Abstract
The practice of regional anaesthesia is rapidly changing with the introduction of ultrasound into the working domain of the anaesthesiologist. New techniques are being pioneered. Among the recent techniques, notable are the truncal blocks, for example, the transversus abdominis plane block, rectus sheath block, hernia block and quadratus lumborum block in the abdomen and the pectoral nerves (Pecs) block 1 and 2, serratus anterior plane block and intercostal nerve block. This narrative review covers the brief anatomical discourse along with technical description of the ultrasound-guided truncal blocks.
Key words: Pecs block, transversus abdominis plane block, truncal blocks, ultrasound-guided regional anaesthesia
INTRODUCTION
With the introduction of portable ultrasound machine in the operating theatres, the practice of regional anaesthesia has seen a transition from landmark-based techniques to regional blocks administered under direct vision through the new eye of the anaesthetist, the ultrasound machine. Use of ultrasound in regional anaesthesia was initially limited to peripheral nerve blocks until Hebbard et al.[1] described the ultrasound-guided transversus abdominis plane (TAP) block. Following years saw emergence of newer regional anaesthesia techniques that are performed on the trunk, hence called the truncal blocks.
The unique feature of the ultrasound-guided truncal blocks is that in all of these techniques, in contrast to peripheral nerve blocks, no nerve or plexus needs to be identified: Local anaesthesia (LA) is injected in a particular muscle plane, in which the injectate spreads and reaches the intended nerves. This simple mechanism has made delivery of nerve blocks easy and versatile.
In this article, we have described the truncal blocks, many of which are still in research phase and yet to find regular clinical application. The truncal blocks can be broadly divided into blocks of the abdominal wall and blocks of the chest wall [Table 1].
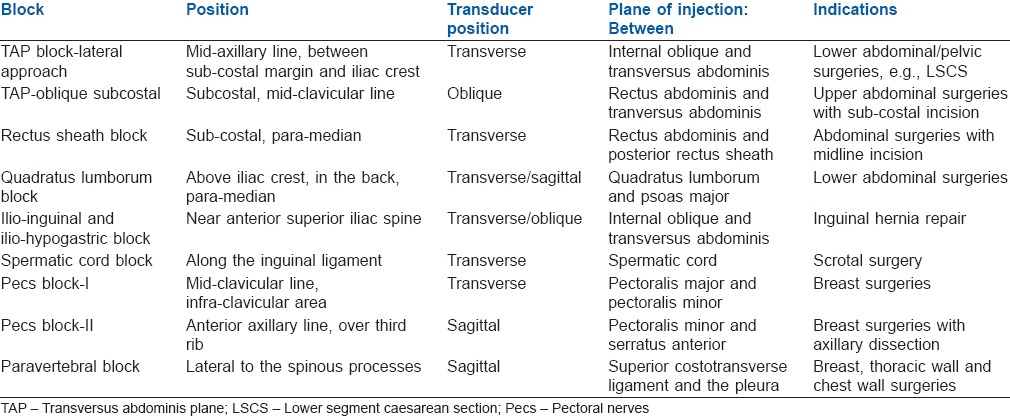
Table 1.
Ultrasound-guided truncal blocks: summary
BLOCKS OF THE ANTERIOR ABDOMINAL WALL
Transversus abdominis plane block
The anterior branches of the intercostal nerves T7–12 that innervate the anterior abdominal wall along with anterior rami of the first lumbar spinal nerve (L1) travel in the plane between the internal oblique muscle (IOM) and transversus abdominis muscle (TAM).[2] The technique aims to inject 15–20 mL LA in the plane between these muscles [Figure 1]. The landmark-based technique was first described by Dr. Rafi.[3] The technique comprised eliciting two pops or loss of resistance (LOR) by a blunt-tipped needle entering perpendicularly at the lumbar triangle of Petit. For midline surgeries, the block has to be repeated on both sides. TAP block is the easiest to learn and most widely practised truncal block.
Figure 1.
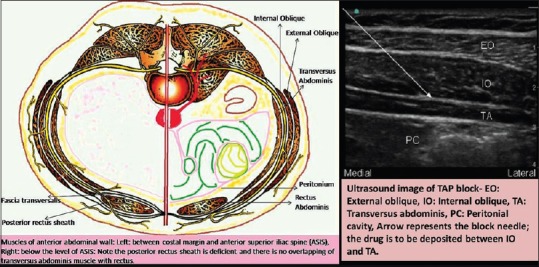
Left: Diagram showing the anatomical basis of transversus abdominis plane block and rectus sheath block. Right: ultrasound image of transversus abdominis plane (arrow)
There are three described approaches to TAP block:
Posterior approach: Injection in the lumbar triangle of Petit. Usually employed in the landmark-based technique[4,5,6,7]
Lateral approach: LA is injected in the neurovascular plane between the IOM and TAM with the ultrasound transducer (UST) placed transversely in the anterior axillary line, above the iliac crest[6,7]
Oblique subcostal approach: Injection in the subcostal area; LA is injected between the posterior rectus sheath (PRS) and TAM.[8]
Oblique subcostal TAP (OSTAP) is also called upper TAP block. The term dual TAP means administration of TAP block in both lower, (i.e., by lateral approach), and upper areas.[9,10] Bilateral administration of dual TAP block is required to provide complete analgesia to the anterior abdominal wall. This method is also known as four-quadrant TAP block.[11]
Ultrasound technique
Ultrasound-guided TAP block is considered as a basic level skill block. The patient is placed supine, but a lateral position may be helpful in an obese patient.[12] A linear UST with frequency between 10 and 18 MHz with depth setting adjusted between 3 and 5 cm (depending on the amount of adipose tissue) is placed transversely across the abdomen above the iliac crest at the anterior axillary line. External oblique muscle (EOM), IOM and TAM (superficial to deep) can be easily identified below the adipose tissue, and IOM is usually the most prominent muscle among the three. The peritoneal cavity lies deep to the TAM and can be identified by the movement of the bowel loops. If it is difficult to identify all the three layers, then the UST should be placed at the midline and rectus abdominis muscle (RAM) is identified and the UST is moved laterally where RAM tapers and ends in the linea semilunaris and the obliques begin. The UST is then moved laterally to a point where the three muscles can be clearly demarcated and the needle is introduced. A 100 mm 20-gauge/22-gauge Tuohy needle is chosen and introduced from anterior to posterior direction. The aim is to inject 15–20 mL LA in the plane between the IOM and TAM. Accurate placement of the needle tip may be facilitated by injection of a small amount of fluid (1–2 mL saline or LA) to hydro-dissect the appropriate plane. Correct placement of the injectate is confirmed by seeing the spindle-shaped hypo-echoic fluid pocket in the space lined by the hyper-echoic fascia of the IOM and the TAM after the injection.
For the OSTAP muscle block, the UST is placed just below the costal margin close to the midline and RAM is identified. In the sub-costal area, TAM lies deep to the rectus muscle. The block needle is then introduced into the plane between PRS and TAM. Block needle is gradually advanced laterally through hydro-dissection till we can see EOM and IOM along the lateral border of the rectus. A volume of 20–25 mL of anaesthetic solution is given along the line between the xiphoid process and iliac crest. OSTAP is considered advanced level block.
Indications
Analgesia for laparoscopic surgery, hysterectomy, lower segment caesarean section, herniorrhaphy, etc., An upper TAP block presumably, is more effective in upper abdominal surgeries while pain relief for sub-umbilical surgeries is well addressed by lower TAP block. Four-quadrant TAP block has been used for post-operative analgesia in laparotomies using a larger incision [Figure 2].
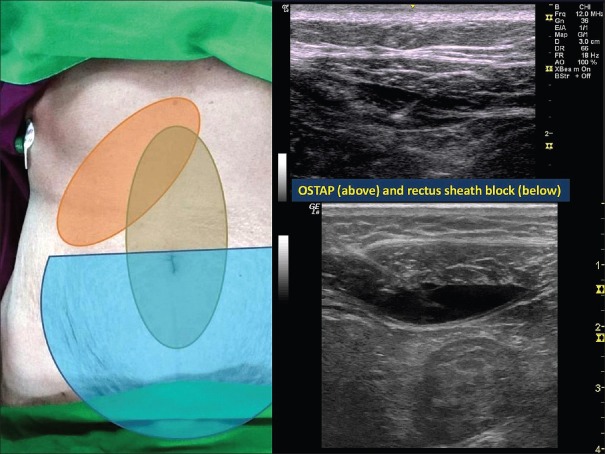
Figure 2.
Left: Comparison of sensory block achieved by bilateral rectus sheath block (grey area over midline), bilateral transversus abdominis plane block (green semi-circle over lower abdomen) and unilateral oblique subcostal transversus abdominis plane block (which can vary but approximately covers the area shaded in orange); Right: Above: Ultrasound image of oblique subcostal transversus abdominis plane block: the needle is seen depositing the drug (black area) between the posterior rectus sheath and the transversus abdominis muscle. Below: Rectus sheath block: the needle is seen depositing the drug between the rectus abdominis muscle and the posterior rectus sheath
Complications
Complications such as intraperitoneal injection, liver trauma and catheter breakage have been reported with TAP block; however, with the use of ultrasound, the incidence of complications has reduced considerably.
Rectus sheath block
The rectus sheath block (RSB) was first described in 1899 and was initially used for the purpose of abdominal wall muscle relaxation during laparotomy before the introduction of neuromuscular block. Now, it is used for analgesia after umbilical or incisional hernia repairs and other midline surgical incisions. The aim is to block the terminal branches of the T9–11 intercostal nerves which run between IOM and TAM to penetrate the posterior wall of RAM and end in an anterior cutaneous branch supplying the skin of the umbilical area.[13] A catheter can be placed for continuous infusion of LA.[14]
Ultrasound technique
A high-frequency linear array UST is held transversely over the RAM, which can be easily identified by its spindle-like shape on transverse section. A 22-gauge Tuohy needle is inserted into the plane between RAM and the PRS and 10–15 mL of LA is injected. A catheter may be placed for a continuous block. For inserting the catheter, the UST is rotated by 90° and a plane is created between RAM and PRS by hydro-dissection. The catheter is advanced 5–6 cm into the space. Bilateral catheter is required for a midline surgery.
Indications
post-operative analgesia for umbilical hernia repair and other umbilical surgeries.
Transducer position is transverse on the abdomen immediately lateral to the umbilicus.
Complications
Wound infection and catheter migration to intraperitoneal space are known complications of RSB.
Quadratus lumborum block
Quadratus lumborum block (QLB) is a posterior extension of the TAP block. It was first described by Dr. Blanco,[15] and it was later modified by Sauter et al.[16] The transmuscular approach involves injection of LA in the plane between quadratus lumborum (QL) and the psoas major muscles (PMMs) [Figure 3]. A catheter can also be inserted for continuous infusion.
Figure 3.
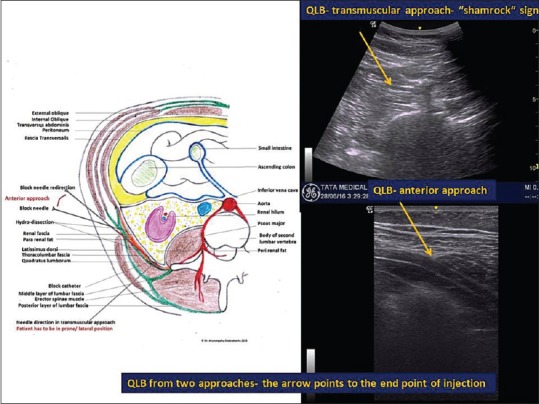
Quadratus lumborum block: Left: Anatomical basis of anterior and transmuscular approaches. Right above: The transmuscular approach. Right below: The anterior approach
Ultrasound technique
The patient is kept in a lateral or prone position. A curvilinear UST is held transversely above the iliac crest. The transducer is then moved dorsally keeping the transverse orientation until the QL muscle is identified with its attachment to the lateral edge of the transverse process of the L4 vertebrum. With the PMM anteriorly, the erector spinae muscle posteriorly and the QL muscle adherent to the apex of the transverse process, a well recognisable pattern of a shamrock with three leaves can be seen.[16] Imaging studies have shown that in QLB, the LA reaches the paravertebral space.[17,18] Thus, QLB has been claimed to cause better analgesia than TAP block as it not only provides analgesia to the anterior abdominal wall but also blocks visceral pain.
Recently, an anterior approach[19] has also been described in paediatric patients, where a linear UST is held transversely in the posterior axillary line, and LA is injected in the plane between the anterior surface of the QL and the thoracolumbar fascia. QLB targets the lumbar plexus as well. Some clinical reports suggest its use in hip surgeries.
Indications
QLB is used for unilateral abdominal surgeries such as nephrectomy.
Complications
No complications have been reported so far with this block; however, catheter migration to retroperitoneal space is a concern.
Ilio-inguinal nerve and ilio-hypogastric nerve block or the hernia block
The ilio-inguinal nerve (IIN) and ilio-hypogastric nerve (IHN) arise from the first lumbar nerve and emerge from the upper part of the lateral border of the PMM. IIN is smaller of the two and travels caudally to IHN. As the lateral cutaneous branch of IHN may pierce the internal and EOMs immediately above the iliac crest, the nerves should be blocked as proximal as possible, i.e., just above the iliac crest, so these cutaneous branches are not spared.
Field block for inguinal hernia surgery has been administered since the 1980s.[20,21,22,23]
Studies indicate that the ultrasound-guided TAP block approach is superior to landmark-based approaches of IIN and IHN block.[24,25,26,27] This block has been used extensively in paediatric anaesthesia practice.[28]
Ultrasound technique
The patient is placed supine and the UST (linear) is placed obliquely just above the iliac crest along the line joining the anterior superior iliac spine and the umbilicus.[23,24] A 5–8 cm 22-gauge needle is inserted in the plane. LA is deposited in the same plane as that of TAP block, i.e. between the IOM and TAM. LA is injected per side about 10–15 mL. Correct placement of the needle is identified by the expansion of the space lined by the hyper-echoic fascia of IOM and TAM after the injection.
Indications
Anaesthesia and postoperative analgesia for inguinal hernia repair and surgeries following suprapubic incision.
Complications
Intraperitoneal injection and femoral nerve block are known complications.
Spermatic cord block or genitofemoral nerve block
The spermatic cord contains the genital branch of the genitofemoral nerve and the testicular sympathetic plexus while the IIN lies just lateral to the cord. It also contains three arteries, viz. testicular artery, cremasteric artery and deferential artery and three veins, viz. pampiniform plexus and testicular vein, cremasteric vein and deferential vein. Landmark-based approach of spermatic cord block has been used by the surgeons for surgeries of scrotum and the testes, but the blind block often damages the blood vessels and cause haematoma.
Ultrasound technique
With ultrasound, it is easy to find out the spermatic cord and its contents. A high-frequency linear UST is used to image and identify the spermatic cord as an oval structure lying medial and superficial to the femoral artery.[29] Block can be attempted below or at the level of inguinal ligament, just medial and above the pubic tubercle. Care must be taken to avoid the blood vessels in close vicinity.[30,31]
Indications
The indications are scrotal surgeries, chronic pain in the genitofemoral nerve area.[29]
Complications
Vascular trauma is apprehended; however, with the use of ultrasound, the block is safer.
BLOCKS OF THE CHEST WALL
Pecs block
The lateral pectoral nerve (LPN) and the medial pectoral nerve (MPN) are the main branches of the brachial plexus that innervates pectoral muscles. LPN arises from the lateral cord of the brachial plexus and the roots of T5–7 cervical nerves. MPN originates from the medial cord of the brachial plexus from roots C8 and T1.[32] LPN pierces the coracoclavicular fascia and is distributed to the deep surface of the pectoralis major muscle (PMm) and innervates its clavicular head. LPN provides sensory innervation to acromioclavicular joint, sub-acromial bursa, periosteum of the clavicle and anterior articular capsule of the shoulder joint and costoclavicular ligaments.[33] MPN enters the deep surface of the pectoralis minor muscle (Pmm), where it supplies the muscle. Two or three of its branches pierce the muscle and end in the PMm and innervate its costal head. MPN gives sensory innervation to inferolateral part of the PMm, ventral aspect of the arm and chest wall near the armpit along with the intercostobrachial nerve [Figure 4].
Figure 4.
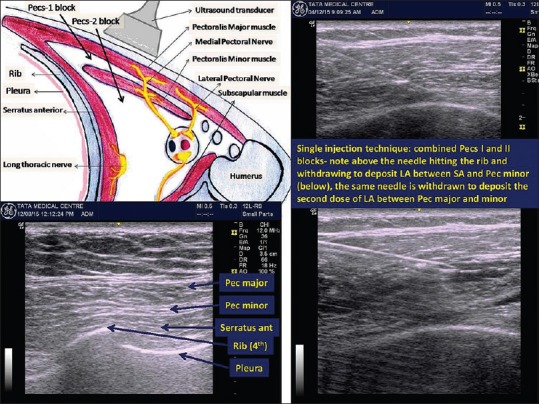
Left above: Anatomical basis of pectoral nerves block. Left below: Initial ultrasound scan showing chest wall muscles, ribs and pleura. Right: Ultrasound images of performing combined Pecs-1 and Pecs-2 blocks in single injection technique
Pecs-1
The Pecs-1 block is an interfascial plane block that aims to block the lateral and MPNs. LA about 10–15 mL is injected between the PMm and Pmm. The block is safely and reliably done under ultrasound guidance with the help of high-resolution linear UST.
Ultrasound technique
For the pectoral blocks, the patient has placed supine and a linear high-frequency UST is used. Depth is usually set at 3–5 cm. The UST is either held in a sagittal plane (same as in infraclavicular brachial plexus block) as described by Blanco[34] or placed below the lateral one-third of the clavicle transverse to the axis of the body.[35] The needle is directed from superomedial to inferolateral direction in both the approaches. Cranially, we can see the clavicle and below it we can see PMm (superficial) and Pmm (deep). Deep to the muscles, we can see the axillary artery and the vein. If a rib is visualised, it is usually the second rib and the pleura can be seen as bright hyper-echoic line beneath it. For Pecs-1 block, the 5–8 cm 22-gauge block needle is inserted and advanced in-plane to the UST from cranial to caudal direction and 10 mL of LA solution is injected between the two muscle layers.
Indications
Breast surgeries such as lumpectomy andinvolving breast expander/prosthesis.[34]
Pecs-2
In Pecs-2 block, 20 mL of LA is injected between the lateral edge of the Pmm and the serratus muscle at the level of the third rib. The aim is to block the lateral rami of intercostal nerves and the long thoracic nerve. This block is useful for most of the breast surgeries including axillary dissections.[35,36]
Ultrasound technique
The UST is moved caudally from the Pecs-1 position till the third and the fourth ribs are visualised. The UST is then rotated 90° so that it lies transversely and moved laterally towards the anterior axillary line keeping the third rib at the centre so that the lateral border of Pmm is identified. Serratus anterior muscle is seen deeper to the Pmm lying on top of the third rib. The needle is advanced from medial to lateral side parallel to the ultrasound beam, and 20 mL of LA solution is injected in the plane between Pmm and serratus anterior.
Recently, a single injection technique of combined Pecs-1 and Pecs-2 blocks has been described.
Indications
Breast surgery with axillary node dissections.
Complications
No complications have been reported so far, but pneumothorax and trauma to vessels such as the thoracodorsal artery are concerns with these techniques.
Serratus anterior plane block
The serratus anterior plane (SAP) block is a recently described regional block, designed to block the thoracic intercostal nerves along with the thoracodorsal and the long thoracic nerves. It aims to provide analgesia to the anterolateral and part of the posterior side of the chest wall as an alternative to epidural and paravertebral blocks. SAP block was described in healthy volunteers without clinical validation. The sensory paraesthesia was described in dermatomes from T2–9. In this block, the injectate is administered either superficial or deep to the serratus anterior muscle, and the difference is only the duration of the block. Duration of the block was found to be doubled if the LA solution was injected superficial to the SA muscle. Serratus plane block is a variation of Pecs-2; only the needle is placed in more caudally and posteriorly compared to Pecs-2 block. The needle is advanced “in plane” from caudal to cranial approach at the level of mid-axillary line.[37,38]
Ultrasound technique
This block is usually performed in lateral or sitting decubitus. The UST is moved caudally (from Pecs-2 position) and laterally towards the mid-axillary line counting the ribs and serratus anterior muscle is identified as a thin sheet lying above the ribs. Keeping the 5th rib in the middle of the ultrasound screen, the block needle is inserted in plane from anteromedial to posterolateral direction. LA solution about 20 mL is injected in mid-axillary line at the level of the 5th rib either superficial or deep to the serratus anterior. To prevent inadvertent pneumothorax, it is important to aim the needle towards the rib. The Pecs-2 and the SAP block are considered “advanced level” skill block because of the vicinity of crucial structures and demanding technique.
Indications
SAP produces analgesia of the hemi-thorax. A few clinical reports are available about its efficacy for post-operative analgesia.[39]
Complications
No complications have been reported so far, but pneumothorax is a concern.
Intercostal nerves block
The intercostal nerves arise from the ventral rami of the thoracic spinal nerve. They are mixed nerves containing both sensory and motor fibres. The collateral branch of the intercostal nerve runs along the upper border of the rib below. It gives motor innervations to the intercostal muscles, latissmus dorsi, serratus anterior and abdominal wall muscles and sensory innervations to the pleura, peritoneum, anterior and lateral chest and abdominal walls.
Intercostal block produces stretch of band-like anaesthesia along the chosen plane.[40,41]
Ultrasound technique
Patient decubitus is lateral, sitting or prone. A high-frequency linear array transducer is used. The ribs are identified by their curved hyper-echogenic surface outline and the acoustic shadow underneath them in a parasagittal view (between adjacent ribs, the intercostal muscles and pleura is identified (hyper-echoic line in gliding motion during respiration). Initial scanning is performed in the transverse plane of the rib to identify the level. The level of the block is marked by counting the ribs from above downwards starting from the 2nd rib or in opposite direction starting from the 12th rib.[40,41] Another landmark used is T7 at the level of tip of scapula.[41] The ideal point to block the nerve is at the angle of the rib (6–7 cm lateral to the spinous process) before the nerves branches out.[42,43] The neurovascular bundle lies between the internal intercostal and the innermost intercostal muscles.
In-plane or out-of-plane approach can be used. It is very important to identify the plane by hydro-dissection at every level to prevent damage to the pleura[44,45] or the vascular bundle lying in proximity to the nerve. It is prudent to check for pnemothorax by seeing the gliding movement of the pleura and the comet tail appearance underneath (they both disappear in case of pneumothorax).[45] Once the correct plane is reached, 3–5 mL of LA solution should be injected after careful aspiration. The needle is introduced usually from the superior border of the rib below.
Indications
For providing surgical anaesthesia for thoracic and upper abdominal procedures and analgesia in case of chest trauma, flail chest and intercostal drain placement. This block is also given for chronic pain management in cases of postherpetic neuralgia.[42,43,44,45,46,47,48,49]
Complications
Pneumothorax is a known complication.
Interpleural block
LA is injected between the two layers of pleura. It is effective for thoracic and upper abdominal surgeries. Some centres regularly practice this block while others refrain from it citing the reported 2% incidence of pneumothorax among other complications such as pleural infection and adhesion.[50,51] Landmark-based technique using a saline infusion has been practiced widely.[52] Use of ultrasound is expected to bring down the complication rate.
Ultrasound technique
Patient can be in sitting, lateral, semi-prone or prone position. A high-frequency linear UST is held transversely to image the pleura at 5–6th intercostal space in the posterior axillary line. The two layers of pleura may be difficult to identify. The needle is inserted in plane to breach the internal intercostal membrane, directly beneath which lies the pleura, which can be seen as a shiny white line. The needle then is very slowly inserted further to breach the parietal pleura. A saline infusion technique can be used for additional safety to find out the inter-pleural space. A saline drip is attached to the block needle and made air free in the beginning. Inter-pleural space being a negative pressure space, the saline starts flowing freely once the needle enters the parietal pleura. Alternatively, an LOR syringe can also be used.[53,54] A catheter can be placed in situ for continuous analgesia.
Indications
Inter-pleural block has been shown to provide safe, high-quality analgesia after cholecystectomy, thoracotomy, renal and breast surgery and invasive radiological procedures of the renal and hepatobiliary systems. It has been used successfully in the treatment of pain from multiple rib fractures, herpes zoster, complex regional pain syndromes, thoracic and abdominal cancer and pancreatitis.[53,54,55]
Complications
Pneumothorax, pleural infection and adhesion are known complications.
THORACIC PARAVERTEBRAL BLOCK
The thoracic paravertebral space in transverse section is triangular in shape. The base is formed by the posterolateral aspect of the vertebral body, intervertebral discs, intervertebral foramina and articular processes; anterolateral border by the parietal pleura and the posterior border by the superior costotransverse ligament (CTL). This space communicates with the intercostal space laterally, and caudally, it extends up to L1 at the origin of psoas muscle.[56] Medially, it communicates with the epidural space through the intervertebral foramen. It contains fatty tissue, thoracic spinal nerves, intercostal vessels and the sympathetic chain.
Ultrasound technique
Patient can be in sitting, lateral or prone position. A high-frequency linear UST is held in the mid-scapular line in the sagittal plane and the desired level is found by counting the ribs or by counting the vertebrae. The rib surfaces (upper and lower) are seen as elevated dome-like structures, and in between them, three layers of intercostal muscles can be seen above the pleura, which is a shiny hyper-echoic line moving with respiration. The UST is then moved medially from there to reach the paravertebral space, which is at the level of the transverse processes where the upper surface is flat and intercostal muscles disappear. CTL may be seen as a hyper-echoic line between the two transverse processes. At the base of the space lies pleura.[57]
Both in-plane and out-of-plane approaches can be taken, the latter being preferred usually.[58] The target is to inject LA between the CTL and the pleura. Upon injection of LA, pleura is seen moving down, which is a hallmark of correct needle placement.
Indications
Thoracic paravertebral block (TPVB) can be used for perioperative pain relief after thoracic wall, chest wall and breast surgeries and renal surgeries. It can also provide pain relief after multiple rib fractures.
Complications
Pleural puncture, pneumothorax and epidural spread of the LA are the known complications of TPVB.
CONCLUSION
Ultrasound-guided regional anaesthesia techniques are safer and more effective than comparable landmark-based approaches.[59] Although the journey started from imaging the known landmark-based approaches, the direction of current research is towards an era when ultrasound will become a necessity for the practice of regional anaesthesia as many techniques will be plausible only with the help of ultrasound. The truncal blocks are early representatives of that category of blocks. A working knowledge of regional anatomy is essential as well as ergonomics such as selecting the right position, side and equipment.[60] With the principles maintained, working with ultrasound can be an enjoyable educational journey for anaesthesiologists.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–7. [PubMed] [Google Scholar]
- 2.Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: A new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–33. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 3.Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 4.McDonnell JG, O'Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 5.Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66:1023–30. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 6.Abdallah FW, Chan VW, Brull R. TAM plane block: The effects of surgery, dosing, technique, and timing on analgesic outcomes. A systematic review. Reg Anesth Pain Med. 2012;37:193–209. doi: 10.1097/AAP.0b013e3182429531. [DOI] [PubMed] [Google Scholar]
- 7.Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: A meta-analysis. Br J Anaesth. 2013;111:721–35. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 8.Hebbard PD, Barrington MJ, Vasey C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: Description of anatomy and clinical technique. Reg Anesth Pain Med. 2010;35:436–41. doi: 10.1097/aap.0b013e3181e66702. [DOI] [PubMed] [Google Scholar]
- 9.Børglum J, Maschmann C, Belhage B, Jensen K. Ultrasound-guided bilateral dual transversus abdominis plane block: A new four-point approach. Acta Anaesthesiol Scand. 2011;55:658–63. doi: 10.1111/j.1399-6576.2011.02430.x. [DOI] [PubMed] [Google Scholar]
- 10.Børglum J, Jensen K, Christensen AF, Hoegberg LC, Johansen SS, Lönnqvist PA, et al. Distribution patterns, dermatomal anesthesia, and ropivacaine serum concentrations after bilateral dual transversus abdominis plane block. Reg Anesth Pain Med. 2012;37:294–301. doi: 10.1097/AAP.0b013e31824c20a9. [DOI] [PubMed] [Google Scholar]
- 11.Niraj G, Kelkar A, Hart E, Horst C, Malik D, Yeow C, et al. Comparison of analgesic efficacy of four-quadrant TAM plane (TAP) block and continuous posterior TAP analgesia with epidural analgesia in patients undergoing laparoscopic colorectal surgery: An open-label, randomised, non-inferiority trial. Anaesthesia. 2014;69:348–53. doi: 10.1111/anae.12546. [DOI] [PubMed] [Google Scholar]
- 12.Toshniwal G, Soskin V. Ultrasound-guided transversus abdominis plane block in obese patients. Indian J Anaesth. 2012;56:104–5. doi: 10.4103/0019-5049.93368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sandeman DJ, Dilley AV. Ultrasound-guided rectus sheath block and catheter placement. ANZ J Surg. 2008;78:621–3. doi: 10.1111/j.1445-2197.2008.04592.x. [DOI] [PubMed] [Google Scholar]
- 14.Cornish P, Deacon A. Rectus sheath catheters for continuous analgesia after upper abdominal surgery. ANZ J Surg. 2007;77:84. doi: 10.1111/j.1445-2197.2006.03982.x. [DOI] [PubMed] [Google Scholar]
- 15.Blanco R. Optimal Point of Injection: The Quadratus Lumborum Type I and II Blocks. Anaesthesia. 2013. p. 68. Available from: http://www.respond2articles.com/ANA/forums/post/1550.aspx .
- 16.Sauter AR, Ullensvang K, Niemi G, Lorentzen HT, Bendtsen TF, Børglum J, et al. The Shamrock lumbar plexus block: A dose-finding study. Eur J Anaesthesiol. 2015;32:764–70. doi: 10.1097/EJA.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 17.Kadam VR. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J Anaesthesiol Clin Pharmacol. 2013;29:550–2. doi: 10.4103/0970-9185.119148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Visoiu M, Yakovleva N. Continuous postoperative analgesia via quadratus lumborum block - An alternative to transversus abdominis plane block. Paediatr Anaesth. 2013;23:959–61. doi: 10.1111/pan.12240. [DOI] [PubMed] [Google Scholar]
- 19.Chakraborty A, Goswami J, Patro V. Ultrasound-guided continuous quadratus lumborum block for postoperative analgesia in a pediatric patient. A A Case Rep. 2015;4:34–6. doi: 10.1213/XAA.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 20.Ecoffey C. Regional anaesthesia in children. In: Raj PP, editor. Textbook of Regional Anaesthesia. Philadelphia: Churchill Livingstone; 2002. pp. 379–93. [Google Scholar]
- 21.Kopacz DL, Thompson GE. Celiac and hypogastric plexus, intercostal, interpleural and peripheral neural blockade of the thorax and abdomen. In: Cousins MJ, Bridenbaugh PO, editors. Neural Blockade in Clinical Anaesthesia and Management of Pain. Philadelphia: Lippincott; 1998. pp. 451–85. [Google Scholar]
- 22.Reynolds L, Kedlaya D. Ilioinguinal-iliohypogastric and genitofemoral nerve blocks. In: Waldman SD, editor. Interventional Pain Management. Philadelphia: WB Saunders; 2001. pp. 508–11. [Google Scholar]
- 23.Waldman SD, editor. Atlas of Interventional Pain Management. Philadelphia: Saunders; 2004. Ilioinguinal and iliohypogastric nerve block; pp. 294–301. [Google Scholar]
- 24.Willschke H, Marhofer P, Bösenberg A, Johnston S, Wanzel O, Cox SG, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95:226–30. doi: 10.1093/bja/aei157. [DOI] [PubMed] [Google Scholar]
- 25.Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: Accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth. 2006;97:238–43. doi: 10.1093/bja/ael103. [DOI] [PubMed] [Google Scholar]
- 26.Aveline C, Le Hetet H, Le Roux A. Comparison between ultrasound-guided TAM plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380–6. doi: 10.1093/bja/aeq363. [DOI] [PubMed] [Google Scholar]
- 27.Gofeld M, Christakis M. Sonographically guided ilioinguinal nerve block. J Ultrasound Med. 2006;25:1571–5. doi: 10.7863/jum.2006.25.12.1571. [DOI] [PubMed] [Google Scholar]
- 28.Lee S, Tan JS. Ultrasonography-guided ilioinguinal-iliohypogastric nerve block for inguinal herniotomies in ex-premature neonates. Singapore Med J. 2013;54:e218–20. doi: 10.11622/smedj.2013230. [DOI] [PubMed] [Google Scholar]
- 29.Shanthanna H. Successful treatment of genitofemoral neuralgia using ultrasound guided injection: A case report and short review of literature. Case Rep Anesthesiol. 2014;2014:371703. doi: 10.1155/2014/371703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wipfli M, Birkhäuser F, Luyet C, Greif R, Thalmann G, Eichenberger U. Ultrasound-guided spermatic cord block for scrotal surgery. Br J Anaesth. 2011;106:255–9. doi: 10.1093/bja/aeq301. [DOI] [PubMed] [Google Scholar]
- 31.Birkhäuser FD, Wipfli M, Eichenberger U, Luyet C, Greif R, Thalmann GN. Vasectomy reversal with ultrasonography-guided spermatic cord block. BJU Int. 2012;110:1796–800. doi: 10.1111/j.1464-410X.2012.11099.x. [DOI] [PubMed] [Google Scholar]
- 32.Porzionato A, Macchi V, Stecco C, Loukas M, Tubbs RS, De Caro R. Surgical anatomy of the pectoral nerves and the pectoral musculature. Clin Anat. 2012;25:559–75. doi: 10.1002/ca.21301. [DOI] [PubMed] [Google Scholar]
- 33.Macéa JR, Fregnani JH. Anatomy of the thoracic wall, axilla and breast. Int J Morphol. 2006;24:691–704. [Google Scholar]
- 34.Blanco R. The ‘pecs block’: A novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 35.Pérez MF, Miguel JG, de la Torre PA. A new approach to pectoralis block. Anaesthesia. 2013;68:430. doi: 10.1111/anae.12186. [DOI] [PubMed] [Google Scholar]
- 36.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 37.Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: A novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–13. doi: 10.1111/anae.12344. [DOI] [PubMed] [Google Scholar]
- 38.Tighe SQ, Karmakar MK. Serratus plane block: Do we need to learn another technique for thoracic wall blockade? Anaesthesia. 2013;68:1103–6. doi: 10.1111/anae.12423. [DOI] [PubMed] [Google Scholar]
- 39.Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: A new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18:E421–4. [PubMed] [Google Scholar]
- 40.Moore DC. Anatomy of the intercostal nerve: Its importance during thoracic surgery. Am J Surg. 1982;144:371–3. doi: 10.1016/0002-9610(82)90025-3. [DOI] [PubMed] [Google Scholar]
- 41.Bhatia A, Gofeld M, Ganapathy S, Hanlon J, Johnson M. Comparison of anatomic landmarks and ultrasound guidance for intercostal nerve injections in cadavers. Reg Anesth Pain Med. 2013;38:503–7. doi: 10.1097/AAP.0000000000000006. [DOI] [PubMed] [Google Scholar]
- 42.Peng PW, Narouze S. Ultrasound-guided interventional procedures in pain medicine: A review of anatomy, sonoanatomy, and procedures: Part I: Nonaxial structures. Reg Anesth Pain Med. 2009;34:458–74. doi: 10.1097/AAP.0b013e3181aea16f. [DOI] [PubMed] [Google Scholar]
- 43.Moore DC, Bridenbaugh LD. Intercostal nerve block in 4333 patients: Indications, technique, and complications. Anesth Analg. 1962;41:1–11. [PubMed] [Google Scholar]
- 44.Shanti CM, Carlin AM, Tyburski JG. Incidence of pneumothorax from intercostal nerve block for analgesia in rib fractures. J Trauma. 2001;51:536–9. doi: 10.1097/00005373-200109000-00019. [DOI] [PubMed] [Google Scholar]
- 45.Reissig A, Kroegel C. Accuracy of transthoracic sonography in excluding post-interventional pneumothorax and hydropneumothorax. Comparison to chest radiography. Eur J Radiol. 2005;53:463–70. doi: 10.1016/j.ejrad.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 46.Curatolo M, Eichenberger U. Ultrasound-guided blocks for the treatment of chronic pain. Tech Reg Anaesth Pain Manag. 2007;11:95–102. [Google Scholar]
- 47.Byas-Smith MG, Gulati A. Ultrasound-guided intercostal nerve cryoablation. Anesth Analg. 2006;103:1033–5. doi: 10.1213/01.ane.0000237290.68166.c2. [DOI] [PubMed] [Google Scholar]
- 48.Shankar H, Eastwood D. Retrospective comparison of ultrasound and fluoroscopic image guidance for intercostal steroid injections. Pain Pract. 2010;10:312–7. doi: 10.1111/j.1533-2500.2009.00345.x. [DOI] [PubMed] [Google Scholar]
- 49.Ozkan D, Akkaya T, Karakoyunlu N, Arik E, Ergil J, Koc Z, et al. Effect of ultrasound-guided intercostal nerve block on postoperative pain after percutaneous nephrolithotomy: Prospective randomized controlled study. Anaesthesist. 2013;62:988–94. doi: 10.1007/s00101-013-2253-z. [DOI] [PubMed] [Google Scholar]
- 50.Morris CJ, Bunsell R. Intrapleural blocks for chest wall surgery. Anaesthesia. 2014;69:85–6. doi: 10.1111/anae.12550. [DOI] [PubMed] [Google Scholar]
- 51.Strømskag KE, Minor B, Steen PA. Side effects and complications related to interpleural analgesia: An update. Acta Anaesthesiol Scand. 1990;34:473–7. doi: 10.1111/j.1399-6576.1990.tb03126.x. [DOI] [PubMed] [Google Scholar]
- 52.Scott PV. Interpleural regional analgesia: Detection of the interpleural space by saline infusion. Br J Anaesth. 1991;66:131–3. doi: 10.1093/bja/66.1.131. [DOI] [PubMed] [Google Scholar]
- 53.Dravid RM, Paul RE. Interpleural block - Part 1. Anaesthesia. 2007;62:1039–49. doi: 10.1111/j.1365-2044.2007.05183.x. [DOI] [PubMed] [Google Scholar]
- 54.Dravid RM, Paul RE. Interpleural block - Part 2. Anaesthesia. 2007;62:1143–53. doi: 10.1111/j.1365-2044.2007.05181.x. [DOI] [PubMed] [Google Scholar]
- 55.Sadana N, Mayall M. Interpleural blocks and clotting abnormalities: A case report. Anaesthesia. 2008;63:553. doi: 10.1111/j.1365-2044.2008.05528.x. [DOI] [PubMed] [Google Scholar]
- 56.Lönnqvist PA, Hildingsson U. The caudal boundary of the thoracic paravertebral space. A study in human cadavers. Anaesthesia. 1992;47:1051–2. doi: 10.1111/j.1365-2044.1992.tb04200.x. [DOI] [PubMed] [Google Scholar]
- 57.Batra RK, Krishnan K, Agarwal A. Paravertebral block. J Anaesthesiol Clin Pharmacol. 2011;27:5–11. [PMC free article] [PubMed] [Google Scholar]
- 58.Krediet AC, Moayeri N, van Geffen GJ, Bruhn J, Renes S, Bigeleisen PE, et al. Different approaches to ultrasound-guided thoracic paravertebral block: An illustrated review. Anesthesiology. 2015;123:459–74. doi: 10.1097/ALN.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 59.McDermott G, Korba E, Mata U, Jaigirdar M, Narayanan N, Boylan J, et al. Should we stop doing blind transversus abdominis plane blocks? Br J Anaesth. 2012;108:499–502. doi: 10.1093/bja/aer422. [DOI] [PubMed] [Google Scholar]
- 60.Wilson JM, Germain G, Vaghadia H, Tang R, Sawka A. In-plane ultrasound-guided needle insertion ALONG or ACROSS the visual axis hand positions. Br J Anaesth. 2014;113:717–8. doi: 10.1093/bja/aeu324. [DOI] [PubMed] [Google Scholar]