Abstract
Little is known about how emotion dysregulation (ED) and trauma exposure differentially affect the relationship between abuse in childhood and adult substance use. We examined associations between child abuse, trauma exposure, ED, and current substance use in an already existing dataset. Participants (N = 2,014 adults, 90% African American) had been recruited from an urban hospital for a parent study. Analyses showed that drug and alcohol use was significantly positively correlated with child abuse (emotional, physical, and sexual), later trauma exposure, and ED (all ps < .001). Linear regression showed that exposure to abuse when older than a child was significantly associated with drug and alcohol use independent of child abuse and demographic variables (R 2Δ = .08, p < .001; R 2Δ = .04, p < .001). ED was significantly associated with drug and alcohol use independently of child abuse, nonabuse trauma, and demographic variables (R 2Δ = .02, p < .001; R 2Δ = .04, p < .001). Multiple mediation analyses showed that ED and later trauma exposure accounted for variance in the association between emotional abuse and substance use (p < .001). A better understanding of vulnerabilities to additional traumatization and emotion‐regulation deficits in individuals who have been exposed to child abuse and in addition have comorbid substance use problems may inform treatments that lead to improved outcomes.
Resumen
Regulación Emocional como mediador de la niñez
Poco se sabe acerca de cómo la disregulación emocional (DE) y el trauma afectan diferencialmente la relación entre el maltrato en la infancia y el consumo de sustancias en la adultez. Se examinaron las asociaciones entre el maltrato infantil, la exposición al trauma, la disregulación emocional y el uso de sustancias actual en un conjunto de datos ya existente. Los participantes (N = 2.014 adultos, 90% afroamericanos) habían sido reclutados en un hospital urbano para un estudio parental. Los resultados fueron que las drogas y el alcohol se correlacionaron significativamente con el maltrato infantil (emocional, físico y sexual), exposición a trauma posterior y disregulación emocional (todos los p < .001). La regresión lineal mostró que la exposición al maltrato cuando se es mayor, más que cuando se es niño, se asoció significativamente con uso de drogas y alcohol independiente del maltrato infantil y de las variables demográficas (R2Δ = .08, p < .001; R2Δ = .04, p < .001). La disregulación emocional se asoció significativamente con el consumo de drogas y alcohol, independientemente del maltrato infantil, el trauma no causado por maltrato y las variables demográficas (R2Δ = .02, p < .001; R2Δ = .04, p < .001). Los análisis de mediación múltiples mostraron que la disregulación emocional y la exposición a trauma posterior contribuyeron a la varianza en la relación entre el maltrato emocional y el consumo de sustancias (p < .001). Una mejor comprensión de ambas vulnerabilidades, a la traumatización adicional y al déficit de regulación emocional, pueden dar mejor información a los tratamientos que tienen mejores resultados en los individuos que han estado expuestos a maltrato infantil y, que además, tienen problemas de consumo de sustancias comórbidos.
Traditional Chinese and Simplified Chinese Abstracts by AsianSTSS
標題: 兒時受虐和後期濫用藥物༚情緒失調和創傷經歷的間接影響
撮要: 對於情緒失調(ED)和創傷經歷如何有差別地影響兒時受虐和成年時濫藥之間的關係༌我們仍缺乏了解。本研究透過現有的數據樣本༌檢視兒時受虐、創傷經歷、ED和當前濫用藥物狀況之間的關連。本研究樣本取自一家都市醫院的家長研究(N = 2,014 名成人, 90.0% 為非裔美國人)。研究發現༌濫用藥物和酒精跟兒時受虐༈情緒、身體及性虐待༉、後來的創傷經歷、和ED有顯著關連(全部 ps < .001)。線性迴歸法反映༌在童年過後受虐跟濫用藥物和酒精有顯著關連༌並不受兒時受虐情況和人口變量影響(R2Δ = .08, p < .001; R2Δ = .04, p < .001)༛ED跟濫用藥物和酒精有顯著關連༌並不受兒時受虐情況、非受虐創傷和人口變量影響(R2Δ = .02, p < .001; R2Δ = .04, p < .001)。多重中介分析顯示༌ED和後來創傷經歷能解釋情緒虐待和濫藥之間關連的方差(p < .001)。若我們能多加了解兒時受虐及有共病濫藥問題的人士༌其對額外創傷及情緒調節障礙的脆弱度༌可能有助提升治療效果。
标题: 儿时受虐和后期滥用药物༚情绪失调和创伤经历的间接影响
撮要: 对于情绪失调(ED)和创伤经历如何有差别地影响儿时受虐和成年时滥药之间的关系༌我们仍缺乏了解。本研究透过现有的数据样本༌检视儿时受虐、创伤经历、ED和当前滥用药物状况之间的关连。本研究样本取自一家都市医院的家长研究(N = 2,014 名成人, 90.0% 为非裔美国人)。研究发现༌滥用药物和酒精跟儿时受虐༈情绪、身体及性虐待༉、后来的创伤经历、和ED有显著关连(全部 ps < .001)。线性回归法反映༌在童年过后受虐跟滥用药物和酒精有显著关连༌并不受儿时受虐情况和人口变量影响(R2Δ = .08, p < .001; R2Δ = .04, p < .001)༛ED跟滥用药物和酒精有显著关连༌并不受儿时受虐情况、非受虐创伤和人口变量影响(R2Δ = .02, p < .001; R2Δ = .04, p < .001)。多重中介分析显示༌ED和后来创伤经历能解释情绪虐待和滥药之间关连的方差(p < .001)。若我们能多加了解儿时受虐及有共病滥药问题的人士༌其对额外创伤及情绪调节障碍的脆弱度༌可能有助提升治疗效果。
The devastating effects of child abuse on adult mental health morbidity has been well documented (e.g., Edwards, Holden, Felitti, & Anda, 2003; Herrenkohl, Hong, Klika, Herrenkohl, & Russo, 2013; Horwitz, Widom, Mclaughlin, & White, 2001). One area of particular interest has been substance use disorders (SUDs) because substance use often emerges as a maladaptive strategy used to manage the negative results of trauma exposure, including posttraumatic stress disorder (PTSD) and depression. Childhood abuse has been linked to substance use problems, including both alcohol and illicit drug use with effect sizes ranging from r = .14 to .38 (Dembo, Williams, la Voie, & Berry, 1990; Galaif, Stein, Newcomb, & Bernstein, 2001). Prospective research has shown that individuals abused and neglected as children were approximately 1.5 times more likely to report illicit drug use in the past year compared to healthy, nonabused, nonneglected controls (Spatz Widom, Marmorstein, & White, 2006). Additionally, studies have shown that some adults with SUDs have a long history of abuse as children (Banducci, Hoffman, Lejuez, & Koenen, 2014; Simpson & Miller, 2002).
Research also has suggested a positive association between lifetime exposure to trauma and substance use (Kevorkian et al., 2015; Lawson, Back, Hartwell, Maria, & Brady, 2013). Lawson et al. (2013) studied the traumatic experiences of substance‐dependent individuals, finding that 96.5% of those with SUDs had experienced at least one traumatic event in their lifetime. Additionally, in a longitudinal study of U.S. adults, Kevorkian et al. (2015) found that lifetime exposure to trauma was associated with a greater likelihood of lifetime cannabis use. There is growing evidence to support the view that later trauma exposure may mediate the relationship between exposure to child abuse and later development of psychiatric disorders (Banyard, Williams, & Siegel, 2001; Horwitz et al., 2001). Other studies, however, have suggested that childhood trauma contributes to adult psychopathology above and beyond later adult trauma exposure (Cloitre et al., 2009). Therefore, research suggests that both exposure to childhood abuse and later exposure to trauma can contribute to substance use problems. Consequently, to move the field forward, it is necessary to disentangle the differential impact of child abuse and nonabuse trauma on later substance use. It is also beneficial to identify other risk factors that play a role in the effects of early exposure to trauma.
One important factor that likely also plays a role in increasing risk for the development of substance use problems is emotion dysregulation (ED; Cole, Michel, & Teti, 1994). Emotion regulation is a set of interrelated psychological and physiological processes that allow individuals to modulate feelings, behaviors, and physiological responses to events that elicit emotion (Gross, 1998). Problems with emotion regulation can lead to difficulty managing negative emotional states and impair functioning, affecting one's ability to work, understand and be accepted by others, and enjoy oneself (Gross, 1998; Kulkarni, Pole, & Timko, 2013). ED is common across many psychological disorders including SUDs, and is often seen as a risk factor for both the development and maintenance of psychopathology, including binge eating, depression, and PTSD (Cole et al., 1994; Saxena, Dubey, & Pandey, 2011).
Emotional development occurs throughout infancy and childhood and extensive cross‐sectional and developmental research suggests that exposure to childhood abuse is a strong risk factor for ED in adulthood (Shields, Ryan, & Cicchetti, 2001; Shipman, Zeman, Penza, & Champion, 2000). Emotion regulation strategies in childhood are often developed through interactions with parents and other supportive adults (Bariola, Gullone, & Hughes, 2011; Parke, 1994). When the home environment is harmful or unsupportive (including childhood abuse), children are less likely to be exposed to appropriate emotional labeling, expression, and regulation behaviors often modeled by primary caregivers (Bariola et al., 2011; Parke, 1994). Parental responsiveness and encouragement of emotional expression is associated with positive emotional and social developmental status for children (Roberts & Strayer, 1987). In contrast, growing up in an invalidating environment where appropriate emotional expression is ignored, rejected, or punished can lead to emotion regulation problems (Linehan, 1993). Although individuals with high levels of ED often experience retraumatization in adulthood, studies have shown that childhood abuse is uniquely predictive of ED beyond the effects of adult retraumatization—individuals exposed to additional trauma in adulthood— suggesting a particularly important positive association between them (Cloitre et al., 2009; Kulkarni et al., 2013).
Previous research has also shown a significant connection between SUDs and emotional difficulties (Bonn‐Miller, Vujanovic, & Zvolensky, 2008; Dvorak et al., 2014). These associations may in part be explained by the self‐medication hypothesis of addictive disorders, which posits that substance use happens in response to self‐regulation vulnerabilities including difficulty regulating emotions (Khantzian, 1997). Individuals may experience negative emotions, a lack of resources to help manage those emotions, and as a consequence turn to substances to temporarily relieve the undesirable feeling of negative emotional states (Khantzian, 1997, 2003). Researchers suggest that exposure to traumatic events can elicit negative emotions that persist over time, are difficult for individuals to manage, and potentially lead to using substances to self‐medication (Garland, Pettus‐Davis, & Howard, 2013; Jacobsen, Southwick, & Kosten, 2001). Particularly among individuals who do not have adequate emotion regulation strategies to tolerate strong negative emotions, substance use may become a maladaptive coping mechanism used repeatedly when these emotions arise. Substance use may, in fact, be exacerbated in the presence of multiple traumatic experiences (Lawson et al., 2013).
Because exposure to child abuse increases the risk of ED, and ED may be a vulnerability factor for the development of substance use problems, it is possible that ED could be one pathway through which childhood abuse increases the likelihood of substance use problems as an adult. Cross‐sectional studies in samples with SUD have shown associations between child abuse and ED, with some evidence that emotional abuse in particular may have a strong association (Banducci et al., 2014; Weiss, Tull, Lavender, & Gratz, 2013). Additional exposure to trauma as an adult likely also contributes to substance use on its own and may, especially in combination with ED, create particular risk for problematic substance use behavior (Kevorkian et al., 2015). To our knowledge, there are no studies that have examined the separate roles of ED and later trauma exposure on the relationship between childhood abuse exposure and substance use in adulthood. Furthermore, there have been few studies that have been conducted with inner city, minority civilian populations, which have a particularly high rate of trauma exposure and psychopathology, with 95% of the sample having been exposed to trauma compared to a national average of 75% (Gillespie et al., 2009; Horesh et al., 2015; Sledjeski, Speisman, & Dierker, 2008). The aim of this study was to examine the relationship between the reported severity of childhood abuse, ED, lifetime trauma exposure (excluding abuse), and adult substance use. More specifically, we hypothesized that ED would mediate the relationship between the levels of reported childhood abuse and lifetime alcohol and illicit drug use. We also included overall trauma exposure in study analyses to help us better understand the differential effects of child abuse exposure, other trauma exposure, and ED on substance use. We predicted that ED would have a stronger correlation with substance use than would lifetime trauma exposure, although both would be significantly positively related with lifetime substance use.
Method
Participants and Procedure
Data for the present study were drawn from a completed National Institute of Mental Health‐funded study researching genetic and environmental risk factors for the development of PTSD in a low socioeconomic, primarily African American urban population. In the completed study, participants were recruited from waiting rooms in the pharmacy, the gynecology clinic, and the primary care medical clinic at Grady Memorial Hospital, a publicly funded hospital in Atlanta, Georgia. To be eligible for participation, subjects had to be age 18–65 years, not actively psychotic, and able to give informed consent. After signing the informed consent approved by the Institutional Review Boards of Emory University School of Medicine and Grady Memorial Hospital, an interview was administered with questionnaires regarding trauma history and psychological variables, which took 45–75 min to complete. Participants were compensated for their time. Graduate and undergraduate research assistants were rigorously trained in the administration of questionnaires, with an average of 1–2 months of supervised training and shadowing (see Gillespie et al., 2009, for more details on the study procedure).
The sample consisted of 2,014 individuals (71.9% females, M age = 39.84, SD = 12.40) of which 89.7% self‐identified as African American. The remainder of the racial composition was as follows: White (6.1%), Hispanic/Latino (0.7%), mixed/other (3.5%). The sample was predominantly low income with 74.0% currently unemployed and 61.6% reporting a monthly income of below $1,000. The present study was a secondary analysis of data; participants were only included if they had completed all measures of interest for this study.
Measures
The Childhood Trauma Questionnaire (CTQ) is a 25‐item, validated, reliable self‐report measure of childhood abuse (Bernstein, Stein, Newcomb, Walker, & Pogge, 2003). The CTQ assesses abuse using a Likert‐like scale ranging from 1 = never true to 5 = always true. In the present study, Cronbach's α was .95 for sexual abuse, .83 for physical abuse, and .86 for emotional abuse. This measure was used to assess overall severity of child abuse exposure, with higher scores indicative of more abuse (for sexual abuse, M = 8.12, SD = 5.46, range = 5–25; for physical abuse, M = 8.46, SD = 4.24, range = 5–25, for emotional abuse, M = 8.31, SD = 5.09, range = 5–25). Bernstein and Fink (1998) have established cut scores for none, mild, moderate, and severe physical abuse, sexual abuse, and emotional abuse. We categorized participants as having moderate‐to‐severe emotional abuse (score ≥ 13), physical abuse (score ≥ 10), and sexual abuse (score ≥ 8). Table 1 presents the frequency of each type of abuse.
Table 1.
Frequency Distribution of Exposure to Types of Traumatic Events
| Variable | n | % |
|---|---|---|
| Lifetime trauma exposure | 1,914 | 95.0 |
| Natural disaster | 600 | 29.9 |
| Serious or life‐threatening accident/injury/illness | 1,212 | 60.3 |
| Military combat | 43 | 2.1 |
| Attacked with a weapon | 732 | 36.7 |
| Attacked with a weapon (romantic partner) | 500 | 24.9 |
| Attacked without a weapon | 638 | 31.7 |
| Attacked without a weapon (romantic partner) | 828 | 41.2 |
| Witnessed loved one murdered | 351 | 17.5 |
| Witnessed loved one attacked by weapon | 548 | 27.3 |
| Witnessed someone else attacked by weapon | 632 | 31.5 |
| Witnessed loved one attacked without weapon | 774 | 38.5 |
| Witnessed someone else attacked without weapon | 820 | 40.9 |
| Witnessed violence between parents or caregivers | 724 | 36.1 |
| Moderate/severe abuse | 874 | 43.3 |
| Physical abuse | 493 | 24.5 |
| Sexual abuse | 605 | 30.1 |
| Emotional abuse | 464 | 23.0 |
| ≥ 2 types of abuse | 456 | 22.6 |
The Traumatic Events Inventory (TEI) assesses having been exposed over the lifetime to 17 categories of traumatic events using a yes/no response (see Table 2 for a list of traumas included and prevalence rates; Gillespie et al., 2009). For this study, the TEI was used to measure overall trauma exposure, excluding child abuse. The trauma exposure variable was the sum of the different types of traumatic events experienced or witnessed by the participant (M = 4.73, SD = 2.91, range = 0–15).
Table 2.
Correlations of Emotion Dysregulation, Trauma Exposure, and Substance Use
| Variable | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|
| 1. Lifetime alcohol use | – | |||||
| 2. Lifetime drug use | .61 | – | ||||
| 3. Other trauma exposure | .35 | .44 | – | |||
| 4. Sexual abuse severity | .09 | .13 | .25 | – | ||
| 5. Physical abuse severity | .20 | .21 | .39 | .50 | – | |
| 6. Emotional abuse severity | .21 | .23 | .40 | .57 | .70 | – |
| 7. Emotion dysregulation | .27 | .25 | .26 | .29 | .30 | .41 |
Note. n = 2,014. All coefficients were significant at p < .001.
The Emotional Dysregulation Scale (EDS) is a 12‐item self‐report measure of ED (Bradley et al., 2011; Powers, Stevens, Fani, & Bradley, 2015). Items are rated on a Likert‐like scale from 1 = not true to 7 = very true with higher scores indicating higher ED (M = 39.97, SD = 21.92, range = 12–84). For this study, Cronbach's α was .95.
The Alcohol Use Disorder Identification Test (AUDIT) is an 18‐item scale that queries lifetime and past‐year alcohol use (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Questions in the World Health Organization (WHO) interview version focus on frequency and quantity of drinks consumed (eight items for lifetime and eight items for past year), as well as the social repercussion of drinking (two items). For the present study, only lifetime items were summed as a measure of alcohol use in this sample (M = 11.35, SD = 10.30, range = 0–40). A score ≥ 8 is indicative of hazardous drinking, and 45.3% of participants in this sample met this cutoff (Saunders et al., 1993). The AUDIT lifetime measure had a Cronbach's α of .89.
The Drug Abuse Screening Test (DAST) is a 20‐item measure assessing illicit drug use using a yes/no response (Bohn, Babor, & Kranzler, 1991). Questions are split equally, half examining lifetime drug use and the other half over the past year. For the purposes of the present study, only lifetime substance use responses were summed for a total substance use score (M = 3.66, SD = 2.63, range = 0–10). A score ≥ 6 indicates increased likelihood of a SUD and 24.3% of participants in this sample met this cutoff (Skinner, 1982). The DAST lifetime measure had a Cronbach's α of .80.
Data Analysis
Analyses were performed using SPSS 22 software to test the mediational relationship of childhood trauma, overall trauma exposure (excluding child abuse), and ED on lifetime alcohol and drug use. We first examined the distributions of all key predictor and outcome variables. ED, overall trauma exposure, childhood abuse severity, and substance use were all positively skewed. The level of kurtosis for CTQ sexual and physical abuse (2.14 and 3.42, respectively) was higher than suggested, but transformations could not reduce the nonnormal distributions. Analyses run without these variables of interest remained significant; therefore, the results are presented with these variables included. The level of skewness (range from 0.43 to 1.87), however, fell within the acceptable range (Tabachnick & Fidell, 2007). Descriptive statistics and bivariate correlations were computed. We ran linear regression analyses while adjusting for age, gender, level of education, and household income in all analyses. Finally, mediation analyses were performed with INDIRECT (Preacher & Hayes, 2008) for SPSS, which estimates the multiple mediating effects of a variable conditioned on the effects of other variables in the model. Bootstrapping with 1,000 resamples and 95% confidence intervals (CIs) was used to determine the significance of the mediation effects. Preacher and Hayes (2008) have noted that bootstrapping is a preferred method for interpreting mediation analyses because it does not assume that sampling distributions of the indirect effects are normally distributed. Age, gender, level of education, and household income were adjusted to test the mediation of ED and overall trauma history upon the relationship between emotional abuse, physical abuse, and sexual abuse on substance use outcomes. There were no missing data.
Results
Ninety‐five percent of the sample reported exposure to at least one traumatic event. More than one third (43.3%) also reported exposure to moderate‐to‐severe child abuse. The most common types of trauma reported included serious accident/injury and domestic violence. See Table 1 for prevalence rates across all types of traumas assessed.
Correlation analyses showed that lifetime drug and alcohol use were positively associated with self‐reported exposure to childhood physical, sexual, and emotional abuse severity, overall trauma exposure, and higher levels of ED (p < .001). All child abuse types were positively associated with ED (p < .001). See Table 2 for all correlations among the variables of interest.
Linear regression results (shown in Table 3) with all three types of child abuse included in the model accounted for 7% of the variance in alcohol use (p < .001); in this model only physical and emotional abuse were significantly predictive of higher alcohol use scores (sexual: β = .04, t = 1.37, p = .17; physical: β = .06, t = 2.03, p = .043; emotional: β = .20, t = 6.48, p < .001), beyond the effects of the demographic variables. When other trauma exposure was included in the model, trauma load accounted for 4% of additional variance in alcohol use (p < .001); in this model, only emotional abuse (β = .13, t = 4.10, p < .001) and other trauma exposure (β = .24, t = 10.66, p < .001) was significantly predictive of higher alcohol use scores. When ED was added to the model, it accounted for 4% of additional variance in alcohol use beyond the effect of demographic variables, child abuse, and other trauma load (p < .001). Overall trauma exposure (β = .21, t = 9.36, p < .001) and ED (β = .21, t = 9.83, p < .001) were significantly associated with lifetime alcohol use scores. Emotional abuse was also significantly associated with lifetime alcohol use, but the significance was reduced (β = .06, t = 2.15, p = .032), suggesting potential partial indirect effects of ED and overall trauma exposure on the association between childhood emotional abuse and lifetime alcohol use scores.
Table 3.
Hierarchical Linear Regressions for Alcohol Use and for Drug Use
| Variable | R 2 | R 2 ∆ | F∆ |
|---|---|---|---|
| Alcohol use | |||
| Step 1: Demographic variables | .13 | .13 | 72.39*** |
| Step 2: Child abuse severity | .20 | .07 | 55.03*** |
| Step 3: Lifetime trauma exposure | .24 | .04 | 113.68*** |
| Step 4: Emotion dysregulation | .28 | .04 | 96.56*** |
| Drug use | |||
| Step 1: Demographic variables | .12 | .12 | 64.05*** |
| Step 2: Child abuse severity | .19 | .08 | 62.90*** |
| Step 3: Lifetime trauma exposure | .28 | .08 | 240.17*** |
| Step 4: Emotion dysregulation | .30 | .02 | 52.92*** |
Note. N = 2,014. Demographic variables: Age, gender, education, and household income.
*** p < .001.
Similar results emerged for drug use (see Table 3). When child abuse types were included in the model, they accounted for 8% of the variance in substance use (p < .001); in this model sexual and emotional abuse were significantly predictive of higher substance use scores (sexual: β = .06, t = 2.10, p = .036; emotional: β = .21, t = 6.80, p < .001) and physical abuse was trending toward significance (β = .06, t = 1.87, p = .061). When other trauma exposure was included in the model, trauma load accounted for 8% of additional variance in substance use (p < .001); in this model, only emotional abuse severity (β = .11, t = 3.54, p < .001) and other trauma exposure (β = .35, t = 15.50, p < .001) was significantly predictive of higher substance use scores. When ED was added to the model, it accounted for 2% of additional variance in alcohol use beyond the effect of the demographic variables, child abuse, and other trauma load (p < .001). Overall trauma exposure (β = .32, t = 14.46, p < .001) and ED (β = .16, t = 7.27, p < .001) were significantly associated with lifetime drug use scores. Emotional abuse was also significantly associated with lifetime drug use, but the significance was reduced (β = .06, t = 2.05, p = .040), suggesting potential partial indirect effects of ED and overall trauma exposure on the association between childhood emotional abuse and lifetime drug use scores. In both models, older age (β = .20, p < .001, and β = 0.19, p < .001), male gender (β = −0.21, p < .001 and β = −0.17, p < .001), lower education (β = −0.08, p < .001, and β = −0.07, p = .001), and lower household income (β = −0.06, p = .002, and β = −.08, p < .001) were predictive of higher alcohol and drug use, respectively, in the final model.
Results of the bootstrapping yielded, similar to the regression results, a significant partial indirect effect of both ED symptoms and overall trauma exposure on the relation between childhood emotional abuse severity and alcohol use, F = 324.69, R 2 = 0.60, p < .001, bias‐corrected 95% CI [0.03, 0.04]; and drug use, F = 324.58, R 2 = 0.60, p < .001, bias‐corrected 95% CI [0.12, 0.18] (see Figures 1 and 2, respectively), independent of demographic and other child abuse exposure.
Figure 1.
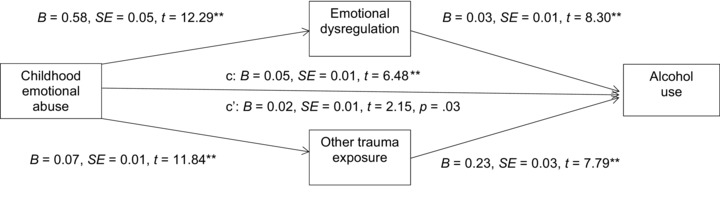
N = 2,014; Multiple mediation model. The indirect effects of emotion dysregulation and trauma exposure on the relation between childhood emotional abuse and alcohol use. **p < .001.
Figure 2.
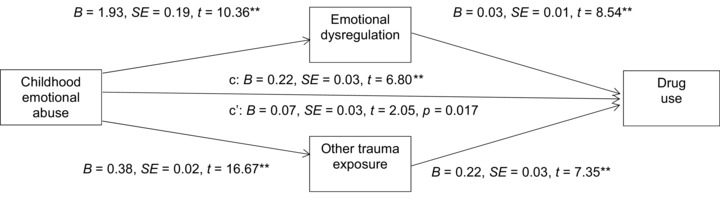
N = 2,014. Multiple mediation model showing the indirect effects of emotion dysregulation and trauma exposure on the relationship between childhood emotional abuse and drug use. **p < .001.
Discussion
This was the first study of which we are aware to examine the separate effects of childhood abuse, lifetime trauma exposure, and ED on lifetime drug and alcohol use in a sample of adults who were highly traumatized and from an urban community. In support of previous research (e.g., Bonn‐Miller et al., 2008; Dvorak et al., 2014; Lawson et al., 2013; Spatz Widom et al., 2006), we found that all forms of childhood abuse, other trauma exposure, and ED were related to lifetime alcohol and drug use. Furthermore, we found that ED and other exposure to trauma indirectly affect the relationship between child emotional abuse and the likelihood of lifetime engagement in substance use in this sample. These findings supported our hypothesis that ED would positively affect the relationship between child abuse exposure and later substance use. Our results also demonstrated, however, that overall exposure to trauma significantly contributed to the risk for substance use, and both exposure to trauma and ED were important factors to consider. In contrast to our predictions, although associations were similar in strength for alcohol use, exposure to trauma was a particularly strong predictor of substance use in comparison to ED, suggesting that finding ways to reduce retraumatization following exposure to child abuse may be a particularly critical step to reduce vulnerability to substance use over the lifetime.
Although all three types of child abuse were significantly associated with alcohol and substance use, our results showed that emotional abuse was significantly related to substance use above and beyond the effects of physical and sexual abuse when other trauma exposure was accounted for in the statistical model. This finding was contrary to some research findings that have showed the particularly detrimental effect of sexual abuse (Kendler et al., 2000; Simpson & Miller, 2002), but it also provided further support of previous research that has identified the importance of emotional abuse on negative mental health outcomes (e.g., Banducci et al., 2014). This finding is helpful to consider in the context of developmental models of emotion regulation and evidence for the detrimental effects of negative family environment and early abuse on mental health outcomes (Cole et al., 1994; Shipman et al., 2000). The presence of emotional abuse may be an indicator of a particularly invalidating, toxic home environment where the primary caregivers are initiating the abuse. Such invalidating environments where emotional expression is often shut down or ignored—as presented in Linehan's (1993) invalidating environment model—can lead to significant difficulty in regulating emotions and consequently lead to various psychological difficulties, including substance use.
These results expanded upon previous studies that have identified the role of ED in substance use to suggest that ED may play an important role in understanding the relationship between child abuse and later substance use. Although it cannot be determined using cross‐sectional data, our results provided some initial evidence that ED may help to explain the relationship between child abuse exposure and later substance use, particularly alcohol use. In line with the self‐medication theory, childhood emotional abuse may hinder the development of healthy emotion regulation skills, which may subsequently result in drug or alcohol use to alleviate emotional distress. It is important to note that the effect sizes for the association between ED and substance use (drug use in particular) were small; therefore, the clinical significance needs to be tested further. Future research should investigate what dimensions of ED may be particularly relevant to substance use and trauma, as this could be a critical next step in determining its usefulness as an intervention strategy and identifying specific treatment targets.
We also found that overall trauma exposure had a significant indirect effect on the relationship between child abuse and lifetime substance use. This may be representative of the risk associated with a cumulative effect of trauma on substance use. More specifically, individuals with increased exposure to traumatic events may resort to substance use as a means of alleviating the long‐term negative effects of trauma exposure (Garland et al., 2013; Khantzian, 1997). Because exposure to multiple traumatic events significantly increases the likelihood of developing trauma‐related disorders, like PTSD and depression, those long‐term effects of trauma exposure may include greater severity of psychiatric symptoms (e.g., reexperiencing symptoms), which then would lead to substance use as a way to avoid such symptoms. These associations may also be exacerbated by a lack of adaptive emotion regulation strategies in the presence of frequent negative emotional experiences. It is also possible that substance use may lead individuals to engage in risky behavior increasing the likelihood of trauma exposure throughout adulthood, as past research has shown substance use is a risk factor for sexual revictimization (Ullman, 2003). Although causal relationships cannot be determined in the present study, due to the indirect impact of ED and later traumatic experiences, it is clear that there was an important relationship between trauma exposure and substance use that pointed to the particular benefit of early interventions with children exposed to maltreatment as a way to reduce the development of SUDs.
It is important to note that we found ED had a stronger indirect effect on alcohol use than drug use. It is unclear why this was the case, but one possibility was that because it is legal, alcohol is often seen as a more socially acceptable drug and easier to obtain. This may lead to initial use, that when coupled with strong negative emotional experiences and inadequate emotion regulation strategies turns into heavier use over time; nevertheless, lifetime trauma exposure (excluding child abuse) was more strongly related to lifetime substance use in our sample. It is possible that increased exposure to traumas results in increased severity of psychiatric symptoms and leads individuals to engage in more extreme drug use to dampen symptoms. It is also possible that substance use may lead individuals to engage in dangerous activities (e.g., walking to find drugs late at night), which increases the risk of retraumatization. Further longitudinal research is needed to better understand the interplay between early traumatization, ED, and later traumatization and when unhealthy substance use begins in that context.
There were a number of limitations of the study. One was the use of retrospective self‐report measures. Given the cross‐sectional nature of this study, we were unable to make assertions about causality, time of onset for ED, trauma exposure, or substance use. Prospective, longitudinal studies are required to examine the temporal course of trauma exposure and psychiatric symptoms to determine if the proposed relationships between ED, later trauma, childhood abuse, and future substance use will be supported by the evidence from such studies. The indirect model presented was also vulnerable to the problem of omitted variables because the mediators were not randomly assigned. In addition, the study utilized screening measures that assessed risky behaviors and symptoms that may be associated with SUDs, but could not provide diagnoses, thus limiting the clinical implications of our results.
The generalizability of our findings was also limited by our sample, which was largely low‐income, minority, and highly traumatized. The benefits of studying risk factors in this sample may have outweighed these limitations. This population is highly understudied and could inform efforts in other understudied and highly traumatized groups. This sample had a 95% rate of exposure to trauma, which is significantly higher than 75% for the general population (Gillespie et al., 2009; Khoury, Tang, Bradley, Cubells, & Ressler, 2010; Sledjeski et al., 2008). The high rate of trauma, paired with lower levels of education and income, very likely puts this population at high risk for mental health issues. The role of the urban environment in compounding these individual level risk factors for mental illness are further propagated by limited access to mental health care, schooling, and steady housing, all of which can lead to a cyclical pattern of trauma exposure (McAllister, Thomas, Wilson, & Green, 2009). Better understanding of the mechanisms of risk on the development of substance use problems could inform and thus aid clinicians in devising treatment plans geared toward substance abuse in at‐risk minority civilian populations.
Overall, our findings suggested that both ED and later traumatization added to our understanding of the relationship between childhood abuse and later substance use. Similar to previous research highlighting the comorbid nature of PTSD and substance use, the effects of exposure to trauma, in particular, emerged as important to both lifetime alcohol and substance use, further highlighting the need for awareness about trauma comorbidity when diagnosing and treating substance use problems (Jacobsen et al., 2001). Incorporating emotion regulation training into SUD treatment protocols may help to enhance effectiveness in the treatment of substance use problems in adults. Ultimately, early intervention following childhood exposure to trauma and training in emotion regulation for at risk youth could help to reduce risk of retraumatization and subsequent increased risk for SUDs.
This work was primarily supported by the National Institute of Mental Health (MH071537; MH100122) and the National Institute of Child Health and Human Development (HD071982). Support also included Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01 RR00039). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government. Amar Mandavia and Gabriella G. N. Robinson contributed equally to the work and are co‐first authors.
References
- Banducci, A. N. , Hoffman, E. M. , Lejuez, C. W. , & Koenen, K. C. (2014). The impact of childhood abuse on inpatient substance users: Specific links with risky sex, aggression, and emotion dysregulation. Child Abuse & Neglect, 38, 928–938. doi:10.1016/j.chiabu.2013.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banyard, V. L. , Williams, L. M. , & Siegel, J. A. (2001). The long‐term mental health consequences of child sexual abuse: An exploratory study of the impact of multiple traumas in a sample of women. Journal of Traumatic Stress, 14, 697–715. doi:10.1023/A:1013085904337 [DOI] [PubMed] [Google Scholar]
- Bariola, E. , Gullone, E. , & Hughes, E. K. (2011). Child and adolescent emotion regulation: The role of parental emotion regulation and expression. Clinical Child and Family Psychology Review, 14, 198–212. doi:10.1007/s10567-011-0092-5 [DOI] [PubMed] [Google Scholar]
- Bernstein, D. P. , & Fink, L. A. (1998). CTQ: Childhood Trauma Questionnaire: A retrospective self‐report. San Antonio, TX: Psychological Corp. [Google Scholar]
- Bernstein, D. , Stein, J. , Newcomb, M. , Walker, E. , & Pogge, D. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect, 27, 169–190. doi:10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Bohn, M. J. , Babor, T. F. , & Kranzler, H. R. (1991). Validity of the Drug Abuse Screening Test (DAST‐10) in inpatient substance abusers: Problems of drug dependence (DHHS Publication No. 92–1888, NIDA Research Monograph, Vol. 119, pp. 233–235). Rockville, MD: U.S. Department of Health and Human Services. [Google Scholar]
- Bonn‐Miller, M. O. , Vujanovic, A. A. , & Zvolensky, M. J. (2008). Emotional dysregulation: Association with coping‐oriented marijuana use motives among current marijuana users. Substance Use & Misuse, 43, 1653–1665. doi:10.1080/10826080802241292 [DOI] [PubMed] [Google Scholar]
- Bradley, B. , DeFife, J. A. , Guarnaccia, C. , Phifer, J. , Fani, N. , Ressler, K. J. , & Westen, D. (2011). Emotion dysregulation and negative affect: Association with psychiatric symptoms. Journal of Clinical Psychiatry, 72, 685–691. doi:10.4088/JCP.10m06409blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M. , Stolbach, B. C. , Herman, J. L. , Kolk, B. V. D. , Pynoos, R. , Wang, J. , & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22, 399–408. doi:10.1002/jts.20444 [DOI] [PubMed] [Google Scholar]
- Cole, P. M. , Michel, M. K. , & Teti, L. O. D. (1994). The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development, 59(2–3), 73–100. doi:10.2307/1166139 [PubMed] [Google Scholar]
- Dembo, R. , Williams, L. , la Voie, L. , & Berry, E. (1990). Physical abuse, sexual victimization and marijuana/hashish and cocaine use over time: A structural analysis among a cohort of high risk youths. Journal of Prison & Jail Health, 9, 13–43. [Google Scholar]
- Dvorak, R. D. , Sargent, E. M. , Kilwein, T. M. , Stevenson, B. L. , Kuvaas, N. J. , & Williams, T. J. (2014). Alcohol use and alcohol‐related consequences: Associations with emotion regulation difficulties. American Journal of Drug and Alcohol Abuse, 40, 125–130. doi:10.3109/00952990.2013.877920 [DOI] [PubMed] [Google Scholar]
- Edwards, V. J. , Holden, G. W. , Felitti, V. J. , & Anda, R. F. (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry, 160, 1453–1460. doi:10.1176/appi.ajp.160.8.1453 [DOI] [PubMed] [Google Scholar]
- Galaif, E. R. , Stein, J. A. , Newcomb, M. D. , & Bernstein, D. P. (2001). Gender differences in the prediction of problem alcohol use in adulthood: Exploring the influence of family factors and childhood maltreatment. Journal of Studies on Alcohol, 62, 486–493. doi:10.15288/jsa.2001.62.486 [DOI] [PubMed] [Google Scholar]
- Garland, E. L. , Pettus‐Davis, C. , & Howard, M. O. (2013). Self‐medication among traumatized youth: Structural equation modeling of pathways between trauma history, substance misuse, and psychological distress. Journal of Behavioral Medicine, 36, 175–185. doi:10.1007/s10865-012-9413-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie, C. F. , Bradley, B. , Mercer, K. , Smith, A. K. , Conneely, K. , Gapen, M. , … Ressler, K. J. (2009). Trauma exposure and stress‐related disorders in inner city primary care patients. General Hospital Psychiatry, 31, 505–514. doi:10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross, J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2, 271–299. doi:10.1037/1089-2680.2.3.271 [Google Scholar]
- Herrenkohl, T. I. , Hong, S. , Klika, J. B. , Herrenkohl, R. C. , & Russo, M. J. (2013). Developmental impacts of child abuse and neglect related to adult mental health, substance use, and physical health. Journal of Family Violence, 28, 191–199. doi:10.1007/s10896-012-9474-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh, D. , Lowe, S. R. , Galea, S. , Uddin, M. , & Koenen, K. C. (2015). Gender differences in the long‐term associations between posttraumatic stress disorder and depression symptoms: Findings from the Detroit Neighborhood Health Study. Depression and Anxiety, 32, 38–48. doi:10.1002/da.22267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz, A. V. , Widom, C. S. , McLaughlin, J. , & White, H. R. (2001). The impact of childhood abuse and neglect on adult mental health: A prospective study. Journal of Health and Social Behavior, 42, 184–201. doi: 10.2307/3090177 [PubMed] [Google Scholar]
- Jacobsen, L. K. , Southwick, S. M. , & Kosten, T. R. (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry, 158, 1184–1190. doi:10.1176/appi.ajp.158.8.1184 [DOI] [PubMed] [Google Scholar]
- Kendler, K. S. , Bulik, C. M. , Silberg, J. , Hettema, J. M. , Myers, J. , & Prescott, C. A. (2000). Childhood sexual abuse and adult psychiatric and substance use disorders in women: An epidemiological and cotwin control analysis. Archives of General Psychiatry, 57, 953–959. doi:10.1001/archpsyc.57.10.953 [DOI] [PubMed] [Google Scholar]
- Kevorkian, S. , Bonn‐Miller, M. , Belendiuk, K. , Carney, D. M. , Roberson‐Nay, R. , & Berenz, E. C. (2015). Associations among trauma, posttraumatic stress disorder, cannabis use, and cannabis use disorder in a nationally representative epidemiologic sample. Psychology of Addictive Behaviors, 29, 633–638. doi:10.1037/adb0000110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian, E. J. (1997). The self‐medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4, 231–244. doi:10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Khantzian, E. J. (2003). The self‐medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry, 10(9), 47–54. [Google Scholar]
- Khoury, L. , Tang, Y. L. , Bradley, B. , Cubells, J. F. , & Ressler, K. J. (2010). Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety, 27, 1077–1086. doi:10.1002/da.20751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni, M. , Pole, N. , & Timko, C. (2013). Childhood victimization, negative mood regulation, and adult PTSD severity. Psychological Trauma: Theory, Research, Practice, and Policy, 5, 359–365. doi:10.1037/a0027746 [Google Scholar]
- Lawson, K. M. , Back, S. E. , Hartwell, K. J. , Maria, M. M. , & Brady, K. T. (2013). A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. The American Journal on Addictions, 22, 127–131. doi:10.1111/j.1521-0391.2013.00319.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan, M. M. (1993). Skills training manual for treating borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- McAllister, C. L. , Thomas, T. L. , Wilson, P. C. , & Green, B. L. (2009). Root shock revisited: Perspectives of early Head Start mothers on community and policy environments and their effects on child health, development, and school readiness. American Journal of Public Health, 99, 205–210. doi:10.2105/AJPH.2005.068569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parke, R. D. (1994). Progress, paradigms, and unresolved problems: A commentary on recent advances in our understanding of children's emotions. Merrill‐Palmer Quarterly, 40, 157–169. [Google Scholar]
- Powers, A. , Stevens, J. , Fani, N. , & Bradley, B. (2015). Construct validity of a short, self‐report instrument assessing emotional dysregulation. Psychiatry Research, 225, 85–92. doi:10.1016/j.psychres.2014.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher , K. J., & Hayes, A. F. (2008). Assessing mediation in communication research. The Sage sourcebook of advanced data analysis methods for communication research, 13–54. doi:10.4135/9781452272054 [Google Scholar]
- Roberts, W. L. , & Strayer, J. (1987). Parents' responses to the emotional distress of their children: Relations with children's competence. Developmental Psychology, 23, 415–422. doi:10.1037/0012-1649.23.3.415 [Google Scholar]
- Saunders, J. B. , Aasland, O. G. , Babor, T. F. , de la Fuente, J. R. , & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction, 88, 791–804. doi:10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Saxena, P. , Dubey, A. , & Pandey, R. (2011). Role of emotion regulation difficulties in predicting mental health and well‐being. SIS Journal of Projective Psychology & Mental Health, 18, 147–154. [Google Scholar]
- Shields, A. , Ryan, R. M. , & Cicchetti, D. (2001). Narrative representations of caregivers and emotion dysregulation as predictors of maltreated children's rejection by peers. Developmental Psychology, 37, 321–337. doi:10.1037/0012-1649.37.3.321 [DOI] [PubMed] [Google Scholar]
- Shipman, K. , Zeman, J. , Penza, S. , & Champion, K. (2000). Emotion management skills in sexually maltreated and nonmaltreated girls: A developmental psychopathology perspective. Development and Psychopathology, 12, 47–62. doi:10.1017/S0954579400001036 [DOI] [PubMed] [Google Scholar]
- Simpson, T. L. , & Miller, W. R. (2002). Concomitance between childhood sexual and physical abuse and substance use problems: A review. Clinical Psychology Review, 22, 27–77. doi:10.1016/S0272-7358(00)00088-X [DOI] [PubMed] [Google Scholar]
- Skinner, H. A. (1982). The Drug Abuse Screening Test. Addictive Behaviors, 7, 363–371. [DOI] [PubMed] [Google Scholar]
- Sledjeski, E. M. , Speisman, B. , & Dierker, L. C. (2008). Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey‐Replication (NCS‐R). Journal of Behavioral Medicine, 31, 341–349. doi:10.1007/s10865-008-9158-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spatz Widom, C. , Marmorstein, N. R. , & Raskin White, H. (2006). Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors, 20, 394–403. doi:10.1037/0893-164X.20.4.394 [DOI] [PubMed] [Google Scholar]
- Sprang, G. (1997). J Psychopathol Behav Assess 19, 257. doi:10.1007/BF02229182 [Google Scholar]
- Tabachnick, B. G. , & Fidell, L. S. (2007). Using multivariate statistics (5th ed.). Boston, MA: Allyn & Bacon/Pearson Education. [Google Scholar]
- Ullman, S. E. (2003). A critical review of field studies on the link of alcohol and adult sexual assault in women. Aggression and Violent Behavior, 8, 471–486. doi:10.1016/S1359-1789(03)00032-6 [Google Scholar]
- Weiss, N. H. , Tull, M. T. , Lavender, J. , & Gratz, K. L. (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37, 944–954. doi:10.1016/j.chiabu.2013.03.014 [DOI] [PubMed] [Google Scholar]


