Abstract
Purpose
Patients with symptoms, but without an identified disease are a challenge to primary care providers. A 22-item measure is introduced and evaluated to offer medical care providers with an instrument to assess and discuss possible deficiencies in resilience resources that may contribute to symptoms without identifiable pathology. This instrument highlights psychosocial and lifestyle resources that serve as buffers to life’s stressors rather than focusing on stress and its related symptoms.
Methods
The measure included items from five resilience domains – relational engagement, emotional sensibility, meaningful action, awareness of self and others, and physical health behaviors (REMAP). Its structure and function were evaluated using two different samples.
Results
Results suggest that scores from the REMAP have reasonable psychometric properties. Higher REMAP scores were predictive of fewer health symptoms in a sample representative of the US population. In a second sample, REMAP was positively associated with perceived resilience, ego strength and mindfulness attention and negatively related to perceived stress, depression, sleep disturbances, and loneliness, providing evidence of convergent and divergent validity. Furthermore, the REMAP scale was sensitive to change following a life style intervention.
Conclusion
This suggests that REMAP can be a useful tool in practice settings for counseling patients with unexplained symptoms. With insight into the biopsychosocial aspect of their symptoms, patients may become more receptive to cognitive behavioral options to improve their resilience resources and lifestyle choices.
Keywords: resilience, symptom management, somatic symptoms, biopsychosocial medicine
Introduction
Patients with somatic symptoms, but without an identified cause are a significant challenge to primary care providers and emergency room personnel [1, 2]. In light of both patient dissatisfaction with the process of evaluating and managing these symptoms [3, 4] and the financial burden to the healthcare system, there is a need for new approaches to symptom management.
Recent theoretical models emphasize the synergetic effects of multiple resiliency systems on health outcomes [5]. Drawing from studies on well-being and biopsychosocial models of illness, we created a new 22-item resilience resources instrument that assessed 5 domains associated with the resilient phenotype (REMAP): Relational engagement (i.e., connectedness with family members and friends), Emotional sensibility (i.e., expressions of a healthy emotional life), Meaningful engagement (satisfaction and meaning in different life domains), Awareness of self and others (i.e., perceptions and reflections that influence how we feel about ourselves and how we relate to others), and Physical health behaviors (i.e., a focus on health promotion via nutrition, exercise, smoking abstinence and sleep). These psychosocial domains have all been independently associated with better health outcomes across both healthy and medically ill individuals [6]. However, no instrument assessing quickly these different domains at once is currently available.
Our intent is to provide medical care providers with an instrument to assess patients’ resilience resources, to alert patients to their strengths, and to share with them possible shortcomings in resilience resources that may manifest in somatic symptoms without identifiable pathology. With insight into the biopsychosocial aspect of their symptoms, patients may become more receptive to cognitive behavioral options to improve their resilience resources and lifestyle choices.
Methods
The psychometric properties were assessed in two different samples. Study 1 is an online study with a large sample approximating the characteristics of the US population. These data were used to explore the internal psychometric properties of REMAP as well as examine how REMAP scores relate to somatic symptoms. Study 2 is a sample drawn from a randomized controlled trial evaluating the effects of two lifestyle interventions on health-related outcomes and provided some initial validity evidence for REMAP scores.
Study 1 Overview
In addition to providing data for examining psychometric properties, this online study evaluated the relationship between the REMAP resilience resources and the likelihood of having one or more health symptoms within 3 months prior to the survey in a sample approximating the US population. Given the greater prevalence of poor health in lower income populations [7–10], we also examined whether a higher REMAP score could act as a buffer to the development of health symptoms among lower income participants (< $30k per year).
Participants were recruited from a panel of consumers maintained by Toluna, which offers samples for web surveys for a fee. The link to the study was distributed via email by Toluna and participants accrued points to qualify for small awards. Quotas were monitored to ensure that the sample approximated the U.S population on key demographic variables. In all, 1120 participants began the survey and 1080 completed all the sections of the survey, which took approximately 15–20 minutes. The analysis reported in this paper is limited to the 1080 participants who completed the survey.
Study 1 Participant Characteristics
The sample consisted of females (55.3%) and males (44.7%) who were between 19–75 years of age (M = 43.7, SD = 16.48). The majority of the participants were non-Hispanic Whites (68.7%), with a representation of African Americans (11.5%), Hispanic or Latino (12.7%), Asian (3.8%) and Others (3.3%). One out of two participants was married (50.1%), and one out of four (25.5%) was never married. Divorced, separated and single after the death of a spouse accounted for 10.9% of the sample and 7.5% reported that they were a partner of an unmarried couple. Approximately one out of four (23.8%) participants had an undergraduate degree and 13.4% reported having an advanced degree or post-graduate education. Other participants reported 1 to 3 years of college or technical school (40.8%), GED or high school (19.8%), and less than high school (2.3%). Annual household income ranged from less than 10K to more than $100K, with 29.2% reporting less than 30K, 33.5% reporting 30—60K, 24.5% reporting 60—100K, and 12.8% reporting an income higher than 100K.
Study 1 Procedure
The survey began with a consent page explaining the purpose of the study and expected duration of the survey. To minimize order effects, the order of listing of symptoms was randomized for each participant. Likewise, the order of listing of items in the REMAP scale was randomized for each participant. The study was approved by The Ohio State University Institutional Review Board and data were collected in November and December of 2009.
Study 1 Measures
Symptoms
Common symptoms were obtained from The Ohio State University outpatient clinic symptom review. Participants were asked if they had experienced these symptoms within the last three months. Summary data for symptoms are reported in Table 1.
Table 1.
Common Symptoms Reported by Participants
| Total | Gender | Income | |||
|---|---|---|---|---|---|
|
N=1080 n (%) |
Male n=483 n (%) |
Female n=597 n (%) |
≤ 30K n=312 n (%) |
> 30K n=755 n (%) |
|
| Fatigue‡ | 689 (63.8) | 282 (58.4)*§ | 407 (68.2) | 224 (71.8)†‖ | 459 (60.8) |
| Sleep problems | 445 (41.4) | 182 (38.1) | 263 (44.1) | 158 (51.0)†‖ | 282 (37.7) |
| Tire easily | 428 (39.7) | 169 (35.0) | 259 (43.5) | 160 (51.3)†‖ | 264 (35.0) |
| Lack of sex drive | 353 (32.8) | 139 (28.8) | 214 (36.0) | 116 (37.4) | 234 (31.1) |
| Pain‡ | 666 (61.7) | 283 (58.7) | 383 (64.2) | 210 (67.5) | 448 (59.3) |
| Back pain | 461 (43.0) | 184 (41.6) | 277 (46.6) | 156 (50.5)†§ | 301 (40.1) |
| Joint discomfort | 435 (40.4) | 200 (41.6) | 235 (39.5) | 147 (47.4)†§ | 282 (37.5) |
| Neck pain | 288 (26.8) | 108 (22.5) | 180 (30.4) | 97 (31.3) | 189 (25.2) |
| Jaw pain | 73 (6.8) | 22 (4.6) | 51 (8.6) | 29 (9.4) | 44 (5.9) |
| GI‡ | 573 (53.1) | 236 (48.9) | 337 (56.4) | 186 (59.6) | 383 (50.7) |
| Heart burn or acid reflux | 292 (27.3) | 138 (28.8) | 154 (26.1) | 91 (32.0) | 191 (25.5) |
| Stomach or abdomen pain | 242 (22.5) | 86 (17.8)*‖ | 156 (26.3) | 80 (25.8) | 162 (21.5) |
| Diarrhea | 204 (19.10 | 96 (20.6) | 106 (17.8) | 63 (20.5) | 140 (18.7) |
| Constipation | 197 (18.3) | 65 (13.5)*‖ | 132 (22.1) | 72 (23.2) | 124 (16.5) |
| Nausea | 185 (17.2) | 62 (12.9)*‖ | 123 (20.6) | 67 (21.6) | 118 (15.7) |
| ENT‡ | 418 (38.7) | 165 (34.2) | 253 (42.4) | 149 (47.9)†‖ | 265 (35.1) |
| Sinus | 359 (33.3) | 143 (29.7) | 216 (36.2) | 126 (40.5)†§ | 230 (30.5) |
| Persistent cough | 153 (14.2) | 57 (11.9) | 96 (16.2) | 58 (18.7) | 93 (12.4) |
| Cardio‡ | 147 (13.6) | 67 (13.9) | 80 (13.4) | 57 (18.3) | 90 (11.9) |
| Chest pain | 85 (7.9) | 43 (9.0) | 42 (7.1) | 39 (12.6)†‖ | 46 (6.1) |
| Heart skipping beats | 82 (7.8) | 32 (6.7) | 50 (8.5) | 27 (8.8) | 55 (7.3) |
Note.
Significant difference by gender after applying Holm’s correction.
Significant difference by income after applying Holm’s correction. All significant differences based on Chi-square tests.
% reporting at least one symptom within cluster.
p ≤ .01,
p ≤ .001.
REMAP
The REMAP scale assesses resilience resources from 5 theoretically-relevant domains: relational engagement (defined by items such as “I attend social functions” and “I feel supported by friends”), emotional sensibility (e.g., “I am optimistic”), meaningful engagement (e.g., “I feel my life has meaning”), awareness of self and others (e.g., “I reflect on my life”), and physical health behaviors (e.g., “I exercise”). The full set of 22 items created to assess each of these 5 domains using behavioral indicators are shown in Table 2. These items were rated on a 4-point Likert scale (1 = Rarely, 2 = Occasionally, 3 = Frequently, 4 = Very Frequently). The total score was averaged a with greater score indicating greater resilience resources.
Table 2.
Ratings of Resilience through REMAP Items
| Total | Gender | Income | |||
|---|---|---|---|---|---|
|
N=1080 M (SD) |
Male n=483 M (SD) |
Female n=597 M (SD) |
≤ 30K n=312 M (SD) |
> 30K n=755 M (SD) |
|
| Relational | |||||
| I feel supported by friends | 2.82 (0.90) | 2.72 (0.90)*§ | 2.91 (0.89) | 2.63 (0.96)†§ | 2.90 (0.86) |
| I attend social functions | 2.24 (0.92) | 2.20 (0.91) | 2.26 (0.93) | 2.01 (0.90)†§ | 2.32 (0.92) |
| I talk with family members | 3.15 (0.87) | 2.95 (0.90)*§ | 3.31 (0.82) | 3.04 (0.94)†§ | 3.19 (0.84) |
| Emotional | |||||
| I laugh | 3.19 (0.77) | 3.12 (0.80) | 3.25 (0.74) | 3.06 (0.82)†§ | 3.25 (0.73) |
| I like myself | 3.05 (0.82) | 3.10 (0.81) | 3.02 (0.83) | 2.89 (0.90) | 3.12 (0.78) |
| I am peaceful | 2.95 (0.82) | 3.00 (0.80) | 2.90 (0.84) | 2.84 (0.86) | 2.99 (0.80) |
| I am optimistic | 2.90 (0.86) | 2.88 (0.86) | 2.91 (0.86) | 2.73 (0.91)†§ | 2.96 (0.82) |
| I relax | 2.81 (0.84) | 2.85 (0.81) | 2.78 (0.86) | 2.79 (0.85) | 2.82 (0.84) |
| Meaning | |||||
| I use my mental ability at work | 3.00 (0.95) | 3.01 (0.91) | 2.98 (0.98) | 2.76 (1.01)†§ | 3.08 (0.90) |
| I feel satisfied by my work | 2.55 (0.97) | 2.52 (0.95) | 2.58 (0.98) | 2.35 (1.01)†§ | 2.64 (0.94) |
| I feel my life has meaning | 2.94 (0.91) | 2.85 (0.92) | 3.01 (0.90) | 2.75 (0.95)†§ | 3.01 (0.88) |
| Awareness | |||||
| I feel in control of my life | 2.76 (0.84) | 2.79 (0.90) | 2.74 (0.88) | 2.54 (0.93)†§ | 2.84 (0.86) |
| I am learning | 3.22 (0.75) | 3.15 (0.75)*§ | 3.27 (0.74) | 3.19 (0.79)†§ | 3.22 (0.74) |
| I reflect on my life | 2.97 (0.82) | 2.87 (0.82)*§ | 3.05 (0.80) | 2.97 (0.84) | 2.96 (0.81) |
| I am a good listener | 3.30 (0.70) | 3.21 (0.73)*§ | 3.37 (0.67) | 3.30 (0.77) | 3.30 (0.67) |
| I pray or meditate | 2.43 (1.12) | 2.17 (1.07)*§ | 2.65 (1.11) | 2.44 (1.11) | 2.42 (1.12) |
| I appreciate nature | 3.32 (0.78) | 3.26 (0.78) | 3.36 (0.78) | 3.32 (0.84) | 3.31 (0.76) |
| I give to or serve others | 2.78 (0.90) | 2.65 (0.89)*§ | 2.89 (0.90) | 2.74 (0.92) | 2.80 (0.90) |
| Physical | |||||
| I eat properly | 2.68 (0.81) | 2.68 (0.82) | 2.69 (0.79) | 2.65 (0.82) | 2.69 (0.80) |
| I exercise | 2.38 (0.99) | 2.41 (0.99) | 2.36 (0.98) | 2.22 (0.99)†§ | 2.44 (0.98) |
| I abstain from smoking | 3.25 (1.21) | 3.23 (1.20) | 3.25 (1.23) | 3.04 (1.30)†§ | 3.32 (1.18) |
| I get refreshing sleep | 2.55 (0.91) | 2.50 (0.91) | 2.59 (0.91) | 2.40 (0.95)†§ | 2.61 (0.89) |
| REMAP total score | 2.89 (.49) | 2.83 (0.48) *§ | 2.93 (0.49) | 2.76 (0.52) †§ | 2.93 (0.47) |
Note. Ratings are on a 4-point scale (1 = rarely, 4 = very frequently).
Significant difference by gender after applying Holm’s correction.
Significant difference by income after applying Holm’s correction. All significant differences based on t-tests.
p ≤ .01,
p ≤ .001.
Study 1 Statistical Analysis
Differences in gender and income (≤ 30K, > 30K) were examined using Chi-squares for symptoms and t-tests for the REMAP items and the Holm-Bonferroni method was used to correct for type I error [11]. Exploratory Factor Analysis with oblimin rotation was used to group symptoms into illness domains. Confirmatory factor analysis (CFA) was used to evaluate the REMAP scale and assess fit. As the CFAs were conducted on categorical data, polychoric correlations were analyzed and diagonally weighted least squares estimation was used [12]. After finding an acceptable measurement model for REMAP, the relationship between REMAP and symptoms was analyzed using a structural equation model (SEM) with maximum likelihood estimation [13]. LISREL 8.7 was used for the CFA and SEM analysis [14] and the cutoff criteria suggested by Hu and Bentler [13] were used.
Study 2 Overview
Faculty and staff from a large Midwestern university participated in a lifestyle intervention in which they were assigned to a mindful meditation arm (n = 93) or a health education arm (n = 93) [15]. Participants completed a series of psychosocial measures at baseline and 8 weeks later after the end of the intervention.
Study 2 Participant Characteristics
The 199 participants had a mean age of 50 (SE = .08) and were predominately female (87.5%), Caucasians (74.5%) and college graduates (65.1 %).
Psychosocial measures
REMAP is described above.
Ego Resilience Measure [16] is a 14-item scale assessing a form of adaptive flexibility evaluated by the ability to adjust one’s level of control according to the circumstances. Greater score are associated with higher flexibility.
Brief Resilience Scale [17] is a 6-item scale assessing the ability to bounce back and recover quickly from stress. Items are rated on a 5-point Likert-type scale with greater score indicating greater resilience.
Mindfulness: The Mindful Attention Awareness Scale (MAAS) is a 15-item scale that measures awareness and attention to what is taking place in the present moment. It is related to and predictive of other self –regulation and well-being instruments [18].
The Perceived Stress Scale (PSS) is a 10-item scale assessing the degree to which situations in life are appraised as stressful [19]. Items are designed to evaluate how overloaded, unpredictable and uncontrollable one finds his or her life. It is the most widely used scale to measure perception of stress.
The Center for Epidemiological Studies Depression (CES-D) evaluated depressive symptoms in the past week [20]. The 20 symptom-related items ask how often one experienced depressive cognitions, affect, and behaviors, e.g., feeling depressed and lonely, disturbed appetite and sleep. The CES-D has excellent psychometric characteristics. Scores of 16 or above reflect clinically significant levels of depressive symptoms.
The Pittsburgh Sleep Quality Index (PSQI) is a self-rated instrument that assesses sleep quality and sleep dysfunction over a one-month interval [21]. It has good diagnostic sensitivity and specificity (a score of 6 or above yields a diagnostic sensitivity of 89.6% and a specificity of 86.5%) in distinguishing good and poor sleep. Greater score indicates more sleep disturbances.
The UCLA loneliness scale has excellent psychometric properties and significant correlations with other measures of loneliness, health and well-being [22].
Results
Study 1
Somatic Symptoms
Exploratory factor analysis on symptoms yielded 5 interpretable factors: Musculoskeletal Pain, Fatigue, Cardiovascular Distress, ENT, and Gastrointestinal Distress (GI). The prevalence of symptoms in the sample by gender and income are presented in Table 1. Significant differences by income were found for sleep problems, fatigue, back pain, joint discomfort, ENT symptoms, sinus, and chest pain. With the exception of three GI symptoms (stomach or abdomen pain, nausea, and constipation) differences by gender were not significant after applying the Holm’s correction for Type 1 error.
REMAP: Measurement Structure
Tables 2 presents the individual REMAP items and their distribution across gender and income. On average, women had higher REMAP scores which appears driven by greater relational and awareness resources. Significant income differences were noted in all facets of the REMAP scale. We split the total sample from Study 1 to allow for exploration and cross-validation. Given the relatively small amount of missing data, we opted for listwise deletion which left us with N=491 and N=494 in the exploration and cross-validation data sets, respectively. We were interested in testing both a 1-factor and 5-factor model. The 1-factor model, which posits a single underlying resiliency construct, fit the data well (RMSEA = 0.08, CFI = 0.96, GFI = 0.98). The 5-factor model also fit well (RMSEA = 0.07, CFI = 0.97, GFI = 0.98), but this is not surprising given the additional parameters being estimated. Looking at the fairly trivial improvement to fit that is achieved with the 5-factor model leads us to prefer a single factor model. The 1-factor model also fit well in the cross-validation sample (RMSEA = 0.07, CFI = 0.96, GFI = 0.98), which further supports the adequacy of a 1-factor model to account for individual’s responses to the REMAP items. Further, correlational analyses indicated that the REMAP total score was a more stable predictor of somatic symptoms across the different symptom factors than the individual facets of the 5-factor model. Coefficient alpha for REMAP scores was 0.895 in the combined Study 1 sample.
REMAP and Symptoms
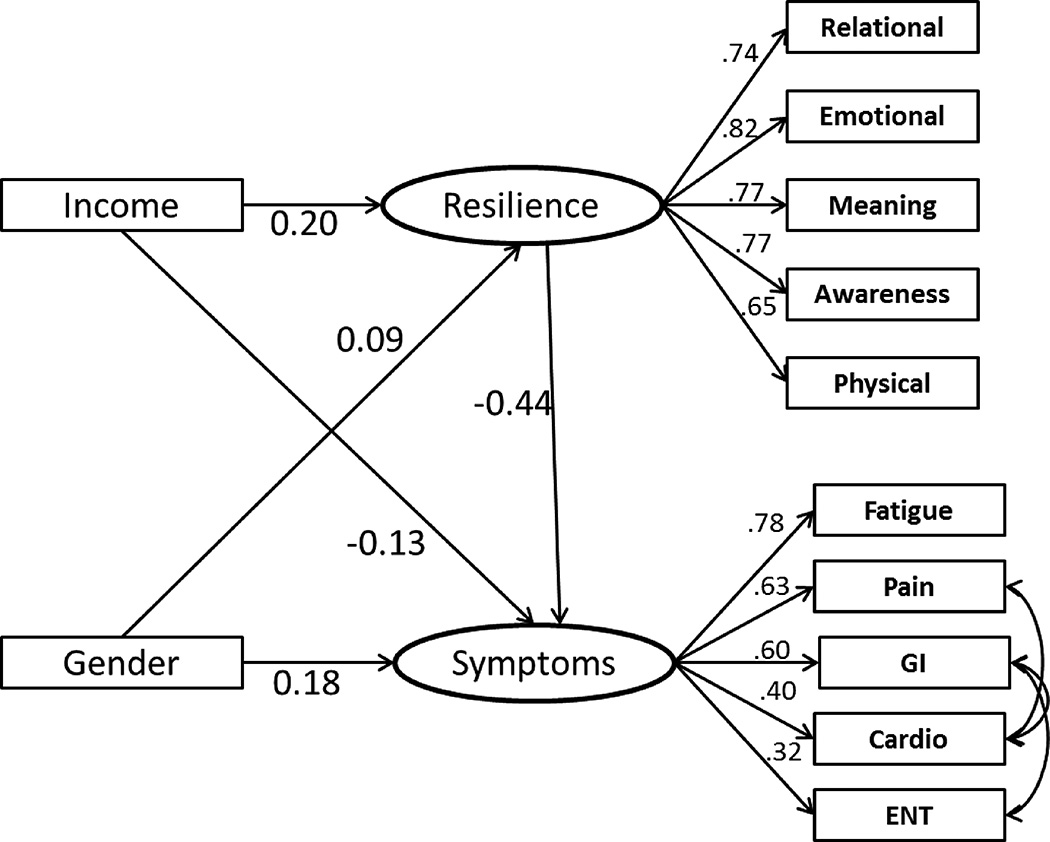
Correlations among the REMAP score and the five symptom factors were examined. All correlations were significant at p < .001 with small to medium effect sizes (see Table 3). A structural equation was then drawn with causal parameters and tested to examine the association between resilience and symptoms of ill health. To control for possible demographic differences, gender and income were added to the structural model as independent predictors of both resilience and physical symptoms and the model fit was acceptable (RMSEA = .07, CFI = .96, GFI =.97).
Table 3.
Pearson Correlations for REMAP Factors and Symptom Clusters
| N=1080 | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. REMAP | ||||||
| 2. Fatigue | −.38* | |||||
| 3. Pain | −.21* | .48* | ||||
| 4. GI | −.24* | .44* | .40* | |||
| 5. ENT | −.13* | .23* | .29* | .29* | ||
| 6. Cardio | −.16* | .30* | .27* | .34* | .16* | |
| M | 2.89 | 1.14 | 1.17 | 1.03 | 0.47 | 0.15 |
| SD | 0.49 | 1.06 | 1.17 | 1.27 | 0.65 | 0.41 |
p ≤ .001.
Figure 1 displays the standardized results and a significant relationship between the Resilience construct and Symptoms construct, which was the underlying construct leading to reports of symptoms within the five clusters previously described. The path from Resilience to Symptoms was significant with a standardized coefficient of −0.44, which suggests that for one standardized unit change in Resilience, a decrease in .44 standardized units in Symptoms can be expected, after controlling for the effects of gender and income.
Figure 1. Parameter Estimates for a SEM Predicting Symptoms from Resilience.
Gastro-Intestinal, ENT = Ear, Nose, Throat. Parameters are fully standardized estimates from LISREL. For Income (0 = less than or equal to 30K, 1 = more than 30K) and Gender (0 = Males, 1 = Females), the dichotomous variable is not standardized. All parameter estimates are standardized and significant at p ≤ .001. Model fit: RMSEA = .065, CFI = .96, GFI = .97. The three correlated errors shown as curved arrows were 0.09, 0.10, 0.11.
Study 2 Results
Participants had a mean REMAP score of 2.79 (SD = .42) at baseline. The internal consistency of the REMAP scale was evaluated using the Cronbach’s alpha statistics. At baseline, the alpha was .85, indicating that scale items show an adequate degree of inter-correlations among each other.
There was a significant correlation between the 2 time points assessed 8 weeks apart, r = .80, p < .001. While there was an intervention conducted between these time points, thus making it unusual from a test-retest reliability standpoint, one could argue that to the extent the intervention had an effect on the time 2 data these would be expected to weaken, not strengthen, this relationship. Furthermore, as expected, there was a small, but significant increase in REMAP scores from pre- to the post-intervention, F (1, 162) =4.35, p =.04, η2 = .03.
The convergent and construct validity of the REMAP scale was examined by computing correlations between baseline REMAP scores and other resilience-related measures. REMAP was positively correlated with the Ego Resilience Measure (r = .55, p < .001, n = 190), Brief Resilience Scale (r = .48, p < .001, n = 190), and the Mindful Attention Awareness Scale (r = .49, p < .001, n = 174). The medium effect sizes of the correlations between the REMAP scores and other resilience measures indicate that REMAP is assessing both common and unique aspects of resilience resources.
Furthermore, evidence for discriminant validity was gathered by correlating REMAP scores with a range of psychological functioning variables. REMAP scores were negatively correlated with the CES-Depression Scale (r = −.36, p < .001, n = 183), UCLA Loneliness Scale (r = −.62, p < .001, n = 174), Pittsburgh Sleep Quality Index (r = −.37, p < .001, n = 182), and Perceived Stress Scale (r = −.20, p = .007, n = 183)1. In summary, the findings from this study suggest that REMAP produces scores with adequate internal consistency, stability over time, and with positive initial evidence regarding convergent and discriminant validity.
Discussion
The REMAP instrument presented in this paper highlights psychosocial and lifestyle resources that serve as buffers to life’s stressors rather than focusing on stress and its related symptoms. Analyses conducted here suggest that the REMAP scale measures a single resilience resources construct and has adequate psychometric properties. Importantly, the REMAP score was correlated with reports of recent somatic symptoms and psychological well-being in two different samples. The REMAP scale is thus a promising tool for initiating discussion with patients regarding psychosocial and lifestyle resources and the development of physical symptoms.
Our goal in developing this instrument was to assess theoretically-relevant resilience resources domains. The scale was constructed to intentionally include items from distinct resilience-related domains. Indeed, empirical data support the idea that the presence of multiple resilience systems can buffer against different life stress [23]. The REMAP score was moderately positively correlated with other resilience scales directly assessing the ability to bounce back from adversity and to adapt to life circumstances. This shows that our instrument that focuses on resources that foster resilience is a good complement to other resilience scales found in the literature. Moreover, the REMAP score was sensitive to the effect of lifestyle interventions.
The REMAP items were worded using simple statements easily understandable by a wide range of participants. In this study, there was a higher prevalence of self-reported somatic symptoms among low-income participants, a key marker of low socioeconomic status (SES). However, even among those with lower income, REMAP had a salutary effect on self-reported somatic symptoms. For example, among low income participants, while 70.5% of those in the bottom quartile of REMAP reported sleep problems, only 28.8% from the highest REMAP quartile reported sleep problems. This suggests that REMAP can be used with patients from different SES levels.
This study has several limitations. The validation of an instrument is a complex and involved process which requires many studies and careful consideration. Modern validity theory focuses on the specific uses and inferences of scores and the case that can be made for the reasonableness of each inference/use. This paper focused on the inferences about the total score relating to an individual’s underlying level of resilience resources. Our examination of test-retest reliability included a treatment between assessments, which may cause some under-estimate of what kind of temporal stability one would expect to see. Future studies would be useful to provide a more traditional measure of test-retest reliability as well as to further add to the evidence regarding valid uses of/inference about REMAP scores.
How will the REMAP instrument benefit the health care provider? Numerous health care visits are made because of common symptoms for which no identifiable pathology is found [1, 2]. This leads to a challenge in meeting patient’s expectations and requests [3, 4]. REMAP can be used to discuss with patients resilience resources that have been associated with symptom reporting and other health outcomes. This mini cognitive-behavioral exercise may convey to the patient that the health care provider accepts the reality of the symptoms, but that the relief from the symptom may be more dependent on the patient than on the physician. Though it is often difficult for individuals to remove stress from their lives, they can control the process of building resilience resources to better deal with life challenges. Reframing the symptom landscape from medical testing to encouraging individuals to actively build resilience in certain life domains should prove beneficial.
Acknowledgments
The project described was supported by Award Number R21AT003670 from the National Center for Complementary and Integrative Health and by the National Center for Research Resources, Grant UL1RR025755 which is now at the National Center for Advancing Translational Sciences, Grant UL1TR001070.
Footnotes
Either due to attrition or missing data, the sample size ranged from 173 to 183.
Conflict of Interest:
William B. Malarkey, MD, Prabu David, PhD, Jean-Philippe Gouin, PhD, Michael C. Edwards, Ph.D., Maryanna Klatt, PhD, and Alex J. Zautra, PhD declare that they have no conflict of interest.
Compliance with Ethical Standards:
Ethical approval:
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent:
Informed consent was obtained from all individual participants included in the study.
References
- 1.Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med. 2001;134(9 Pt 2):917–925. doi: 10.7326/0003-4819-134-9_part_2-200105011-00017. [DOI] [PubMed] [Google Scholar]
- 2.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86(3):262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 3.Hahn SR. Physical symptoms and physician-experienced difficulty in the physician-patient relationship. Ann Intern Med. 2001;134(9 Pt 2):897. doi: 10.7326/0003-4819-134-9_part_2-200105011-00014. [DOI] [PubMed] [Google Scholar]
- 4.Kravitz RL. Measuring patients' expectations and requests. Ann Intern Med. 2001;134(9 Pt 2):881. doi: 10.7326/0003-4819-134-9_part_2-200105011-00012. [DOI] [PubMed] [Google Scholar]
- 5.Puterman E, Epel ES, Lin J, Blackburn EH, Gross JJ, Whooley MA, Cohen BE. Multisystem resiliency moderates the major depression-telomere length association: findings from the Heart and Soul Study. Brain Behav Immun. 2013;33:65–73. doi: 10.1016/j.bbi.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zautra AJ, Arewasikporn A, Davis MC. Resilience: Promoting well-being through recovery, sustainability, and growth. Research in Human Development. 2010;7(3):221–238. [Google Scholar]
- 7.Chen E. Impact of socioeconomic status on physiological health in adolescents: An experimental manipulation of psychosocial factors. Psychosom Med. 2007;69(4):348–355. doi: 10.1097/PSY.0b013e3180592b20. [DOI] [PubMed] [Google Scholar]
- 8.Feinglass J, Lin S, Thompson J, Sudano J, Dunlop D, Song J, Baker DW. Baseline health, socioeconomic status, and 10-year mortality among older middle-aged Americans: Findings from the Health and Retirement Study: 1992–2002. J Gerontol B Psychol Sci Soc Sci. 2007;62(4):S209–S217. doi: 10.1093/geronb/62.4.s209. [DOI] [PubMed] [Google Scholar]
- 9.Gianaros PJ, Manuck SB. Neurobiological pathways linking socioeconomic position and health. Psychosom Med. 2010;72(5):450–461. doi: 10.1097/PSY.0b013e3181e1a23c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trumbetta SL, Seltzer BK, Gottesman II, McIntyre KM. Mortality predictors in a 60-year follow-up of adolescent males: Exploring delinquency, socioeconomic status, IQ, high-school drop-out status, and personality. Psychosom Med. 2010;72(1):46–52. doi: 10.1097/PSY.0b013e3181bfd7d8. [DOI] [PubMed] [Google Scholar]
- 11.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 12.Wirth RJ, Edwards MC. Item factor analysis: Current approaches and future directions. Psychological Methods. 2007;12:58–79. doi: 10.1037/1082-989X.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 14.Jöreskog KG, Sörbom D. LISREL 8 user's reference guide: Scientific Software. 1996. [Google Scholar]
- 15.Malarkey WB, Jarjoura D, Klatt M. Workplace based mindfulness practice and inflammation: A randomized trial. Brain Behav Immun. 2013;27(1):145–154. doi: 10.1016/j.bbi.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. J Pers Soc Psychol. 1996;70(2):349–361. doi: 10.1037//0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- 17.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: Assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 18.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S. Perceived stress in a probability sample of the United States. In: Oskamp SSS, editor. The social psychology of health. Thousand Oaks, CA, US: Sage Publications, Inc; 1988. pp. 31–67. [Google Scholar]
- 20.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 21.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 22.Russell DW. UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure. J Pers Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 23.Puterman E, Epel E. An intricate dance: Life experience, multisystem resiliency, and rate of telomere decline throughout the lifespan. Soc Personal Psychol Compass. 2012;6(11):807–825. doi: 10.1111/j.1751-9004.2012.00465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]