Abstract
Deficits in executive function (EF) have been proposed as a possible explanation for the “cognitive rigidity” often observed in suicidal individuals. This article provides a systematic review of the existing literature testing relations between EF and suicidality, across various diagnostic and demographic populations, using the influential multidimensional model of EF proposed by Miyake and colleagues (2000) as an organizing framework. Forty-three journal articles on this topic published before January of 2014 were reviewed. Collectively, results from these studies provide tentative support for an association between EF deficits and suicidality. However, there is some evidence that this association is moderated other factors (e.g., suicide attempt lethality). Importantly, this relationship may vary across diagnostic groups. Specifically, more studies that used depressive disorder samples reported some positive findings (75%), followed by mixed diagnostic samples (54%). In contrast, fewer positive findings have emerged from studies with bipolar or psychotic disorder samples (29% and 33% respectively), and some even found that suicidality is associated with better EF in individuals with psychotic disorders. Firm conclusions about relationships between specific dimensions of EF and/or aspects of suicidality are difficult to draw this time. Limitations of the existing literature and corresponding directions for future research are discussed.
Keywords: suicidality, suicide attempt, executive function, inhibition, shifting, updating
Despite major advances in the available options to treat mental health problems over the last several decades (e.g. cognitive-behavioral therapies, new psychotropic medications), rates of suicide (i.e., intentional self-inflicted death) have not decreased appreciably (see Centers for Disease Control and Prevention [CDC], 2014 and Kessler et al., 2005). At least in part, this discrepancy highlights the need to develop a better understanding of factors that contribute to risk for suicide (see Nock et al., 2008). To achieve this, we need more and stronger research on what makes people attempt to end their own lives, prepare to do so, and/or think about doing so (which we collectively refer to as ‘suicidality’ throughout this review), beyond these phenomena simply being considered consequences (or even symptoms) of mental illness.
For several decades, clinicians and theorists have argued that suicidal individuals are characterized by “cognitive rigidity” (e.g., Neuringer, 1964; Patsiokas et al., 1979). However, given the abstractness of this construct, it has been conceptualized and operationalized in a variety of different ways (King et al., 2000). As a result, this idea has proven difficult to evaluate scientifically, and early empirical findings were mixed (see Arffa, 1983 for a review). Drawing upon cognitive and neuropsychological theories and research, some now argue that this apparent rigidity could reflect deficits in executive function (EF; e.g., see King et al., 2000 and Keilp et al., 2001). In fact, cognitive deficits in domains such as EF have been proposed as candidate “endophenotypes” for research on the genetics of suicide (Mann et al., 2009).
Broadly speaking, EF involves the effortful guidance of behavior towards some sort of goal state (Banich, 2009). But the pursuit of goals can be quite complex, and in fact research and theorizing suggests that EF is multidimensional (e.g., Baddeley, 1996; Burgess et al., 1998; Fisk & Sharp, 2004; Kerns et al., 2008). According to a highly influential model/framework proposed by Miyake and colleagues (e.g., Miyake, Friedman, Emerson, Witzki, & Howerter, 2000), which was developed based on an extensive review of the EF literature as well as sophisticated psychometric research, goal-oriented behavior relies heavily upon three distinguishable abilities or “functions”: 1) avoiding/suppressing habitual or “pre-potent” responses (i.e., inhibition); 2) switching between tasks or mental “sets” (i.e., shifting); and 3) monitoring/controlling the contents of working memory (i.e., updating). These abilities regulate lower-order cognitive processes (e.g., perception, motor responses), are particularly important in non-routine situations, and rely heavily upon the prefrontal cortex (see Alvarez & Emory, 2006 and Banich, 2009). Further, there is emerging evidence that individual differences in these abilities have important and wide-reaching psychological and behavioral consequences (see Miyake & Friedman, 2012).
There are several reasons why deficits in EF might contribute to suicide risk. Generally speaking, EF deficits can lead to a wide range of difficulties regulating one’s emotions, thoughts, and actions, which in turn might culminate in suicidal thinking and/or behavior. For example, people with deficits in EF (and perhaps specifically, in shifting) may have more difficulty controlling thoughts about self-harm and/or switching to more positive or adaptive forms of coping in response to stress. In line with this idea, suicidality is associated with the tendency to ruminate (e.g., Miranda et al., 2007) and impaired social problem solving (e.g., Pollock & Williams, 2004), as are EF deficits (e.g., Davis & Nolen-Hoeksema, 2000; Muscara et al., 2008). Also, deficits in EF (and perhaps specifically, in updating) may lead to difficulty retrieving memories of episodes from the past (e.g., Williams, 2006), which in turn leads to difficulty imagining possible future outcomes (see Williams et al., 1996) and thus might contribute to hopelessness (a robust predictor of suicidal behavior; see Beck et al., 2006). Further, people with EF (or more specifically, inhibition) deficits might have difficulty resisting the urge to act on thoughts about self-harm when they occur. In fact, both impaired EF and suicidality are associated with difficulties in decision making (e.g., Brand et al., 2007; Jollant et al., 2005) and impulsivity (e.g., Logan et al., 1997; McGirr et al., 2008). Additional indirect evidence to support a relationship between deficits in EF and suicidality include: 1) established EF deficits in a number of different psychological disorders that are associated with increased suicide risk (e.g., depression - Snyder, 2013; schizophrenia - Kerns et al., 2008; see Harris & Barraclough, 1997); and 2) structural and functional abnormalities in the prefrontal cortex associated with suicidality (e.g., Audenaert et al., 2002; Oquendo et al., 2003; see Jollant et al., 2011).
On the other hand, there are also some reasons to predict that EF deficits might not be linked to suicidality, or could even be a protective factor. For example, EF deficits might undermine one’s ability to plan and/or carry out a suicide attempt. Perhaps in line with this reasoning, most evidence suggests that dementia is not associated with a general increase in suicide risk (see Harris & Barraclough, 1997 and Haw et al., 2009; but for some conflicting evidence, see Erlangsen et al. 2008), which is noteworthy given that impaired EF is a diagnostic feature of dementia (APA, 2013). In fact, some have proposed that amongst those with dementia, risk for suicide might be highest in those with preserved EF (e.g., Cohen et al., 1998; see also Haw et al., 2009). Further, there is some evidence that (general) cognitive impairments are not associated with suicide risk in elderly populations (Turvey et al., 2002), and are inversely associated with planning in those who do make a suicide attempt (Conner et al., 2007). Finally, from a methodological standpoint, it is important to consider that any EF deficits observed in suicidal individuals could be linked to the psychological distress/disorders they are experiencing, rather than their suicidality per se (given the well-established links between impaired EF and many forms of psychopathology).
Notably, like EF, suicidality is not a monolithic construct (see Wedig & Weinstock, 2012 and Wenzel, Brown, & Beck, 2007 for discussions). At the broadest level, it can be important to distinguish between suicidal thinking (i.e., ideation) and behavior (e.g., attempted suicide), as these aspects of suicidality may be differentially associated with EF. For example, deficits in inhibition (which have been linked with impaired impulse control; e.g., see Logan et al., 1997) may be associated with suicide attempts, whereas shifting deficits (which have been linked with ruminative thinking; e.g., see Davis & Nolen-Hoeksema, 2000) may be associated with ideation. In fact, even finer distinctions might prove to be important when exploring the relationship between EF and suicidality (e.g., passive vs. active ideation, impulsive vs. planned attempts). Finally, EF deficits may be differentially predictive of attempted suicide and death by suicide.
The goals of this paper are to: 1) review the existing literature that specifically examines the relationship between EF and suicidality, across different diagnostic and demographic groups; and 2) explore whether this relationship might vary across different dimensions of EF (using Miyake and colleagues’ [2000] model as an organizing framework) and/or aspects of suicidality. While some related reviews have been published, they have been broader in scope, narrower in scope, or both (e.g., Jollant et al., 2011; Richard-Devantoy et al., 2014a, 2014b). For example, Richard-Devantoy and colleagues (2014a) recently published a meta-analysis examining neurocognitive deficits associated with suicidality, including (but not limited to) EF deficits. However, this review only examined this relationship in samples of adults with mood disorders, and (because it was a meta-analysis) only included data from behavioral tasks that had been administered in at least three studies. Reviewing work on this topic across diverse samples should foster more definitive conclusions about the proposed link between EF and suicidality (and in turn, whether EF could influence risk for becoming suicidal). Conversely, exploring potential unique links between established domains of EF and/or suicidality will inform theorizing (e.g., about putative mechanisms), and in turn possible clinical applications. Based on the nature and breadth of these research questions as well as our preliminary review of the literature, we expected there to be a great deal of heterogeneity in the studies we would include. Thus, to fully capture and interrogate this heterogeneity, we chose to conduct a systematic qualitative review (as opposed to a quantitative review; i.e., meta-analysis). Nevertheless, information about effect sizes will be presented and discussed when available.
Methods
Literature search process/parameters
We conducted systematic literature searches using PsycINFO and PubMed, combining the search terms “executive function” AND “suicide” OR “suicidal.” To ensure comprehensiveness, we also: 1) searched through reference lists of articles we found; 2) conducted follow-up searches using other words/phrases that are sometimes considered synonymous with EF (e.g., “cognitive control”, “neurocognitive deficits”), as well as specific EF domains (e.g., “inhibition”, “working memory”) and tasks (e.g., “Wisconsin Card Sort”, “Stroop”); and 3) conducted follow-up searches using Google Scholar (given the broad scope of this search engine). Initial searches were conducted in January of 2014, so only articles that were published by this date are included.
Study inclusion/exclusion criteria
Abstracts were reviewed and selected based on items from the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) checklists, which describe information that should be included in reports on empirical studies of this sort. When necessary to collect additional details pertinent to study inclusion/exclusion (discussed more below), Methods sections were examined. Final determinations were made through consensus by the authors.
One inherent challenge in reviewing literature on EF is that this construct has been defined and operationalized in a number of different ways (see Jurado & Rosselli, 2007), and often very broadly. Both for practical purposes and following the Miyake et al. framework, we chose to adopt a relatively narrow operational definition of EF, excluding more basic/automated cognitive functions (e.g., information processing, semantic memory) thought to be regulated by EF. Similarly, we distinguished between EF and other higher-order cognitive processes (which may be supported in part by EF, yet can be considered distinct constructs), most notably decision making and divergent thinking. As a result, we planned to exclude data from tasks designed to measure these other constructs (e.g., Wechsler intelligence and memory scales, the Iowa Gambling Task, the Alternate Uses Test; for evidence to support these decisions, see Ardila et al., 1998, 2000, Gilhooly et al., 2007, Richard-Devantoy et al., 2013a, and Toplak et al., 2010). Importantly, although we drew upon the Miyake et al. model to help us operationalize EF in a precise fashion, we did not limit our review to measures known to tap the dimensions of EF from that framework – rather, we also include other widely accepted measures of EF, such as fluency and tower tasks (following Snyder, 2013, a review paper on EF and depression that also utilized the Miyake framework). Conversely, this guiding framework did lead us to include some performance tasks/indices that are not always conceptualized as measures of EF, such as the color-word Stroop paradigm (sometimes characterized as a selective attention measure) and commission errors from continuous performance tasks (sometimes considered a behavioral measure of impulsivity). Also following Snyder (2013), we only planned to review data from tasks that used emotional neutral stimuli, to avoid confounding EF and emotional processing.
In contrast, we employed a relatively broad operational definition of ‘suicidality’, which included suicidal thinking and behavior of various forms and levels of severity. However, we did not plan to include articles that focused exclusively on individuals who are at risk for suicide (e.g., based on family history; McGirr et al., 2012a) but never engaged in any suicidal thinking or behavior. Further, we did not include studies focused exclusively on non-suicidal self-injury (NSSI; e.g., Fikke et al., 2011), or self-harm more broadly (e.g., Young et al., 2006). Finally, a few articles have explored potential cognitive consequences of specific suicide attempt methods (e.g., carbon monoxide poisoning; Hay et al., 2002), which we did not plan to review primarily since the overarching motivation for our paper was to examine EF as a factor that could influence risk for suicidality.
In summary, to be included in our review, the study needed to: 1) directly assess EF, as operationalized above; 2) collect information about some form of suicidality, as reflected in the measures described or clearly implied in group inclusion criteria; and 3) directly examine and report on the relationship between the two (e.g., correlations between measures, comparisons with an appropriate control group). Consistent with the goals of our paper, we did not plan to exclude studies based on any characteristics of the sample (e.g., age, primary diagnosis).
Follow-up analyses
In support of the secondary goal of our paper, we planned to categorize each EF measure administered in every study (following Snyder, 2013), using available evidence to identify a specific EF dimension within the Miyake et al. framework that it predominantly maps onto (inhibition, shifting, or updating). This allowed us to review and integrate findings within each of these dimensions, in order to explore whether the relationship between EF and suicidality might vary across them, and in a manner that should minimize the influence of task-specific confounds (i.e., “task impurity” – see Miyake et al., 2000). Of note, while we focus on dimensions of EF from the Miyake et al. framework, we also planned to provide sufficient methodological details from each study to permit other follow-up analyses (e.g., applying alternative EF models, focusing on specific EF measures).
We initially considered doing the same with regard to separate aspects of suicidality, but discovered in our preliminary review of the literature that: 1) a bulk of the studies focused exclusively on attempted suicide; and 2) of those that did assess and examine other aspects of suicidality (e.g., suicidal ideation), many did so in such a way that would not facilitate such comparisons (e.g., grouping together individuals with a history of suicide attempts and ideation). Thus, we decided that attempting to systematically examine findings within different aspects of suicidality would not be sufficiently informative at this time.
Results
A flow chart that summarizes our literature search process and results is presented in Figure 1. As shown in this figure, a total of 43 peer-reviewed journal articles published before January of 2014 were located and reviewed (20 identified through our primary searches, and 23 through secondary search processes). Two unpublished dissertations abstracts on the topic were identified (McCarthy, 2002; Wyatt, 2004), along with one book chapter that presented data (Claes et al., 2012) and one journal article not published in English (Gharaipoor et al., 2007). These studies are not included in our review for practical purposes, but careful reading of their abstracts suggested that doing so would not have altered our conclusions in any meaningful way. One article was excluded because it only reported data from an EF task as part of a composite measure of ‘neurobehavioral disinhibition’ (which also included measures of temperament, etc.; Tarter et al., 2004), another combined suicide attempts and NSSI “episodes” (Miller et al., 2012), and one did not provide sufficient details about the neuropsychological assessment to determine if the EF measure met our inclusion criteria (Machado et al., 2011). Of note, just two studies were excluded altogether because they only examined measures that tap (cognitive) constructs we consider distinct from EF (Clark et al., 2011 and Jollant et al., 2005, both of which focused on decision making). However, data from some tasks within a majority of the studies we review below were excluded for this reason (note that many were being used as control measures).
Figure 1.
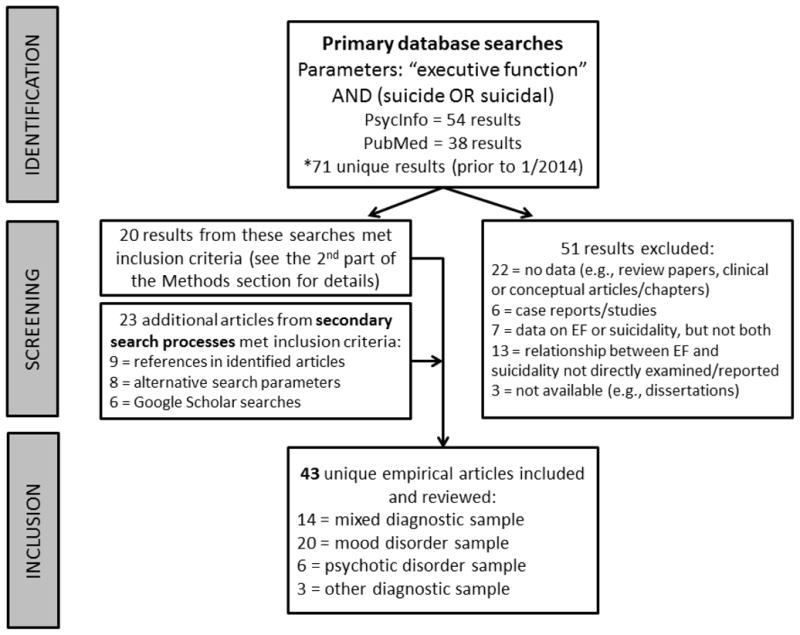
Flow chart summarizing our literature review process and results.
Only two of the studies included in our review were published prior to 2000 (Bartfai et al., 1990; Ellis et al., 1992), highlighting that this is an emerging area of research. Across all of these studies, the most commonly administered measures of EF were the Wisconsin Card Sort Task (WCST, 20 studies [47%]; predominantly measures shifting – see Miyake et al., 2000), the color-word Stroop task (16 studies [37%]; predominantly measures inhibition – see Miyake et al., 2000), and Trails Making Test, Part B (16 studies [37%]; predominantly measures shifting – see Arbuthnott & Frank, 2000). Not surprisingly, a number of studies administered measures of fluency (e.g., verbal fluency, design fluency) – while these tasks are widely used to study EF, they have not been shown to map onto any specific dimension within the Miyake et al. model, and thus were placed into their own category (following Snyder, 2013). Other EF measures administered in these studies that have not been linked to a particular EF dimension and/or seem to measure multiple dimensions were placed into a miscellaneous category – decisions about inclusion/exclusion regarding each of these measures were made carefully (but conservatively, erring on the side of inclusion) based on a review of available psychometric data, examination of task instructions/stimuli, and in one case (Dougherty et al., 2004), consultation with a neuropsychologist.
The key methods (including our categorical coding of each EF measure) and findings from all of these studies are summarized in Table 1 (for more detailed summaries, see Table A.1 in the Appendix). For both practical and substantive reasons, the tables are organized based on the diagnostic makeup of the study sample (as is the rest of this section). However, a number of studies (including some of the earliest ones published) did not focus on a single diagnostic group or category, so findings from these studies are summarized together first.
Table 1.
Summary of study methods and results.
| Study | Sample | EF measure(s) | Suicide measure(s) | Significant Findings |
|---|---|---|---|---|
| Mixed samples | ||||
| Bartfai et al., 1990 | 9 adult men with a recent suicide attempt; control groups = healthy controls (no suicide or psychopathology history; n = 8), chronic pain patients (n = 7) | WCST (S), Stroop (I), COWAT letter & S-a verbal fluency tasks (F), Design Fluency Test (F) | Defined suicide attempts broadly as “purposely inflicted self-harm”; additional details not provided | Attempters scored lower than healthy controls (but not chronic pain patients) on COWAT letter fluency and the Design Fluency Test |
| Ellis et al., 1992 | 20 adults admitted inpatient for self-injurious acts; control group = 27 adults at the same facility with no past suicidality | WCST (S), Trails (S) | Details about assessment of suicidality not provided | Marginal group difference on Trails A, with the suicidal group performing better than controls |
| Horesh, 2001 | 37 adolescents admitted inpatient for a suicide attempt; control group = 23 adolescents admitted for other reasons | CPT (I) | Child Suicide Potential Scale | Suicide attempter group made more commission errors |
| Dougherty et al., 2004 | 50 adults recruited via advertisements - 20 reported one suicide attempt, 10 reported multiple attempts, and 10 had no attempt history | Immediate & Delayed Memory Test (?) | Lifetime Parasuicide Count-2; attempt defined “as a self-harm behavior with a definite intent to die” | Single attempters made more commission errors than controls (on both the immediate and delayed portions of the task), while multiple attempters made the most |
| Raust et al., 2007 | 30 adults who made a suicide attempt but were currently euthymic recruited before discharge from an inpatient facility; control group = 19 healthy adults (no personal or family history of psychopathology) recruited from a blood donation center | Stroop (I), Go/No- go (I), Hayling sentence completion test - part B (I), spatial n-back (U) | Defined as “an attempt by the subject to kill him or herself, resulting in a need for (medical) hospitalization”; additional details not provided | Suicidal patients performed worse than controls on most measures of inhibition, including Hayling test part B, Stroop reaction times, and Go/No-go accuracy (with the exceptions of Hayling errors, Stroop interference, and Go/No-go reaction times), as well as the n-back |
| Ayalon & Litwin, 2009 | 1,712 older adults (national Israeli sample) – 111 reported experiencing passive SI in the past month (dichotomous) | Category fluency (F) | Interview item about passive SI – “in the past month, have you felt that you would rather be dead?” | No significant relationship |
| Dougherty et al., 2009 | 56 adolescents with a history of NSSI – 31 also had made at least one suicide attempt; recruited from any inpatient psychiatric facility | GoStop Task (I) | Lifetime Parasuicide Count-2; Scale for Suicidal Ideation | No significant group differences |
| Andover et al., 2011 | 173 adult male inmates in maximum-security prisons referred for neuropsychological evaluations - 90 reported having made an attempt | Trails (S), COWAT – letter & category (F) | Single interview item - “have you ever tried to kill yourself?” | No significant group differences |
| Burton et al., 2011 | 77 adults recruited from an inpatient facility currently being treated for a suicide attempt (37) or SI (40) | WCST (S), Trails (S), Stroop (I), COWAT – letter & category (F) | Recent SI and behavior confirmed through chart review | Greater Stroop interference predicted attempter status, as did better WCST performance |
| Dour et al., 2011 | 87 adolescents recruited via advertisements; ~60% met diagnostic criteria for at least one psychiatric disorder | DKEFS Tower Task – move-accuracy ratio (?) | Self-Injurious Thoughts & Behaviors Interview - assessed attempts in the past year | EF task performance did not directly predict attempts, but these scores and self-reported emotional reactivity interactively did |
| Miranda et al., 2012 | 45 young adults selected from a larger screening (n = 1011) - 13 participants had made a suicide attempt, while the remaining 32 had not; ~24% met diagnostic criteria for at least one mood or anxiety disorder | WCST (S) | Suicide Behavior Screening (baseline); Scale for Suicidal Ideation used to measure past week SI (at baseline and 6 month follow-up) | No significant difference in perseverative errors between attempters and non-attempters at baseline, but these errors predicted SI at follow-up; also, there was a interaction between perseverative errors and attempt history predicting SI at follow-up |
| Chamberlain et al., 2013 | 304 younger adults recruited through advertisements to participate in a larger study – 45 were considered high risk for suicide (based on reported SI) and 16 had made an attempt | Stop-signal (I) | Suicidality module of Mini International Neuropsychiatric Inventory | No significant group differences |
| Loyo et al., 2013 | 50 adults with symptoms of depression and anxiety - 25 had made a suicide attempt in the past 3 months; control group = 25 volunteers with no distress | WCST (S), Stroop (I), Behavior Rating Inventory of Executive Function, Adult version (S, I, ?) | Self-reported history of suicide attempts (defined as “conscious, self-destructive act carried out with the express intent of dying”); Plutchik Risk of Suicide Scale | Attempt group scored worse than both comparison groups on the BRIEF shifting scale, and worse than healthy controls (but not distressed controls) on Stroop interference and several other BRIEF scales; most of the BRIEF scales were correlated with suicide risk |
| Miranda et al., 2013 | 56 young adults recruited for the 96 who participated in the baseline portion of Miranda et al., 2012 after being contacted again 2–3 years later - 22 reported making an attempt | WCST (completed during baseline for Miranda et al., 2012) (S) | See Miranda et al., 2012 for details about assessment of attempt history; Scale for Suicidal Ideation | WCST perseverative errors significantly predicted SI at the follow-up assessment (2–3 years later); this relationship was partially mediated by brooding rumination |
| Mood disorders | ||||
| King et al., 2000 | 47 older adults with MDD; recruited from inpatient psychiatric facility -18 were admitted for a suicide attempt (excluded those with a past attempt; n = 10) | WCST (S), Trails (S), verbal fluency – ‘F words’, Ruff Figural Fluency Test (F) | Defined attempt broadly as “an intentional self- damaging act”; additional details not provided | No significant group differences but attempter status and age interactively predicted Trails B sequencing, such that attempters got slower with age but nonattempters did not |
| Keilp et al., 2001 | 50 adults currently in an MDE but not on psychotropic medication, recruited through referrals - 29 reported past attempts (15 classified as high lethality); control group = 22 healthy volunteers (no diagnosable pathology) recruited through advertisements | WCST (S), Trails (S), Stroop (I), CPT (I), FAS letter & animal category fluency (F), Baddeley A not B reaction time task (?) | Detailed history of suicidal behavior obtained through a structured interview; attempts rated for severity based on Beck’s medical damage scale, with scores of 5–7 considered ‘high lethality’ | High lethality attempter group scored worse than all 3 other groups across EF measures; follow-up analyses revealed that this pattern held for A not B reaction time; high lethality group also scored worse than low lethality and depressed nonattempters on letter fluency and WCST failure to maintain set, worse than depressed nonattempters on category fluency, and worse than controls on Stroop interference |
| Audenaert et al., 2002 | 20 adults with MDD but no comorbid psychopathology admitted for a suicide attempt in the past week; control group = 20 healthy volunteers (no history of psychopathology or psychotropic medications) | COWAT – letter & category fluency (F) | Details about assessment of suicidality not provided (unclear whether previous attempts were considered) | Suicide attempter group scored worse than controls on both fluency tasks |
| Martinez-Aran et al., 2004 | 108 adults with bipolar I or II disorder recruited from a hospital treatment program – number with past attempts not reported (sample mean = 0.7) | WCST (S), Trails (S), Stroop (I), COWAT – letter & category fluency (F) | Self-reported number of past suicide attempts | No significant correlations between EF scores and past suicide attempts |
| Marzuk et al., 2005 | 53 adults currently in an MDE recruited from an inpatient facility; 25 reported ongoing SI | WCST (S), Trails (S), Stroop (I), COWAT –verbal fluency (F), Five Point Test (F) | Scale for Suicidal Ideation; past suicide attempts assessed via self-report (number, dates, circumstances) | Group with ongoing SI scored worse on Trails B minus A and WCST perseverative errors |
| Swann et al., 2005 | 48 adults with a bipolar disorder, recruited from an inpatient facility - 24 reported at least one suicide attempt | Immediate and Delayed Memory Test (?) | Details of attempt history obtained through clinical records and interviews with participants and significant others | Attempters made more commission errors than non-attempters on the immediate (but not delayed) memory portion of the task; attempters also responded more quickly on the immediate memory portion |
| Harkavy-Friedman et al., 2006 | 51 adults with a bipolar disorder, all with a history of at least one suicide attempt, recruited from outpatient clinics and emergency rooms | Trails (S), Stroop (I), Go/No-go (I), CPT (I), N-back (U), FAS letter fluency (F), Baddeley A not B reaction time (?) | Details about assessment of attempt history not provided – sample was from a treatment study for suicide attempters | All bipolar attempters performed worse than controls on the n-back and go/no-go tasks; also, bipolar II group performed worse than controls on A not B reaction time and letter fluency, and worse than both other groups on Stroop errors |
| Dombrovski et al., 2008 | 32 older adults with a unipolar mood disorder with a suicide attempt or SI serious enough to require hospitalization in the past 3 months; control group = 32 age, gender, and education matched adults with MDD | Executive Interview (EXIT-25) (?) | Suicide item from the Hamilton Rating Scale for Depression; attempts rated for severity using Beck’s medical damage scale | Suicidal group performed worse on the EXIT25; 10 of 32 in suicidal group scored above established cutoff for significant functional impairment, compared to 3 of 32 in the control group |
| Keilp et al., 2008 | 178 adults currently in an MDE but unmedicated; recruited through clinician referrals - 95 reported past attempts (42 had a high lethality attempt); control group = 66 healthy volunteers (no psychopathology) recruited through advertisements | Stroop (with negative priming trials) (I), CPT (I) | Detailed history of suicidal behavior obtained through a structured interview; attempts rated for severity using Beck’s medical damage scale | Stroop interference scores were worse in all the clinical groups relative to controls, and worse in the high lethality attempt group relative to low lethality and depressed nonattempters; Stroop interference was also correlated with SI prior to admission and number of attempts |
| Westheide et al., 2008 | 29 adults with MDD without psychotic features admitted inpatient for a suicide attempt in the past 3 months – 14 had ongoing SI; control group = 29 healthy adults with no past psychiatric problems, recruited through advertisements | Go/No-go (I), delayed alternation task (?) | Suicide attempt characteristics were assessed using the Suicide Intent Scale; lethality of last attempt rated by attending physician; Scale for Suicidal Ideation | Suicidal patients with current SI (but not those without current SI) scored worse than controls on go/no-go gain scores and commission errors |
| Yen et al., 2008 | 96 adults with bipolar I disorder but in remission – 9 had experienced SI or made an attempt in the past year | WCST (S), Trails (S), CPT (I), COWAT (F) | 2 suicide items from the Violence & Suicide Assessment Scale | No significant group differences |
| Malloy-Diniz et al., 2009 | 39 adults with bipolar I disorder, recruited from outpatient clinic - 18 had at least one past suicide attempt; control group = 50 healthy adults matched on age, education level, and IQ | WCST (S), Stroop (I), CPT (I) | Suicide attempt history obtained through semi- structured interview, medical records review, and confirmation from family | No significant differences between those with and without an attempt (though patients scored worse than controls on most measures); number of attempts correlated with Stroop errors, but only on part of the task |
| Dombrovski et al., 2010 | 51 older adults with MDD (but no psychotic features) - 15 had a suicide attempt history, 12 with a history of SI requiring a higher level of treatment; control group = 14 with no diagnosable psychopathology | Stockings of Cambridge test (?) | Current and lifetime suicidality assessed using the SCID, other clinical interviews, review of medical records, and the Scale for Suicidal Ideation | No significant group differences on the EF task |
| Gilbert et al., 2011 | 67 adults with a bipolar disorder, recruited from inpatient and outpatient clinics – 28 categorized as attempters | WCST (S), Trails (S), Stroop (I), letter & category fluency (F) | Prior attempts assessed using the Columbia Suicide History Form | EF factor scores (derived through principle components analysis) did not differentiate groups, nor did individual task performance indices |
| Martino et al., 2011 | 85 adults with bipolar I or II disorder but currently euthymic, recruited from an outpatient treatment clinic - 22 had made at least one attempt | WCST (S), Trails (S), phonological & semantic fluency (F) | Defined an attempt as “a self-damaging act carried out with some intent to die”; assessed using the SCID | No significant group differences |
| Richard-Devantoy et al., 2011 | 20 older adults hospitalized for a current episode of MDD – 10 made a suicide attempt in the past 10 days, excluded those with previous attempts | Trails (S), Stroop (I), Go/No-go (I) | Specific details about assessment of attempt history not provided, though structured interviews (e.g., SCID) were administered | Suicidal group scored worse on the go/no-go task |
| McGirr et al., 2012 | 63 older adults with MDD without psychotic features, recruited from an inpatient facility or outpatient clinic – 34 had made an attempt (14 classified as high lethality); control group = 30 older adults with no history of psychiatric problems or treatment | WCST (S) | Suicide attempt history obtained through chart review, interviews, and confirmation from family; characterized attempts using the Beck Lethality and Suicide Intent Scales | High lethality group performed worse than the other 3 groups on conceptual understanding, and worse than the low-lethality group and controls on total errors and perseverative errors |
| Richard-Devantoy et al., 2012 | 40 older adults in a current MDE, recruited from inpatient facility - 20 had made an attempt in the past 10 days; control group = 20 older adults with no history of depression, suicide attempts, or current psychotropic medications, recruited through advertisements | Trails (S), Rule Shift Cards test (S), Stroop (I), Go/No- go (I), Hayling sentence completion task (I), verbal fluency test (F), Reading With Distraction task (?), Baddeley dual-task performance (?) | Suicide attempt history obtained via the treating psychiatrist, using information obtained during clinical interviews, chart review, and information from family or acquaintances | Attempters performed worse than healthy controls on all of the EF task indices, and worse than depressed controls on go/no-go scores and Stroop errors, as well as some (but not all) indices from the Trails, reading with distraction, rule shift cards, and Hayling tasks; number of attempts correlated with Stroop interference |
| Keilp et al., 2013 | 152 adults currently in an MDE but unmedicated, recruited through clinician referrals - 72 had a past attempts (27 classified as high lethality); control group = 66 healthy volunteers (no diagnosable psychopathology) recruited through advertisements | WCST (S), Trails (S), Stroop (I), CPT (I), Go/No-Go (I), N-back (U), Baddeley A not B reaction time (?) | Prior attempts assessed using the Columbia Suicide History Form; attempts rated for severity based on Beck’s medical damage scale | Attempters performed worse than depressed nonattempters and controls on the n-back and Stroop interference; both depressed groups scored worse than controls on letter and category fluency; Stroop interference correlated with number of attempts and SI prior to admission |
| Richard-Devantoy et al., 2013 | 66 adults with a history of mood disorder(s) who were currently euthymic – 35 had made a serious suicide attempt in the past, while the remaining 31 had not made attempts; control group = 37 adults with no history of mood disorders or suicide attempts | Verbal working memory task (U), semantic & phonemic fluency (F) | Defined an attempt as a” self-injurious act with a clear intent to end one’s own life”, and a serious attempt as one that led to ICU admission or qualified as violent using criteria proposed by Asberg; additional assessment details not provided | Serious suicide attempt group scored lower than both control groups on verbal working memory and semantic fluency; serious attempters also scored worse than healthy controls (but not patient controls) on the phonemic fluency |
| Psychotic disorders | ||||
| Potkin et al., 2002 | 188 adults with schizophrenia or schizoaffective disorder at high risk for suicide (made an attempt in past 3 years or SI with depression or command hallucinations) recruited from a large suicide prevention trial | Trails (S), CPT (I), COWAT verbal fluency (F), category naming (F) | Clinical Global Impression of Severity of Suicidality made by treating psychiatrist; adapted version of the Scale for Suicidal Ideation | No significant correlations between EF performance and lifetime suicide attempts, attempts in the past 36 months, global severity ratings, or recent SI |
| Kim et al., 2003 | 333 adults with schizophrenia recruited from hospital settings - 200 reported an attempt or SI during the course of their illness, and 101 endorsed suicidality in the past month | WCST (S), Consonant Trigram Test (U), COWAT verbal fluency (F), Category Instance Generation (F) | Information about current and lifetime suicidality obtained through a structured clinical interview | Participants with lifetime suicidality scored better on the Consonant Trigram Test, WCST perseverative errors, and Category Instance Generation |
| Nangle et al., 2006 | 78 adults with schizophrenia or schizoaffective disorder, all were currently being treated as outpatients - 28 classified as having at least one past attempt | Trails (S), CPT (I), n-back (U), COWAT verbal fluency (F) | Suicide attempt history obtained using the mood module of the SCID, confirmed through chart review and interviews with family/providers | Attempters scored significantly better than non-attempters on 0-back portion of n-back task, Trails B time, and COWAT verbal fluency; n-back and verbal fluency effects remained significant after controlling for age and positive symptoms |
| Barrett et al., 2011 | 174 adults with a schizophrenia spectrum disorder recruited for a larger translational study – 53 had made an attempt (24 made multiple attempts), 51 reported current suicidality | DKEFS category & set shifting tasks (S), Stroop (I) | Self-reported suicide attempts from SCID; current suicidality assessed using the Inventory of Depressive Symptoms | No significant differences between groups; currently suicidal participants made more DKEFS set- shifting errors, but this effect went away when controlling for current positive symptoms |
| Delaney et al., 2012 | 310 adults with schizophrenia or schizoaffective disorder – 75 had made an attempt, 63 had experienced SI only | CANTAB intra- dimensional/extra- dimensional (S) & spatial working memory (?) tasks | Past and current SI and attempts assessed using the SCID mood module | Combined SI and single attempt group performed better on the CANTAB Intra-dimensional/extra- dimensional but this effect went away when covarying depression |
| Huber et al., 2012 | 152 adults hospitalized during a first episode of psychosis - 28 classified as ‘severely suicidal’ at admission (i.e., hospitalization for imminent suicide risk required) | WCST (S) | Suicidality defined as “SI, intent, or having attempted suicide”; data extracted during a structured file audit | WCST composite (categories completed and perseverative errors) negatively associated with suicidality at admission |
| Other | ||||
| Espinosa et al., 2010 | 42 older adolescents and adults with temporal lobe epilepsy, recruited from an outpatient (epilepsy) clinic – 24 classified as risk for suicide (risk score > 7), and 12 had a suicide attempt | WCST (S) | Plutchik Risk of Suicide Scale | Perseverative errors predicted suicide risk and attempts, as did other and total errors; findings held in regression analyses accounting for disease duration, depression, and family history of psychopathology |
| Homaifar et al., 2012 | 47 adult veterans diagnosed with traumatic brain injury – 18 had made a suicide attempt | WCST (S), Immediate & Delayed Memory Test (?) | Attempt history assessed using the Columbia Suicide History Form | WCST perseverative errors predicted attempter status |
| Legris et al., 2012 | 42 adult women with Borderline Personality Disorder (number who had made suicide attempts not reported); control group = 41 healthy adults | Stroop (I), Stop signal (I) | Suicide Behavior Questionnaire, Revised | Stroop interference was correlated with overall suicide risk and lifetime suicide attempt - remained true in regression analyses which included depression severity |
EF task coding abbreviations: S = shifting, I = inhibition, U = updating, F = fluency, ? = unknown or multiple dimensions
Other abbreviations: CANTAB = Cambridge Neuropsychological Test Automated Battery; COWAT = California Oral Word Association Test; CPT = Continuous Performance Test; DKEFS = Delis-Kaplin Executive Function System; MDD(E) = Major Depressive Disorder (Episode); NSSI = non-suicidal self-injury; SCID = Structured Clinical Interview for DSM Disorders; SI = suicidal ideation; Stroop = Color-Word Stroop; Task Trails = Trails Making Test (A and) B; WCST = Wisconsin Card Sort Task
Mixed diagnostic samples
It is well established that psychological distress/disorders confer risk for suicide (e.g., see Beautrais et al., 1996 and Bertolote et al., 2004). In light of this, 14 of the studies we reviewed examined relations between EF and suicidality in diagnostically heterogeneous groups of individuals receiving psychiatric treatment. It is noteworthy (though expected, given diagnostic base rates) that these samples consisted largely of individuals with unipolar mood (i.e., depressive) disorders, at least among those reporting diagnostic information. Most of these studies used the same basic research design – “cases” were recruited on the basis of having some history of suicidality (usually a past suicide attempt), and control participants were recruited that did not have any history of suicidality. Some but not all of these studies used a psychiatric control group (i.e., individuals with a history of psychiatric difficulties and/or treatment but not suicidality), in addition to (or instead of) “healthy” controls. Only two of these studies (Ayalon et al., 2009; Chamberlain et al., 2013) examined whether EF predicted suicidality in samples that were not initially recruited on the basis of suicidality history. Further, Burton and colleagues (2011) compared EF in inpatients being treated for a recent suicide attempt or suicidal ideation, and thus did not include controls without a history of suicidality (so these results are not included in percentage calculations presented in the next two paragraphs).
Of these (13) studies, 7 (54%) found some evidence that deficits in EF are (significantly) associated with greater suicidality (Bartfai et al., 1990; Dougherty et al., 2004; Horesh, 2001; Loyo et al., 2013; Miranda et al., 2012, 2013; Raust et al., 2007). Not surprisingly, the percentage was somewhat lower when focusing on comparisons with psychiatric controls – specifically, 3 of 8 studies (38%) found evidence for significantly worse EF in patients with suicidality relative to control patients without suicidality (Dougherty et al., 2004; Horesh, 2001; Loyo et al., 2013). Amongst the studies that did not find any evidence for a direct association between EF and suicidality, it is important to note that two had questionable statistical power – specifically, Ellis and colleagues (1992) used a small sample, whereas Chamberlain and colleagues (2013) had a relatively low base rate of participants with significant suicidality histories (e.g., suicide attempts) in their sample. Further, two of these studies (Ayalon et al., 2009; Dougherty et al., 2009) reported group differences that bordered on statistical significance (ps < .1), and one (Dour et al., 2011) found a significant interaction between EF and levels of self-reported emotional reactivity predicting suicide attempts in the past year.
Amongst the studies with positive findings that reported information about effect size(s), the magnitude of the observed relationships varied considerably. More importantly, the majority of these studies reported some null findings – that is, most studies administered multiple measures of EF but only found positive results for some (see Table 1). In order to look for potential patterns in this variability, and in line with the second goal of this review, we examined whether the percentages of studies reporting positive results might differ when focusing on measures of specific EF dimensions (inhibition, shifting, updating, and fluency). Amongst this set of studies (that used mixed diagnostic samples), the percentage with positive results was the same for measures of shifting and inhibition (50%). Fewer (3) studies measured fluency, and only one (Barfai et al., 1990) reported any positive findings on such measures. Finally, only Raust and colleagues (2007) measured updating (using a spatial n-back task) – while they found that participants with a prior suicide attempt performed significantly worse on this task, the effect became non-significant when statistically controlling for self-reported motor impulsivity.
A few studies amongst this set deserve special note. First and foremost, Miranda and colleagues published the only two studies included in our review that examined the relationship between EF and suicidality longitudinally (Miranda et al., 2012; Miranda et al., 2013). Both studies showed that worse performance on the WCST prospectively predicted levels of suicidal ideation in young adults (which the second study showed was partially mediated by rumination). Of note, neither of these studies found a significant association between WCST performance and baseline suicidal ideation, and the two samples were not completely independent. Second, Burton and colleagues (2011) found that performance on some EF tasks differentiated those being treated for a suicide attempt and those being treated for suicidal ideation – specifically, attempters scored worse on the color-word Stroop but better on the WCST. Though preliminary, these findings are consistent with some other evidence that suicidal thinking and behavior can have distinct correlates (see Klonsky & May, 2014), as well as the argument that better EF might be associated with increased risk in certain circumstances. Third, three of these studies used adolescent samples, with mixed results (Dougherty et al., 2009; Dour et al., 2011; Horesh, 2001). Finally, one study (Ayalon et al., 2009) focused on older adults and had a much larger sample than any of the others we reviewed (n = 1,712), but did not yield positive results. However, it is important to note that this study used narrow measures of both EF (a single trial of a category fluency task) and suicidality (a dichotomously scored question about passive suicidal ideation in the past month).
Mood disorder samples
Mood disorders are amongst the strongest diagnostic predictors of suicide risk (e.g., see Chen & Dilsaver, 1996 and Harris & Barraclough, 1997). Thus, it is not surprising that the bulk of the studies we reviewed (20 of 43) examined whether EF is associated with suicidality in samples of individuals suffering from mood disorders. Like those using mixed diagnostic samples, many of these studies seem to have recruited/selected participants based specifically upon suicide attempt history (often during an inpatient hospitalization), though a few used samples that were not recruited in this fashion (comprehensive details about recruitment methods were not provided in all of these articles, and thus specific numbers are not provided here).
Overall, 65% (13 of 20) of these studies reported some evidence for a significant negative relationship between EF and suicidality (Audenaert et al., 2002; Dombrovski et al., 2008; Keilp et al., 2001, 2008, 2013; Harkavy-Friedman et al., 2006; Marzuk et al., 2005; McGirr et al., 2012b; Richard-Devantoy et al., 2011, 2012, 2013b; Swann et al., 2005; Westheide et al., 2008), whereas 56% (10 of 18) reported significantly worse EF in participants with a history of suicidality compared to psychiatric controls (Dombrovski et al., 2008; Keilp et al., 2001, 2008, 2013; Marzuk et al., 2005; McGirr et al., 2012b; Richard-Devantoy et al., 2011, 2012, 2013b; Swann et al., 2005). Again, some of the null findings reported could potentially be attributed to questionable power (e.g., King et al., 2000; Yen et al., 2008), and the observed effect sizes for the positive findings varied considerably (consistent with the effect size heterogeneity reported in a recent meta-analysis by Richard-Devantoy and colleagues [2014a]).
While some of these studies (5) used a mixed mood disorder sample, others only included individuals with unipolar depressive disorder (8) or bipolar disorder (7) diagnoses. Examining the latter studies separately, an interesting (and potentially important) pattern emerged – specifically, the percentage of studies yielding positive results was higher for depressive disorder samples (75% overall, or 57% when focusing on comparisons with psychiatric controls) compared to bipolar disorder samples (29% or 17%). In short, the evidence for a link between EF deficits and suicidality appears stronger in depressive disorders. However, it should be noted that all of the studies that used unipolar samples appear to have selected participants on the basis of suicidality history, whereas 3 of the 7 bipolar studies did not – thus, sampling strategy is a potential confound to consider.
In contrast to those that used mixed diagnostic samples, examining the results separately within different dimensions of EF also yielded a noteworthy pattern in this set of studies. Specifically, there were a higher percentage of positive results for measures of inhibition (67%), relative to measures of shifting or fluency (27% for both). Generally, these patterns seem consistent with meta-analytic results showing a reliable association between suicidality and impaired performance on the color-word Stroop task (which measures inhibition) but not certain measures of shifting or fluency (e.g., the WCST, Trails Making, category fluency) in adults with mood disorders (see Richard-Devantoy et al., 2014a). The results were again encouraging for the dimension of updating, though measures of this dimension were less frequently administered – specifically, only three of these studies measured this construct (Harkavy-Friedman et al., 2006; Keilp et al., 2013; Richard-Devantoy et al., 2013b), all with positive findings.
Again, a few findings from this set of studies deserve some additional discussion. First, several studies found that the relationship between EF and suicidality was moderated by attempt severity/lethality – these studies found that EF deficits were stronger in (and possibly limited to) individuals who had made more serious suicide attempts (Keilp et al., 2001, 2008; McGirr et al., 2012b; Richard-Devantoy et al., 2013b; Swann et al. 2005 – see also Jollant et al., 2005), highlighting potentially important diversity in EF amongst those with a history of suicidality. Similarly, two studies found that EF deficits were linked with suicidal ideation, independent of attempt history (Marzuk et al., 2005; Westheide et al., 2008). Finally, five of these studies focused on (depressed) elderly adults (Dombrovski et al., 2008, 2010; King et al., 2000; Richard-Devantoy et al., 2011, 2012) – the results from these studies were comparable to those using younger adult samples, with 3 of 5 (60%) yielding positive findings.
Psychotic disorder samples
Elevated suicide risk in individuals with chronic psychotic disorders (e.g., schizophrenia, schizoaffective disorder) is well documented (e.g., see Harris & Barraclough, 1997 and Meltzer, 2003), and thus there has been longstanding interest in identifying factors that might predict those who are at risk for suicide amongst these individuals (e.g., Bolton et al., 2007). We found six articles that tested whether EF is associated with suicidality in samples of adults with psychotic disorders. Of note, in contrast to the studies with mixed diagnostic and mood disorder samples reviewed above, none of these studies seemed to use samples initially recruited/selected on the basis of suicidality history. In other words, suicidality appears to have been a secondary outcome in all of these studies, which again should be considered as a possible confound (when comparing the results with those reviewed above).
Only two of these studies (33% - Barrett et al. 2011; Huber et al., 2012) found evidence that EF deficits were significantly associated with increased suicidality. More specifically, both studies found a negative association between recent/ongoing suicidality and performance in the EF domain of shifting. Of note, one of these effects (Barrett et al., 2011) became non-significant when statistically controlling for positive symptoms of psychosis. On the other hand, three studies (50% - Delaney et al., 2012; Kim et al., 2003; Nangle et al., 2006) found some evidence that a history of suicidality was associated with significantly better EF performance (but note that the samples from Delaney et al. and Nangle et al. overlapped). Richard-Devantoy and colleagues (2014b) did not review all of these studies (and were focused on memory), yet observed this same general (divergent) pattern. One study (Kim et al., 2003) tested whether greater insight (i.e., awareness of one’s own condition) might mediate the positive relationship between EF and suicidality, but this hypothesis was not supported. While the small number of studies in this area clearly limits our ability to look more closely at specific dimensions of EF, evidence for this effect (EF being positively associated with suicidality) was reported within the domains of updating (2 of 2 studies), fluency (2 of 3 studies), and shifting (3 of 6 studies), but not inhibition (0 of 3 studies). All of these observed effects were small to medium in size.
Other diagnostic samples
The remaining three articles included in our review examined relations between EF and suicidality in other diagnostic groups known to have an elevated risk of suicide: individuals with temporal lobe epilepsy (see Christensen et al., 2005), traumatic brain injury (see Simpson & Tate, 2007), and Borderline Personality Disorder (see Paris & Zweig-Frank, 2001). All three studies yielded some evidence for a significant negative relationship between EF and suicidality in these populations. Legris and colleagues (2012) found that higher interference scores on the color-word Stroop task were associated with lifetime suicide attempts, suicidal ideation in the past year, and overall suicide risk (based on a composite score of suicidal behaviors) in women with Borderline Personality Disorder. The other two studies reported significantly more perseverative errors on the WCST in participants who had attempted suicide, amongst individuals with temporal lobe epilepsy (Espinosa et al., 2010) and veterans with traumatic brain injuries (Homaifar et al., 2012a) respectively. The effect sizes reported in these three studies were medium to large. Nevertheless, it should be noted that two of these studies also yielded some negative findings. Specifically, Legris and colleagues (2012) did not find a significant association between suicidality and performance on a stop-signal task in their sample, whereas Homaifar and colleagues (2012a) did not find a significant association between attempter status and commission errors on a type of continuous performance task (the Immediate and Delayed Memory Test; developed by Dougherty et al., 2004).
Discussion
The primary goal of this paper was to review the existing evidence for an association between EF and suicidality. We found 43 published, peer-reviewed articles that explored this question – 20 of these used mood disorder samples, 14 used mixed diagnostic samples, six used psychotic disorder samples, and three looked at other diagnostic groups. Collectively, the results of these studies provide tentative support for a link between EF deficits and suicidality, including some evidence that these deficits are not fully accounted for by psychological distress/disorders. However, examining these results separately within different diagnostic groups yielded an intriguing, and potentially very important, pattern. Specifically, the evidence for EF deficits being linked with increased suicidality was strongest in depressive disorder samples, followed by mixed diagnostic samples. In contrast, fewer positive findings emerged from studies that used bipolar and psychotic disorder samples, and some found evidence that suicidality is associated with better EF in those with psychotic disorders. While a few studies found promising evidence for a link between EF deficits and increased suicidality in other high-risk diagnostic populations (e.g., Borderline Personality Disorder), more research is clearly needed on those groups.
Importantly, it is not yet clear whether EF contributes to risk for suicidal thinking or behavior, as the vast majority of the existing research on this topic is cross-sectional. Likewise, there are currently no published studies examining whether EF predicts deaths by suicide. While a secondary goal of our review was to examine whether EF and suicidality might vary across different dimensions/aspects of these constructs, firm conclusions about this are difficult to draw at this time. Overall, results from the existing literature suggest that suicidality may be associated with broad (i.e., general) EF deficits, rather than unique deficits in one or more specific domain(s) of EF, given that some positive findings were reported for measures from all of the EF dimensions we examined (inhibition, shifting, updating, and fluency). There was also some indication that suicidality might be more reliably linked with inhibition deficits (as conceptualized within the Miyake et al. framework), but only in those with mood disorders. Fewer conclusions can be drawn about different aspects of suicidality, since so many of these studies simply compared individuals who had made a past suicide attempt and those who had not (and in fact, the conclusions discussed above may be limited to attempted suicide). However, there is evidence to suggest that attempt seriousness or lethality is important to consider, and perhaps also ongoing suicidal ideation. These lingering questions are closely connected with important limitations of the existing literature, which are discussed next.
Methodological limitations of existing research
Beyond the general need for more research on the topic of EF and suicidality, our review highlights several specific areas that have been relatively understudied (e.g., psychotic disorders, the EF dimension of updating) and warrant further investigation. In planning such work, it is important to ensure that future studies have adequate statistical power – while most studies we reviewed were not underpowered per se, many had sample sizes that were likely constrained by practical considerations, rather than dictated by a priori power analyses. Our hope is that this review will not only inspire more research on EF and suicidality, but also aid investigators in estimating the sample sizes needed to adequately test for hypothesized effects.
Perhaps the most glaring limitation of the existing literature on this topic is that most of the published studies are cross-sectional. Only two (non-independent) studies examined relations between EF and suicidality prospectively, and these studies focused on suicidal ideation – none have tested whether EF prospectively predicts suicidal behavior. Thus, the nature of observed links between EF and suicidality remains unclear (e.g., whether deficits in EF can be considered a risk factor in certain populations), and in turn so do the clinical implications (discussed later). Also regarding the nature of these relationships, though speculations have been made about potential mechanisms involved in observed relationships between EF and suicidality, only a few studies have statistically tested for mediation. Finally, it doesn’t appear any of the studies we reviewed considered or tested for possible non-linear relationships between EF and suicidality (and note that certain sorts of non-linear effects might be masked when comparing group means). In fact, we wonder whether a non-linear relationship (e.g., suicidality increases in the context of mild EF deficits, but decreases in the context of severe ones) could possibly explain the divergent results found in studies that used psychotic disorder samples, if those samples had relatively more severe EF deficits. A simple comparison of samples means from the studies we reviewed does lend some support to this idea, though such comparisons have inherent limitations, and this idea is not clearly supported in the broader literature comparing severity of EF deficits across diagnostic populations (e.g., see Fossati et al., 1999).
As can be seen in Table 1, some studies used simple and potentially biased procedures for collecting data about participants’ suicidality histories (e.g., reviewing medical records, unstructured interviews), while others did not provide important details about their procedures and/or employed very broad definitions of a suicide attempt. Still others used relatively narrow assessments of suicidality, such as one or a few questions from a clinical interview or questionnaire. In short, the reliability and validity of the methods used to assess suicidality is a concern for some studies we reviewed. Along these same lines, many of these studies used the same basic research design, contrasting EF in individuals who had made suicide attempts and those who had not (either psychiatric controls, “healthy” controls, or both). While this sort of methodological consistency can be valuable (e.g., to facilitate comparison and integration of findings), it also limits the conclusions that we can draw about the relationship between EF and other aspects of suicidality (e.g., suicidal ideation, aborted attempts, preparatory behavior).
The use of retrospective designs also raises an important concern regarding this particular research question – specifically, that EF deficits observed in individuals who have made suicide attempts could be the result of (brain) injuries experienced during these attempts. While many studies did take some measures to address this (e.g., excluding those with known brain damage), we would argue that this remains an issue to consider when interpreting data from any studies on attempted suicide that used a retrospective design (e.g., since some brain injuries can be difficult to detect). Also, a number of studies recruited participants who had experienced a recent suicidal crisis and were in intensive (e.g., inpatient) treatment – not only can this limit generalizability, but there is reason to be concerned that recent/ongoing interventions (e.g., certain psychotropic medications) could impact EF. Again, while some studies took measures to address this issue (e.g., excluding those on medications known to impact EF), we would argue that it is another limitation of this widely used study design (since such measures also impact generalizability). Finally, and again related to generalizability, many studies excluded individuals with histories of substance abuse or dependence. While there is a clear methodological rationale for doing this (since substance use can impair cognitive abilities; e.g., see Peterson et al., 1990 and Lundquist, 2005), there is a known and strong link between substance use and suicide risk (e.g., see Harris & Barraclough, 1997 and Schneider, 2009). On this note, we are surprised no published studies have specifically aimed to examine the relationship between EF and suicidality in individuals with substance use disorders, given that EF deficits are hypothesized to play a role in the development of problematic substance use (e.g., Giancola & Tarter, 1999).
In contrast to the methods used to assess suicidality, there was a great deal of variability in the methods used to assess EF within the studies we reviewed – while such methodological heterogeneity also has advantages (e.g., ruling out mono-method bias, testing generalizability), it complicates the interpretation of divergent findings. Also, many studies administered more than one EF measure, raising concerns about inflated risk of Type I error – some studies took measures to address this issue (e.g., using adjusted p-values), but others did not. While it can be argued that different measures tap different dimensions of EF (and thus test different hypotheses), it is important to note that many of the most commonly used tasks in the literature (e.g., the WCST, Trails Making) have been characterized as “complex” or “impure” (see Miyake et al., 2000), in that they rely on multiple cognitive abilities (both executive and non-executive). In turn, this complicates the interpretation of results, particularly efforts to determine if separate dimensions of EF are differentially associated with suicidality. More generally, the interpretation of a single score or performance index is clouded by any sources of variance aside from the construct of interest. We attempted to address this issue in our review by integrating findings from different measures within EF dimensions across studies, but this approach has important limitations (including some ambiguity categorizing specific tasks, particularly given that “complex” tasks were commonly used) – in the next section, we discuss alternative approaches to address this issue (as well as other methodological limitations discuss above).
Future directions for research
Rigorous and comprehensive measurement of EF
As previously mentioned, many widely used EF tasks rely on multiple cognitive abilities – as a result, performance differences can be difficult to interpret. Following work by Miyake and colleagues (2000, 2012), an alternative approach is to use simpler EF measures that were specifically designed to tap a particular dimension of EF. Further, if multiple EF tasks are administered within the same study, it is then possible to create composite or latent EF variables – this can increase statistical power (by reducing method variance), as well as address concerns about inflated risk of Type I errors. Note that our approach in this review (integrating findings from measures across studies) mirrors this, yet has key limitations (e.g., due to potential confounds across studies). Finally, alternatives to traditional performance-based measures of EF should be considered, including self/informant reports of EF and even neuroimaging. In fact, these sorts of measures could be employed as supplements (rather than alternatives) to performance tasks when feasible, and then efforts to incorporate the data into composite/latent variables can be explored.
Rigorous and comprehensive measurement of suicidality
Future research on this topic could also benefit from using cutting-edge methods for assessing suicidality. First and foremost, the use of standardized and structured suicidality measures is critical to ensure reliability and validity of these sorts of data. Further, there is growing acknowledgment that there are a variety of important and distinguishable aspects of both suicidal thinking (e.g., intent, controllability) and suicidal behavior (e.g., aborted or interrupted attempts, preparatory behavior) that can be overlooked if not directly assessed, and that it can sometimes be challenging to distinguish suicidal behavior from NSSI (e.g., see Posner et al., 2007 and Matarazzo et al., 2013). Emerging gold-standards in the field (e.g., the Columbia Suicide Severity Rating Scale, the [Beck] Scale for Suicidal Ideation) reflect the variety, complexity, and nuances of this broad construct, and thus can provide a more rigorous assessment of suicidality (and in turn, test of the relationship between EF and suicidality). A few studies we reviewed did employ these sorts of instruments, but we hope this will become the standard in future research on this topic.
Alternative study designs
In addition measuring EF and suicidality in a comprehensive and rigorous fashion, alternative study designs should be considered. As previously mentioned, a bulk of the existing studies on this topic used a fairly basic retrospective design, comparing individuals who had made suicide attempts and those who had not. A variety of alternative designs can and should be employed in future research, but the approach that we feel would have the most value given the current state of the literature is to conduct prospective studies examining whether EF predicts future suicidal thinking and/or behavior. Of course, in addition to the usual challenges that longitudinal research entails (e.g., difficulties with tracking/attrition), this work would be difficult given the (relatively) low incidence of suicidality in the general population (see Ten Have et al., 2009). Beyond simply extending the length of study follow-ups, there are a variety of sampling approaches that investigators can use to help address this issue, including targeting individuals with prominent risk factors (e.g., major psychiatric disorders, family history of suicide) and/or during high-risk periods (e.g., after discharge from the hospital, after being diagnosed with a major medical problem). On this note, even when the focus of the study is on future suicidality, individuals with past suicide attempts make sense to target as well (since past attempts are strong risk factor for suicide; see Harris & Barraclough, 1997), though longitudinal work on high-risk individuals without past attempts would help rule out the concern that EF deficits might be a consequence (rather than a cause) of suicidal behavior. Finally, it is important to keep in mind the unique ethical challenges that this sort of work would entail, as high-risk individuals cannot be studied in a completely naturalistic fashion. Yet when participants are in active treatment, differences in the type or intensity of this treatment might confound results. There are a variety of ways to address this issue as well (e.g., matching participants on current treatment, using samples that are at elevated risk but do not necessitate active treatment), but one that we feel might be particular worthwhile to consider is to examine whether EF predicts suicidality in the context of controlled clinical trials – this would have direct clinical implications (for predicting who is likely to respond to the treatments being evaluated), and there is reason to think that EF deficits might disrupt treatment engagement. Conversely, it also would be interesting to test whether improvements in EF might mediate (at least in part) the effects of established treatments for suicidality (e.g., cognitive therapy; see Brown et al., 2005).
Exploring whether EF predicts death by suicide would unquestionably prove to be even more difficult (since completed suicides are more rare than attempts; see Nock et al., 2008), and likely would necessitate very large samples (and in turn, very simple and efficient EF measures). Nevertheless, these sorts of efforts could certainly be considered in elevated risk populations, within contexts where: 1) a large number of patients are seen; 2) there is routine long-term follow-up; and 3) EF data might be useful for other clinical reasons (e.g., primary care settings for elderly patients, large outpatient psychiatric clinics). Alternatively, the use of “psychological autopsies” could even prove to have utility for addressing this question, to the extent that reliable and valid information about EF can be obtained from family members or acquaintances of suicide victims (note that this sort of approach is sometimes used to assess premorbid EF in individuals who have suffered brain injuries).
Useful statistical analytic strategies
As previously mentioned, employing multiple measures of EF within the same study creates the potential for computing composite variables. If three or more are administered, more sophisticated statistical approaches can be used to accomplish this, such as factor analysis or structural equation modeling. Otherwise, in the absence of specific hypotheses regarding different EF indices, it is important to consider statistical methods for limiting the chances of spurious findings (e.g., Bonferroni corrections). Further, given that it is not possible to definitely establish a causal relationship through prospective studies alone, it is important to measure and then attempt to statistically address potential confounds (i.e., “third variables”) using techniques such as multiple regression (including controlling for baseline suicidality in prospective studies). That said, it is important to note that any method for addressing substantive group differences, statistical or otherwise, poses interpretive challenges (see Miller & Chapman, 2001). Finally, we recommend future studies formally test for non-linear associations between EF and suicidality, using techniques such as curvilinear regression (or even growth curve modeling, in prospective studies).
Exploring potential moderators
Some studies found evidence that other variables moderate the relationship between EF and suicidality, such as suicide attempt severity/lethality. But most notably, our review suggests that this link may be moderated by clinical diagnosis, though this conclusion would be strengthened by formally testing for an interaction between diagnosis and EF in well-powered studies with mixed diagnostic samples (or, given a sufficient number of studies in each area, testing for moderation meta-analytically). In fact, it remains possible that the divergent results we observed across diagnostic groups could be explained by sampling and/or measurement differences between studies. That said, we suspect that diagnosis might simply be a proxy for other meaningful variables that will ultimately explain these divergent findings. For example, the link between EF and suicidality may be moderated by other symptoms/deficits (e.g., delusions, thought disorder) that are diagnostic of (or at least more common in) psychotic disorders.
There are other variables that we hypothesize might exacerbate the effects of EF deficits on suicidality (and thus, moderate this link), based on our current understanding of their relationship with suicide risk, most notably stressful life events (see Liu & Miller, 2014) and sleep disturbances (see Pigeon et al., 2012). More generally, we suspect that EF inherently functions interactively with situational factors to precipitate suicidal crises, given that these deficits are generally fairly stable over time (e.g., see Biederman et al., 2007). Further, the multidimensional nature of EF opens up the possibility that different EF dimensions could interact with one another to predict suicidality (e.g., the relationship between inhibition and attempted suicide might be stronger in people with shifting deficits) – to our knowledge, this has not been tested. Finally, while a few studies have used adolescent or elderly samples, it would be worthwhile to formally test if age moderates the relationship between EF and suicidality, given the significant developmental changes that occur in both EF (see Blakemore & Choudhury, 2006, De Luca et al., 2003, and Jurado & Rosselli, 2007) and rates of suicide (see CDC, 2014).
Exploring potential mediators
As previously mentioned, despite the growing number of studies that have been conducted on this topic, mechanisms that could account for links between EF and suicidality remain largely a matter of speculation. Only a few studies have directly tested hypothesized mediators. Future research should do so, focusing on variables with known links to EF as well as to suicidal thinking and/or behavior (e.g., overgeneral memory; see Williams, 2006 and Richard-Devantoy et al., 2014b). Understanding mechanisms responsible for the observed associations between EF and suicidality would help clarify and concretize clinical implications of this research (discussed in the next section).
Since the relationship between EF and suicidality seems to vary across diagnostic groups, it may be necessary to explore the issue of mediation separately within different populations – or, using an even more sophisticated approach, test for ‘moderated mediation’ in mixed diagnostic samples (see Muller et al., 2005). In fact, doing this also might help us to better understand why such group differences exist. For example, measures of inhibition might be more consistently linked with attempted suicide in mood disorder samples because inhibition deficits lead to general impulse control problems (see Fikke et al., 2011 and Logan et al., 1997) that are more likely to culminate in suicidal behavior when they occur in the context of stable difficulties linked to risk for these disorders, such as rumination (see Alloy et al., 2006 and Nolen-Hoeksema et al., 2008). In fact, such ruminative tendencies might themselves reflect persistent EF deficits (and perhaps specifically, shifting deficits; e.g., see Bredemeier et al., 2011, Davis & Nolen-Hoeksema, 2000, and De Lissnyder et al., 2012) and promote/exacerbate suicidal thinking (see Miranda et al., 2007, 2013 and Marzuk et al., 2005). Of course, this proposal is speculative and warrants testing (along with alternative accounts for these findings).
While the evidence for a positive association between EF and suicidality in some psychotic disorder samples clearly diverges from findings in mixed and mood disorder samples (none of which reported any significant positive correlations), these findings seem consistent with other evidence linking higher general intelligence with elevated suicide risk in individuals with psychotic disorders (e.g., Batty et al., 2010; De Hert et al., 2001). A few possible mechanisms that could be responsible for such findings have been proposed (e.g., greater insight leading to more distress, greater ability to plan and execute an attempt), but have not received empirical support. Further investigation of this is clearly warranted.
Potential clinical implications
Research examining the relationship between EF and suicidality might ultimately have important clinical implications/applications. First and foremost, interventions to directly address or “remediate” EF deficits could possibly be incorporated into suicide prevention efforts. Even though EF is relatively stable, emerging evidence suggests that certain types of interventions can improve EF (e.g., cognitive training, aerobic exercise; see Diamond & Lee, 2011). Of course, this idea critically hinges on future research determining whether or not EF deficits can be considered a true risk factor for suicidal thinking and/or behavior within a particular population.
Even if individual differences in EF do not directly contribute to suicide risk, this work still might have clinical utility if EF measures can in fact predict future suicidal thinking and/or behavior. If so, it might be appropriate to include EF measures in clinical risk assessments (see Homaifar et al., 2012b), particularly in populations for which this data may be useful for other clinical purposes (e.g., adolescents, older adults). However, the viability of this idea hinges on the extent to which EF predicts suicidality above and beyond other variables that are traditionally examined in such risk assessments (e.g., psychiatric symptoms, hopelessness). Further, definitive estimates of effect sizes within different populations would be needed.
Conclusion
In summary, the existing literature examining the relationship between EF and suicidality provides tentative support for an association between these constructs. But importantly, this relationship appears to vary across diagnostic populations, and may be moderated by other factors as well (e.g., attempt seriousness/lethality). More research on this topic is clearly needed, and we encourage investigators to consider the recommendations discussed above when pursuing this work. Ultimately, research on EF and suicidality may have important implications for suicide risk assessment and/or prevention.
Supplementary Material
Highlights.
We reviewed the literature on links between executive function and suicidality.
43 articles examining this issue in different diagnostic populations were located.
There is tentative support for a link between executive function and suicidality.
However, this relationship may vary across diagnostic populations.
Limitations of this research and recommendations for future work are discussed.
Acknowledgments
Role of Funding Sources
Both authors received salary support from the National Institute of Mental Health (Bredemeier: grants U01MH088278 and T32MH082745; Miller: grants U01MH088278, R01MH095786, R01MH097741, and R01MH101129) during the time that this review was conducted and written. However, NIMH had no direct role in the process, or the decision to submit the manuscript for publication.
Both authors received salary support from the National Institute of Mental Health (Bredemeier: grants U01MH088278 and T32MH082745; Miller: grants U01MH088278, R01MH095786, R01MH097741, and R01MH101129) during the time that this review was conducted and written. However, NIMH had no direct role in the process, or the decision to submit the manuscript for publication. The idea for this paper was generated collaboratively by the authors. Bredemeier conducted the literature review and consulted with Miller regularly on issues/decisions that arose (e.g., regarding study inclusion). Then, Bredemeier wrote the initial draft of the manuscript, which Miller edited and provided feedback on. The authors have no financial interests to disclose, and would like to Lisa Uebelacker, Lauren Weinstock, and other members of the Department of Psychosocial Research at Brown University for their feedback on preliminary portions of the manuscript. Also, we would like to thank two anonymous reviewers for their helpful feedback and suggestions.
Footnotes
Keith Bredemeier is now at the Aaron T. Beck Psychopathology Research Center and the Department of Psychiatry, University of Pennsylvania.
Contributions
The idea for this manuscript was generated collaboratively by the authors. Bredemeier conducted the literature review and consulted with Miller regularly on issues/decisions that arose (e.g., regarding study inclusion). Then, Bredemeier wrote the initial draft of the manuscript, which Miller edited and provided feedback on.
Conflict of Interest
The authors have no financial interests to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
*references for articles from our literature review that are cited in the Results but not elsewhere in the text are presented in the Appendix
- Alloy LB, Abramson LY, Walshaw PD, Neeren AM. Cognitive vulnerability to unipolar and bipolar mood disorders. Journal of Social and Clinical Psychology. 2006;25:726–754. [Google Scholar]
- Alvarez JA, Emory E. Executive function and the frontal lobes: a meta-analytic review. Neuropsychology Review. 2006;16:17–42. doi: 10.1007/s11065-006-9002-x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association [APA] Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Ardila A, Galeano LM, Rosselli M. Toward a model of neuropsychological activity. Neuropsychology Review. 1998;8:171–190. doi: 10.1023/a:1021618218943. [DOI] [PubMed] [Google Scholar]
- Ardila A, Pineda D, Rosselli M. Correlation between intelligence test scores and executive function measures. Archives of Clinical Neuropsychology. 2000;15:31–36. [PubMed] [Google Scholar]
- Arbuthnott K, Frank J. Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. Journal of Clinical and Experimental Neuropsychology. 2000;22:518–528. doi: 10.1076/1380-3395(200008)22:4;1-0;FT518. [DOI] [PubMed] [Google Scholar]
- Arffa S. Cognition and suicide: a methodological review. Suicide and Life-Threatening Behavior. 1983;13:109–122. doi: 10.1111/j.1943-278x.1983.tb00009.x. [DOI] [PubMed] [Google Scholar]
- Audenaert K, Goethals I, Van Laere K, Lahorte P, Brans B, Versijpt J, et al. SPECT neuropsychological activation procedure with the Verbal Fluency Test in attempted suicide patients. Nuclear Medicine Communications. 2002;23:907–916. doi: 10.1097/00006231-200209000-00015. [DOI] [PubMed] [Google Scholar]
- Baddeley A. Exploring the central executive. The Quarterly Journal of Experimental Psychology: Section A. 1996;49:5–28. [Google Scholar]
- Banich M. Executive function: the search for an integrative account. Current Directions in Psychological Science. 2009;18:89–94. [Google Scholar]
- Batty GD, Whitley E, Deary IJ, Gale CR, Tynelius P, Rasmussen F. Psychosis alters association between IQ and future risk of attempted suicide: cohort study of 1,109,475 Swedish men. BMJ. 2010;340:c2506. doi: 10.1136/bmj.c2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beautrais AL, Joyce PR, Mulder RT, Fergusson DM, Deavoll BJ, Nightingale SK. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: a case-control study. American Journal of Psychiatry. 1996;153:1009–1014. doi: 10.1176/ajp.153.8.1009. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. FOCUS: The Journal of Lifelong Learning in Psychiatry. 2006;4:291–296. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- Bertolote JM, Fleischmann A, De Leo D, Wasserman D. Psychiatric diagnoses and suicide: revisiting the evidence. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2004;25:147–155. doi: 10.1027/0227-5910.25.4.147. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Fried R, Doyle AE, Spencer T, Seidman LJ, et al. Stability of executive function deficits into young adult years: a prospective longitudinal follow-up study of grown up males with ADHD. Acta Psychiatrica Scandinavica. 2007;116:129–136. doi: 10.1111/j.1600-0447.2007.01008.x. [DOI] [PubMed] [Google Scholar]
- Blakemore SJ, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. Journal of Child Psychology and Psychiatry. 2006;47:296–312. doi: 10.1111/j.1469-7610.2006.01611.x. [DOI] [PubMed] [Google Scholar]
- Bolton C, Gooding P, Kapur N, Barrowclough C, Tarrier N. Developing psychological perspectives of suicidal behaviour and risk in people with a diagnosis of schizophrenia: we know they kill themselves but do we understand why? Clinical Psychology Review. 2007;27:511–536. doi: 10.1016/j.cpr.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Brand M, Recknor EC, Grabenhorst F, Bechara A. Decisions under ambiguity and decisions under risk: correlations with executive functions and comparisons of two different gambling tasks with implicit and explicit rules. Journal of Clinical and Experimental Neuropsychology. 2007;29:86–99. doi: 10.1080/13803390500507196. [DOI] [PubMed] [Google Scholar]
- Bredemeier K, Warren SL, Berenbaum H, Miller GA, Heller W. Executive functioning deficits associated with past depressive symptoms. Annual meeting of the Society for Research on Psychopathology; Boston, MA. 2011. [Google Scholar]
- Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association. 2005;294:563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- Burgess PW, Alderman N, Evans J, Emslie H, Wilson BA. The ecological validity of tests of executive function. Journal of the International Neuropsychological Society. 1998;4:547–558. doi: 10.1017/s1355617798466037. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Fatal Injury Reports and Nonfatal Injury Reports. Atlanta, GA: National Center for Injury Prevention and Control; 2014. Web-based Injury Statistics Query and Reporting System. Available at: www.cdc.gov/injury/wisqars/index.html. [Google Scholar]
- Chen YW, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other Axis I disorders. Biological Psychiatry. 1996;39:896–899. doi: 10.1016/0006-3223(95)00295-2. [DOI] [PubMed] [Google Scholar]
- Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case–control study. The Lancet Neurology. 2007;6:693–698. doi: 10.1016/S1474-4422(07)70175-8. [DOI] [PubMed] [Google Scholar]
- Cohen D, Vergon TL, Malphurs J. Case studies of suicide in older persons with Alzheimer’s disease and related dementias. Journal of Mental Health and Aging. 1998;4:397–402. [Google Scholar]
- Conner KR, Duberstein PR, Beckman A, Heisel MJ, Hirsch JK, Gamble S, Conwell Y. Planning of suicide attempts among depressed inpatients ages 50 and over. Journal of Affective Disorders. 2007;97:123–128. doi: 10.1016/j.jad.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Davis RN, Nolen-Hoeksema S. Cognitive inflexibility among ruminators and nonruminators. Cognitive Therapy and Research. 2000;24:699–711. [Google Scholar]
- De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophrenia Research. 2001;47:127–134. doi: 10.1016/s0920-9964(00)00003-7. [DOI] [PubMed] [Google Scholar]
- De Lissnyder E, Koster EH, Everaert J, Schacht R, Van den Abeele D, De Raedt R. Internal cognitive control in clinical depression: general but no emotion-specific impairments. Psychiatry Research. 2012;199:124–130. doi: 10.1016/j.psychres.2012.04.019. [DOI] [PubMed] [Google Scholar]
- De Luca CR, Wood SJ, Anderson V, Buchanan JA, Proffitt TM, Mahony K, Pantelis C. Normative data from the CANTAB. I: development of executive function over the lifespan. Journal of Clinical and Experimental Neuropsychology. 2003;25:242–254. doi: 10.1076/jcen.25.2.242.13639. [DOI] [PubMed] [Google Scholar]
- Diamond A, Lee K. Interventions shown to aid executive function development in children 4 to 12 years old. Science. 2011;333:959–964. doi: 10.1126/science.1204529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlangsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. The American Journal of Geriatric Psychiatry. 2008;16:220–228. doi: 10.1097/JGP.0b013e3181602a12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fikke LT, Melinder A, Landro NI. Executive functions are impaired in adolescents engaging in non-suicidal self-injury. Psychological Medicine. 2011;41:601–610. doi: 10.1017/S0033291710001030. [DOI] [PubMed] [Google Scholar]
- Fisk JE, Sharp CA. Age-related impairment in executive functioning: updating, inhibition, shifting, and access. Journal of Clinical and Experimental Neuropsychology. 2004;26:874–890. doi: 10.1080/13803390490510680. [DOI] [PubMed] [Google Scholar]
- Fossati P, Amar G, Raoux N, Ergis AM, Allilaire JF. Executive functioning and verbal memory in young patients with unipolar depression and schizophrenia. Psychiatry Research. 1999;89:171–187. doi: 10.1016/s0165-1781(99)00110-9. [DOI] [PubMed] [Google Scholar]
- Giancola PR, Tarter RE. Executive cognitive functioning and risk for substance abuse. Psychological Science. 1999;10:203–205. [Google Scholar]
- Gilhooly KJ, Fioratou E, Anthony SH, Wynn V. Divergent thinking: strategies and executive involvement in generating novel uses for familiar objects. British Journal of Psychology. 2007;98:611–625. doi: 10.1111/j.2044-8295.2007.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. The British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Haw C, Harwood D, Hawton K. Dementia and suicidal behavior: a review of the literature. International Psychogeriatrics. 2009;21:440–453. doi: 10.1017/S1041610209009065. [DOI] [PubMed] [Google Scholar]
- Hay PJ, Denson LA, van Hoof M, Blumenfeld N. The neuropsychiatry of carbon monoxide poisoning in attempted suicide: a prospective controlled study. Journal of Psychosomatic Research. 2002;53:699–708. doi: 10.1016/s0022-3999(02)00424-5. [DOI] [PubMed] [Google Scholar]
- Homaifar BY, Bahraini N, Silverman MM, Brenner LA. Executive functioning as a component of suicide risk assessment: clarifying its role in standard clinical applications. Journal of Mental Health Counseling. 2012b;34:110–120. [Google Scholar]
- Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, et al. Impaired decision making in suicide attempters. American Journal of Psychiatry. 2005;162:304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- Jollant F, Lawrence NL, Olié E, Guillaume S, Courtet P. The suicidal mind and brain: a review of neuropsychological and neuroimaging studies. World Journal of Biological Psychiatry. 2011;12:319–339. doi: 10.3109/15622975.2011.556200. [DOI] [PubMed] [Google Scholar]
- Jurado MB, Rosselli M. The elusive nature of executive functions: a review of our current understanding. Neuropsychology Review. 2007;17:213–233. doi: 10.1007/s11065-007-9040-z. [DOI] [PubMed] [Google Scholar]
- Kerns JG, Nuechterlein KH, Braver TS, Barch DM. Executive functioning component mechanisms and schizophrenia. Biological Psychiatry. 2008;64:26–33. doi: 10.1016/j.biopsych.2008.04.027. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock MK, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. Journal of the American Medical Association. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Sackeim HA, Brodsky BS, Oquendo MA, Malone KM, Mann JJ. Neuropsychological dysfunction in depressed suicide attempters. American Journal of Psychiatry. 2001;158:735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- King DA, Conwell Y, Cox C, Henderson RE, Denning DG, Caine ED. A neuropsychological comparison of depressed suicide attempters and nonattempters. The Journal of Neuropsychiatry and Clinical Neurosciences. 2000;12:64–70. doi: 10.1176/jnp.12.1.64. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM. Differentiating suicide attempters from suicide ideators: a critical frontier for suicidology research. Suicide and Life-Threatening Behavior. 2014;44:1–5. doi: 10.1111/sltb.12068. [DOI] [PubMed] [Google Scholar]
- Liu R, Miller IW. Life events and suicidal ideation and behavior: a systematic review. Clinical Psychology Review. 2014;34:181–192. doi: 10.1016/j.cpr.2014.01.006. [DOI] [PubMed] [Google Scholar]
- Logan GD, Schachar RJ, Tannock R. Impulsivity and inhibitory control. Psychological Science. 1997;8:60–64. [Google Scholar]
- Lundqvist T. Cognitive consequences of cannabis use: comparison with abuse of stimulants and heroin with regard to attention, memory and executive functions. Pharmacology Biochemistry and Behavior. 2005;81:319–330. doi: 10.1016/j.pbb.2005.02.017. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Arango VA, Avenevoli S, Brent DA, Champagne FA, Clayton P, et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biological Psychiatry. 2009;65:556–563. doi: 10.1016/j.biopsych.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzuk PM, Hartwell N, Leon AC, Portera L. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatrica Scandinavica. 2005;112:294–301. doi: 10.1111/j.1600-0447.2005.00585.x. [DOI] [PubMed] [Google Scholar]
- Matarazzo BB, Clemans TA, Silverman MM, Brenner LA. The Self-Directed Violence Classification System and the Columbia Classification Algorithm for Suicide Assessment: a crosswalk. Suicide and Life-Threatening Behavior. 2013;43:235–249. doi: 10.1111/j.1943-278x.2012.00131.x. [DOI] [PubMed] [Google Scholar]
- McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychological Medicine. 2008;38:407–417. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- McGirr A, Jollant F, Turecki G. Neurocognitive alterations in first-degree relatives of suicide completers. Journal of Affective Disorders. 2012a;145:264–269. doi: 10.1016/j.jad.2012.05.062. [DOI] [PubMed] [Google Scholar]
- Meltzer HY. Reducing the risk for suicide in schizophrenia and affective disorders. Journal of Clinical Psychiatry. 2003;64:1122–1129. doi: 10.4088/jcp.v64n0920. [DOI] [PubMed] [Google Scholar]
- Miller GA, Chapman JP. Misunderstanding analysis of covariance. Journal of Abnormal Psychology. 2001;110:40–48. doi: 10.1037//0021-843x.110.1.40. [DOI] [PubMed] [Google Scholar]
- Miller M, Nevado-Montenegro AJ, Hinshaw SP. Childhood executive function continues to predict outcomes in young adult females with and without childhood-diagnosed ADHD. Journal of Abnormal Child Psychology. 2012;40:657–668. doi: 10.1007/s10802-011-9599-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Nolen-Hoeksema S. Brooding and reflection: rumination predicts suicidal ideation at 1-year follow-up in a community sample. Behaviour Research and Therapy. 2007;45:3088–3095. doi: 10.1016/j.brat.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda R, Valderrama J, Tsypes A, Gadol E, Gallagher M. Cognitive inflexibility and suicidal ideation: Mediating role of brooding and hopelessness. Psychiatry Research. 2013;210:174–181. doi: 10.1016/j.psychres.2013.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake A, Friedman NP. The nature and organization of individual differences in executive functions: four general conclusions. Current Directions in Psychological Science. 2012;21:8–14. doi: 10.1177/0963721411429458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cognitive psychology. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- Muscara F, Catroppa C, Anderson V. Social problem-solving skills as a mediator between executive function and long-term social outcome following paediatric traumatic brain injury. Journal of Neuropsychology. 2008;2:445–461. doi: 10.1348/174866407x250820. [DOI] [PubMed] [Google Scholar]
- Neuringer C. Rigid thinking in suicidal individuals. Journal of Consulting Psychology. 1964;28:54–58. doi: 10.1037/h0045809. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008b;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Placidi GP, Malone KM, Campbell C, Keilp J, Brodsky B, et al. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Archives of General Psychiatry. 2003;60:14–22. doi: 10.1001/archpsyc.60.1.14. [DOI] [PubMed] [Google Scholar]
- Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Comprehensive psychiatry. 2001;42:482–487. doi: 10.1053/comp.2001.26271. [DOI] [PubMed] [Google Scholar]
- Patsiokas AT, Clum GA, Luscomb RL. Cognitive characteristics of suicide attempters. Journal of Consulting and Clinical Psychology. 1979;47:478. doi: 10.1037//0022-006x.47.3.478. [DOI] [PubMed] [Google Scholar]
- Peterson JB, Rothfleisch J, Zelazo PD, Pihl RO. Acute alcohol intoxication and cognitive functioning. Journal of Studies on Alcohol and Drugs. 1990;51:114–122. doi: 10.15288/jsa.1990.51.114. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. The Journal of clinical Psychiatry. 2012;73:e1160–7. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- Pollock LR, Williams JMG. Problem-solving in suicide attempters. Psychological Medicine. 2004;34:163–167. doi: 10.1017/s0033291703008092. [DOI] [PubMed] [Google Scholar]
- Posner K, Oquendo M, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. American Journal of Psychiatry. 2007;164:1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard-Devantoy S, Olié E, Guillaume S, Bechara A, Courtet P, Jollant F. Distinct alterations in value-based decision-making and cognitive control in suicide attempters: Toward a dual neurocognitive model. Journal of Affective Disorders. 2013a;151:1120–1124. doi: 10.1016/j.jad.2013.06.052. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Berlim MT, Jollant F. A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychological Medicine. 2014a;44:1663–1673. doi: 10.1017/S0033291713002304. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Berlim MT, Jollant F. Suicidal behaviour and memory: a systematic review and meta-analysis. The World Journal of Biological Psychiatry. 2014b:1–23. doi: 10.3109/15622975.2014.925584. [DOI] [PubMed] [Google Scholar]
- Schneider B. Substance use disorders and risk for completed suicide. Archives of Suicide Research. 2009;13:303–316. doi: 10.1080/13811110903263191. [DOI] [PubMed] [Google Scholar]
- Simpson G, Tate R. Suicidality in people surviving a traumatic brain injury: prevalence, risk factors and implications for clinical management. Brain Injury. 2007;21:1335–1351. doi: 10.1080/02699050701785542. [DOI] [PubMed] [Google Scholar]
- Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychological Bulletin. 2013;139:81–132. doi: 10.1037/a0028727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ten Have M, de Graaf R, Van Dorsselaer S, Verdurmen J, van’t Land H, Vollebergh W, Beekman A. Incidence and course of suicidal ideation and suicide attempts in the general population. Canadian Journal of Psychiatry. 2009;54:824–833. doi: 10.1177/070674370905401205. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Sorge GB, Benoit A, West RF, Stanovich KE. Decision-making and cognitive abilities: a review of associations between Iowa Gambling Task performance, executive functions, and intelligence. Clinical Psychology Review. 2010;30:562–581. doi: 10.1016/j.cpr.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R. Risk factors for late-life suicide: a prospective, community-based study. The American Journal of Geriatric Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- Wedig M, Weinstock LM. Suicide and bipolar disorder: The state of the evidence. In: Plunkett JM, editor. Bipolar disorder: Causes, diagnosis, and treatment. New York: Nova Science Publishers; 2012. pp. 293–312. [Google Scholar]
- Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: Scientific and clinical applications. Washington DC: American Psychological Association; 2009. [Google Scholar]
- Williams JMG. Capture and rumination, functional avoidance, and executive control (CaRFAX): three processes that underlie overgeneral memory. Cognition & Emotion. 2006;20:548–568. doi: 10.1080/02699930500450465. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Ellis NC, Tyers C, Healy H, Rose G, MacLeod AK. The specificity of autobiographical memory and imageability of the future. Memory & Cognition. 1996;24:116–125. doi: 10.3758/bf03197278. [DOI] [PubMed] [Google Scholar]
- Young MH, Justice JV, Erdberg P. Risk of harm: inmates who harm themselves while in prison psychiatric treatment. Journal of Forensic Sciences. 2006;51:156–162. doi: 10.1111/j.1556-4029.2005.00023.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


