Abstract
Mild traumatic brain injury (mTBI), the signature injury of the recent wars in Afghanistan and Iraq, is a prevalent and potentially debilitating condition that is associated with symptoms of post-traumatic stress/post-traumatic stress disorder (PTS/PTSD). Prior mTBI, severity and type of injury (blast vs. non-blast), and baseline psychiatric illness are thought to impact mTBI outcomes. It is unclear if the severity of pre-morbid PTS/PTSD is a risk factor of post-injury levels of PTS and mTBI symptoms. The objective of the study was to examine predictors of post-injury PTS/PTSD, including pre-morbid PTS symptoms, and physical and cognitive symptoms in the sub-acute phase (1 week-3 months) following an acute mTBI. A retrospective review of medical records was performed of 276 servicemen assigned to the United States Army Special Operations Command referred for mTBI evaluation between December 2009 and March 2011. Post-Concussion Symptom Scale and PTSD Checklist scores were captured pre- and post-injury. A total of 276 records were reviewed. Pre-morbid and post-injury data were available for 91% (251/276). Of the 54% (136/251) of personnel with mTBI, 29% (39/136) had positive radiology findings and 11% (15/136) met criteria for clinical PTS symptoms at baseline. Logistic regression analysis found baseline PTS symptoms predicted personnel who met clinical levels of PTSD. Receiver operating characteristic curve analysis revealed that baseline PTS (p = 0.001), baseline mTBI symptoms (p = 0.001), and positive radiology (magnetic resonance imaging or computed tomography) findings for complicated mTBI (p = 0.02) accurately identified personnel with clinical levels of PTSD following mTBI. Years of military service, combat deployment status, age, and injury mechanism (blast vs. non-blast) were not associated with increased risk of PTS following mTBI. Pre-morbid PTS symptoms are associated with an increased risk for clinical levels of PTS following a subsequent mTBI. Symptom severity and positive radiologic findings may amplify this risk. At-risk personnel may benefit from early identification and intervention.
Keywords: : blast, concussion, mTBI, PTSD
Introduction
United States military personnel have experienced more than 250,000 mild traumatic brain injuries (mTBIs) between 2000 and 2014.1 Mild TBI has been recognized as the “signature injury” of the wars in Afghanistan and Iraq, with nearly a quarter of deployed military personnel experiencing one or more mTBIs.2 The direct cost associated with care for this injury among U.S. military veterans is estimated to be more than $646 million annually.3 Symptoms following mTBI are well documented and span multiple domains, including physical (headache, tinnitus, dizziness), cognitive (memory, concentration), and behavioral (depression, anxiety, irritability).4–7 Functional impairments following mTBI include cognitive function (memory, decision making, attention), vestibular, and oculomotor/visual (spatial processing, vergence dysfunction) deficits.4,8–12 One of the more problematic outcomes associated with mTBI in military personnel is post-traumatic stress (PTS) symptoms and post-traumatic stress disorder (PTSD), which occur in nearly 40% of personnel with mTBI exposure.13 In fact, researchers have reported that post-injury PTSD is more highly associated with mTBI than with any other injury.4,14
It is difficult to distinguish PTS symptoms from chronic symptoms of mTBI, known as post-concussive syndrome (PCS), which is defined by persistent mTBI symptoms beyond 3 months. The severity and incidence of persistent symptoms is variable in the literature, but is reported to be as high as 10 to 20% of military individuals with mTBI.15,16 Both PTS symptoms and PCS are marked by similar symptoms, including anxiety, insomnia, memory problems, agitation, and irritability.17 Some researchers have suggested that PTS symptoms and concurrent psychiatric illness, as opposed to the repercussions from mTBI itself, may account for the chronic symptoms reported by many military personnel returning from a combat zone.4,18,19
Pre-morbid psychosocial factors are also known to interact with injury characteristics to influence symptomatology after mTBI. For instance, younger personnel (< 25 years) were more likely than older personnel (> 25 years) to meet PTSD criteria at 1 month post-injury.20 Pre-injury PTS symptom severity, as well as combat intensity, were both predictive of post-injury rates of PTSD at 3 months post-deployment.21 Incidence of injury also varies with rank, occurring twice as often in junior enlisted personnel than senior officers.22 Further, cumulative effects of multiple mTBIs are well documented,6,23 suggesting potential for greater impairment and symptoms in those with greater exposure time (i.e., deployment duration), though not necessarily longer time in service. Chapman and Diaz-Arrastia24 noted that mTBI occurring in combat theater is inherently different than other injuries, with increased obstacles to injury reporting, occurrence of injury within prolonged missions, and greater psychological stress surrounding the injury. Recently, researchers also have indicated that the type of mTBI may play a role in the development and character of PTS symptoms. For instance, one study reported that blast injuries were associated with increased flashbacks and nightmares but not with other PTS symptoms.25
Overall, research comparing blast to non-blast (i.e., blunt) mTBI has been equivocal. Several studies have reported no difference in PTS symptoms between personnel exposed to blast mTBI and those exposed to non-blast mTBI.26–28 In contrast, other studies have supported an association between rates of PTS and clinical PTSD and exposure to blast mTBI.4,23,25,29,30 Most research has focused on PTS symptoms at several months to years after exposure to blast mTBI.29,30 However, researchers have not focused on PTS symptoms in the sub-acute (1 week to 3 months) time period following exposure to blast mTBI.26 In a recent prospective study utilizing a clinical evaluation of military personnel 6–12 months post-injury, similar neurocognitive performance, as well as rates of clinical PTSD, were reported for both blast and blunt mTBI.27
In summary, the previous findings suggest that blast mTBI is associated with PTSD in military personnel. Evidence also suggests that the risk of sustaining mTBI and subsequent development of PTS symptoms is related to demographic factors, including age, total length of deployments, and previous blast mTBI, as well as presence of baseline psychiatric illness. However, little is known about the role of pre-morbid PTS and mTBI symptoms or the severity of mTBI with regard to subsequent clinical levels of PTS symptoms. The objective of the current study was to determine if pre-morbid factors, including select demographics (age, length of deployment, years in service, prior exposure to mTBI), injury characteristics (blast vs. blunt, severity) and baseline PTS and mTBI symptoms were associated with clinical levels of PTS symptoms following mTBI. We expected that higher levels of baseline PTS and mTBI symptoms would be associated with greater incidence of clinical PTS levels following mTBI. Further, we expected that exposure to current or previous blast mTBI and a greater severity of injury, marked by positive radiological (i.e., computed tomography [CT] or magnetic resonance imaging [MRI]) findings for complicated mTBI, would be associated with higher rates of clinical levels of PTS symptoms.
Methods
Between December 2009 and March 2011, we collected consecutive electronic medical record (EMR) data for 276 U.S. Army Special Operations Command (USASOC) personnel who were referred for an initial evaluation for a suspected mTBI within 1 week to 3 months of injury. An mTBI was defined as a head injury with a Glasgow Coma Scale (GCS) score of 13–15 with reported symptoms and/or observed signs or impairment related to the injury. We de-limited our sample to less than 3 months post-injury, as beyond this time period represents diagnostic criteria for post-concussion syndrome (PCS).
Medical personnel from USASOC headquarters organized and aggregated de-identified data for the study from existing EMRs. Data obtained included demographic data (age, sex, total months deployed, and total years of military service) and data on mTBI events to include number and type (blast, blunt, combination). Only medically-diagnosed previous mTBIs that occurred during military service and appeared in the EMR were included. Additionally, PTS symptom data and mTBI symptom data were obtained from PTSD Checklist (PCL) and Post-Concussion Symptom Scale (PCSS) documentation found in EMRs. Data were collected during the study period from consecutive patients treated in deployed (i.e., Afghanistan, Iraq) and training (i.e., Fort Benning, Georgia; Fort Bragg, North Carolina; Fort Lewis, Washington) locations. The study was approved by the institutional review boards at the University of Pittsburgh, Pennsylvania and Womack Army Medical Center, North Carolina using an exempt de-identified medical records protocol.
The PCL assesses self-reported PTS symptoms. The PCL encompasses 17 items and requires individuals to indicate on a scale of 1 (not at all) to 5 (extremely) how much each item bothered them during the past month. The PCL yields a PTSD symptom score that ranges from 17–85. Clinical PTSD cut-offs for the PCL were set at 28 or higher per current guidelines for recent veterans of combat in Afghanistan and Iraq.25,31
The PCSS assesses mTBI symptoms. The PCSS contains 22 self-report mTBI symptoms (e.g., headache, fogginess, dizziness) rated on a 0- (none) to 6- (severe) point Likert scale. The total PCSS score ranges from 0–132.
Chi-square and independent Mann-Whitney U tests were used to assess differences between groups on demographic variables. A logistic regression was performed using the enter method for multiple independent variables that predict PTS. A receiver operating characteristic (ROC) curve with area under the curve (AUC) analysis was used to determine the diagnostic utility of pre-morbid and post-injury variables for PTS. All analyses were conducted using SPSS version 22.
Results
Population
A total of 276 records were reviewed. Complete pre-morbid and post-injury data were available for 91% (251/276) of personnel who were then identified for inclusion in the study. A total of 40% (100/251) of patients included in the study were determined by USASOC medical personnel not to have mTBI. The mechanism of injury was unknown for 6% (15/251) of patients. The remaining 54% (136/251) of patients were diagnosed with mTBI. The demographics for the sample are representative of the overall USASOC population.23 The average age for the sample was 28.9 (standard deviation [SD] = 6.1). Of patients with mTBI, a total of 26% (35/136) were deployed at the time of their evaluation. Two PTS groups were created based on PCL score (< 28 and ≥28)23 to examine which variables predicted clinical levels of PTSD. Only 11% (15/136) of patients met the criteria for clinically significant PTSD symptoms (a PCL score above the threshold value). A summary of key demographic data for the entire sample, as well as each PTS group, are provided in Table 1. Results of chi-square and Mann Whitney U tests indicated that the positive screen PTSD group (PCL >28) had a greater number of personnel with migraine history, compared with the no PTSD group (40% [6/15] vs. 1.7% [2/121]; p < 0.05). The groups did not differ on any other demographic variables.
Table 1.
Summary of Demographic Data for the Total Sample (N = 136) and Clinical PTS Sub-Groups
| Clinical PTS (n = 15) M (SD) Range | No PTS (n = 121) M (SD) Range | Total sample (N = 136) M (SD) Range | |
|---|---|---|---|
| Age | 29.5 (5.0) 21–37 |
28.9 (6.2) 18–47 |
29.0 (6.1) 18–47 |
| Height (cm) | 178.0 (6.9) 165.1–193.0 |
179.2 (6.8) 165.1–193.0 |
179.1 (6.8) 165.1–193.0 |
| Weight (kg) | 83.8 (12.7) 65.8–108.4 |
85.2 (10.3) 65.3–122.5 |
85.1 (10.5) 65.3–122.5 |
| Total years of service | 7.6 (4.9) 1–18 |
7.4 (5.5) 0–23 |
7.4 (5.4) 0–23 |
| Total months deployed | 17.3 (17.3) 0–48 |
13.5 (12.0) 0–43 |
13.9 (12.6) 0–48 |
| Currently deployed % yes (n) | 11.8% (4) |
25.6% (31) |
25.7% (35) |
| Total previous mTBIs | 1.3 (1.7) 0–5 |
0.8 (1.0) 0–5 |
0.9 (1.1) 0–5 |
| mTBI history % yes (n) | 57.1% (8) |
54.9% (67) |
55.1% (75) |
| Migraine history % yes (n) | 42.9% (6)* |
1.7% (2) |
5.9% (8) |
p < 0.05.
PTS, post-traumatic stress; M, mean; SD, standard deviation; mTBI, mild traumatic brain injury.
Mild traumatic brain injury and post-traumatic stress
Of personnel with mTBI, 32% (43/136) were from blast, 57% (77/136) were from blunt, and 11% (16/136) were from combined blast-blunt injury mechanisms. The time from injury to medical evaluation of that injury ranged from 1 week to 3 months. Glasgow Coma Scale scores for all mTBIs ranged from 13–15, and 29% (40/136) of patients had a positive radiology finding (i.e., bleed, contusion) related to their injury on CT or MRI. The PCL scores following mTBI for the overall sample ranged from 17–67, with a mean of 20.9 (SD = 9.2). As expected, the positive screen PTSD group had a higher (p < 0.001) PCL score (mean = 41.8, SD = 12.3, range = 28–67) than the no PTSD group (mean = 18.7, SD = 4.7, range = 16–27).
Predictors of post-traumatic stress
Results of a logistic regression using an enter method supported a model that accounted for 77% of the variance between the two PTSD groups (Nagelkerke R2 = 0.77, χ2[8] = 63.3, p < 0.001). The resulting model had 79% sensitivity in predicting personnel with clinical levels of PTSD symptoms (PCL ≥28) and 98% specificity predicting personnel without clinical levels of PTSD symptoms (PCL <28). Significant predictors in the model included positive radiology findings for complicated mTBI (adjusted odds ratio [OR] = 79.40) and PTS scores at baseline (adjusted OR = 1.42; Table 2).
Table 2.
Summary of Results of a Logistic Regression for Select Demographic, Pre-Injury, and Injury Predictors on Clinical Levels of PTSD (n = 136)
| B (SE) | Adjusted OR | 95% CI | p | |
|---|---|---|---|---|
| Constant | −14.51 (5.98) | |||
| Age | 0.08 (0.12) | 1.08 | 0.86–1.35 | .52 |
| Years of service | −0.84 (0.48) | 0.43 | 0.17–1.10 | .08 |
| Total months Deployed | 0.17 (0.10) | 1.19 | 0.97–1.45 | .10 |
| Baseline mTBI Symptoms | 0.09 (0.06) | 1.09 | 0.97–1.23 | .14 |
| Baseline PTS Symptoms | 0.35 (0.16) | 1.42 | 1.04–1.94 | .02 |
| Previous history of blast/combo mTBI | −1.81 (1.56) | 0.17 | 0.01–3.51 | 0.25 |
| Current mTBI Mechanism (blast/combo) | −2.02 (1.55) | 0.13 | 0.01–2.75 | 0.19 |
| Positive radiology results | 4.37 (2.19) | 79.40 | 1.09–5766.03 | 0.04 |
PTSD, post-traumatic stress disorder; B, coefficient; SE, standard error; OR, odds ratio; CI, confidence interval; mTBI, mild traumatic brain injury; PTS, post-traumatic stress.
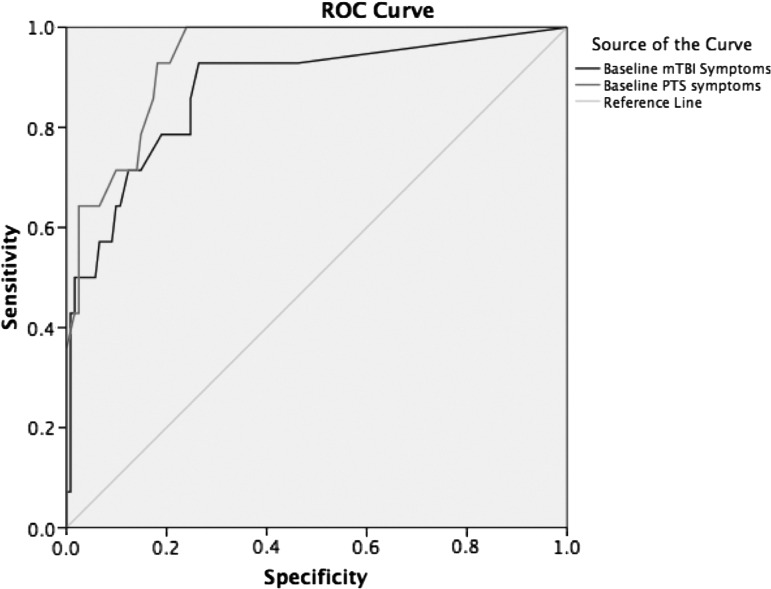
Results from the ROC curve analysis revealed that baseline PTS (p = 0.001) and baseline mTBI symptom scores (p = 0.001) and positive radiology findings for complicated mTBI (p = 0.02) accurately identified personnel with clinical levels of PTSD following mTBI. The AUCs were 0.94 for PTS symptom scores, 0.88 for mTBI symptom scores, and 0.70 for positive radiology results for complicated mTBI (Table 3). A PTS total symptom score cut-off of 22.5 on the PCL resulted in 93% sensitivity and 83% specificity for identifying PTSD following mTBI (Fig. 1). A total mTBI symptom score cut-off of 13.5 on the PCSS resulted in 80% sensitivity and 81% specificity for clinical levels of PTSD (Fig. 1). None of the other variables were significant in identifying clinical levels of PTSD following mTBI, including years of military service, combat deployment status, age, and injury mechanism.
Table 3.
AUC, 95% CI, and p Values from the ROC Curve Analysis for Select Demographic, Pre-Injury, and Injury Predictors on Clinical Levels of PTSD (n = 136)
| AUC | 95% CI | p | |
|---|---|---|---|
| Age | 0.57 | 0.42–0.71 | 0.43 |
| Years of service | 0.54 | 0.38–0.71 | 0.62 |
| Total months Deployed | 0.54 | 0.37–0.71 | 0.62 |
| Baseline mTBI Symptoms | 0.88 | 0.77–0.98 | 0.001 |
| Baseline PTS Symptoms | 0.94 | 0.89–0.99 | 0.001 |
| Previous history of blast/combo mTBI | 0.43 | 0.28–0.58 | 0.41 |
| Current mTBI Mechanism (blast/combo) | 0.49 | 0.33–0.65 | 0.92 |
| Positive radiology results | 0.70 | 0.54–0.85 | 0.02 |
AUC, area under the curve; CI, confidence interval; ROC, receiver operator characteristic; PTSD, post-traumatic stress disorder; mTBI, mild traumatic brain injury; PTS, post-traumatic stress.
FIG. 1.
Receiver operating characteristic (ROC) curve analysis of post-traumatic stress (PTS) and mild traumatic brain injury (mTBI) symptom scores for clinical levels of post-traumatic stress disorder (reference line = 0.50 probability).
Discussion
This study was novel in its examination of the role of pre-morbid PTS and mTBI symptoms, demographic factors, and mTBI characteristics on clinical levels of PTS following mTBI in military personnel. The key finding was that pre-morbid mTBI and PTS symptoms, together with positive radiological findings for complicated mTBI, were significant predictors of clinical levels of PTS symptoms following mTBI. The findings from a ROC curve analysis identified a PTS total symptom score cut-off of 22.5 on the PCL and a total mTBI symptom score cut-off of 13.5 on the PCSS as providing high levels of both sensitivity (93%, 80%) and specificity (83%, 81%) for clinical levels of PTS symptoms. Demographic factors including age, years of service, and total months deployed were not associated with increased risk for clinical levels of PTS following mTBI. In addition, neither a blast mTBI injury mechanism for the current injury nor a history of exposure to blast mTBI were associated with increased risk for clinical levels of PTS symptoms.
We found that both pre-morbid psychiatric illness and mTBI symptoms are predictors of subsequent levels of PTS. This expands on prior research suggesting that psychiatric illness is a prognostic variable for post-injury outcomes, including development of PCS.5,18,19 However, our results also identified symptoms of mTBI in the acute and sub-acute time period as an independent risk factor for the development of post-injury PTSD. Notably, in our cohort, sub-clinical levels of PTS symptoms (i.e., scores >22.5 vs. established criteria of >28 for a positive screen) accurately predicted post-mTBI levels of PTS symptoms. Based on our results, we suggest that pre-morbid PTS, as well as post-mTBI symptoms, should be clinically correlated as prognostic markers for PTSD.
In our study, severity of mTBI, as indicated by positive radiological findings for complicated mTBI, was associated with a greater incidence of clinical levels of PTS symptoms following mTBI. This finding is consistent with previous research that has indicated that other markers of injury severity associated with increased post-mTBI symptoms (including loss of consciousness and post-traumatic amnesia) may be confounded by recall bias.2,32 From a clinical perspective, positive findings on CT or MRI represent a potential objective marker for identifying military personnel at increased risk for clinical levels of PTS symptoms following mTBI.
The current findings also add to recent literature indicating that mechanism of injury—blast vs. non-blast—is unrelated to clinical levels of PTS symptoms following mTBI in military personnel.26–28 Notably, we measured PTS symptoms within the sub-acute time period (1 week to 3 months) following mTBI, which is earlier than in prior studies that reported an effect of blast mTBI on subsequent PTSD.29,30 Perhaps there is a progressive component to the effects of blast mTBI on PTS symptoms that results in a subset of military personnel with chronic clinical levels of PTS that fall outside of the sub-acute time period. Therefore, blast mTBI may be associated with clinical levels of PTS when assessed after a longer follow-up interval than in the current study, as reported previously.4,23,25,29,30 There also may be a dose–response relationship between blast exposures and PTS symptoms, as indicated in two recent studies.6,23 Additional prospective research is warranted to determine if there is a specific blast mTBI exposure threshold associated with increased risk for development of PTS.
Although years of military service was not significantly associated with post-injury symptoms, we observed a trend toward less PTS symptoms with longer total years of service. Presumably, this reflects resiliency of personnel who are able to cope, wisdom through experience that helps individuals avoid injury, or an inherent physiological difference and selection process by which some individuals are impacted less given the same injury exposure. However, this also may reflect evolving occupational duties with professional advancement over time and a decreased risk of injury exposure and proximity to exposure. In addition, most personnel assigned to USASOC undergo some type of assessment and selection process that leads to a more resilient soldier population. In contrast to our hypothesis, deployment status at the time of injury was not prognostic for increased clinical levels of PTS symptoms. Combat zone injuries are typically associated with greater emotional trauma24; however, our cohort did not show increased rates of clinical levels of PTS symptoms after mTBI while actively deployed. One explanation for this lack of difference may be variable exposure to emotional trauma resulting from different levels of combat intensity encountered by military personnel,5,18 as well as the variable degree of associated pain and subsequent treat of that pain.
Strengths, limitations, and future research
A notable strength of this study is the inclusion of both pre- and post-injury assessments allowing comparison within individuals and analysis of baseline predictive features. The use of baseline measures allowed comparison of outcomes for those with and without PTS symptoms. Another strength of the study is our cohort, which was comprised of only those with a formal diagnosis of mTBI based on clinical review by a medical provider and not solely on self-reported history.
The potential limitations of this study are related to our limited sample size. Although the initial sample size of 136 military personnel with mTBI was substantial, only 15 of the subjects reported PTS symptoms at a clinical cut-off level. As a result, our group of cases with clinical levels of PTS symptoms was small and may not represent the overall populations of USASOC or the U.S military as a whole. Our use of logistic regression with a relatively small sample size is potentially biased toward higher ORs, such as the one reported for positive radiologic findings in the current study. However, as Nemes and colleagues33 suggest, this bias may be considered to be small when compared with the standard error of the value in question. Other limitations are related to our selected follow up time interval of 7 days to 3 months, which allowed us to define sub-acute symptoms after injury, but was too short an interval for a discussion on chronic symptoms and long-term sequelae (i.e., years after injury). We do not know if any personnel developed PTSD subsequent to our research interval. We also did not examine acute (< 7days post-injury) characteristics in our study; therefore, immediate symptom reporting was not assessed.
Future research should include a longer follow-up interval to examine if the predictors of post-mTBI PTS symptoms—namely baseline PTS symptoms, mTBI symptoms, and positive radiology findings—are also predictive of outcomes in the chronic (> 3-month) time period. A future study allowing for expanded data approaches would clarify the relationship between baseline and post-mTBI PTSD status. Further modifier analyses of combat intensity and exposure on PTS symptoms also are warranted.
Conclusion
Overall, our results indicate that pre-morbid PTS symptoms are associated with an increased likelihood for the development of clinical levels of PTS following a subsequent mTBI. Our data reinforce previous efforts, which have indicated that military personnel with prior psychiatric symptoms are at greater risk for development of clinical levels of PTS symptoms following exposure to mTBI.21,34–36 Our findings suggest that this increased risk may be compounded by pre-morbid mTBI symptom severity and positive radiologic findings for complicated mTBI. Surprisingly, our findings did not support worse PTS-related outcomes associated with a current or previous history of blast mTBI. From a clinical perspective, the current findings may help identify, using both pre-morbid and post-mTBI information, at-risk military personnel who might benefit from early intervention to minimize the effects or prevent the development of clinical levels of PTS following mTBI.
Author Disclosure Statement and Funding Acknowledgments
Dr. Collins owns a 10% share in ImPACT Applications, Inc. With regard to the study data, Dr. Collins was not involved in the data collection, entry, or analysis; he was only involved in the data interpretation. This research was supported in part by grants to the University of Pittsburgh from the National Institute on Deafness and Other Communication Disorders (1K01DC012332-01A1) to Dr Kontos, and from the US Special Operations Command Biomedical Initiatives Steering Committee to Dr. Kontos and Dr. Collins.
The views expressed herein are those of the authors and do not reflect the officialpolicy of the Department of the Army, Department of Defense, or the US Government. Citations of commercial products or organizations do not constitute an official Department of Defense endorsement or approval of the products or services of these organizations.
This report was approved for public release by the US Army Special Operations Command Operational Security Office and Public Affairs Office.
References
- 1.Department of Defense Worldwide TBI Numbers. (2014). DoD Numbers for Traumatic Brain Injury. Available at: http://dvbic.dcoe.mil/dod-worldwide-numbers-tbi Accessed February20, 2016
- 2.O'Neil M., Carlson K., Storzbach D., Brenner L., Freeman M., Quiñones A., Motu'apuaka M., Ensley E., and Kansagara D. (2013). Complications of Mild Traumatic Brain Injury in Veterans and Military Personnel: A Systematic Review. Department of Veterans Affairs: Washington, D.C. [PubMed] [Google Scholar]
- 3.Boyle E., Cancelliere C., Hartvigsen J., Carroll L.J., Holm L.W., and Cassidy J.D. (2014), Systematic review of prognosis after mild traumatic brain injury in the military: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 95(3 Suppl), S230–S237 [DOI] [PubMed] [Google Scholar]
- 4.Belanger H.G., Proctor-Weber Z., Kretzmer T., Kim M., French L.M., and Vanderploeg R.D. (2011). Symptom complaints following reports of blast versus non-blast mild TBI: does mechanism of injury matter? Clin. Neuropsychol. 25, 702–715 [DOI] [PubMed] [Google Scholar]
- 5.Hoge C.W., McGurck D., Thomas J.L., Cox A.L., Engel C.C., and Castro C.A. (2008). Mild traumatic brain injury in U.S. soldiers returning from Iraq. N. Engl. J. Med. 358, 453–463 [DOI] [PubMed] [Google Scholar]
- 6.Reid M.W., Miller K.J., Lange R.T., Cooper D.B., Tate D.F., Bailie J., Brickell T.A., French L.M., Asmussen S., and Kennedy J.E. (2014). A multisite study of the relationships between blast exposures and symptom reporting in a post-deployment active duty military population with mild traumatic brain injury. J. Neurotrauma 31, 1899–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryan L.M. and Warden D.L. (2003). Post concussion syndrome. Int. Rev. Psychiatry 15, 310–316 [DOI] [PubMed] [Google Scholar]
- 8.Belanger HG, Spiegel E, and Vanderploeg RD. (2010). Neuropsychological performance following a history of multiple self-reported concussions: a meta-analysis. J. Int. Neuropsychol. Soc. 16,262–267 [DOI] [PubMed] [Google Scholar]
- 9.Drew A.S., Langan J., Halterman C., Osternig L.R., Chou L.S., and van Donkelaar P. (2007). Attentional disengagement dysfunction following mTBI assessed with the gap saccade task. Neurosci. Lett. 417, 61–65 [DOI] [PubMed] [Google Scholar]
- 10.Hoffer M.E., Balaban C., Gottshall K., Balough B.J., Maddox M.R., and Penta J.R. (2010). Blast exposure: vestibular consequences and associated characteristics. Otol. Neurotol. 31, 232–236 [DOI] [PubMed] [Google Scholar]
- 11.Mendez M.F., Owens E.M., Reza Berenji G., Peppers D.C., Liang L.J., and Licht E.A. (2013). Mild traumatic brain injury from primary blast vs. blunt forces: post-concussion consequences and functional neuroimaging. NeuroRehabilitation 32, 397–407 [DOI] [PubMed] [Google Scholar]
- 12.Thiagarajan P., Ciuffreda K.J., and Ludlam D.P. (2011). Vergence dysfunction in mild traumatic brain injury (mTBI): a review. Ophthalmic Physiol. Opt. 31, 456–468 [DOI] [PubMed] [Google Scholar]
- 13.Carlson K.F., Kehle S.M., Meis L.A., Greer N., Macdonald R., Rutks I., Saye,r N.A., Dobscha S.K., and Wilt TJ. (2011). Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: a systematic review of the evidence. J. Head Trauma Rehabil. 26, 103–115 [DOI] [PubMed] [Google Scholar]
- 14.Schneiderman A.I., Braver E.R., and Kang H.K. (2008). Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. Am. J. Epidemiol. 167, 1446–1452 [DOI] [PubMed] [Google Scholar]
- 15.Karr J.E., Areshenkoff C.N., and Garcia-Barrera M.A. (2014). The neuropsychological outcomes of concussion: a systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology 28, 321–336 [DOI] [PubMed] [Google Scholar]
- 16.Ruff R. Two decades of advances in understanding of mild traumatic brain injury. (2005). J Head Trauma Rehab. 20, 5–18 [DOI] [PubMed] [Google Scholar]
- 17.Stein M.B. and Mcallister T.W. (2009). Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am. J. Psychiatry 166, 768–776 [DOI] [PubMed] [Google Scholar]
- 18.Cooper D.B., Kennedy J.E., Cullen M.A., Critchfield E., Amador R.R., and Bowles A.O. (2011). Association between combat stress and post-concussive symptom reporting in OEF/OIF service members with mild traumatic brain injuries. Brain Inj, 25, 1–7 [DOI] [PubMed] [Google Scholar]
- 19.Wilk J.E., Herrell R.K., Wynn G.H., Riviere L.A., and Hoge C.W. (2012). Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom. Med. 4, 249–257 [DOI] [PubMed] [Google Scholar]
- 20.Grieger T., Cozza S., and Ursano R. (2006). Posttraumatic stress disorder and depression in battle-injured soldiers. Am. J. Psychiatry 163, 1777–1783 [DOI] [PubMed] [Google Scholar]
- 21.Yurgil K.A., Barkauskas D.A., Vasterling J.J., Nievergelt C.M., Larson G.E., Schork N.J., Litz B.T., Nash W.P., and Baker D.G.; Marine Resiliency Study Team. (2014). Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty Marines. JAMA Psychiatry, 71, 149–157 [DOI] [PubMed] [Google Scholar]
- 22.Cameron K.L., Marshall S.W., Sturdivant R.X., and Lincoln A.E. (2012). Trends in the incidence of physician-diagnosed mild traumatic brain injury among active duty U.S. military personnel between 1997 and 2007. J. Neurotrauma 29, 1313–1321 [DOI] [PubMed] [Google Scholar]
- 23.Kontos A.P., Kotwal R.S., Elbin R., Lutz R.H., Forsten R.D., Benson P.J., and Guskiewicz K.M. (2012). Residual effects of combat-related mild traumatic brain injury. J. Neurotrauma 30, 680–686 [DOI] [PubMed] [Google Scholar]
- 24.Chapman J.C. and Diaz-Arrastia R. (2014). Military traumatic brain injury: a review. Alzheimers Dement. 10(3 Suppl), S97–S104 [DOI] [PubMed] [Google Scholar]
- 25.Kennedy J.E., Leal F.O., Lewis J.D., Cullen M.A., and Amador R.R. (2010). Posttraumatic stress symptoms in OIF/OEF service members with blast-related and non-blast-related mild TBI. NeuroRehabilitation, 26, 223–231 [DOI] [PubMed] [Google Scholar]
- 26.Luethcke C.A., Bryan C.J., Morrow C.E., and Isler W.C. (2011). Comparison of concussive symptoms, cognitive performance, and psychological symptoms between acute blast-versus nonblast-induced mild traumatic brain injury. J. Int. Neuropsychol. Soc. 17, 36–45 [DOI] [PubMed] [Google Scholar]
- 27.MacDonald C.L., Johnson A.M., Wierzechowski L., Kassner E., Stewart T., Nelson E.C., Werner N.J., Zonies D., Oh J., Fang R., and Brody D.L. (2014). Prospectively assessed clinical outcomes in concussive blast vs nonblast traumatic brain injury among evacuated US military personnel. JAMA Neurol. 71, 994–1002 [DOI] [PubMed] [Google Scholar]
- 28.Wilk J.E., Thomas J.L., McGurk D.M., Riviere L.A., Castro C.A., and Hoge C.W. (2010). Mild traumatic brain injury (concussion) during combat: lack of association of blast mechanism with persistent postconcussive symptoms. J. Head Trauma Rehabil. 25, 9–14 [DOI] [PubMed] [Google Scholar]
- 29.Belanger H.G., Kretzmer T., Yoash-Gantz R., Pickett T., and Tupler L.A. (2009). Cognitive sequelae of blast-related versus other mechanisms of brain trauma. J. Int. Neuropsychol. Soc. 15, 1–8 [DOI] [PubMed] [Google Scholar]
- 30.Lippa S.M., Pastorek N.J., Benge J.F., and Thornton G.M. (2010). Postconcussive symptoms after blast and nonblast-related mild traumatic brain injuries in Afghanistan and Iraq war veterans. J. Int. Neuropsychol. Soc. 16, 856–866 [DOI] [PubMed] [Google Scholar]
- 31.McDonald S.D. and Calhoun P.S. The diagnostic accuracy of the PTSD Checklist: a critical review. Clin. Psychol. Rev. 30, 976–987 [DOI] [PubMed] [Google Scholar]
- 32.Verfaellie M., Lafleche G., Spiro A., Tun C., and Bousquet K. (2013). Chronic postconcussion symptoms and functional outcomes in OEF/OIF veterans with self-report of blast exposure. J. Int. Neuropsychol. Soc. 19, 1–10 [DOI] [PubMed] [Google Scholar]
- 33.Nemes S., Jonasson J.M., Genell A., and Steineck G. (2009). Bias in odds ratios by logistic regression modelling and sample size. BMC Med. Res. Methodol. 9, 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carroll L., Cassidy J.D., Peloso P., Borg J., von Holst H., Holm L., Paniak C., andPépin M.; WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. (2004). Prognosis for mild traumatic brain injury: results of the WHO collaborating centre task force on mild traumatic brain injury. J. Rehabil. Med. 36, 84–105 [DOI] [PubMed] [Google Scholar]
- 35.Kashluba S., Paniak C., and Casey J.E. Persistent symptoms associated with factors identified by the WHO Task Force on Mild Traumatic Brain Injury. Clin. Neuropsychol. 22, 195–208 [DOI] [PubMed] [Google Scholar]
- 36.Ponsford J., Cameron P., Fitzgerald M, Grant M, Mikocka-Walus A., and Schönberger M. (2012). Predictors of postconcussive symptoms 3 months after mild traumatic brain injury. Neuropsychology 26, 304–313 [DOI] [PubMed] [Google Scholar]