Abstract
Little is known about the assessment and treatment of self-stigma in substance abusing populations. This article describes the development of an acceptance based treatment (Acceptance and Commitment Therapy – ACT) for self-stigma in individuals in treatment for substance use disorder. We report initial outcomes from a study with 88 participants in a residential treatment program. The treatment involves 6 h of a group workshop focused on mindfulness, acceptance, and values work in relation to self-stigma. Preliminary outcomes showed medium to large effects across a number of variables at post-treatment. Results were as expected with one potential process of change, experiential avoidance, but results with other potential mediators were mixed.
Keywords: Substance abuse, stigma, treatment, shame
Introduction
Individuals with substance use problems suffer immense disadvantages. In addition to the deleterious effects directly resulting from substance use problems, the social and economic opportunities available to people with substance use problems, even when in recovery, are sharply reduced. Negative effects from stigma have been demonstrated across a range of mental health problems, including mood disorders (Kelly and Jorm 2007), schizophrenia (Corrigan 2004), borderline personality disorder (Aviram et al. 2006), and substance abuse (Luoma et al. 2007), with enacted stigma (i.e., discrimination toward those with substance problems) occurring in areas such as employment (Link 1987; Penn and Martin 1998; Penn et al. 2002), housing (Page 1983), and social relationships (Luoma et al. 2007; Perlick et al. 2001). These problems are particularly severe in the area of substance abuse, which tends to evoke even greater negative social attitudes than schizophrenia (Corrigan et al. 2000; Crisp et al. 2000).
In addition to the effects of enacted stigma, individuals with a substance use disorder may be negatively impacted through the effects of self-stigma. Self-stigma can be defined as shame, evaluative thoughts, and fear of enacted stigma that results from individuals’ identification with a stigmatized group that serves as a barrier to the pursuit of valued life goals. For example, a person in recovery might avoid treatment, not apply for jobs, or avoid intimate social relationships due to a belief that they are not to be trusted based on their substance abuse history. Critical to this definition is the notion that it is not simply the presence of negative evaluative attitudes, emotions, and thoughts, but also their deleterious impact that is important.
The data on the impact of self-stigma are most extensive with the seriously mentally ill, the majority of whom also have substance use problems. In this population, self-stigma has been associated with delays in treatment seeking (Kushner and Sher 1991; Scambler 1998; Starr et al. 2002), diminished self-esteem/self-efficacy (Wright et al. 2000; Corrigan and Watson 2002; Link et al. 2002) and lower quality of life (Rosenfield 1997). Some similar data are available for substance use problems per se. For example, the fear of being stigmatized is a reported barrier to seeking treatment among those with substance abuse problems (Tuchfeld 1981; Hingson et al. 1982; Klingeman 1991; Cunningham et al. 1993; Tucker et al. 1994).
Stigma intervention research
Stigma intervention research to date has largely focused on reducing enacted stigma through intervention such as protesting stigma, education, or promoting positive contact (Corrigan and Penn 1999). Little evidence supports the use of protest or education as an effective form of stigma reduction in the long term (Langer et al. 1976; Macrae et al. 1994; Smart and Wegner 1999, 2000). The strongest evidence is found for interventions that focus on creating personal contact between stigmatizers and those stigmatized, in a positive context (Link et al. 2002; Couture et al. 2006).
Unfortunately, these previously developed interventions do not readily translate into a self-stigma paradigm. To date, there appear to be no published studies targeting self-stigma in substance abuse. One recent study that focused more on coping with enacted stigma than on self-stigma per se targeted the seriously mentally ill (Link et al. 2002), by educating participants about stigma, suggesting methods to combat and cope with stigma, and fostering discussion about personal experiences. Rehabilitation clubhouse members (N = 88) were randomly assigned either to receive 16 group sessions of this intervention or no treatment. At a 6-month follow-up the intervention group was not significantly different from controls on any measure. The control group then also received the intervention and a second follow-up occurred at 2 years. Pre-treatment correlations between feeling set apart or different (two components of stigma) and depression (r = 0.57) and self esteem (r = 0.49) appeared to be lower at the 2 year follow-up (depression, r = 0.27; self-esteem, r = −0.14), which the authors interpreted to mean that the intervention may have impacted the relationship between stigmatizing beliefs and measures of psychological health even though the presence of these beliefs continued unchanged.
The possibility that it may be easier to modify the link between private experiences and overt behavior rather than the content or frequency of those experiences per se provides an important lead that seems worth exploring in the area of self-stigma. We know that the common stereotypes of a culture are not unlearned once they are learned (Devine 1989) and direct efforts to get rid of thoughts can result in paradoxical increases in those very thoughts (Macrae et al. 1994; Wenzlaff and Wegner 2000). This suggests that it may be less fruitful to directly attempt to eliminate particular stereotypes, but rather that it may be a more effective strategy to modify the functional link between thoughts, feelings and overt behavior rather than the content or frequency of those thoughts and feelings.
Acceptance and mindfulness strategies provide one way of changing the relationship between thoughts, feelings, and overt actions (Hayes et al. 2004b). Procedures such as Dialectical Behavior Therapy (Linehan 1993), Acceptance and Commitment Therapy ACT (Hayes et al. 1999), Mindfulness-Based Cognitive Therapy (Segal et al. 2002), are examples. These procedures are similar in focusing on the relationship between thoughts, feelings, and overt behavior, rather than on attempts to modify the problematic thoughts and feelings themselves. Mindfulness and acceptance procedures appear to be helpful across a wide range of behavioral problems (Hayes et al. 2004c), and both DBT (Linehan et al. 1999, 2002), and ACT (Gifford et al. 2004; Hayes et al. 2004e), have demonstrated impact in the area of addictions.
The treatment we chose to apply to self-stigma, ACT, is based on a contemporary behavior analytic theory of language and cognition called Relational Frame Theory (Hayes et al. 2001), which differentiates between contextual events that change the structure of cognitive networks and those that change their function. In ACT, patients are taught to watch their thoughts mindfully and to feel their feelings fully, rather than trying to change their form, and then to focus on overt actions that will move them in valued directions. Changes in processes of this kind are assessed by such measures as the Acceptance and Action Questionnaire (Hayes et al. 2006), which examines people’s willingness to accept their undesirable thoughts and feelings, while acting in a way that is congruent with their values and goals, or through measures of the literal believability of negative thoughts (Hayes et al. 2006). Across a range of studies these measures have proven to mediate outcomes in ACT, indicating that changes in the function of private experiences, and not their form explains ACT outcomes (Hayes et al. 2006).
These ideas have already been applied to stigma in the substance abuse area (Hayes et al. 2004a). From an ACT perspective, the negative impact of stigmatizing beliefs and attitudes comes not from the presence of such thoughts, but from the function of the thoughts. Procedures used in ACT attempt to help people develop a more accepting, mindful relationship with their thoughts and feelings, such that these thoughts and feelings can be disconnected from the previously acquired overt behavior that may serve to obstruct recovery.
In what appears to be the only controlled intervention study to date on enacted substance abuse stigma, ACT was applied as an intervention for substance abuse counselors (Hayes et al. 2004d). In this controlled trial, 93 drug and alcohol counselors were randomly assigned to one of three 6 h groups, either Acceptance and Commitment Therapy (ACT; n = 30), Multicultural Training (n = 34), or training in a biological model of substance abuse (n = 29). On a measure of the frequency of stigmatizing attitudes, multicultural training improved more than the educational control from pre- to post-treatment while ACT did not. However, at a 3 month follow-up, the ACT condition showed significant improvements in a measure of burnout. What is perhaps most important for present purposes, a measure of believability of stigmatizing attitudes successfully mediated follow-up outcomes (i.e., burnout and the frequency of stigmatizing attitudes) for ACT, but not Multicultural Training. Said more simply, it was a change in function of private experiences, not their form, that proved predictive in ACT outcomes.
This same model appears to be readily applicable to self-stigma. For example, a common thought that individuals with substance use problems have about themselves is, ‘‘I hurt people that I love.’’ Taken literally or fully believed, this might lead the person to escape or avoid thinking about being someone who hurts others, but doing so would probably include avoiding situations where the possibility of thinking these thoughts exist. Unfortunately, the very situations that would likely be part of recovery, such as creating a recovery support system, or reuniting with one’s family and friends, are likely to call forth this thought and related fears. If a person is unwilling to experience these negatively evaluated thoughts and feelings and must instead avoid them, they are unlikely to move forward in their lives in these areas. ACT attempts to help people be able to respond in new, more effective, ways when some of these previously obstructive thoughts and feelings emerge.
Problems in the measurement self-stigma
As defined above, self-stigma consists of shame, evaluative thoughts, and fear of enacted stigma that results from individuals’ identification with a stigmatized group. No direct measure of this variable exists as we have defined it. However, existing measures do exist for components of this variable, such as shame. Fortunately, a well-validated measure of internalized shame exists (Cook 1996). When we started the study, we hypothesized that this would be our primary outcome variable. However, during the time we were running the study a measure of internalized stigma in mental illness was published (Ritsher et al. 2003). The idea of internalized stigma was quite similar to that of self-stigma and so we adapted the Risher et al. (2003) measure to use in a substance using population and added it as a second primary outcome variable in the latter half of the study. While neither of these measures conforms perfectly to our definition of self-stigma, they do appear to capture a good part of phenomena of interest so that treatment develop can continue while we are developing a better measure of self-stigma.
In this article, we outline the initial adaptation of an ACT model to the problem of self-stigma in substance abuse, describe the training of study therapists, and report pilot outcomes. To our knowledge, these data, though uncontrolled, describe the first treatment specifically measuring and targeting self-stigma and shame in substance abuse. Over the period of intervention we expected to see decreases in internalized shame and internalized stigma as well as changes in variables measuring hypothesized change processes.
Method
Participants
Participants were 88 adults (47 female, 41 male; mean age = 35.8) diagnosed with a substance use disorder, who were participating in a 28-day residential treatment program with a general orientation toward a 12-step model. Thirty percent of the participants identified themselves as non-Caucasians [African-American (N = 1), American Indian (N = 3), Asian/Pacific Islander (N = 1), Hispanic (N = 11), ‘‘other’’ (N = 7)]. Participants used a variety of substances (Table I) in the 30 days before program entry, with the most common being alcohol, methamphetamine, and marijuana. Additional demographic data is listed in Table I.
Table I.
Participant background information.
| Completers (n = 48) | Noncompleters (n = 40) | |
|---|---|---|
| During 30 days prior to admission used any: | ||
| Alcohol | 39% (n = 18) | 56% (n = 22) |
| Methamphetamines | 24% (n = 9) | 47% (n = 18) |
| Marijuana | 18% (n = 7) | 26% (n = 10) |
| Other hallucinogens | 0% | 5% (n = 2) |
| Inhalants | 3% (n = 1) | 3% (n = 1) |
| Cocaine | 3% (n = 1) | 8% (n = 3) |
| Heroin | 3% (n = 1) | 8% (n = 3) |
| Other opiates | 5% (n = 2) | 18% (n = 7) |
| Methadone | 3% (n = 1) | 5% (n = 2) |
| Major tranquilizers | 11% (n = 3) | 24% (n = 8) |
| Tobacco | 65% (31) | 82% (n = 33) |
| During 30 days prior to admission: | ||
| Had Unprotected sex | 42% (n = 18) | 57% (n = 20) |
| Drinking and driving | 23% (n = 10) | 24% (n = 8) |
| Shared drug paraphernalia | 12% (n = 5) | 21% (n = 7) |
| Had ‘‘serious thoughts of suicide’’ | 41% (n = 17) | 50% (n = 17) |
| Attempted suicide | 24% (n = 10) | 39% (n = 13) |
| No. of previous treatments in lifetime | 2 (SD = 1.85) | 1.92 (SD = 2.6) |
| Taking psychiatric medications | 19% (n = 9) | 18% (n = 7) |
| Completed at least High school | 72% (n = 34) | 68% (n = 26) |
| Completed at least some college | 28% (n = 13) | 18% (n = 7) |
| Employed | 19% (n = 9) | 15% (n = 6) |
| On probation/parole, bail, or awaiting trial | 50% (n = 22) | 50% (n = 20) |
| Percentages were calculated based on percent of complete data | ||
Recruitment
All potential study participants were given a recruitment flyer describing the study and invited to the initial assessment session, which was held on the residential unit. During this initial assessment session, those that consented to participate in the study completed the pre-intervention assessment battery. Participants received a $5 gift certificate to a local department store for completing the pre-assessment battery and a $10 gift certificate for completion of the post-treatment assessment battery about 1 week later. We excluded from recruitment those on the unit who were not available to participate (about to be discharged), or who the unit staff felt had severe cognitive impairment that would obstruct participation in the group (e.g., mental retardation, dementia, or unstable psychotic disorders).
Procedure
Participants attended a 6 h ACT group in place of their normal treatment that would have occurred at the same time. The overall treatment schedule at this facility averaged 34 h per week in a wide variety of therapy, psychoeducational, or educational groups.
For all groups, pre- and post-assessments were held one week apart. Between the two assessment points the group intervention was delivered. A total of nine cohorts completed the groups. For eight of them, the intervention was conducted in three 2 h sessions. Due to scheduling difficulties, one group with four participants was 5 h in length, conducted across two sessions. Completers were defined as participants who completed at least 4 h of group intervention and attended the post-intervention assessments. Groups varied in size from 3 to 9 completers. Several measures were included in the first five groups that were different from those in the last four groups. This was done to allow us to examine the effect of our intervention on a variety of measures without overly burdening participants.
ACT for self-stigma
The group sessions were both experiential and didactic, and focused on using the processes of psychological acceptance, cognitive defusion, and contact with important values to help participants learn to respond to their stigmatizing thoughts and behaviors in a way that would not obstruct recovery. Acceptance techniques encourage participants to feel difficult feelings more fully while reducing their automatic link to overt action. Cognitive defusion techniques help group members ‘‘deliteralize’’ the content of thoughts – that is, to focus more on the process of thinking and the workability of behavior tied to particular thoughts than on their content. For example, the group generated a particularly potent self-evaluation and reduced it to a single word (e.g., one group arrived at the word ‘‘loser’’). The entire group then repeated that word rapidly out loud for about 30 s, a procedure known to reduce both fusion with thoughts and the distress they evoke (Masuda et al. 2004). Mindfulness exercises and metaphors (e.g., watching thoughts like one would watch leaves on a stream) were used to help individuals stay in the present moment and not get ‘‘hooked’’ on thoughts or live in the past or future (Hayes et al. 1999). Participants were encouraged to explore their goals and values in life and to link accomplishment of desired goals to values rather that to automatic thoughts and feelings. A final target of the stigma-combating process is to build a positive agenda of human connection and mutual acceptance. Techniques specific to each targeted process are described in more detail in ACT treatment and self-help manuals (Eifert and Forsyth 2005; Hayes and Smith 2005; Hayes and Strosahl 2005; Hayes et al. 1999).
While the same ACT processes were targeted in all nine groups, the technical content evolved during an iterative developmental process. Each intervention group was followed by a focus group with participants. Supervision was provided by experienced ACT therapists, who listened to audio taped sessions and who provided detailed feedback. Study therapists were experienced ACT therapists, and they provided peer supervision for one another. The treatment manual was then modified based on supervision feedback, group leaders’ experiences, objective outcomes and focus group feedback, and specific techniques were added or subtracted.
Measures
A relatively large number of measures were used to explore the preliminary outcomes of the group. Some measures were changed after the first five groups.
Demographics
Information on demographics, drug use information, and functional status was collected using a modified version of the Treatment Outcomes Measurement Instrument (TOMI), which is a 36-item interview that was converted into a paper-and-pencil questionnaire. A few additional items were added that asked about whether participants had ever experienced certain forms of enacted stigma.
Shame
The Internalized Shame Scale (Cook 1996), consists of 30 items measuring participants’ level of internalized shame and is thought to be related to self–stigma. Internal consistency (coefficient alpha) and test–retest reliabilities of 0.94 and 0.71 were obtained for the ISS (Cook 1989). The present study obtained higher coefficient alphas; a Cronbach’s alpha of 0.97 was obtained at both pre- and post-assessment.
Internalized stigma
The Internalized Stigma of Substance Abuse (ISSA) was adapted from the Internalized Stigma of Mental Illness scale (Ritsher et al. 2003), to focus on substance abuse specifically rather than mental illness. It is designed to measure the subjective experience of stigma, including alienation, stereotype endorsement, perceived discrimination, social withdrawal, and stigma resistance. The scale consists of 29 items. The original scale had high internal consistency (coefficient α = 0.90) and test–retest reliability (r = 0.92). The adopted scale used in the current study also obtained high internal consistency scores; coefficient alpha estimates were 0.82 and 0.92 at pre- and post-assessment.
Experiential avoidance and psychological flexibility
The Acceptance and Action Questionnaire (AAQ) is a nine-item measure of the willingness to accept undesirable thoughts and feelings, while acting in a way that is congruent with values and goals. This version demonstrated low Cronbach’s alphas (0.50 and 0.69 at pre- and post-assessment) in the current study with the first five groups. A second nine-item version of the AAQ with simplified items (Hayes et al. 2004d), was administered for groups 6–9. The second version obtained coefficient alphas of 0.81 and 0.94 at pre- and post-assessment.
Stigmatizing attitudes – believability (SAB)
This measure was adapted from a scale used in Hayes et al. (2004d) that measured common stigmatizing thoughts providers have towards clients with substance abuse problems. The original scale was developed by generating common negative thoughts providers have about difficult substance abuse clients. The scale was adapted to reflect a first-person perspective. Examples items include ‘‘I am not going to change no matter what I do’’ and ‘‘If I really wanted to get sober, I would.’’ Participants are asked to ‘‘imagine that the following thoughts occurred to you right now’’ and, if they occurred, how valid or believable they would be. Item responses are summed to an overall score ranging from 20 to 140. Higher scores indicate a greater level of cognitive fusion with stigmatizing thoughts. In the current study, adequate reliability was obtained, with an estimate of 0.72 and 0.78 (coefficient alphas) at pre- and post-assessment.
Overall mental health
The General Health Questionnaire-12. (Goldberg 1972; Vieweg and Hedlund 1983) The GHQ, available in several forms, is a widely used self-report questionnaire designed to measure general mental health and stress. The 12-item version used in this study asks participants to respond based on a four-point Likert scale with higher scores indicating better health. The GHQ-12 has been shown to have high internal consistency; Cronbach’s alpha for the GHQ-12 ranges from 0.82 to 0.90. The current study obtained slightly higher estimates, obtaining a Cronbach’s alpha of 0.91 at pre- and 0.92 at post-assessment.
Quality of life
The Quality of Life Scale, (Flanagan 1978) is a 16 item scale that measures several aspects of functional status, including tasks of daily living, work, social activity, family contact and daily activities. The coefficient alpha estimate obtained in the present study was 0.93.
Perceived social support
The Multidimensional Scale of Perceived Social Support, (Zimet et al. 1988) is a 12-item self-report inventory that attempts to assess the adequacy of the respondent’s perceived social support. Lower scores indicate stronger social support. The total scale obtained high coefficient alphas, with reliability estimates of 0.92 and 0.95 at pre- and post-assessment. Each individual scale also had high internal consistency. The ‘‘significant other’’ subscale obtained coefficient alphas of 0.93 and 0.96 at pre- and post-assessment, the ‘‘family’’ subscale obtained coefficient alphas of 0.86 and 0.91 at pre- and post-assessment, and the ‘‘friends’’ subscale obtained coefficient alphas of 0.90 and 0.95 at pre- and post-assessment.
Self-esteem
The Rosenberg Self-Esteem Scale (Rosenberg 1965), is a 10 item scale and is the most commonly used measure of global self-esteem. High scores indicate higher self-esteem. The use of this scale is well established in the literature (Blascovich and Tomaka 1991). The current study obtained coefficient alphas of 0.91 at pre-assessment and 0.85 at post-assessment.
Perceived stigma
This 12 item measure was adapted from Link’s (Link et al. 1997), perceived-discrimination-devaluation questionnaire, and is intended to measure the extent to which the public at large holds stigmatizing beliefs. The present study obtained Cronbach’s alphas of 0.91 at pre-assessment and 0.92 at post-assessment.
Stigma-related rejection
A survey of mental health consumer’s experiences with stigma that was originally developed by Wahl (1999), was adapted to use with a substance using population by replacing the term ‘‘I am a consumer’’ with ‘‘I have been in treatment for my substance use.’’ The scale includes nine statements such as worrying that others will view one unfavorably, being treated as less competent, and hearing others say unfavorable things about oneself. Additionally, the statements were converted to a 7-point Likert scale never (1) to always (7), rather than the original 5-point Likert used by Wahl (1999). While this change limits our ability to make direct comparisons with mental health consumer samples, it seems unlikely to affect the validity of this measure for the purposes of our study. Estimates of internal consistency (coefficient alpha) of 0.83 at pre- and 0.91 at post-assessment were obtained in the current study.
Self-concealment
The Self-Concealment Scale (Larson and Chastain 1990), measures a person’s tendency to conceal personal information that is distressing or negative. Greater values indicate greater self-concealment. Larson and Chastain obtained high internal consistency reliability (coefficient alpha) of 0.83. The present study obtained a coefficient alpha of 0.92 at pre-assessment and 0.95 at post-assessment.
Believability of reasons for using drugs
The Believability of Reasons Scale (BOR) is a measure of the believability of common reasons given for using drugs. It has been used once previously in Bissett (Bissett 2002), and in that study showed a greater decrease with ACT than with a control treatment. This 22-item scale is summed to provide one overall score, with higher ratings indicating greater believability in their thoughts. Cronbach’s alphas indicate high internal validity; the present study obtained coefficient alphas at 0.95 at pre- and 0.97 at post-assessment.
Working alliance
The Working Alliance Inventory–Short Form (Tracey and Kokotovic 1989), is composed of 12 items. Ratings yield three four-item scales (task, bond and goal). However, the short form is used primarily for one total General Alliance score and secondarily for the three specific aspects of the alliance. Busseri and Tyler (2003), obtained an internal consistency estimate (coefficient alphas) of 0.91 for clients after four sessions with a therapist. An estimate of 0.92 (coefficient alpha) was obtained in the present study.
Satisfaction
The Client Satisfaction Questionnaire-3 (Larsen et al. 1979) is a 3-item self-report measure that has been adapted for a variety of populations and contexts. In this case, the measure has been adapted to assess the participants’ satisfaction with the intervention. Participants respond to each item on a 4-point scale, with higher scores indicating greater satisfaction with the intervention. Previous studies (Larsen et al. 1979), obtained a Cronbach’s alpha of 0.92. The present study obtained an adequate internal consistency estimate of 0.84 (coefficient alpha).
Results
Data analysis
All data analyses were conducted using SPSS12.0.1. (SPSS 2003). Primary analyses of interest were within-subject changes on our self-stigma variables, internalized shame and internalized stigma. Continuous variables were analyzed using a within-subjects t-test. Categorical variables were analyzed using chi-squares. Given the exploratory purposes of this preliminary trial, no attempt was made to adjust for experiment-wise alpha.
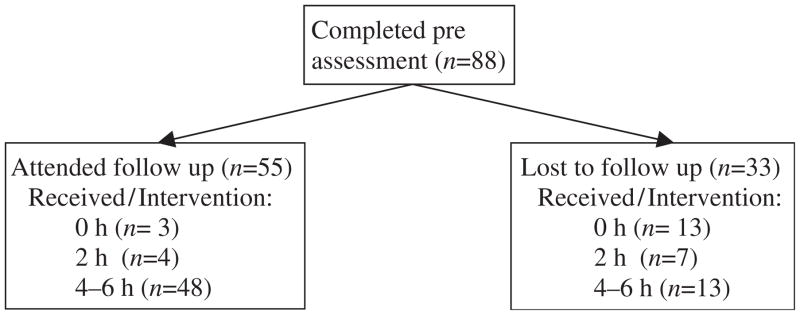
Completers
Completers were defined as those who attended at least half of the intervention and also completed the post assessment. Of the 88 participants who completed the preassessment, 55 (63%) completed follow up. Of these, 48 participants (55%) also attended at least 4 h of the intervention and were therefore defined as completers. Additional detail on subject flow can be seen in Figure 1. Patient and staff reports indicated that the vast majority of non-completers missed sessions or post-assessment due to conflicting medical or legal appointments or because they were unexpectedly discharged from the residential program.
Figure 1.
Participant flow.
No statistically significant differences were found between completers and non-completers on any pretreatment measures or demographic variables. Of the 27 who attended less than 4 h of intervention, 7 completed follow-up assessments enabling assessment of treatment outcomes. This subgroup did not significantly improve on any measures. All additional analyses of treatment effects are reported using only the completer sample. Other than focusing on completers, the only missing data in the study was the rare missing item from a scale. When an individual item was missing from a scale, we substituted the mean of the other scale items for that participant. All analyses reported below were for the completer sample. When analyses were conducted with all participants in the model, results were very similar to those reported below.
Characterizing the sample
Some measures were included in order to characterize the sample. To assess the entry levels of enacted stigma, participants were asked about a number of specific areas identified by Link (Link et al. 1997). Sixty-seven percent (N = 16) reported having had some of their friends reject them when they found out they were using substances. Sixty-five percent (N = 17) reported that some of their family gave up on them when they found out they were using substances. Sixty-four percent (N = 16) reported that some people were afraid of them when they found out they were using substances. Sixty-three percent (N = 19) reported unfair treatment because others knew they were using substances. Thirteen percent (N = 4) reported that employers had paid them a lower wage because they knew they had a substance use history. Seven percent (n = 6) reported no experiences with stigma on these questions and over 61% (n = 50) reported 3 or more types of rejection.
On our measure of stigma-related rejection, the mean item score was 3.14 (SD = 1.61), which corresponds to ‘‘seldom’’ on the scale. On average across the 9 items, 18.9% of respondents reported ‘‘frequently’’, ‘‘almost always’’ or ‘‘always’’ experiencing the various forms of rejection listed in the scale.
At pre-intervention, completers scored an average of 69.07 (SD = 18.0) on the QOLS. This corresponds to an average rating somewhere between ‘‘mixed’’ and ‘‘mostly satisfied’’ on ratings of different domains of life. These scores are fairly low, that is, about one standard deviation worse than a sample of patients with chronic physical illnesses (Burckhardt et al. 1989).
Outcome analyses
Mean pretreatment and post-treatment scores for each primary outcome measure in each set of groups and the resulting effect size and significance level are presented in Table II. Note that some measures were changed after the fifth cohort in an attempt to investigate new pilot measures of outcome and mediators. A particularly important addition was the primary outcome variable of internalized stigma, a measure which was only added after the investigators discovered a related version in a recently published manuscript (Ritsher et al. 2003).
Table II.
Mean scores on outcome variables.
| Pre-treatment
|
Post-treatment
|
Effect size
|
|||
|---|---|---|---|---|---|
| M | SD | M | SD | d | |
| Primary outcomes | |||||
| Internalized shame (N = 48) | 101.1 | 25.8 | 87.8 | 27.1 | 0.50*** |
| Internalized stigma (N = 18) | 39.3 | 8.8 | 31.2 | 15.5 | 0.67* |
| Secondary Outcomes | |||||
| General health Questionnaire (N = 48) | 35.40 | 8.42 | 39.19 | 7.63 | 0.49* |
| Stigma-related Rejection (N = 48) | 28.25 | 9.07 | 29.17 | 9.28 | 0.13 |
| Self concealment scale (N = 17) | 27.47 | 9.12 | 33.12 | 9.4 | 0.65* |
| Total social support (MSPSS; N = 15) | 3.42 | 1.31 | 2.95 | 1.26 | 0.42 |
| Family social support (N = 17) | 3.03 | 1.53 | 2.71 | 1.26 | 0.22 |
| Sig. other social support (N = 17) | 3.32 | 1.76 | 3.09 | 1.65 | 0.25 |
| Friends social support (N = 16) | 3.91 | 1.24 | 3.06 | 1.37 | 0.54* |
| Rosenberg self-esteem Scale (N = 15) | 15.24 | 6.8 | 20.88 | 5.89 | 0.89** |
| Perceived stigma (N = 30) | 53.57 | 14.38 | 50.07 | 11.27 | 0.27 |
| Process measures | |||||
| Stigmatizing attitudes Believability (N = 48) | 61.25 | 18.02 | 60.33 | 16.26 | 0.05 |
| AAQ (N = 30) | 37.63 | 5.62 | 33.6 | 7.19 | 0.56** |
| Believability of reasons for using (N = 48) | 92.43 | 34.23 | 94.67 | 37.57 | −0.07 |
| AAQ-II (N = 18) | 29.17 | 9.10 | 37.56 | 12.04 | 0.84** |
Note: Asterisks indicate significant pre-post changes at:
= p < 0.05,
= p < 0.01,
= p < 0.001.
Primary outcomes
Primary outcomes were pre- to post-treatment changes on internalized shame and internalized stigma. Data were available from all nine groups using the internalized shame scale. Participants showed a significant decrease in shame at post treatment as measured by the ISS, t(47) = 4.59, p < 0.001, d = 0.66. Data were available from the last four groups on the in terms of internalized stigma, with participants significantly improving from pre- to post-treatment, t(17) = 2.39, p = 0.029, d = 0.67.
Secondary outcomes
Secondary outcome measures that were available across all nine groups were the general mental health and stigma-related rejection. Participants showed a significant improvement in general mental health as measured by the GHQ, t(47) = 3.79, p = 0.001, d = 0.49, with no significant change in stigma-related rejection, t(47) = 0.89, p = 0.38. Participants did not show any significant change in perceived stigma, t(29) = 1.53, p = 0.14, a measure only available for the first five cohorts. On measures that were only available for the last four cohorts, participants showed a significant decrease in self-concealment as measured by the SCS, t(16) = 2.66, p = 0.017, d = 0.65, and a significant improvement in self-esteem as measured by the RSE, t(14) = 3.68, p = 0.002, d = 0.89. On the MSPSS, there was a significant change on the subscale indicating increased social support from friends, t(16) = 2.56, p = 0.038, but not on subscales measuring social support from family t(16) = 0.91, p = 0.376 or significant others, t(16) = 1.04, p = 0.31.
Process measures
Believability of stigmatizing attitudes was available for all nine cohorts and did not change significantly, t(47) = 0.35, p = 0.73. On measures that were available for the first five cohorts, participants showed significant improvements on experiential avoidance as measured by the AAQ, t(29) = 3.07, p = 0.005, d = 0.56, but did not show any significant changes on rated change in the believability of their reasons for using as measured by the BOR, t(29) = 0.36, p = 0.72, d = 0.07. Experiential avoidance as measured by the AAQ-II (available for the last four cohorts) changed significantly, t(17) = 3.56, p = 0.002, d = 0.84.
Cohort effects
To assess whether outcomes improved over time as the intervention protocol was refined, we conducted a one way ANOVA on each variable that was available for all nine cohorts; we used a planned linear contrast with cohort number as the grouping variable. If the variable was measured at both pre and post assessment points, we used change scores rather than simply post-test scores. There were no significant effects for change scores on perceived stigma or stigmatizing attitudes believability, which is not surprising as these did not change from pre- to post-treatment in the overall analysis. However, change scores did increase over time for internalized shame, F(1, 7, 39) = 6.89, p = 0.01, and for overall mental health, F(1, 7, 39) = 4.17, p = 0.048. In addition, post assessment working alliance, F(1, 46) = 16.54, p < 0.001, and client satisfaction scores, F(1, 44) = 9.66, p = 0.003, increased over time.
Satisfaction and working alliance
Participants reported being generally satisfied with the intervention on the CSQ-3, M = 2.73 (SD = 0.78). Seventy-two percent of respondents reported being mostly or very satisfied with the workshop. About the same number, 71%, reported that were they to seek help again, they would be interested in returning to this same workshop. Forty-four percent reported that most or all of their needs were met by the program, while an additional 42% reported that some of their needs were met. The lower level of endorsement of this final question is perhaps not surprising given the length and limited focus of the workshop.
While as noted above, working alliance improved across groups, at post-intervention working alliance scores were M = 5.08 (SD = 1.23). These scores are also somewhat low, about one standard deviation on alliance below that found in a general outpatient sample in the fourth session of individual counseling (Busseri and Tyler 2003). However, the comparison may not be apt since this scale has apparently not been previously used to assess brief group therapies.
Relationships between outcomes and processes
While mediational analyses are not possible due to the lack of a control group, we did examine correlations between the only process variable to significantly change from pre- to post-intervention and that had an adequate sample size to run a correlation, the AAQ and our primary outcome variable, internalized shame. We did not have adequate sample size to look for relationships between process variables and internalized stigma. Post-treatment AAQ and shame scores were highly correlated, r(29) = 0.70, p < 0.0001, in cohorts 1–5. In order to focus on the impact of treatment, adjusting for baseline differences, we also examined the correlation between changes from pre to post on the AAQ and internalized shame and found that these were also strongly correlated, r(29) = 0.51, p < 0.01.
Discussion
This is the first study specifically designed to assess and reduce self-stigma in substance abusing populations. Although ACT has previously been shown in controlled studies to reduce stigmatizing attitudes toward persons in recovery (Hayes et al. 2004d), and to reduce actual substance use (Hayes et al. 2004e, 2004f), it has not previously been applied to self-stigma in any population.
This initial pilot study resulted in a manual that has promise in the reduction of self-stigma. Our sample showed fairly high initial levels of stigma, on par with those reported in the literature for patients with chronic mental illness (Link et al. 2002; Ritsher and Phelan 2004). During the week of intervention, we also found (using Cohen’s definition of effect sizes, (Cohen 1988) large pre- to post-treatment effects on measures of self-esteem and experiential avoidance, and medium sized effects on internalized shame, internalized stigma, general mental health, and social support from friends.
Interestingly, only some aspects of stigma changed during the week of intervention. Measures of internalized stigma, shame, and perceived stigma might all be considered aspects of self-stigma as we have defined it – shame, self-evaluative thoughts, and fear of enacted stigma that relate to membership in a stigmatized group. Perceived stigma did not change during the intervention period. This might suggest that perceived stigma is perhaps a less fruitful target for intervention or it might simply reflect that we did not intentionally target. Our intervention focused, however, on participants’ relationship to stigmatizing self evaluative thoughts and shame. The fact that shame and internalized stigma did decrease during the week of intervention suggests that these processes may be more amenable to change in this fashion.
While internalized stigma and shame decreased during the study, we did not adequately document that people’s relationship to shame changed, beyond the changes seen in scores on our measure of experiential avoidance. More work needs to be done on that front. The relationship between these variables and outcomes such as substance use and treatment attendance will be explored in larger follow on studies.
As reviewed above, ACT largely attempts to modify two specific processes, experiential avoidance and cognitive fusion. Measures of both of these constructs were included in this study and results were mixed. Changes in experiential avoidance, as measured by the AAQ, reached statistical significance. In addition, the level of experiential avoidance at post-treatment was highly correlated (r = 0.70) with our primary outcome variable, internalized shame, and change in these shame scores were moderately correlated with change in AAQ scores. While the lack of a control group does not permit mediational analysis, and thus alternative explanations besides mediation are plausible, these results consistent with other studies that have shown that the AAQ tends to improve significantly as a result of an ACT intervention (Hayes et al. 2006), and the AAQ has even been shown to mediate ACT outcomes in at least one study (Bond and Bunce, 2000). Conversely, the two measures of cognitive defusion included in this study did not change as a result of the intervention. It is not known whether the intervention was not successful in promoting defusion or whether the measures assessed thoughts that were not targeted by the intervention. The Stigmatizing Attitudes-Believability Scale was developed by asking drug and alcohol counselors to describe common stigmatizing attitudes towards clients, but these may not be the same thoughts that people in recovery have about themselves. The Believability of Reasons for Using Scale demonstrated a significant pre- to post-treatment change following ACT in a previous study, on the treatment of polysubstance abuse (Hayes et al. 2004e). However, in the present groups reasons for using were not directly targeted. More measurement development appears to be needed, both in terms of measures of stigma and the process of change that may impact it.
This study also presents interesting findings in relation to the study of shame in substance addiction. It is common lore in the addictions field that shame is an important part of addiction and a number of theorists have suggested that shame needs to be directly targeted in treatment (Dearing et al. 2005; Wiechelt 2007) In this study, we have shown that interventions can reduce internalized shame. However, in this study, while shame did go down at follow up, it’s also important to keep in mind that the target of the intervention was not the reduction of shame per se, but rather increasing participant’s acceptance of the feeling of shame and mindfulness of stigmatizing thoughts and evaluations. We hope that future studies on shame in addiction take into account people’s psychological relationship to shame rather than simply focusing on reducing the experience of shame. We believe that it may be the case that attempts to help people to ‘‘feel better’’ by directly attempting to reduce the experience of shame may not necessarily be helpful, but may actually serve to feed the addictive cycle. Exploration of this idea awaits future studies.
Methodological weaknesses of this study include the use of only self-report measures, the lack of a follow-up, the lack of a control group, and concurrent nonspecific treatment. Future studies should include more objective outcomes, such as drug use, employment status, or treatment attendance. Larger studies are also needed with a longer follow-up to assess durability of effects. Probably the biggest threat to the validity of these outcomes is the presence of ongoing concurrent treatment. Thus a viable alternative interpretation for all of the results obtained is that treatment in general, rather than the specific intervention, resulted in improved outcomes on all or some of the measures. However, the finding that the treatment development process appeared to result in larger effects over time suggests that some of these outcomes may not be solely due to nonspecific treatment effects since no significant changes occurred in the concurrent treatment program. We are not aware of any other study in the literature that has shown improved outcomes over time during a manual development process.
Visual inspection of the data showed an interesting pattern. Dr Hayes, the creator of ACT, was one of the co-leaders of the first two groups and these groups showed effect sizes on shame that corresponded to those of some of the later groups. Once others were leading the groups, the outcomes were initially of lower effect size, but later recovered to levels higher than those obtained by Dr Hayes in the initial two groups. These findings further suggest that ACT is a trainable technique that can be learned by others.
The absence of any extant literature on the treatment of self-stigma in substance abuse populations must be placed against the clear methodological weaknesses of this initial study. This study provides the first preliminary evidence that methods such as defusion, mindfulness, acceptance, and commitment to valued action may reduce self-stigma in a substance abuse population. Controlled studies of these methods are the next logical step.
Acknowledgments
This research was supported by grant #5 R21 DA017644 from The National Institute on Drug Abuse (PI: Barbara Kohlenberg). We would like to thank Jenna LeJeune, PhD for her helpful advice in reading early versions of this manuscript, Jody Eble for her dynamic presence, and the staff at Bristlecone Family Resources for supporting this project.
References
- Aviram RB, Brodsky BS, Stanley B. Borderline personality disorder, stigma, and treatment implications. Harvard Review of Psychiatry. 2006;14(5):249–256. doi: 10.1080/10673220600975121. [DOI] [PubMed] [Google Scholar]
- Bissett RT. Processes of change: Acceptance versus 12-step in polysubstance-abusing methadone clients. ProQuest Information & Learning. 2002;63(2):10146. [Google Scholar]
- Blascovich J, Tomaka J. Measures of self-esteem. In: Robinson John P, Shawer Philip R, Wrightsman Laurence S, editors. Measures of personality and social psychological attitudes. San Diego, CA, USA: Academic Press; 1991. pp. 115–160. [Google Scholar]
- Bond FW, Bunce D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. Journal of Occupation, Health and Psychologist. 2000;5(1):156–163. doi: 10.1037//1076-8998.5.1.156. [DOI] [PubMed] [Google Scholar]
- Burckhardt CS, Woods SL, Schultz AA, Ziebarth DM. Quality of life of adults with chronic illness: A psychometric study. Research in Nursing and Health. 1989;12(6):347–354. doi: 10.1002/nur.4770120604. [DOI] [PubMed] [Google Scholar]
- Busseri MA, Tyler JD. Interchangeability of the working alliance inventory and working alliance inventory, short form. Psychological Assessment. 2003;15(2):193–197. doi: 10.1037/1040-3590.15.2.193. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cook D. Internalized Shame Scale. 1989. [Google Scholar]
- Cook DR. Empirical studies of shame and guilt: The internalized shame scale. In: Nathanson Donald L, editor. Knowing feeling: Affect, script, and psychotherapy. New York: W W Norton & Co; 1996. pp. 132–165. [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. American Psychologist. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Penn DL. Lessons from social psychology on discrediting psychiatric stigma. American Psychologist. 1999;54(9):765–776. doi: 10.1037//0003-066x.54.9.765. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, River LP, Lundin RK, Wasowski KU, Campion J, Mathisen J, Goldstein H, Bergman M, Gagnon C, Kubiak MA. Stigmatizing attributions about mental illness. Journal of Community Psychology. 2000;28(1):91–102. [Google Scholar]
- Corrigan PW, Watson AC. The paradox of self-stigma and mental illness. Clinical Psychology-Science and Practice. 2002;9(1):35–53. [Google Scholar]
- Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: A review. Schizophrenia Bulletin. 2006;32:S44–S63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. British Journal of Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Sobell LC, Sobell MB, Agrawal S, Toneatto T. Barriers to Treatment – Why alcohol and drug-abusers delay or never seek treatment. Addictive Behaviors. 1993;18(3):347–353. doi: 10.1016/0306-4603(93)90036-9. [DOI] [PubMed] [Google Scholar]
- Dearing RL, Stuewig J, Tangney JP. On the importance of distinguishing shame from guilt: Relations to problematic alcohol and drug use. Addictive Behaviors. 2005;30(7):1392–1404. doi: 10.1016/j.addbeh.2005.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine P. Stereotypes and prejudice: Their automatic and controlled components. Journal of Personality and Social Psychology. 1989;56(1):5–18. [Google Scholar]
- Eifert G, Forsyth J. Acceptance and commitment therapy for anxiety disorders: A practitioner’s treatment guide to using mindfulness, acceptance, and values-based behavior change strategies. Oakland, CA: New Harbinger Publications; 2005. [Google Scholar]
- Flanagan JC. A research approach to improving our quality of life. American Psychologist. 1978;33(2):138–147. [Google Scholar]
- Gifford EV, Kohlenburg BS, Hayes SC. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35(4):689–705. [Google Scholar]
- Goldberg DP. The detection of psychiatric illness by questionnaire: A technique for the identification and assessment of non-psychotic psychiatric illness. Oxford, UK: Oxford University Press; 1972. [Google Scholar]
- Hayes SC, Barnes-Holmes D, Roche B. Advances in child development and behavior. San Diego, CA: Academic Press; 2001. Relational frame theory: A post-Skinnerian account of human language and cognition. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Bissett R, Roget N, Padilla M. The impact of acceptance and commitment training and multicultural training on the stigmatizing attitudes and professional burnout of substance abuse counselors. Behavior Therapy. 2004a;35(4):821–835. [Google Scholar]
- Hayes SC, Follette VM, Linehan MM. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York: Guilford Press; 2004b. [Google Scholar]
- Hayes SC, Luoma J, Bond F, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Masuda A, Bissett R, Luoma J, Guerro LF. DBT, FAR and ACT: How empirically oriented are the new behavior therapy technologies? Behavior Therapy. 2004c;35(1):35–54. [Google Scholar]
- Hayes SC, Smith S. Get out of your mind and into your life: The new acceptance and commitment therapy. Oakland, CA: New Harbinger; 2005. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, Polusny MA, Dykstra TA, Batten SV, Bergan J, Stewart SH, Zvolensky MJ, Eifert GH, Bond FW, Forsyth JP, Karekla M, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. Psychological Record. 2004d;54(4):553–578. [Google Scholar]
- Hayes SC, Strosahl KD. A practical guide to acceptance and commitment therapy. New York: Springer Science, Business Media; 2005. [Google Scholar]
- Hayes SC, Strosahl KD, Wlison KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV. A preliminary trial of twelve-step facilitation and acceptance and commitment therapy with polysubstance-abusing methadone-maintained opiate addicts. Behavior Therapy. 2004e;35(4):667–688. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV. A randomized controlled trial fo twelve-step facilitation and acceptance and commitment therapy with polysubstance abusing methadone maintained opiate addicts. Behavior Therapy. 2004f;35:667–688. [Google Scholar]
- Hingson R, Mangione T, Meyers A, Scotch N. Seeking help for drinking problems – a study in the Boston Metropolitan area. Journal of Studies on Alcohol. 1982;43(3):273–288. doi: 10.15288/jsa.1982.43.273. [DOI] [PubMed] [Google Scholar]
- Kelly CM, Jorm AF. Stigma and mood disorders. Current Opinion in Psychiatry. 2007;20(1):13–16. doi: 10.1097/YCO.0b013e3280113cf5. [DOI] [PubMed] [Google Scholar]
- Klingeman HKH. The Motivation for change from problem alcohol and heroin use. British Journal of Addictions. 1991;86:727–744. doi: 10.1111/j.1360-0443.1991.tb03099.x. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ. The relation of treatment fearfulness and psychological service utilization – an overview. Professional Psychology-Research and Practice. 1991;22(3):196–203. [Google Scholar]
- Langer EJ, Fiske S, Taylor SE, Chanowitz B. Stigma, staring, and discomfort – novel-stimulus hypothesis. Journal of Experimental Social Psychology. 1976;12(5):451–463. [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Eval Program Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Larson DG, Chastain RL. Self-concealment: Conceptualization, measurement, and health implications. Journal of Social & Clinical Psychology. 1990;9(4):439–455. [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, Kivlahan DR. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug and Alcohol Dependence. 2002;67(1):13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Schmidt H, 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. The American Journal on Addictions. 1999;8(4):279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Link BG. Understanding labeling effects in the area of mental-disorders – an assessment of the effects of expectations of rejection. American Sociological Review. 1987;52(1):96–112. [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. On describing and seeking to change the experience of stigma. Psychiatric Rehabilitation Skills. 2002;6(2):201–231. [Google Scholar]
- Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior. 1997;38(2):177–190. [PubMed] [Google Scholar]
- Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, Fisher G. An investigation of stigma in individuals receiving treatment for substance abuse. Addictive Behaviors. 2007;32(7):1331–1346. doi: 10.1016/j.addbeh.2006.09.008. [DOI] [PubMed] [Google Scholar]
- Macrae CN, Bodenhausen GV, Milne AB, Jetten J. Out of mind but back in sight – Stereotypes on the rebound. Journal of Personality and Social Psychology. 1994;67(5):808–817. [Google Scholar]
- Masuda A, Hayes SC, Sackett CF, Twohig MP. Cognitive defusion and self-relevant negative thoughts: Examining the impact of a ninety year old technique. Behaviour Research and Therapy. 2004;42(4):477–485. doi: 10.1016/j.brat.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Page S. Psychiatric stigma: Two studies of behaviour when the chips are down. Canadian Journal of Community Mental Health. 1983;2(1):13–19. [Google Scholar]
- Penn DL, Martin J. The stigma of severe mental illness: Some potential solutions for a recalcitrant problem. Psychiatric Quarterly. 1998;69(3):235–247. doi: 10.1023/a:1022153327316. [DOI] [PubMed] [Google Scholar]
- Penn DL, Ritchie M, Francis J, Combs D, Martin J. Social perception in schizophrenia: The role of context. Psychiatry Research. 2002;109(2):149–159. doi: 10.1016/s0165-1781(02)00004-5. [DOI] [PubMed] [Google Scholar]
- Perlick DA, Rosenheck RA, Clarkin JF, Sirey JA, Salahi J, Struening EL. Adverse effects of perceived stigma on social adaptation of persons diagnosed with bipolar affective disorder. Psychiatric Services. 2001;52(12):1627–1632. doi: 10.1176/appi.ps.52.12.1627. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research. 2003;121(1):31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257–265. doi: 10.1016/j.psychres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Rosenfield S. Labeling mental illness: The effects of received services and perceived stigma on life satisfaction. American Sociological Review. 1997;62(4):660–672. [Google Scholar]
- Scambler G. Stigma and disease: Changing paradigms. Lancet. 1998;352(9133):1054–1055. doi: 10.1016/S0140-6736(98)08068-4. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams JM, Gemar MC. The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology & Psychotherapy. 2002;9(2):131–138. [Google Scholar]
- Smart L, Wegner DM. Covering up what can’t be seen: Concealable stigma and mental control. Journal of Personality and Social Psychology. 1999;77(3):474–486. doi: 10.1037//0022-3514.77.3.474. [DOI] [PubMed] [Google Scholar]
- Smart L, Wegner DM. The hidden costs of hidden stigma. In: Heatherton Todd F, Kleck Robert E, Hebl Michelle R, Hull Jay G, editors. The social psychology of stigma. New York: Guilford Press; 2000. pp. 220–242. [Google Scholar]
- SPSS IS. SPSS v12.0.1. Chicago, IL: SPSS, Inc; 2003. [Google Scholar]
- Starr S, Campbell LR, Herrick CA. Factors affecting use of the mental health system by rural children. Issues in Mental Health Nursing. 2002;23(3):291–304. doi: 10.1080/016128402753543027. [DOI] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic AM. Factor structure of the working alliance inventory. Psychological Assessment. 1989;1(3):207–210. [Google Scholar]
- Tuchfeld BS. Spontaneous remission in alcoholics – Empirical observations and theoretical implications. Journal of Studies on Alcohol. 1981;42(7):626–641. doi: 10.15288/jsa.1981.42.626. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Gladsjo JA. Environmental events surrounding natural recovery from alcohol-related problems. Journal of Studies on Alcohol. 1994;55(4):401–411. doi: 10.15288/jsa.1994.55.401. [DOI] [PubMed] [Google Scholar]
- Vieweg BW, Hedlund JL. The general health questionnaire (GHQ): A comprehensive review. Journal of Operational Psychiatry. 1983;14(2):74–81. [Google Scholar]
- Wahl OF. Mental health consumers’ experience of stigma. Schizophrenia Bulletin. 1999;25(3):467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- Wenzlaff RM, Wegner DM. Thought suppression. Annual Review of Psychology. 2000;51:59–91. doi: 10.1146/annurev.psych.51.1.59. [DOI] [PubMed] [Google Scholar]
- Wiechelt SA. The specter of shame in substance misuse. Substance Use & Misuse. 2007;42(2):399–409. doi: 10.1080/10826080601142196. [DOI] [PubMed] [Google Scholar]
- Wright ER, Gronfein WP, Owens TJ. Deinstitutionalization, social rejection, and the self-esteem of former mental patients. Journal of Health and Social Behavior. 2000;41(1):68–90. [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Ziment SG, Farley GK. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]