT) yielded significant improvements in IQ, adaptive behavior, and autistic symptoms following two years of this intervention in 18‐ to 30‐month olds with ASD [Dawson et al., 2010]. Findings highlight the potential for significant developmental gains in toddlers with ASD, but the resource‐intensity of such programs may limit widespread community uptake. In the infant and toddler age group, a potentially feasible and cost‐effective approach is to train parents to provide the intervention. Primary caregivers can be trained in the use of development‐enhancing strategies that can be applied at a high intensity throughout the child's typical daily routines [Kasari, Gulsrud, Wong, Kwon, & Locke, 2010]. As with many evidence‐based interventions for ASD, parent training is an integral component of PRT [Koegel & Koegel, 2006]. A solid body of evidence supports the feasibility and effectiveness of parent training as part of a comprehensive preschool program, with evidence of positive changes in child behavior, parental affect, and parent‐child interactions [e.g., Koegel, Bimbela, & Schreibman, 1996; Openden, 2005]. In standard PRT programs, parents participate in 25 hr of one‐to‐one training, although preliminary evidence demonstrates the effectiveness of even briefer training models [Koegel & Koegel, 2006; Coolican, Smith, & Bryson, 2010; Minjarez, Williams, Mercier, & Hardan, 2011].
Parent‐mediated interventions for infants and toddlers with ASD have gained traction over the past several years, with mixed, but promising results [Beaudoin, Sébire & Couture, 2014]. An initial evaluation of a parent‐mediated adaptation of ESDM [Vismara, Colombi, & Rogers, 2009] demonstrated early promise. However, an RCT of a 12‐week parent‐mediated ESDM program, for toddlers aged 14–24 months, yielded less positive findings [Rogers et al., 2012]. Specifically, the ESDM‐parent group demonstrated no advantage over a “treatment as usual” community intervention group in terms of parent skill acquisition or child outcomes. More recently, a pilot study evaluating Infant Start, a parent‐delivered adaptation of ESDM for younger infants, has reported reduced ASD‐related symptoms in seven symptomatic infants (aged 7–15 months) following intervention [Rogers et al., 2014]. These findings demonstrate the potential impact of parent‐mediated intervention even for very young babies with emerging ASD, but further evidence is needed. Of particular relevance is whether very early intervention can successfully target core ASD impairments such as social engagement and shared positive affect [e.g., Landa, Holman, O'Neill, & Stuart, 2011].
Several recent RCTs have examined the effectiveness of different parent‐mediated NDBIs for toddlers with confirmed ASD [Kasari et al., 2010; Carter et al., 2011; Schertz, Odom, Baggett, & Sideris, 2013; Wetherby et al., 2014], or for those at risk for ASD, either based on measured risk markers obtained from population screening [Baranek et al., 2015] or sibling status alone [Green et al., 2015]. These studies have provided evidence of improvements in various indices of social development [i.e., response to joint attention, joint engagement, focusing on faces, attentiveness to parent; Kasari et al., 2010; Schertz et al., 2013; Green et al., 2015; Wetherby et al., 2014], gains in parenting responsiveness [Carter et al., 2011; Baranek et al., 2015; Green et al., 2015], and improvements in child communication abilities [Carter et al., 2011; moderated by object interest at baseline; Wetherby et al., 2014] and particularly in receptive language [Baranek et al., 2015; Wetherby et al., 2014].
Thus, evidence is converging to support the efficacy of NDBIs adapted for use with infants and toddlers, and parent‐mediated models hold promise. To date, parent‐mediated models with varying intensities (i.e., from 16 to 96 visits/family, ranging from 4 to 12 months in duration) have demonstrated efficacy in improving child social orienting/attention, play, and receptive language, and for supporting parenting responsiveness. However, positive trials are not universal [e.g., see Rogers et al., 2012] and relatively less success has been demonstrated in terms of improving expressive communication skills and emotional responsivity, arguably core features of ASD, and thus key intervention targets in this age group [Brian, Bryson, & Zwaigenbaum, 2015].
In response to the growing need for evidence‐based, feasible, and sustainable interventions for toddlers with emerging ASD, we developed the Social ABCs. This is a caregiver‐mediated, ABA‐based intervention, with adaptations to address the developmental needs of infants and toddlers (e.g., strategies to promote emotion regulation in infants). Sensitive to these developmental needs, together with an appreciation of the natural social context of infants and toddlers, and the need for cost‐effective models, the Social ABCs involves training a primary caregiver in the home. The Social ABCs [described in Siller et al., 2014] is a live parent‐coaching model that incorporates the principles and procedures of both parent responsiveness training [Landry, Smith & Swank, 2006] and ABA, as represented by PRT [Koegel, et al., 1999], with modifications for infants and toddlers. This is a manualized intervention that primarily targets two early developmental domains argued to play a central and reciprocal role in the emergence of ASD: early functional verbal communication and positive affect sharing [see Brian et al., 2015]. By focusing on these two core domains, we aim to strike a balance between promoting meaningful developmental progress while maximizing feasibility and portability of the intervention. We focus on functional (verbal) communication as this is among the defining deficits in ASD. Moreover, language development has been identified by parents as a key area of concern [Coonrod & Stone, 2004], particularly in the first 2 years of life, and language ability is a strong predictor of later outcomes. Our focus on positive affect sharing was motivated by its important role in the development of reciprocal relationships with caregivers during infancy, combined with evidence of deficits or even declining trajectories beginning in the first year of life in high‐risk infants later diagnosed with ASD [e.g., Zwaigenbaum et al., 2005; Bryson et al., 2007; Ozonoff et al., 2010; Landa, Gross, Stuart, & Faherty, 2013]. Also, smiling together with a primary caregiver very early in life is thought to lay the groundwork for the development of emotional connectedness (or intersubjectivity) involved in understanding others, which is impaired in ASD [Hobson & Meyer, 2005; Gallese, 2006; Mundy, Gwaltney & Henderson, 2010; Brian et al., 2015]. Moreover, learning is facilitated by positive emotion [e.g., Hohenberger, 2011], suggesting that positive affect sharing may play a facilitating role in the development of other skills (e.g., functional communication), and may thus be a pivotal element of intervention.
Our objective was to evaluate feasibility and acceptability of the Social ABCs and to explore the promise of this intervention by examining change, post‐training and at 3‐month follow‐up, in child functional vocal communication and shared positive affect, and the possible collateral effects on child social orienting. We also examined the relationship between fidelity of implementation and child gains. These findings will inform future research using a larger sample in a controlled clinical trial.
Methods
Participants
Table 1 outlines the key participant characteristics. The primary caregivers of 20 toddlers with suspected or confirmed ASD were enrolled (mean age of toddlers at intake: 22 months; range: 12–32 months) at one of two Canadian sites: IWK/Dalhousie in Nova Scotia (NS; n = 9) and SickKids/University of Toronto in Ontario (n = 11). Nine cases (3 from NS) were from our large, multisite longitudinal “Infant Siblings Study” [ISS; Zwaigenbaum et al., 2005], and the remaining 11 (6 from NS) were community referrals, seven of whom also had an older sibling with ASD. Participants were eligible by virtue of elevated scores on our key assessment measures (see below), combined with clinician concern regarding ASD. All were born at 36–42 weeks gestation, weighing >2500 g; none had identifiable neurological or genetic disorders, or severe sensory or motor impairments. At entry, 9 had confirmed ASD diagnoses (3 from NS) and 11 (6 from NS) had suspected ASD or significant ASD‐related concerns (with elevated scores on our ASD symptom measures). Diagnoses were all informed by the Autism Diagnostic Observation Schedule [ADOS; Lord, Rutter, DiLavore, & Risi, 1999], Autism Diagnostic Interview‐Revised [ADI‐R; Lord, Rutter, & LeCouteur, 1994], and clinical impression of diagnosticians with extensive ASD experience. At exit, 18 cases (9 from NS) had confirmed ASD; none of the confirmed cases at intake lost their diagnosis. See Table 1 for details about parents’ ethnicity and educational attainment.
Table 1.
Toddler and Parent Characteristics at Baseline
| Mean (SD) toddler age in months | 22.05 (5.12) |
| Range: 12–32 | |
| Toddler age group (frequency) | <18 months: 2 |
| 18–23 months: 9 | |
| 24–30 months: 8 | |
| >30 months: 1 | |
| Toddler sex (n Males: n Females) | 14:6 |
| Site (n Toronto: n Halifax) | 11:9 |
| Ethnicity | Caucasian: 15 |
| East Indian: 3 | |
| Asian: 2 | |
| Highest level of maternal education (n = 17) | High school: 2 |
| Partial university: 2 | |
| Completed college or | |
| university: 12 | |
| Graduate school: 1 | |
| AOSI Total scores (n = 2) | 13, 8 |
| Mean (SD) ADOS‐2 comparison metric | 5.89 (2.59) |
| Mean (SD) ADOS‐2 Social Affect (SA) score (n = 18) | 10.50 (4.76) |
| Mean (SD) ADOS‐2 Restricted/Repetitive Behavior (RRB) score (n = 18) | 4.83 (1.95) |
| Mean (SD) ADOS‐2 Total Score (SA + RRB) (n = 18) | 15.33 (6.00) |
| Mean (SD) Mullen Scales of Early Learning‐Early Learning Composite Standard Score (n = 18) | 85.61 (25.88)Range: 49–139 |
Note. ADOS‐2 comparison metric and domain scores were derived from ADOS (WPS edition; Lord et al., 1999). Total score diagnostic cut‐offs for ADOS module 1 (no words) are: ASD = 11, Autism = 16; Module 1 (some words): ASD = 8, Autism = 12; Module 2 (under 5 years): ASD = 7, Autism = 10.
Procedure
Intervention
Participants received our Social ABCs parent training by one of four trained parent coaches who were initially trained by PRT‐reliable trainers, and authors SB and JB. All parent coaches achieved fidelity in implementation of and parent coaching in our intervention model. Parent coaches attended a week‐long training workshop that included working directly with toddlers with red flags for ASD or related developmental concerns, followed by one‐on‐one work with at least three families to practice the intervention strategies. Direct work was video‐recorded and reviewed by trained senior staff. Fidelity of implementation was measured for coaches in the same way as for parents (described below). Parent coaching skills were modeled and practiced during a pre‐pilot phase, with regular video review from the team (including SB and JB) until parent coaching fidelity was achieved. The intervention included 12 weeks of in‐home didactic training sessions combined with in vivo parent coaching with a focus on positive reinforcement of accurate use of intervention techniques (8 weeks of “Active Training”, followed by 4 weeks of “Consultation and Refresher”). This was followed by 12 weeks of parent implementation with no additional help from trainers. Each home visit was 1 to 1.5 hours in length, tapering from 3 visits in week 1, to 2 visits in week 2, and then once weekly through to week 8. Weeks 9 and 11 included telephone or email contact as needed, with refresher and consultation sessions in weeks 10 and 12. Didactic sessions were based on our manual's eight modules (The ABCs of Learning, Enhancing Communication, Sharing Positive Emotion, Motivation and Arousal, Play and The Social ABCs, Daily Care‐giving Activities, Managing Behavioral Challenges, and Taking Care of Yourself), and took place for the first 20–30 min of each home visit; resulting in approximately 13 coaching hours per family. Although designed as a 6‐month intervention, actual duration varied slightly due to illnesses and competing demands, for a mean duration of 8.7 months (SD = 1.79). Specific dosage of the intervention (to toddlers) was not measured, because the objective is to learn techniques that can be integrated into the family's daily routines (vs. a set number of hours per day set aside for “intervention”).
Standardized assessments
Standardized assessments were conducted at two time‐points: (1) Intake (Mean = 0.85 month [SD = 1.27] prior to collection of baseline video data), and (2) Follow‐up (Mean = 8.7 months [SD = 1.87] after intake), following active training plus three months of parent implementation without coaching. Assessments were conducted using standardized administration and scoring procedures, by trained clinical‐research staff with research‐level reliability on relevant measures. All evaluations at one site, and 50% at the other site were conducted by examiners who were not involved in the intervention in any way and were blind to intervention status. Cross‐site differences in children's performance on standardized measures were examined statistically to ensure that there was no systematic bias at the site with only 50% independent examiners.
Video data collection and coding
Continuous 10‐minute video clips of parent‐child interactions were taken at three key times: Baseline (BL), post‐training (PT), and follow‐up (F‐up), with three clips collected at each (on different days) to obtain representative behavior samples. Parents were instructed to play with their children as usual, but were told that we wanted to see how they communicate. For each time point, two clips were selected by a blinded coder based on visibility and maximal codable time recorded; mean scores were calculated for each behavior per time point. These data were subjected to the analyses outlined below. All coaching was withheld during data acquisition. For each video‐coded variable, 20% of video segments were coded by a second rater, also blind to study phase, for inter‐rater reliability.
Measures and Coding Scheme
Standardized measures
Standardized assessments were conducted at intake and follow‐up using well‐established measures for this age group, as follows:
The Autism Observation Scale for Infants [AOSI; Bryson, Zwaigenbaum, McDermott, Rombough, & Brian, 2008] is a 15–20 minute semistructured direct observational measure, with good psychometric properties, that identifies early behavioral markers of ASD in infants/toddlers aged 6–18 months. We used a total score cut‐off of ≥7 to identify risk based on evidence of good positive (0.75) and negative predictive value (0.98–0.99) in earlier work [see Bryson & Zwaigenbaum, 2014] for infants in this age group. The AOSI was conducted by research‐reliable staff to capture ASD symptoms at baseline only for participants in the appropriate age range.
The ADOS [WPS edition; Lord et al., 1999] is a standardized, semistructured direct observational measure of communication, social interaction, play, and behavior, with excellent inter‐rater reliability and high stability when used beyond age 2 years [Lord & Schopler, 1989]. Module 1 was mainly used, except for one participant at intake and three at follow‐up who were assessed using Module 2 (all conducted by research‐reliable administrators with supervision by a registered psychologist). To compare scores within and across modules, scores were converted to revised algorithms and the comparison metric was used [ADOS‐2; Lord et al., 2012. Although primarily used to identify ASD symptoms at intake, the ADOS also served as a possible indicator of change at follow‐up.
The Mullen Scales of Early Learning [MSEL; Mullen, 1995] is a standardized direct assessment of five developmental domains for ages 0–68 months: Gross Motor, Fine Motor, Visual Reception, Receptive Language and Expressive Language. The Early Learning Composite (ELC) is a standard score (mean = 100, SD = 15) representing an overall measure of cognitive ability. Domain scores are represented as T‐scores (mean = 50, SD = 10), and age equivalents (AE) are derived from raw scores. The MSEL has good‐to‐adequate psychometric properties. Given our focus on language outcomes, we used the MSEL Receptive and Expressive Language domain scores as outcome measures.
Video‐coded variables
Our primary outcomes of interest were the video‐coded variables. Videos were coded, by a coder blind to study objectives and study time point, in three domains: Communication, Shared Positive Affect, and Social Orienting/Engagement [see Coolican et al., 2010, for detailed operational definitions]. Communication indices were: (1) Language Opportunities provided by caregiver, and four child behaviors; (2) Responsivity; (3) Inappropriate Responses; (4) Initiations; and (5) Functional Vocal Utterances (FVU); see Table 2. All videos were coded for 10 min, except one 9‐min, 46‐sec clip at F‐up. To account for this slight variability, frequencies are reported as behaviors/min (i.e., rate). Shared Positive Affect involved partial interval coding, with each 10‐sec segment coded for presence or absence of: (1) Child smiling at caregiver; (2) Child smiling at toy/activity; (3) Caregiver smiling at child; and (4) Caregiver smiling at toy/activity (very rare so not analyzed); (5) Child and Parent smiling together (i.e., with smiles directed at one another). Social Orienting/Engagement, defined as the child looking toward the caregiver, also used partial interval coding (10‐sec intervals, presence/absence).
Table 2.
Coding Definitions for Video‐Coded Language Variables
| Language opportunities | Number of language opportunities provided by the parent, including direct prompt (i.e., a verbal model), indirect prompt (i.e., “ready, set…”), or time delay (parent holds up the object of interest and waits expectantly for a vocal response). Reported as rate/minute. |
| Responsivity | Proportion of appropriate child vocal responses, following a parental prompt (reported as %; see Inappropriate Responses for exclusionary examples). |
| Inappropriate responses | Proportion of child nonfunctional, noncommunicative, echolalic, out of context, inappropriate, undirected, or disruptive responses to parent prompts. |
| Initiations | Number of child‐initiated functional, appropriate vocalizations (rate/min). |
| Functional vocal utterances (FVU) | Composite measure of the overall number of functional/meaningful, task‐directed, and purposeful vocalizations with appropriate volume and directedness to person or activity (including both initiations and appropriate vocal responses). Reported as rate/minute. |
Fidelity of implementation
Following Koegel and Koegel [2006], parent fidelity was coded from video, using continuous interval coding (ten 1‐min intervals). Each interval was coded as correct or incorrect/not used for each of ten PRT antecedent techniques or responses to child vocal behavior: child choice, child attending (to person or activity/object), shared control, clear opportunity, pace, recast, contingent reinforcement, natural reinforcement, reinforcement of attempts, and positive emotion [see Koegel & Koegel, 2006, for descriptions of these PRT strategies]. The fidelity of implementation score was the average percentage of intervals, across all ten strategies, during which parents demonstrated appropriate use of the techniques.
Parent satisfaction
As a partial index of social validity of this program, we developed a 7‐item questionnaire to assess the acceptability of the intervention, framed in terms of “helpfulness.” Questions were rated on a 5‐point Likert scale (1: “not at all helpful” to 5: “extremely helpful”). Because we designed this questionnaire part‐way through the study, it was only offered to the last 11 participants.
Analyses
Changes across time‐points were examined via paired samples t‐tests. For video‐coded behaviors, we separately compared BL vs. PT (time‐span 1), PT vs. F‐up (time‐span 2), and BL vs. F‐up (time‐span 3), with family‐wise correction for multiple comparisons (0.05/3 = 0.0167). Effect Sizes (ES) were calculated using Cohen's d. To examine associations among variables and changes on video‐coded variables (i.e., 8 variables across 2 time‐points), as well as possible baseline characteristics that predicted change, critical P was adjusted more stringently using family‐wise error correction (0.05/16 = 0.0031).
Results
Participant Characteristics and Performance Across Study Sites
Table 1 presents information on participant characteristics and performance on ADOS/AOSI and MSEL at intake. Fisher's exact tests revealed no significant associations between study site and sex, ethnicity, maternal education, or referral source (P's > 0.32). No between‐site differences were found for mean age, ADOS comparison metric, or MSEL T‐scores or Age Equivalents at intake (all P's > 0.13) or follow‐up (all P's > 0.18), or for video‐coded variables at BL (P's > 0.28), PT (P's > 0.42), or F‐up (P's > 0.18).
Language and Communication
Standardized measures
Significant gains were observed in age‐equivalent scores on both Receptive and Expressive Language domains of the MSEL, both with large effect sizes (see Table 3). An average gain of 6–8 months’ equivalent emerged between assessments. Standard scores did not differ across time for Receptive, P = 1.0, or Expressive Language, P = 0.28, nor did the ADOS comparison metric.
Table 3.
Performance on Standardized Measures of Language and Social Communication at Baseline and Follow‐up
| Measure | Intake/Baseline | Follow‐Up | P value (Effect Size) |
|---|---|---|---|
| MSEL–RL: mean age equivalent, months (SD) | 18.07 (8.78) | 24.67 (10.20) | 0.003 (0.93) |
| MSEL–EL: mean age equivalent, months (SD) | 17.94 (9.10) | 25.50 (11.51) | <0.001 (1.22) |
| MSEL–RL: mean T‐score (SD) | 40.59 (17.39) | 40.59 (15.24) | 1.0 (0.00) |
| MSEL–EL: mean T‐score (SD) | 41.11 (18.25) | 43.78 (16.82) | .28 (.26) |
| ADOS‐2 comparison metric Mean (SD) | 6.18 (2.35) | 6.12 (1.61) | 0.90 (0.03) |
Notes. MSEL: Mullen Scales of Early Learning; RL: Receptive Language domain; EL: Expressive Language domain; ADOS‐2 comparison metric calculated from ADOS‐2 algorithm scores for Social Affect and RRB (Lord et al., 2012).
Video‐coded variables
Intraclass correlations for language indices ranged from 0.940 to 0.964 (mean = 0.955). Statistically significant gains emerged across time‐span 1, that were maintained at follow‐up (time‐span 3), for: Responsivity, Initiations, FVU, and caregiver‐provided Language Opportunities (see Fig. 1), all P's < 0.002, with medium‐to‐large effect sizes (ES, range: 0.72 to 1.26; see Table 4). Changes over time‐span 2 were all non‐significant (P's > 0.25), demonstrating maintenance of gains, but no further increases, after the intensive training period.
Figure 1.
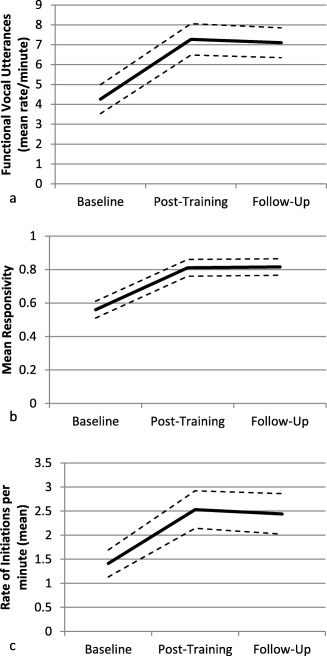
Children's communication gains on video‐coded measures of (a) functional vocal utterances (b) responsivity, and (c) initiations.
Table 4.
Performance on Video‐Coded Indices of Language, Affect, and Social Orienting at Baseline, Post‐Training, and Follow‐Up
| Variable Mean (SD) | Baseline (BL) | Post‐Training (PT) | Follow‐Up (F‐up) | P Value BL vs. PT (Effect Size) | P Value BL vs. F‐up (Effect Size) |
|---|---|---|---|---|---|
| Responsivity (%) | 56.80 (0.24) | 80.90 (0.24) | 81.15 (0.22) | <0.001a (1.26) | <0.001a (1.57) |
| Initiations (rate/min) | 1.41 (1.28) | 2.53 (1.75) | 2.44 (1.88) | 0.003a (0.77) | 0.002a (0.78) |
| Functional vocal utterances (rate/min) | 4.26 (3.29) | 7.27 (3.58) | 7.10 (3.36) | 0.001a (0.93) | <0.001a (1.16) |
| Language opportunities (rate/min) | 6.34 (3.16) | 8.36 (3.14) | 8.21 (2.99) | 0.005a (0.72) | 0.001a (0.88) |
| Child smiling to caregiver (% intervals) | 24.70 (17.08) | 32.85 (19.01) | 30.05 (14.43) | .048 (0.47) | 0.21 (0.29) |
| Child smiling to object/activity (% intervals) | 11.74 (7.41) | 7.10 (6.48) | 8.00 (4.99) | 0.013 (0.63) | 0.06 (0.46) |
| Caregiver smiling (% intervals) | 44.10 (16.43) | 50.65 (19.56) | 46.65 (18.64) | 0.068 (0.43) | 0.42 (0.18) |
| Shared smiling (% intervals) | 15.70(11.09) | 22.65 (14.33) | 20.90 (11.38) | 0.013a (0.61) | 0.11 (0.38) |
| Social orienting (% intervals) | 27.00 (14.04) | 36.55 (16.61) | 34.45 (18.21) | 0.009a (0.64) | 0.16 (0.33) |
Indicates statistically significant difference with corrected P = 0.05/3 = 0.0167.
Shared Positive Affect (Smiling) and Social Orienting
Smiling
Inter‐rater agreement was high for smiling (mean agreement = 87%; range: 65–95%). In time‐span 1, a trend emerged toward gains in Child Smiling to their caregiver (ES = 0.47) but this was nonsignificant with corrected alpha; and a significant decrease emerged in the rate of child smiling to a toy/object/activity (ES = 0.63). A nonsignificant trend toward increased Parent Smiling to their child also emerged during this time‐span (ES = 0.43; see Table 4). Shared Smiling increased significantly during this period (ES = 0.61), but was attenuated at F‐up (no longer different from BL, but with a modest ES = 0.38; see Fig. 2).
Figure 2.
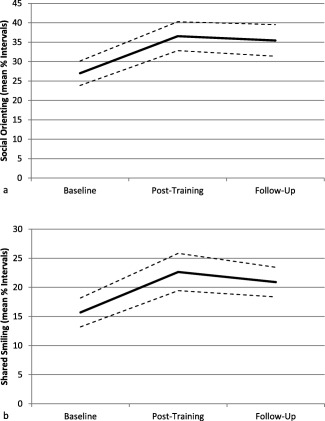
Gains in video‐coded indices of (a) social orienting and (b) shared smiling.
Social orienting
Inter‐rater agreement was also strong for this variable (mean = 85% agreement; range: 68–97%). Statistically significant increases in child orienting toward caregiver emerged in time‐span 1, with a medium effect size (ES = 0.64), but this gain was attenuated at F‐up, and no longer different from BL but with a modest effect size nonetheless (ES = 0.33; see Table 4 and Fig. 2).
Associations Among Variables
To explore possible mediators of treatment response, we examined associations between changes in language and nonlanguage behaviors, as well as between early (i.e., time‐span 1) and later (time‐span 3) changes. We did this by exploring correlations among change in eight variables across these two time‐spans (with corrected P = 0.05/16 = 0.0031): Initiations, Responsivity, Language Opportunities, FVU, Child Smiling, Parent Smiling, Shared Smiling, and Social Orienting. Significant associations emerged between several communication indices (see Table 5) and between Parent and Child Smiling (see Table 6). A moderate association emerged between change in child Social Orienting and change in Parent Smiling across time‐span 3 (r = 0.59; P = 0.007). With the stringent error correction, none of the smiling change data were significantly correlated with changes in communication indices. However, trends indicated possible associations between gains in Child Smiling (time‐span 1) and increased Initiations, FVU, Language Opportunities, as well as improved T‐scores on the MSEL EL domain, P's range = 0.010–0.037 (see Table 7).
Table 5.
Significant Pearson Correlations (r; P values) among Change Scores for Language Variables
| Initiations (Time‐span 3) | FVU (Time‐span 1) | FVU (Time‐span 3) | Language Opportunities (Time‐span 1) | Language Opportunities (Time‐span 3) | ||
|---|---|---|---|---|---|---|
| Initiations | Pearson r | 0.762 | 0.703 | 0.766 | 0.649 | 0.696 |
| (Time‐span 1) | (P) | (<0.001) | (0.001) | (<0.001) | (0.002) | (0.001) |
| Initiations | Pearson r | – | 0.377 | 0.746 | 0.313 | 0.703 |
| (Time‐span 3) | (P) | (0.101) | (<0.001) | (0.179) | (0.001) | |
| FVU | Pearson r | – | – | 0.758 | 0.944 | 0.660 |
| (Time‐span 1) | (P) | (<0.001) | (<0.001) | (0.002) | ||
| FVU | Pearson r | – | – | – | 0.701 | 0.935 |
| (Time‐span 3) | (P) | (0.001) | (<0.001) | |||
| Language opportunities | Pearson r | – | – | – | – | 0.711 |
| (Time‐span 1) | (P) | (<0.001) |
Note. FVU, Functional vocal utterances; Time‐span 1: (Baseline vs. Post‐training); Time‐span 3: (Baseline vs. Follow‐up).
Table 6.
Significant Pearson Correlations (r; P values) amongst Change Scores for Smiling Variables
| Child smile (Time‐span 3) | Parent smile (Time‐span 1) | Parent smile (Time‐span 3) | ||
|---|---|---|---|---|
| Child smile | Pearson r | 0.600 | 0.626 | 0.464 |
| (Time‐span 1) | (P) | (0.005) | (0.003) | (0.039) |
| Child smile | Pearson r | – | 0.506 | 0.688 |
| (Time‐span 3) | (P) | (0.023) | (0.001) | |
| Parent smile | Pearson r | – | – | 0.708 |
| (Time‐span 1) | (P) | (<0.001) |
Table 7.
Nonsignificant Trends (Pearson r, P values) Suggesting Possible Associations between Gains in Child Smiling and Gains in Language Behaviors
| Initiations (Time‐span 1) | Initiations (Time‐span 3) | FVU (Time‐span 3) | Language opportunities (Time‐span 3) | MSEL EL T‐score (intake vs. follow‐up) | ||
|---|---|---|---|---|---|---|
| Child smile | Pearson r | 0.559 | 0.553 | 0.560 | 0.514 | 0.524 |
| (Time‐span 1) | (P) | (0.010) | (0.011) | (0.010) | (0.021) | (0.027) |
Note. FVU, Functional vocal utterances; Time‐span 1: (Baseline vs. Post‐training); Time‐span 3: (Baseline vs. Follow‐up); MSEL: Mullen Scales of Early Learning; EL: Expressive Language.
Baseline language functioning
To explore the role of baseline language level in treatment response, children were divided into “Low” (n = 8) and “High” (n = 11) language groups based on baseline MSEL language T‐scores (i.e., RL or EL T‐score <30 vs. ≥30; ≥2 standard deviations from the standardization mean). Univariate ANOVA revealed two trends that failed to reach significance with the adjusted critical P: specifically, the subgroup with low language scores at baseline made somewhat greater gains in MSEL RL T‐score, F (1,13) = 6.16, P = 0.028; and in Social Orienting (BL vs. F‐Up), F (1,17) = 4.79, P = .043 than the high language group.
Referral source
Given that our sample consisted of both community referrals and participants identified through our ISS, we explored potential group differences on this basis. At baseline, no significant differences emerged, all P's > 0.31. However, significant differences emerged over time‐span 3, favouring ISS participants over community referrals, for both increased rate of Initiations (mean change = 1.99, SD = 1.28 vs. 0.24, SD = 0.57) and FVU (mean change = 4.62, SD = 2.25 vs. 1.40, SD = 1.49), both P's = 0.001.
Feasibility and Acceptability
Parent fidelity of implementation
Inter‐rater reliability for parent fidelity was very strong (mean = 90%; range: 81–100%). Parent fidelity increased significantly from BL (Mean = 52.55%, SD = 10.94) to PT (84.30%, SD = 11.15), and was maintained at F‐up (80.20%, SD = 9.69); t's = −10.47 and −11.95, respectively, both P's < 0.001. At baseline, none of the caregivers reached 75% fidelity; at PT, 18/20 had attained this level, and 16 retained this level at F‐up. Fidelity of implementation at PT was significantly associated with change in children's Responsivity from BL to F‐up, r = 0.58, P = 0.007.
Parent satisfaction
The intervention received extremely positive satisfaction ratings from parents (n = 11; mean = 29.82, SD = 2.82 out of a possible 35). No differences were found across site or referral source.
Discussion
This study demonstrates the feasibility and acceptability of our novel parent‐mediated Social ABCs intervention for infants/toddlers with ASD, and provides evidence of promise of this intervention's efficacy. Strengths include the use of a manualized program, measurement of fidelity, the use of blinded coders and assessment of inter‐rater reliability, the enrollment of a relatively young group with confirmed or suspected ASD, and the inclusion of outcome variables that are associated with core ASD features. Our most informative indices of change were obtained from video‐coding of parent‐child interactions. Significant gains emerged in children's communication on several proximal video‐coded measures, including responsivity to adult prompts, rate of initiations, and functional vocal utterances, which were maintained three months following parent training. Post‐training gains in responsivity and total functional vocal utterances were characterized by strong effect sizes, and gains in self‐initiated language were medium‐to‐large. Using age‐equivalent scores, we also observed gains on standardized measures of receptive and expressive language commensurate with typical developmental rates. Failure to observe gains in standard scores suggests that our participants did not achieve a rate of gain greater than that expected for typical development, but neither did they lose standing relative to their age peers. These findings stand in contrast to previous reports describing the natural histories of high‐risk infants in this age range when followed longitudinally, in the absence of intervention. For example, declining developmental trajectories have been described (based on Mullen T‐scores) in a sizable proportion of high‐risk babies from 6 to 36 months [Landa, Gross, Stuart, & Bauman, 2012], and specifically in those with ASD outcomes. Landa et al. [2013] also reported declining raw language scores (which would necessitate declining standard scores) in 48% of high‐risk babies with ASD outcomes. Similarly, one‐third of the high‐risk infant siblings with ASD outcomes in our larger sample were characterized by declining developmental trajectories of standard scores, and 20% by actual raw score loss or plateau on the MSEL [Brian et al., 2014]. Given these findings, the current sample would arguably not be expected to demonstrate age‐appropriate developmental gains in language functioning, across the time‐span examined, in the absence of intervention.
We observed significant gains in shared smiling and trends toward increased parent smiling to their children, and children smiling to their parents, accompanied by decreased child smiling at toys/objects, indicating a selective increase in smiling to people. Moreover, increased smiling by one social partner was associated with increased smiling in the other, suggesting a reciprocal relationship. Evidence of the natural history of infants later diagnosed with ASD points to a declining pattern of social smiling beginning between 12 and 18 months of age [Ozonoff et al., 2010; Landa et al., 2013]. Our findings of gains, rather than loss, further support the potential efficacy of our intervention.
A collateral post‐training increase in children's social orienting was also observed, and this was moderately associated with parental smiling. Evidence suggests that changes in social orienting may be among the earliest manifestations of ASD, with evidence of declining trajectories beginning as early as 6 months of age [Ozonoff et al., 2010] in the absence of intervention. Our reported medium‐sized gains in social orienting stand out compared with findings from a similar age group, also over a 12‐week period, regardless of intervention [effect sizes of −0.02 and 0.06 for treatment and community control groups, respectively; Rogers et al., 2012], albeit using a different measure of social orienting. Although it has been postulated that reduced social orienting may be secondary to more basic attentional deficits [see Brian et al., 2015, for an overview], a failure to orient selectively to social stimuli (i.e., faces and the affective expressions they hold) may result in fewer opportunities to learn from faces and make sense of the information they can provide. Increased social orienting affords the opportunity for increased affect sharing, and both are known to enhance learning [Kasari, Sigman, Mundy, & Yirmiya, 1990; Messinger, Fogel, & Dickson, 2001; Hohenberger, 2011]. Moreover, our findings suggest a reciprocal relation between child orienting and parent smiling, which highlights the important interaction between child and caregiver, discussed in more detail below.
Unfortunately, increases in both shared smiling and social orienting were not consistently maintained at follow‐up, revealing the possible vulnerability of these gains once coaching ended. In reviewing our intervention strategies, it became clear that we placed greater emphasis on language development (vs. affect sharing and social orienting) in our formal teaching strategies, and these skills were maintained once coaching ended. Social orienting and smiling increased initially but were perhaps less well‐established during the training phase, rendering gains in these behaviors more vulnerable to extinction. However, we note that a consistent pattern has emerged for all video‐coded indices wherein the greatest rate of gain appears to occur during the coaching phase, with leveling out during implementation. It remains possible that, with a larger sample, the apparent non‐significant gains for some variables across Time‐Span 3 would become significant. Moreover, these data may point to the need to enhance the coaching phase in some way to ensure retention of gains once coaching ceases. As we refine our model, considerations include whether we need to place a greater emphasis on shared affect and perhaps target social orienting more directly. Alternatively, it remains an empirical question whether infants may have reached a natural “ceiling” in the rate of these behaviors, in which case, a postcoaching plateau would be an acceptable outcome.
We also identified a positive association between child‐initiated vocalizations and adult‐provided language opportunities. Although we cannot determine causality, this may suggest the importance of establishing the contextually appropriate use of language in the development of functional, self‐initiated language. We were encouraged that increased adult prompting did not result in prompt‐dependency in our program, which has been a perennial challenge in more highly structured ABA‐based models [e.g., Smith, 2001], and may have been mitigated by our use of naturalistic, motivation‐based, PRT procedures [cf. Koegel & Koegel, 2006].
Although preliminary, we observed differential response to treatment based on referral source (ISS vs. community). Specifically, we observed an advantage for children referred through our longitudinal study of high‐risk infant siblings relative to community referrals, despite virtually identical fidelity in the two parent groups, both post‐training and at follow‐up. This finding is preliminary due to small subgroups, but warrants further examination in larger samples. One possibility is that the families enrolled in the ISS may be a somewhat unique group in ways not captured by our data (e.g., motivation/resources to enrol in research well before detection of developmental concerns).
Although not statistically significant, a trend was observed toward greater improvement in receptive language and social orienting for participants with lower baseline language functioning. This may be explained, in part, by “ceiling” effects for the high language group (borne out by initial receptive language T‐scores within average limits). Not to be overlooked, however, is that the subgroup with lower baseline language gained almost a full standard deviation. Although not statistically significant, this meets Jacobson and Truax's [1991] definition of clinically significant change (i.e., scores moving from below, to within, two standard deviations of the population mean). This subgroup also made somewhat greater gains in social orienting, almost doubling their baseline rate. These preliminary findings raise the possibility of an association between improved social orienting and improved receptive language, an interpretation that underscores the importance of social orienting as a potentially pivotal intervention target for this age group. Because these patterns are only nonsignificant trends, we will further consider these apparent differences in future work with larger samples.
Parent gains and associated child gains
Parents provided significantly more language opportunities after training, and showed modest, but nonsignificant increases in smiling at their children. Perhaps more importantly, however, some intriguing associations between caregiver smiling and several important child‐related indices emerged. First, changes in parent smiling were associated with changes in child smiling, which was not directly targeted in our intervention, thus supporting our premise that changes in parent behavior may result in changes in child behavior, even if not targeted directly. The potential to increase positive affect in our participants is encouraging in light of evidence of declining positive affect sharing in high‐risk infants with ASD between 12 and 24 months of age [Ozonoff et al., 2010; Landa et al., 2013], reduced smiling in high‐risk infants with ASD more generally [Filliter et al., 2015], and the important role positive affect plays in learning. Further, a moderate association emerged between gains in parent smiling and increased child orienting to the parent. It is of great interest to us that there may be a relation between child orienting and parent smiling, regardless of the direction. Questions to explore further are whether parents smile more because their children are looking at them more (thus appearing more engaged in the interaction), or if the parents’ smiling (directly targeted in our intervention) may have led to increased child orienting (i.e., children may find it more reinforcing to look at a smiling face). These smiling data highlight the importance of targeting sharing of positive affect, which may have a collateral impact on other important conditions for learning (e.g., attending to a social partner). The attainment of any new skill (e.g., communication) will be facilitated by enhanced positive affect and increased engagement [e.g., see Fossum, Williams, & Smith, 2015, wherein higher rates of baseline positive affect predicted better communication outcomes for preschoolers with ASD in a comprehensive early intervention program].
Parents achieved a high degree of fidelity in implementing the Social ABCs strategies following training. Indeed, the vast majority of parents (90%) achieved at least 75% fidelity, a benchmark recommended by Stahmer and Gist [2001], and fidelity was associated with gains in children's responsivity to adult prompts over the entire treatment period, providing support for the claim that our intervention procedures had an impact on the primary child outcome measure.
In addition to positive parent satisfaction ratings, unsolicited feedback from parents revealed very positive responses to the intervention. One parent beautifully captured the essence of the program in the following statement: “The focus on sharing positive emotions reminded me that play is fun. Because I want to play with my child now, I am spending so much more time interacting… I feel like these interactions have had so much to do with his language burst.”
Limitations
Our findings demonstrate that the Social ABCs is a feasible model for parents to learn and deliver, and that parents find it enjoyable. We recognize that our lack of a control group precludes definitive conclusions about the impact of this intervention. However, three key findings provide evidence of promise regarding the efficacy of our program: First, and perhaps most compelling, is that for every video‐coded variable that demonstrated change, this occurred during the intervention coaching phase, and plateaued once the coaching ceased. This suggests that the coaching was responsible for the observed gains, but this will need to be tested in a more rigorous design. Moreover, given the documented delays in our participants at intake, together with previous reports revealing developmental decline in a substantial proportion of high‐risk babies and those with ASD outcomes in particular, the likelihood of achieving age‐appropriate gains in language simply from maturation (as a group) was low. Finally, the significant correlation between fidelity of implementation and gains in our primary (communication) outcome measure strengthens the argument that the intervention contributed to the observed gains. Although fidelity remained high throughout the implementation phase, it may be surprising that this was not associated with continued gains in social smiling and orienting. One possibility, yet to be explored, is that our participants (and their caregivers) may have reached ceiling levels in smiling and orienting so there was no more room to increase. Alternatively, this may also be explained by our relatively greater emphasis on the communication target during parent coaching (recall that many of the communication gains did maintain post‐training). Our measure of parent satisfaction is also limited by the fact that only half the sample completed it. The relatively well‐educated and primarily Caucasian sample may also limit the generalizability to other socio‐cultural groups. Finally, our relatively small sample may have been under‐powered to detect small subgroup differences, though this remains one of the largest studies of parent‐mediated intervention for toddlers with emerging ASD. We observed trends that indicated possible subgroup differences in response to the intervention, which need to be explored systematically in future studies.
Conclusions and Future Directions
Our findings reveal gains in several language and communication indices, shared positive affect, and social orienting for toddlers with confirmed or suspected ASD, over a relatively short time, with parents as mediators. Parents attained a high degree of fidelity relatively quickly and rated the intervention as highly acceptable. Training parents as mediators presents an opportunity for the integration of intervention into daily activities, allowing for intensive very early intervention that is developmentally sensitive, feasible, and cost‐effective. Bolstered by our preliminary evidence of promise, next steps include a RCT to establish efficacy (currently underway), translation to community settings (e.g., front‐line childcare or infant development specialists), as well as efforts to evaluate systematically any participant or family characteristics that predict differential responses to treatment. Finally, we are highly motivated to explore the cost‐effectiveness of this model compared with more intensive, comprehensive interventions for toddlers with ASD.
Acknowledgments
This research was funded by Autism Speaks as part of the Toddler Treatment Network (AS‐TTN). At the time of the study, Dr. Bryson was supported by the Joan and Jack Craig Chair in Autism Research. Dr. Smith is currently supported by the Joan and Jack Craig Chair in Autism Research. Dr. Zwaigenbaum is supported by the Stollery Children's Hospital Foundation Chair in Autism Research and by an Alberta Innovates‐Health Solutions Health Scholar Award. The authors wish to thank the families for their hard work and dedication and for welcoming us into their homes. We are very grateful for our exceptional parent coaches, Terry McCormick, Erin Dowds, and Stacey MacWilliam. We also wish to thank Daniel Openden for engaging us in thoughtful discussions about coaching positive affect. Finally, we thank our video coders, Julie Longard, Sarah Dhooge, Heather Hiscock, and Jessica Soley, as well as Kate Bernardi for her assistance with assessments and data management.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed). Washington, DC: American Psychiatric Association. [Google Scholar]
- Baranek, G. , Watson, L.R. , Turner‐Brown, L. , Field, S.H. , Crais, E.R. , Wakeford, L. , … Reznick, S.J. (2015). Preliminary efficacy of Adapted Responsive Teaching for infants at risk of autism spectrum disorder in a community sample. Autism Research and Treatment. Article ID 386951, doi: dx.doi.org/10.1155/2015/386951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaudoin, A.J. , Sebire, G. , & Couture, M. (2014). Parent training interventions for toddlers with autism spectrum disorder (Review Article). Autism Research and Treatment, Article ID 839890, http://dx.doi.org/10.1155/2014/839890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brian, J.A. , Bryson, S.E. , & Zwaigenbaum, L. (2015). ASD in infancy: Developmental considerations in treatment targets. Current Opinion in Neurology, 28(2), 117–123. [DOI] [PubMed] [Google Scholar]
- Brian, J.A. , Roncadin, C. , Duku, E. , Bryson, S.E. , Smith, I.M. , Roberts, W. , … Zwaigenbaum, L. (2014). Emerging cognitive profiles in high‐risk infants with and without autism spectrum disorder. Research in Autism Spectrum Disorders, 8(11), 1557–1566. [Google Scholar]
- Bryson, S.E. , & Zwaigenbaum, L. (2014). Autism observation scale for infants In Comprehensive Guide to Autism (pp. 299–310). New York, NY: Springer. [Google Scholar]
- Bryson, S.E. , Zwaigenbaum, L. , McDermott, C. , Rombough, V. , & Brian, J. (2008). The autism observation scale for infants: Scale development and reliability data. Journal of Autism and Developmental Disorders, 38(4), 731–738. doi:10.1007/s10803-007-0440-y [DOI] [PubMed] [Google Scholar]
- Bryson, S.E ., Zwaigenbaum, L ., Brian, J ., Roberts, W ., Szatmari, P ., Rombough, V . & McDermott, C . (2007). A prospective case series of high‐risk infants who developed autism. Journal of autism and developmental disorders, 37(1), 12–24. [DOI] [PubMed] [Google Scholar]
- Carter, A.S. , Messinger, D.S. , Stone, W.L. , Celimli, S. , Nahmias, A.S. , & Yoder P. (2011). A randomized controlled trial of Hanen's ‘More Than Words’ in toddlers with early autism symptoms. Journal of Child Psychology and Psychiatry, 52(7), 741–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2014). Prevalence of autism spectrum disorder among children aged 8 years – Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report, Surveillance Summary, 63(2), 1–20. [PubMed]
- Coolican, J. , Smith, I.M. , & Bryson, S. (2010). Brief parent training in pivotal response treatment for preschoolers with autism. Journal of Child Psychology and Psychiatry, 51(12), 1321–1330. [DOI] [PubMed] [Google Scholar]
- Coonrod, E.E ., & Stone, W.L . (2004). Early concerns of parents of children with autistic and nonautistic disorders. Infants & Young Children, 17(3), 258–268. [Google Scholar]
- Dawson, G. , Rogers, S. , Munson, J. , & Smith, M. (2010). Randomized, controlled trial of an intervention for toddlers with autism: Early Start Denver Model. Pediatrics, 125, e17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filliter, J.H. , Longard, J.C.P. , Lawrence, M.A. , Zwaigenbaum, L. , Brian, J. , Garon, N. , & Bryson, S.E. (2015). Positive affect in infant siblings of children diagnosed with autism spectrum disorder. Journal of Abnormal Child Psychology, 43(3), 567–575. [DOI] [PubMed] [Google Scholar]
- Fossum, K.L. , Williams, L. , & Smith, I.M. (2015, May 14). Predicting growth of communication skills of preschoolers with autism spectrum disorder during treatment in a community‐based pivotal response treatment program. In International Meeting for Autism Research, (IMFAR), Salt Lake City, UT.
- Gallese, V. (2006). Intentional attunement: A neurophysiological perspective on social cognition and its disruption in autism. Brain Research, 1079, 15–24. [DOI] [PubMed] [Google Scholar]
- Green, J. , Charman, T. , Pickles, A. , Wan, M.W. , Elsabbagh, M. , Slonims, V. , … Johnson, M.H. (2015). Parent‐mediated intervention versus no intervention for infants at high risk of autism: a parallel, single‐blind, randomised trial. The Lancet Psychiatry, 2(2), 133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobson, R.P. , & Meyer, J.A. (2005). Foundations for self and other: A study in autism. Developmental Science, 8, 481–491. [DOI] [PubMed] [Google Scholar]
- Hohenberger, A. (2011). The role of affect and emotion in language development In Gokcay D. & Yildirim G. (Eds.), Affective computing and interaction: Psychological, cognitive and neuroscientific perspectives (pp. 208–243). Hershey, PA: IGI Global. [Google Scholar]
- Jacobson, N.S. , & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. [DOI] [PubMed] [Google Scholar]
- Jones, E.J.H. , Gliga, T. , Bedford, R. , Charman, T. , & Johnson, M.H. (2014). Developmental pathways to autism: A review of prospective studies of infants at risk. Neuroscience and Biobehavioral Reviews, 39, 1–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari, C. , Gulsrud, A.C. , Wong, C. , Kwon, S. , & Locke, J. (2010). Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. Journal of Autism and Developmental Disorders, 40(9), 1045–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari, C. , Sigman, M. , Mundy, P. , & Yirmiya, N. (1990). Affective sharing in the context of joint attention interactions. Journal of Autism and Developmental Disorders, 20, 87–100. [DOI] [PubMed] [Google Scholar]
- Koegel, L.K. , Carter, C.M. , & Koegel, R.L. (2003). Teaching children with autism self‐initiations as a pivotal response. Topics in Language Disorders, 23(2), 134–145. [Google Scholar]
- Koegel, L.K , Singh, A.K. , Koegel, R.L. , Hollingsworth, J.R. , & Bradshaw, J. (2014). Assessing and improving early social engagement in infants. Journal of Positive Behavior Interventions, 16(2) 69–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel, R.L. , Bimbela, A. , & Schreibman, L. (1996). Collateral effects of parent training on family interactions. Journal of Autism and Developmental Disorders, 26(3), 347–359. [DOI] [PubMed] [Google Scholar]
- Koegel, R.L. , & Koegel, L.K. (2006). Pivotal response treatments for autism: Communication, social, and academic development. Baltimore, MD: Brookes Publishing. [Google Scholar]
- Koegel, R.L. , Vernon, T. , & Koegel, L.K. (2009). Improving social initiations in young children with autism using reinforcers with embedded social interactions. Journal of Autism and Developmental Disorders, 39(9), 1240–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa, R.J. , Gross, A.L. , Stuart, E.A. , & Bauman, M. (2012). Latent class analysis of early developmental trajectory in baby siblings of children with autism. Journal of Child Psychology and Psychiatry, 53, 986–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa, R.J. , Gross, A.L. , Stuart, E.A. , & Faherty, A. (2013). Developmental trajectories in children with and without ASD: The first 3 years. Child Development, 84, 429–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa, R.J. , Holman, K.C. , O'Neill, A.H. , & Stuart, E.A. (2011). Intervention targeting development of socially synchronous engagement in toddlers with ASD: A randomized controlled trial. Journal of Child Psychology and Psychiatry, 52(1), 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landry, S.H. , Smith, K.E. , & Swank, P.R. (2006). Responsive parenting: Establishing early foundations for social, communication, and independent problem‐solving skills. Developmental Psychology, 42(4), 627–642. [DOI] [PubMed] [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P. , & Risi, S. (1999). Autism diagnostic observation schedule: Manual. Los Angeles: Western Psychological Services. [Google Scholar]
- Lord, C. , Rutter, M. , DiLavore, P.C. , Risi, S. , Gotham, K. , & Bishop, S. (2012). Autism diagnostic observation schedule, Second Edition (ADOS‐2) Manual (Part I): Modules 1–4. Torrance, CA: Western Psychological Services. [Google Scholar]
- Lord, C. , Rutter, M. , & LeCouteur, A.J. (1994). Autism diagnostic interview–revised: A revisedversion of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24, 659–685. [DOI] [PubMed] [Google Scholar]
- Lord, C. , & Schopler, E. (1989). Stability of assessment results of autistic and nonautistic language‐impaired children from preschool years to early school age. Journal of Child Psychology and Psychiatry, 30, 575–590. [DOI] [PubMed] [Google Scholar]
- Messinger, D.S. , Fogel, A. , & Dickson, K.L. (2001). All smiles are positive, but some smiles are more positive than others. Developmental Psychology, 37, 642. [PubMed] [Google Scholar]
- Minjarez, M.B. , Williams, S.E. , Mercier, E.M. , & Hardan, A.Y. (2011). Pivotal response group treatment program for parents of children with autism. Journal of Autism and Developmental Disorders, 41(1), 92–101. [DOI] [PubMed] [Google Scholar]
- Mohammadzaheri, F. , Koegel, L.K. , Rezaee, M. , & Rafiee, S.M. (2014, May). A randomized clinical trial comparison between pivotal response treatment (PRT) and structured applied behavior analysis (ABA) intervention for children with autism. Journal of Autism and Developmental Disorders, 44(11), 2769–2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen, E.M. (1995). Mullen scales of early learning. Circle Pines, MN: American Guidance. [Google Scholar]
- Mundy, P. , Gwaltney, M. , & Henderson, H. (2010). Self‐referenced processing, neurodevelopment and joint attention in autism. Autism, 14, 408–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Openden, D.A. (2005). Pivotal response treatment for multiple families with autism: Probable efficacy and effectiveness of a group parent education workshop. Doctoral Thesis, University of California Santa Barbara, CA.
- Ozonoff, S. , Iosif, A.M. , Baguio, F. , Cook, I.C. , Moore, M. , Hutman, T. , … Young, G.S. (2010). A prospective study of the emergence of early behavioral signs of autism. Journal of the American Academy of Child and Adolescent Psychiatry, 49(3), 256–266. [PMC free article] [PubMed] [Google Scholar]
- Rogers, S.J. , Estes, A. , Lord, C. , Vismara, L. , Winter, J. , Fitzpatrick, A. , … Dawson, G. (2012). Effects of a brief Early Start Denver Model (ESDM)–based parent intervention on toddlers at risk for autism spectrum disorders: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 51(10), 1052–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers, S.J. , Vismara, L. , Wagner, A.L. , McCormick, C. , Young, G. , & Ozonoff, S. (2014). Autism treatment in the first year of life: A pilot study of Infant Start, a parent‐implemented intervention for symptomatic infants. Journal of Autism and Developmental Disorders. 44(12), 2981–2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibman, L. , Dawson, G. , Rogers, S.J. , Ingersoll, B. , Kaiser, A.P. , Kasari, C. , … Halladay, A. (2015). Naturalistic developmental behavioral interventions: Empirically validated treatments for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2411–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schertz, H.H. , Odom, S.L. , Baggett, K.M. , & Sideris, J.H. (2013). Effects of Joint Attention Mediated Learning for toddlers with autism spectrum disorders: An initial randomized controlled study. Early Childhood Research Quarterly, 28(2), 249–258. [Google Scholar]
- Siller, M. , Morgan, L. , Turner‐Brown, L. , Baggett, K.M. , Baranek, G. , Brian, J. , … Zwaigenbaum, L. (2014). Designing studies to evaluate parent‐mediated interventions for toddlers with autism spectrum disorder. Journal of Early Intervention, 35, 355–377. [Google Scholar]
- Smith, I.M. , Flanagan, H.E. , Garon, N. , & Bryson, S.E. (2015). Effectiveness of community‐based early intervention based on Pivotal Response Treatment. Journal of Autism and Developmental Disorders, 45, 1858–1872. [DOI] [PubMed] [Google Scholar]
- Smith, I.M. , Koegel, R.L. , Koegel, L.K. , Openden, D.A. , Fossum, K.L. , & Bryson, S.E. (2010). Effectiveness of a novel community‐based early intervention model for children with autistic spectrum disorder. American Journal on Intellectual and Developmental Disabilities, 115(6), 504–523. [DOI] [PubMed] [Google Scholar]
- Smith, T. (2001). Discrete trial training in the treatment of autism. Focus on Autism and Other Developmental Disabilities, 16(2), 86–92. [Google Scholar]
- Stahmer, A.C. & Gist, K. (2001). The effects of an accelerated parent education program on technique mastery and child outcome. Journal of Positive Behavior Interventions, 3(2), 75–82. [Google Scholar]
- Steiner, A.M. , Gengoux, G.W. , Klin, A. , & Chawarska, K. (2013). Pivotal response treatment for infants at‐risk for autism spectrum disorders: A pilot study. Journal of Autism and Developmental Disorders, 43, 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventola, P.E. , Friedman, H.E. , Anderson, L.C. , Wolf, J.M. , Oosting, D. , Foss‐Feig, J. , … Pelphrey, K.A. (2014). Improvements in social and adaptive functioning following short‐duration PRT program: A clinical replication. Journal of Autism and Developmental Disorders, 44(11), 2862–2870. [DOI] [PubMed] [Google Scholar]
- Vismara, L.A. , Colombi, C. , & Rogers, S.J. (2009). Can one hour per week of therapy lead to lasting changes in young children with autism? Autism, 13, 93–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherby, A.M. , Guthrie, W. , Woods, J. , Schatschneider, C. , Holland, R.D. , Morgan, L. , & Lord, C. (2014). Parent‐implemented social intervention for toddlers with autism: An RCT. Pediatrics, 134, 1084–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwaigenbaum, L. , Bryson, S.E. , Rogers, T. , Roberts, W. , Brain J., & Szatmari, P. (2005). Behavioural manifestations of autism in the first year of life. International Journal of Developmental Neuroscience, 23, 143–152. [DOI] [PubMed] [Google Scholar]


