Abstract
Objective
To assess the recording status of weight management measures among adults presenting to general practices within regional catchments.
Design
Cross‐sectional; secondary data analysis.
Setting
Primary health care – 17 general practices located in the Illawarra Shoalhaven region of regional New South Wales.
Participants
A subset of the Sentinel Practices Data Sourcing project database (n = 118 709 adults) that included information on demographic indicators, chronic disease status, and obesity and overweight‐specific measurement indicators recorded from September 2011 to September 2013.
Main outcome measures
Proportions of coded recording of quantitative measures of overweight and obesity – body mass index (BMI) and waist circumference, and likelihood of BMI recording (odds ratios (ORs)) by various clinical diagnosis and counts of recorded conditions.
Results
Of the patients, 30.9% had a BMI recorded and only 8.0% had a waist circumference recorded in their electronic medical records. There were variations in BMI recording across age with those aged 45–64 years more likely (aOR = 1.25; 95% confidence interval (CI), 1.21–1.29; P‐value < 0.001) to have a recorded BMI. Patients with mental health conditions (a OR = 0.80; 95% CI, 0.76–0.84; P‐value < 0.001) and patients with respiratory conditions (aOR = 0.91; 95% CI, 0.86–0.96; P‐value = 0.001) were significantly less likely to have a BMI recorded.
Conclusions
Recording of measures of obesity and overweight in general practices within regional settings is much lower than optimal. More support and advocacy around weighing patients at all interactions is required for regional general practitioners to increase the weight screening in primary care. These findings have policy‐relevant implications for weight management in regional Australia.
Keywords: obesity, practice‐based research, primary health care, primary health care development, regional and rural general practice
Introduction
With an estimated prevalence figure of 63%, obesity and overweight together form the second highest contributor to the burden of disease in Australia.1 A recent chronic disease prevalence study conducted in the regional NSW catchment of Illawarra Shoalhaven2 found the region to have a higher prevalence of overweight and obesity compared with the Australian national age standardised figures. With 81–85% of the resident population of regional Australia estimated to see a general practitioner at least once a year (as per 2010–2011 figures),3 general practice has the best opportunity to continually screen their attending patients for overweight and obesity status and monitor their body mass index (BMI), and where applicable their waist circumference for prompt weight management as recommended by the National Health and Medical Research Council.4
Although some recent studies have looked at the documentation of weight measures in more metropolitan regions of Australia and have found the recording of obesity measures in general practice to be not consistent with guideline recommendations,5 no such studies have investigated similar patterns in regional locations. A study catchment‐specific comparison of the prevalence of high BMI conditions as per the 2011–2012 National Health Performance Authority analysis of Australian Bureau of Statistics (ABS), Australian Health Survey 2011–2013, reveals that 28% of adults were found to be obese in the Illawarra Shoalhaven catchment of regional NSW compared with 16% in the metropolitan catchment of Inner East Melbourne.6 Prevalence figures for overweight or obesity among adults also differed between the two regions, with 64% for the Illawarra Shoalhaven compared with 56% for Inner East Melbourne.6 This again highlights the greater need for accurate and comprehensive BMI recording and monitoring in regional and rural catchments.
In the absence of a standardised system of monitoring trends of BMI recording within medical settings, this study aimed to assess the recording patterns of overweight and obesity‐specific measures in the Illawarra Shoalhaven catchment of regional NSW. No data on recording of BMI information in regional general practice or community health settings were available at the time of this study, and this hence formed one of the major rationales to undertake this analysis.
What is already known on this subject.
International literature suggests low to moderate level of BMI and weight circumference documentation within primary care settings.
Australian studies have reported low levels of BMI but these studies have only been done in metropolitan catchments.
BMI recording and waist circumference measurements are recommended clinical guidelines for weight management in general practice.
What this study adds.
To date no Australian studies have concentrated on regional or rural catchments to evaluate the documentation of obesity and overweight‐specific measurements.
This study reveals these patterns for a regional catchment of NSW.
This study identifies key chronic conditions, patients of which are likely to be missing out on weight screening in regional primary care settings.
Methods
Secondary analysis of a subset of a large cross‐sectional primary care data set was conducted. The Sentinel Practices Data Sourcing (SPDS) project2 database contains health administrative data obtained through extraction of de‐identified clinical patient information from 17 general practices located in the Illawarra Shoalhaven region of NSW for patient interactions between September 2011 and September 2013. The data set represents 39.7% of the regional population, but due to variable proportional representation of each of the statistical local areas (SLAs) of the Illawarra Shoalhaven, the sample may not be truly representative of the resident population.2 Although it is estimated that 86% of the resident population of the Illawarra Shoalhaven region saw a general practitioner at least once a year in 2011–2012,3 the fact that the sample is only composed of persons who access general practice services, and the unequal representation of constituent SLAs limits its population‐level generalisability.
In this study the adult subset of the SPDS data set was further refined to exclude patients without a recorded age and/or gender to yield a sample of n = 118 709 adult patients and their data on general practitioner coded and recorded chronic disease status, age, sex, and information on recording status of BMI and waist measurements in the two‐year period of September 2011 to September 2013.
The Socio‐Economic Indexes for Areas (SEIFA) – Index for Relative Socioeconomic Disadvantage (IRSD)7 scores of the patient's resident SLA were used as an indicator of their socioeconomic status. The IRSD7 is one of the four indexes that have been created by the ABS from social and economic information obtained in the 2011 Census of Population and Housing. The IRSD is a general socioeconomic index that summarises a range of information about the economic and social conditions of people and households within an area. At an Australian national benchmark of 1000, a score of lower than 1000 indicates relatively greater disadvantage in general.
26 of the major specific diseases reported by and included in the SPDS data set were used for analysis to come up with a total ‘Disease Count’ for every patient. While hypertension and hyperlipidaemia were analysed as recorded, other conditions were grouped into major condition groups instead of using individual conditions as suggested by recent multi‐morbidity literature.8 These groupings were: ‘Mental’, which included bipolar, anxiety and depression; ‘Respiratory’, which included asthma and chronic obstructive pulmonary disease (COPD); ‘Musculoskeletal’, which included osteoarthritis, osteoporosis and inflammatory arthritis; ‘Cardiovascular’, which included congestive heart disease, myocardial infarction, heart failure, acute coronary syndrome, peripheral vascular disease, left ventricular hypertrophy, atrial fibrillation and carotid stenosis; ‘Renal’, which included renal artery stenosis, acute renal failure, chronic renal failure and renal impairment; ‘Cancer’, which included cancer and multiple myeloma; and ‘Diabetes’, which included both type 1 and type 2 diabetes mellitus. These 10 conditions/groups of conditions were then used in the analysis as individual variables as well as to compute individual patient's ‘Disease Count’.
Height, weight and waist circumference recordings were analysed across various demographic (age, sex and SEIFA–IRSD) and clinical variables (individual conditions/groups and total disease counts). Data transformations and database collation were conducted using Microsoft Excel (V2013: Microsoft Corporation, Redmond, WA, USA). Further χ2 tests for difference in gender‐based proportions and logistic regression‐based effect estimates in terms of odds ratios (ORs) and associated 95% confidence intervals (CIs) were calculated using SPSS v21 package (IBM SPSS Statistics for Windows, Version 21.0; IBM Corp., Armonk, NY, USA) Due to the lack of practice level information in the aggregated de‐identified data set, tests to account for practice level clustering within the sample were not conducted. Odds ratios were presented in tabulated formats and as forest plots.
The study was performed under the SPDS project2 ethics approval from the Human Research Ethics Committee (Health and Medical) of the University of Wollongong (HE 12/447).
Results
As indicated in Table 1, the sample had more females (55.5%) compared to males (44.5%). Just over three‐quarter of the patients (76.6%) were aged 18–64 years. Hypertension was the most commonly diagnosed and recorded condition (17.9%) followed by musculoskeletal conditions (14.7%) and mental health conditions (14.2%).
Table 1.
Sample descriptive statistics
| Total sample n = 118 709 | ||
|---|---|---|
| Frequency (n) | Percent (%) | |
| Age group | ||
| 18–44 | 53 680 | 45.2 |
| 45–64 | 37 234 | 31.4 |
| 65–74 | 14 384 | 12.1 |
| 75 and over | 13 411 | 11.3 |
| Sex | ||
| Male | 52 781 | 44.5 |
| Female | 65 928 | 55.5 |
| Specific conditions | ||
| Hypertension | 21 224 | 17.9 |
| Hyperlipidaemia | 15 728 | 13.2 |
| Mental† | 16 829 | 14.2 |
| Respiratory‡ | 11 439 | 9.6 |
| Stroke | 1792 | 1.5 |
| Musculoskeletal§ | 17 433 | 14.7 |
| Diabetes | 7066 | 6.0 |
| Cardiovascular¶ | 7334 | 6.2 |
| Renal†† | 1416 | 1.2 |
| Cancer‡‡ | 2950 | 2.5 |
| Disease counts | ||
| 0 | 67 967 | 57.3 |
| 1 | 24 159 | 20.4 |
| 2 | 12 079 | 10.2 |
| 3 or more | 14 504 | 12.2 |
†Includes bipolar, anxiety and depression. ‡Includes asthma and chronic obstructive pulmonary disease. §Includes osteoarthritis, osteoporosis and inflammatory arthritis. ¶Includes congestive heart disease, myocardial infarction, heart failure, acute coronary syndrome, peripheral vascular disease, left ventricular hypertrophy, atrial fibrillation and carotid stenosis. ††Includes renal artery stenosis, acute renal failure, chronic renal failure and renal impairment. ‡‡Includes cancer and multiple myeloma.
Only 36 674 (30.9%) patients had a height and weight recorded in 2 years from September 2011 to September 2013 to enable the estimation of BMI scores (Table 2). Furthermore only 9491 (8.0%) had a waist circumference recorded. Although males had higher BMI recording proportions than females, this was not statistically significant (χ2 = 1.498, P‐value = 0.221). These recording patterns varied across age groups with greater recording proportions for older ages. Compared with the 18–44 year‐old group, logistic regression‐based odds ratios adjusted for age, sex, SEIFA–IRSD, disease count and individual conditions revealed significantly high likelihood for patients aged 45–64 to have a BMI recorded (aOR = 1.25; 95% CI, 1.21–1.29; P‐value <0.001). Persons aged 75 years and over (a OR = 1.17; 95% CI, 1.11–1.23; P‐value <0.001) also had significantly higher odds of BMI recording compared with 18–44 year‐old patients.
Table 2.
BMI and waist circumference recording
| BMI recorded | Waist circumference recorded | |||
|---|---|---|---|---|
| Frequency (n) | Percent (%) | Frequency (n) | Percent (%) | |
| Total | 36 674 | 30.9 | 9491 | 8.0 |
| Age group | ||||
| 18–44 | 11 153 | 20.8 | 1788 | 3.3 |
| 45–64 | 12 716 | 34.2 | 3675 | 9.9 |
| 65–74 | 6089 | 42.3 | 1601 | 11.1 |
| 75 and over | 6716 | 50.1 | 2427 | 18.1 |
| Sex | ||||
| Male | 16 403 | 31.1 | 4590 | 8.7 |
| Female | 20 271 | 30.7 | 4901 | 7.4 |
| Specific conditions | ||||
| Hypertension | 12 303 | 58.0 | 4049 | 19.1 |
| Hyperlipidaemia | 9304 | 59.2 | 3240 | 20.6 |
| Musculoskeletal | 10 159 | 58.3 | 3124 | 17.9 |
| Mental | 7256 | 43.1 | 1969 | 11.7 |
| Respiratory | 5348 | 46.8 | 1399 | 12.2 |
| Diabetes | 4927 | 69.7 | 2336 | 33.1 |
| Cardiovascular | 4605 | 62.8 | 1651 | 22.5 |
| Renal | 1019 | 72.0 | 478 | 33.8 |
| Stroke | 1084 | 60.5 | 361 | 20.1 |
| Cancer | 1696 | 57.5 | 640 | 21.7 |
| Disease counts | ||||
| 0 | 12 021 | 17.7 | 2246 | 3.3 |
| 1 | 8900 | 36.8 | 2055 | 8.5 |
| 2 | 6300 | 52.2 | 1702 | 14.1 |
| 3 or more | 9435 | 65.1 | 3488 | 24.0 |
Adjusted ORs (Table 3 and Fig. 1a) also revealed that most chronic conditions such as hypertension, hyperlipidaemia, musculoskeletal group of conditions, diabetes, cardiovascular group of conditions and renal group of conditions had statistically significantly high odds of BMI recording. However statistically significantly lower levels of BMI recording were associated with mental health conditions (aOR = 0.80; 95% CI, 0.76–0.84; P‐value <0.001) and patients with respiratory conditions (aOR = 0.91, 95% CI, 0.86–0.96; P‐value = 0.001). Likelihood of BMI recording also increased with the total ‘Disease count’ for patients. Compared with the reference category of patients with no recorded condition, patients with a total ‘Disease count’ of three or more recorded conditions were most likely to have their BMI recorded (Table 3 and Fig. 1b).
Table 3.
BMI recording odds ratios and 95% confidence intervals (adjusted for SEIFA–IRSD and all other variables included this table)
| Adjusted odds ratioa (95% CI) for BMI recording | P‐value | |
|---|---|---|
| Age group | ||
| 18–44 | Reference group | |
| 45–64 | 1.25 (1.21–1.29) | <0.001 |
| 65–74 | 1.05 (1.00–1.10) | 0.057 |
| 75 and over | 1.17 (1.11–1.23) | <0.001 |
| Sex | ||
| Male | Reference group | |
| Female | 1.01 (0.98–1.04) | 0.598 |
| Specific conditions | ||
| Hypertension | 1.11 (1.05–1.18) | <0.001 |
| Hyperlipidaemia | 1.14 (1.08–1.21) | <0.001 |
| Musculoskeletal | 1.21 (1.14–1.28) | <0.001 |
| Mental | 0.80 (0.76–0.84) | <0.001 |
| Respiratory | 0.91 (0.86–0.96) | 0.001 |
| Diabetes | 1.83 (1.71–1.95) | <0.001 |
| Cardiovascular | 1.14 (1.07–1.21) | <0.001 |
| Renal | 1.52 (1.34–1.72) | <0.001 |
| Stroke | 0.99 (0.89–1.10) | 0.876 |
| Cancer | 1.05 (0.97–1.15) | 0.225 |
| Disease counts | ||
| 0 | Reference group | |
| 1 | 2.65 (2.51–2.79) | <0.001 |
| 2 | 4.12 (3.77–4.50) | <0.001 |
| 3 or more | 5.18 (4.47–6.00) | <0.001 |
BMI, body mass index; CI, confidence interval; IRSD, Index for Relative Socioeconomic Disadvantage; SEIFA, Socio‐Economic Indexes for Areas.
Reference category is “no” for specific conditions.
Figure 1.
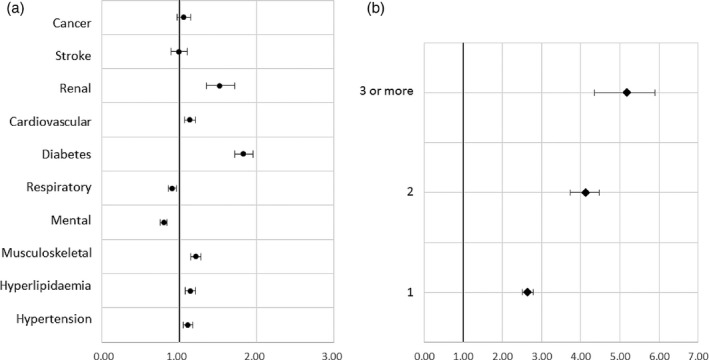
(a) Forest plot of adjusted* odds ratios and 95% confidence intervals for BMI recording – by specific conditions. (b) Forest plot of adjusted* odds ratios and 95% confidence intervals for BMI recording – by total ‘Disease counts’. * adjusted for SEIFA‐IRSD and all other variables included in Table 2.
Discussion
The study reveals some significant findings especially in terms of the low likelihood of BMI recording for patients with chronic mental health conditions and those with chronic respiratory conditions. In particular these findings are extremely relevant for regional parts of Australia that have not been explored in previous literature on the topic. While the results are only specific to the Illawarra Shoalhaven region and cannot be claimed to be generalisable to all of regional Australia, the findings are quite significant from a policy and planning perspective. Unlike other regions, the geographical catchment boundary of the Illawarra Shoalhaven Local Health District were the same as that covered by a single Medicare Local namely the Illawarra‐Shoalhaven Medicare Local at the time of the SPDS data collection.2 This placed the region in a unique and advantageous position in terms of planning and implementing collaborative preventive health initiatives and chronic disease‐monitoring programs across both primary and tertiary sectors of health services delivery. Additionally the region has a diverse socio‐economic profile and has pockets of both higher and lower socioeconomic disadvantage,2 as per the SEIFA–IRSD scores of its constituent SLAs. So findings of low BMI recording in primary care settings within a socioeconomically diverse health catchment that is served by just the one peak health care organisation each at both acute/tertiary sector and the primary sector, poses significant challenges and policy questions that need addressing especially for larger catchments that incorporate multiple local health districts and multiple primary health care organisations.
As clinical management guidelines for obesity depend on ascertainment of BMI and the complications of obesity,9 prompt screening for BMI is clinically vital for appropriate patient management. Previous literature has found issues such as lack of time, inadequate training or lack of confidence in weight management to be reasons for the incomplete documentation of weight management plans in primary care settings.10 A significant role is also played by whether exercise counselling skills are perceived as a priority by the clinician and whether these skills were taught to the respective practitioner during his/her postgraduate year of training.11 Exposure to apt levels of training in advocating weight management to all patients and undertaking exercise/physical activity counselling during postgraduate education of physicians has been found to be significant in improving practitioner skills in real‐world practice and provides the required level of confidence in doing so on a regular basis.10, 11 Although most general practitioners would acknowledge the importance of weight management both in terms of BMI recording and undertaking preventive health counselling, evidence among general practitioners does reveal differences between self‐reports of current practice and perceived desirable practice by general practitioners.12 The low levels of BMI recording therefore could be largely attributable to actual or perceived time constraints during a clinical consultation.10 All these reasons could also be argued as possible reasons for poor recording of height, weight and waist circumference measures in this study sample.
In more metropolitan catchments in Australia, support to practices and general practitioners through dedicated liaison officers has been attempted to support the implementation of weight management guidelines particularly through enhancing organisational capacity.5 However such initiatives have questionable sustainability and are logistically much more difficult to implement in geographically larger yet regional and remote areas such as the one in this study. Within the Illawarra Shoalhaven region of NSW, through the SPDS project,2, 13 the regional Medicare Local has been undertaking ‘Data cleansing’ training and assistance to clinicians wherein staff working in participating practices receive training and support to improve the accuracy and completeness of patient records within their medical software. However this has been reported by the study researchers to be a resource‐intensive and time‐consuming task. The SPDS study reported that “Researchers manually trained the practice staff who then undertook data cleaning”,13 which may have been feasible for the SPDS study with a sample of 17 practices,2 but with the transition from 61 Medicare Locals to 31 larger Primary Health Networks (PHNs) in Australia,14 such practice liaison officer/regional primary care organisational staff led quality improvement initiatives over a larger number of general practices and as larger geographic areas would be even more resource‐intensive, time‐consuming and cost‐prohibitive. While studies have highlighted the higher likelihood of trainee general practitioners (GPs) actively using online mechanisms for post‐graduate training15 within general practice settings, other innovative uses of information technology like linking clinical practice guidelines or continuing medical education prompts into electronic medical records also have been suggested to facilitate evidence‐based general practice.16 More online, web‐based tools to assist primary care practitioners in undertaking evidence‐based consultations consistent with clinical practice guidelines need to be trialled, investigated and evaluated further.
The study has some limitations. While the SPDS methodology indicates having conducted ‘Data cleansing’ training for GPs and practice staff for the participating practices, there still might have been several free‐text entries of BMI and waist circumference recordings. These (if existed) would have been missed by the data set and hence could possibly lead to under‐estimation of the relevant measures. So, despite undertaking significant at‐source as well as post‐collection data cleansing, the SPDS database still has the potential for data entry errors, which is a limitation to this study. Another limitation of the study is that due to the lack of available practice level information within the dataset, tests to examine effects of practice level clustering and undertake cluster adjustment through generalised estimating equations or generalised linear mixed model analysis were not done.
Nevertheless the study has significant implications for general practice and general practitioner‐led preventive health endeavours. Additionally as the percentage of adults who are overweight or obese has been reported to increase with geographic remoteness,6 the efforts for weight management within regional catchments like the Illawarra Shoalhaven need stringent attention. The study clearly identifies that general practice‐based recording of clinical guidelines‐advocated weight measurements is below optimal and that more support is needed to improve levels of screening for obesity and overweight especially in regional Australian general practice settings.
The findings also highlight the low levels of BMI recording for mental health patients and patients with asthma or COPD. There is vast amount of recent literature that illustrates the significant relationship of high BMI and mental health disorders17, 18 with a bidirectional comorbidity relationship.19 Additionally chronic respiratory disease patients such as COPD sufferers who are obese have been found to have poorer quality of life and poorer health outcomes.20 Even in terms of asthma, high BMI has been found to have a dose‐dependent high likelihood of incident asthma in adults and interventions to reduce BMI have been suggested to decrease asthma levels.21 This places the early identification and regular monitoring of BMI as a vital step in chronic disease prevention, control as well as management. With recent studies exploring the high levels of multimorbidity in Australian general practice settings22 and its correlation with poor health outcomes, it is imperative that patients with chronic conditions like depression, anxiety, asthma and COPD undergo regular and prompt general practice screening for obesity and overweight to avoid being at risk of further comorbidities.
Acknowledgements
The author would like to acknowledge the financial and other support from the COORDINARE – South Eastern NSW PHN (formerly the Illawarra‐Shoalhaven Medicare Local), which funded the Sentinel Practices Data Sourcing (SPDS) project under the Illawarra‐Shoalhaven Medicare Local funding from the Australian Government Department of Health.
References
- 1. Australian Institute of Health and Welfare . Overweight and obesity. AIHW, 2015.
- 2. Ghosh A, Charlton K, Girdo L, Batterham M. Using data from patient interactions in primary care for population level chronic disease surveillance: the Sentinel Practices Data Sourcing (SPDS) project. BMC Public Health 2014; 14: 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Health Performance Authority . Healthy communities: Australian's experiences with primary health care in 2010–11. Sydney, NSW 2001 Australia, 2013.
- 4. National Health and Medical Research Council . Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia. Melbourne, Australia, 2013.
- 5. Turner LR, Harris MF, Mazza D. Obesity management in general practice: does current practice match guideline recommendations? Medical Journal of Australia 2015; 202: 370–372. [DOI] [PubMed] [Google Scholar]
- 6. National Health Performance Authority . Healthy communities: overweight and obesity rates across Australia, 2011–12 (in focus). Sydney, NSW 2001 Australia, 2013.
- 7. Pink B. Socio‐Economic Indexes for Areas (SEIFA) – Technical paper. Canberra, ACT: Australian Bureau of Statistics, 2011; ABS Catalogue no. 2033.2030.2055.2001.
- 8. Harrison C, Britt H, Miller G, Henderson J. Examining different measures of multimorbidity, using a large prospective cross‐sectional study in Australian general practice. BMJ Open 2014; 4: e004694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rose S, Turchin A, Grant R, Meigs J. Documentation of body mass index and control of associated risk factors in a large primary care network. BMC Health Services Research 2009; 9: 236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Muo IM, Sacajiu G, Kunins H, Deluca J. Effect of the availability of weight and height data on the frequency of primary care physicians' documented BMI, diagnoses and management of overweight and obesity. Quality in Primary Care 2013; 21: 221–228. [PubMed] [Google Scholar]
- 11. Rogers LQ, Bailey JE, Gutin B et al Teaching resident physicians to provide exercise counseling: a needs assessment. Academic Medicine 2002; 77: 841–844. [DOI] [PubMed] [Google Scholar]
- 12. Bull FC, Schipper EC, Jamrozik K, Blanksby BA. Beliefs and behaviour of general practitioners regarding promotion of physical activity. Australian Journal of Public Health 1995; 19: 300–304. [DOI] [PubMed] [Google Scholar]
- 13. Ghosh A, Charlton KE, Girdo L, Batterham MJ, McDonald K. Addressing the deficiencies in the evidence‐base for primary practice in regional Australia – Sentinel Practices Data Sourcing (SPDS) project: a pilot study. BMC Family Practice 2013; 14: 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Health AGDo . Primary Health Networks (PHNs). Canberra, ACT: Commonwealth of Australia, 2015.
- 15. Kjaer NK, Maagaard R, Wied S. Using an online portfolio in postgraduate training. Medical Teacher 2006; 28: 708–712. [DOI] [PubMed] [Google Scholar]
- 16. Kidd MR, Mazza D. Clinical practice guidelines and the computer on your desk. The Medical Journal of Australia 2000; 173: 373–375. [DOI] [PubMed] [Google Scholar]
- 17. Kim J, Noh J‐W, Park J, Kwon YD. Body mass index and depressive symptoms in older adults: a cross‐lagged panel analysis. PLoS ONE 2014; 9: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McLaren L, Beck C, Patten S, Fick G, Adair C. The relationship between body mass index and mental health. Social Psychiatry and Psychiatric Epidemiology 2008; 43: 63–71. [DOI] [PubMed] [Google Scholar]
- 19. Mumford EA, Liu W, Hair EC, Yu T‐C. Concurrent trajectories of BMI and mental health patterns in emerging adulthood. Social Science and Medicine 2013; 98: 1–7. [DOI] [PubMed] [Google Scholar]
- 20. Cecere LM, Littman AJ, Slatore CG et al Obesity and COPD: associated symptoms, health‐related quality of life, and medication use. COPD: Journal of Chronic Obstructive Pulmonary Disease 2011; 8: 275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta‐analysis of prospective epidemiologic studies. American Journal of Respiratory and Critical Care Medicine 2007; 175: 661–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Medical Journal of Australia 2008; 189: 72–77. [DOI] [PubMed] [Google Scholar]


