Abstract
Eagle syndrome is a rare condition resulting from elongation of the temporal styloid process or calcification of its associated stylohyoid ligaments. Although usually presenting with pain or odynophagia, Eagle syndrome has been reported to cause a multitude of neurologic symptoms or vascular complications, some of which can be life-threatening. We present a case in which an endovascularly placed internal carotid artery stent in close proximity to a calcified stylohyoid ligament resulted in stent fracture with subsequent stent and vessel occlusion. We review and discuss the presentation, diagnosis, etiology, complications and treatment options of the syndrome.
Keywords: Eagle syndrome, stylocarotid syndrome, stent fracture, carotid stent, CT
CASE REPORT
The patient is a 64-year-old male who initially presented in May 2011 with mild inability to speak, who then developed progressively worsening dysarthria and expressive aphasia over the following week. A brain MRI was performed demonstrating acute infarcts in the left middle cerebral artery territory including the left caudate head, lentiform nucleus, and left parietal and occipital lobes. As part of the stroke workup, a head and neck CT angiogram was performed which showed a severe stenosis of the cervical segment of the left internal carotid artery.
The patient subsequently underwent a catheter-based angiogram which confirmed a greater than 90% focal stenosis of the cervical segment of the left internal carotid artery. Endovascular management was felt to be an appropriate therapeutic intervention at this time due to new acute infarcts on the same side as the stenosis, likely embolic from this lesion. Carotid angioplasty was then successfully performed with placement of an Xact carotid artery stent (Abbott Laboratories, Abbott Park, IL; 6–8 mm taper, 40 mm length). The diameter of the vessel at the site of the focal stenosis improved from approximately 1 mm pre-angioplasty to greater than 4 mm following stent placement. The patient did well after the procedure with no new neurologic deficits identified and was subsequently discharged home on both Plavix (75 mg daily) and aspirin (325 mg daily).
Initially, a six-month follow-up CT angiogram was scheduled for assessment of stent patency, but the appointment was missed by the patient. Given that his neurologic status was slightly improved at six-month clinic follow-up, the decision was made to delay rescheduling of the CTA until one year post-stenting. At the one-year follow-up appointment, the patient’s neurologic examination was unchanged. However, CT angiogram showed complete occlusion of the stent as well as stent fracture. Also evident on CT was prominent thickening and calcification of the bilateral stylohyoid ligaments with the ossified left stylohyoid process and ligament in close proximity to the stent with resultant stent fracture within the left internal carotid artery. This was felt to be the most likely etiology for stent fracture. The elongated stylohyoid processes and thickened, calcified stylohyoid ligaments were present on the original CT angiogram when viewed in retrospect, but had not been identified prospectively. Stylocarotid syndrome serves as a possible etiology for the patient’s original internal carotid artery stenosis as well as the subsequent stent fracture and occlusion.
Given that the patient appears to have compensated for the loss of the left internal carotid artery without development of new symptoms, no immediate intervention was performed. The patient was referred to an otolaryngologist for discussion of definitive management of his enlarged stylohyoid processes and ossified/calcified stylohoid ligaments.
DISCUSSION
Clinical & Imaging findings
Eagle syndrome represents a collection of symptoms including neck or facial pain, referred otalgia, dizziness, globus pharyngeus, headache, and dysphagia caused by an elongation of the temporal styloid process or calcification of the stylohyoid ligament. The styloid process is a thin, pointed bone normally projecting down, forward, and slightly medially from the base of the temporal bone. The tip of the styloid process lies between the internal and external carotid arteries with the stylohyoid projecting from the tip of the process to the lesser cornu of the hyoid bone [1].
Watts Weems Eagle first described the association of an elongated styloid process with the aforementioned symptoms in 1937 and divided the syndrome into two types: the classic type and the carotid artery type (stylocarotid syndrome) [2]. The classic type is associated with symptoms caused by the activation of the cranial nerves in the near vicinity of the styloid process including nerves V, VII, IX, and X. Stylocarotid syndrome is associated with symptoms caused by abutment and compression of the carotid artery and surrounding nerve plexus by the styloid process resulting in compression and reduced blood flow through the internal carotid artery [3]. Stylocarotid syndrome has been implicated in several serious vascular complications including vessel stenosis, pseudoaneurysms, and stroke [4].
Although Eagle syndrome is rare, diagnosis can be made in an office setting via a detailed medical history and physical examination [3,5]. An elongated styloid process can be palpated in the lateral tonsillar fossa; also, local anesthetics can be injected into the tonsillar fossa providing relief of symptoms if attributable to Eagle syndrome [5]. Radiographs, both anteroposterior and lateral views, are useful for demonstrating elongation but the superimposition of various other anatomical structures often makes diagnosis challenging[6]. Three-dimensional computed tomography (3-D CT) offers better visualization of the surrounding anatomy and has thus become the preferred imaging modality [5,6]. Imaging studies including 3-D CT are also useful in identifying patients with an elongated styloid process or calcified stylohyoid ligaments who are asymptomatic.
Stent fractures are not specific to stylocarotid syndrome and can occur at locations throughout the body. Other associations with carotid stent fracture include carotid calcification, angulation of the internal carotid artery, microscopic cracks in the stent from the manufacturing process, and high physiologic loading [7]. Given this patient’s CT findings, we hypothesize that stylocarotid syndrome is responsible for the stent fracture; however, it is difficult to definitively state the etiology.
Etiology & Demographics
Eagle defined an elongated styloid process as one longer than 25 mm; however, modern healthcare providers generally designate those longer than 30 mm as elongated. A styloid process coupled with an ossified stylohyoid ligament length greater than 30 mm is considered elongated. Eagle reported a prevalence of elongated styloid process of 4%. A recent study done on 750 random patients presenting for routine dental clinic visits in Turkey showed a prevalence of 7.7%. [8]. Most individuals with an elongated styloid process or a calcified stylohyoid ligament are asymptomatic. Studies have shown that only 4–10.3% of those with an elongated styloid process show symptoms [9,10]. Although there appears to be no gender predilection for elongated styloid processes, symptoms tend to be more common in women and in those over 40 years of age [11].
The exact cause of calcification and elongation is not yet fully understood although several theories have been put forward: 1) Congenital elongation of the styloid process attributed to the abnormal persistence of a cartilaginous analog of the stylohyal (an embryologic precursor of the styloid process), 2) calcification of the stylohyoid ligament by a not yet described process, and 3) growth of osseous tissue at the insertion of the stylohyoid ligament on the lesser cornu of the hyoid bone [12,13]. Many cases of elongated styloid processes are believed to result from tonsillectomy (scars formed after tonsillectomy tighten the mucosa across the tip of the styloid [14]) or other types of trauma in the cervicopharyngeal region. It has also been suggested that local chronic irritations, endocrine disorders in female at menopause, mechanical stress, or trauma during development of styloid process could result in calcified hyperplasia of the styloid process [15]. In one study, increased serum calcium concentration and increased heel bone density were correlated to the length of the calcified stylohyoid complex [16]. Further, Guo et al. reported that elongation of the styloid process and ossification of the stylohyoid ligament were significantly correlated with the presence of ligamentous ossification or osteophytes of the cervical spine at various levels [17].
Treatment & Prognosis
Complications of elongated styloid processes or calcified stylohyoid ligaments include symptoms attributable to the classic type, namely interaction with cranial nerves V, VII, IX, and X, or problems attributable to the stylocarotid syndrome arising from interaction with blood vessels, usually the internal carotid artery and its sympathetic nerve plexus as described in this case report. Stylocarotid syndrome has not been found to correlate with tonsillectomy. Stylocarotid syndrome is generally indicated by cervical pain during compression of the internal carotid artery (ICA) and is worsened by torsion movements of the head and neck. When the internal carotid is involved, pain frequently radiates to the supraorbital and parietal areas which could lead to a misdiagnosis of cluster headaches or migraines. If the external carotid artery (ECA) is involved, pain can radiate to the infra-orbital area [9,18]. However, as most cases of elongated styloid process or calcified stylohyoid ligaments are asymptomatic, severe, unforeseen vascular complications can result.
Ohara et al. reported a case in which a patient presented with a recent history of headache followed by a sudden speech disturbance subsequently found to be caused by a stroke. The stroke was found to be secondary to right ICA dissection attributed to the ICA’s close association to an elongated (37mm) styloid process [19]. Dao et al. reported a case in which a patient presented to the emergency room with a painful, expanding neck mass found to be a pseudoaneurysm of the right ECA. CT angiography with 3D volume rendering showed ossification of bilateral stylohyoid ligaments with a sharpened edge of the right styloid process at the level of the carotid artery. This sharpened edge of the styloid process was felt to be the most likely cause of pseudoaneurysm [9]. Multiple studies have also shown that compression of the ICA against an elongated styloid process or calcified stylohyoid ligaments is known to produce a reduction of blood flow through the ICA significant enough to cause ischemia in the brain with associated neurologic symptoms [16,20]. Further, the majority of cervical carotid artery dissections result from an unknown etiology. Raser et al. found that cervical carotid artery dissection (CCAD) is associated with a longer styloid process and a recent study by Volker et al. has indicated the presence of abnormalities in the outer vessel wall in patients with cervical carotid artery dissection [21,22].
Eagle syndrome can be treated both surgically and nonsurgically. Nonsurgical treatments include steroid injections, non-steroidal anti-inflammatory drugs, and reassurance. The surgical treatment, styloidectomy, can be performed via an intraoral approach or an extraoral approach. The intraoral, or transoral, approach offers the advantage of no external scarring but is plagued by low surgical field visibility and risks the possibility of a deep space neck infection [12]. The extraoral, or transcervical, approach offers better surgical field visibility, lower risk of deep space neck infection, and the ability to remove a larger portion of the styloid process. However, this approach leaves an external scar and requires a longer recovery period than the intraoral approach [3].
TEACHING POINT
An elongated styloid process or calcified stylohyoid ligament, whether symptomatic or asymptomatic, can cause a variety of complications and it is important to identify patients at risk for these complications. CT and CT angiography are essential tools in not only providing diagnostic information but also in identifying at risk patients. The styloid processes and stylohyoid ligaments should be assessed when planning for endovascular stenting of the carotid arteries as continued compression of the artery may result in stent fracture.
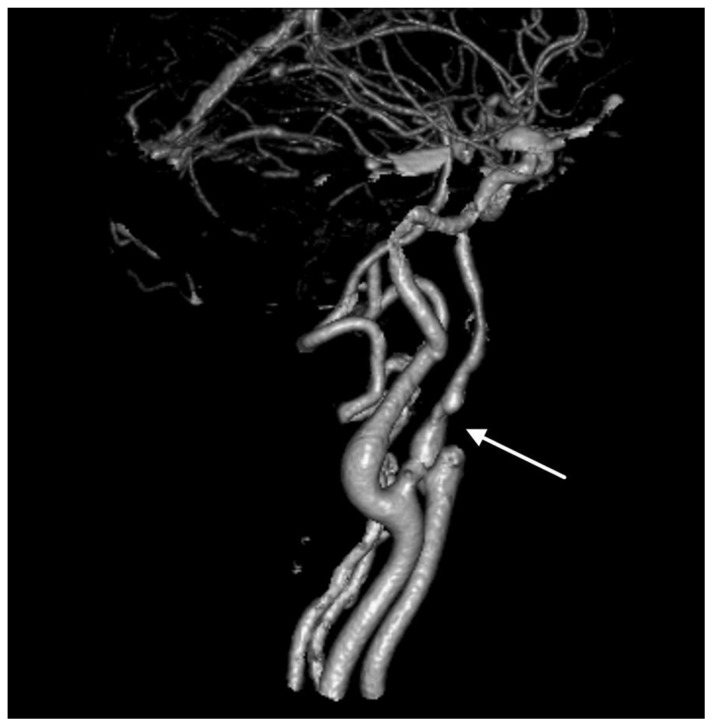
Figure 1.
64-year-old male with left internal carotid artery stenosis presumed to be due to stylocarotid syndrome.
FINDINGS: 3D reconstruction from CTA of the head and neck demonstrates a focal high-grade stenosis (arrow) in the cervical segment of the internal carotid artery with irregularity of the vessel proximal and distal to the stenosis.
TECHNIQUE: Volumetric 3D reconstruction from CTA created in Philips Brilliance, 120 kVp, 498 mAs, 512×512 matrix, FOV 21.6 cm.
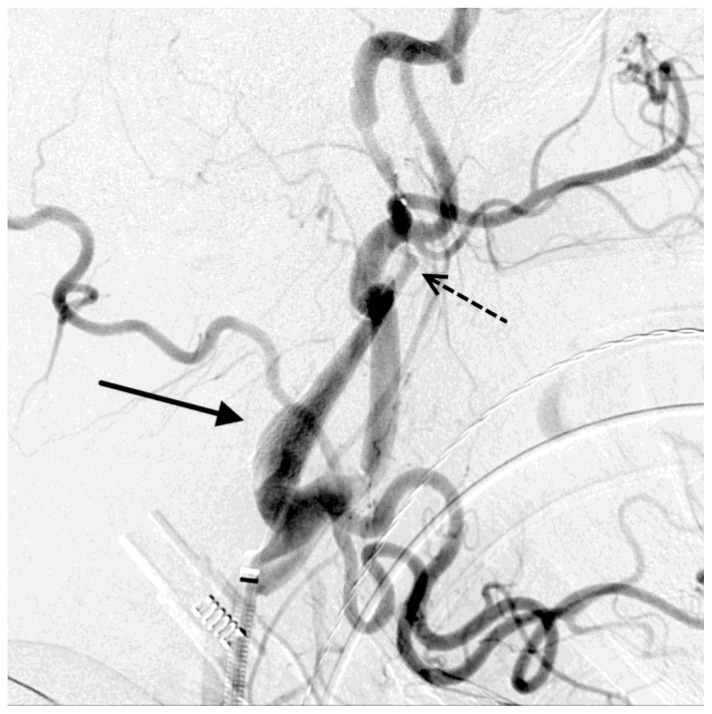
Figure 2.
64-year-old male with left internal carotid artery stenosis presumed to be due to stylocarotid syndrome.
FINDINGS: Short-segment irregularity of the left cervical internal carotid artery with focal severe stenosis (solid arrow) adjacent to the thickened, elongated left styloid process (dashed arrow). The elongated styloid process measured approximately 8 cm.
TECHNIQUE: Axial image from CTA of the neck, slice thickness 2.5mm, 120 kVp, 498 mAs, 512×512 matrix, FOV 21.6 cm.
Figure 3.
64-year-old male with left internal carotid artery stenosis presumed to be due to stylocarotid syndrome.
FINDINGS: Focal severe stenosis (arrow) in the proximal cervical segment of the left internal carotid artery.
TECHNIQUE: Digital subtraction angiography of the neck, lateral view, through a 5-Fr catheter in the left common carotid artery.
Figure 4.
64-year-old male with left internal carotid artery stenosis presumed to be due to stylocarotid syndrome.
FINDINGS: Resolution of focal internal carotid artery stenosis after stent placement (solid arrow). Incidental vasospasm distal to the stent (dashed arrow) which resolved during the procedure.
TECHNIQUE: Digital subtraction angiography of the neck, lateral projection, from a 5-Fr catheter in the left common carotid artery.
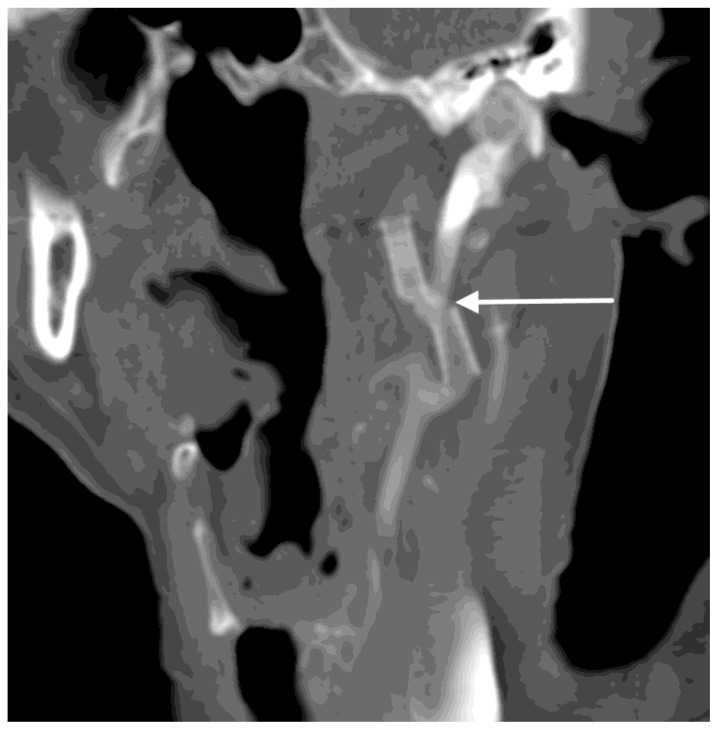
Figure 5.
64-year-old male with occluded, fractured left internal carotid artery stent presumed to be due to stylocarotid syndrome.
FINDINGS: Occlusion of the fractured left internal carotid artery stent (arrow), which abuts the elongated, ossified left styloid process. The elongated styloid process measured approximately 8 cm.
TECHNIQUE: Coronal MIP reconstruction from CT of the head and neck in the arterial phase, 120 kVp, 531 mAs, 512×512 matrix, FOV 20.6 cm with 75mL of intravenous ioversal (Optiray 320).
Figure 6.
64-year-old male with occluded, fractured left internal carotid artery stent presumed to be due to stylocarotid syndrome.
FINDINGS: Fractured left internal carotid artery stent (arrow) which abuts the elongated, ossified left styloid process. Nonopacification of the stent consistent with stent occlusion. The elongated styloid process measured approximately 8 cm.
TECHNIQUE: Coronal reconstruction from CT of the head and neck in the arterial phase, 120 kVp, 531 mAs, 512×512 matrix, FOV 20.6 cm with 75 mL intravenous ioversal (Optiray 320).
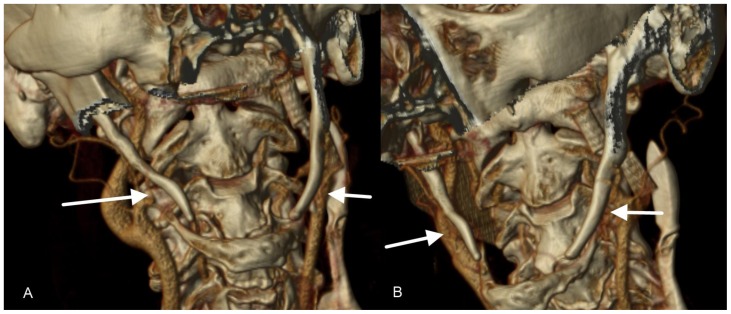
Figure 7.
64-year-old male with bilateral elongated styloid processes and fractured left internal carotid artery stent presumed to be due to stylocarotid syndrome.
FINDINGS: Bilateral elongated styloid processes (arrows). The fractured left internal carotid stent is seen next to the elongated left styloid process. The elongated styloid process measured approximately 8 cm.
TECHNIQUE: 3D reconstruction performed in Philips Brilliance from CT of the head and neck in the arterial phase, 120 kVp, 531 mAs, 512×512 matrix, FOV 20.6 cm with 75mL intravenous ioversal (Optiray 320).
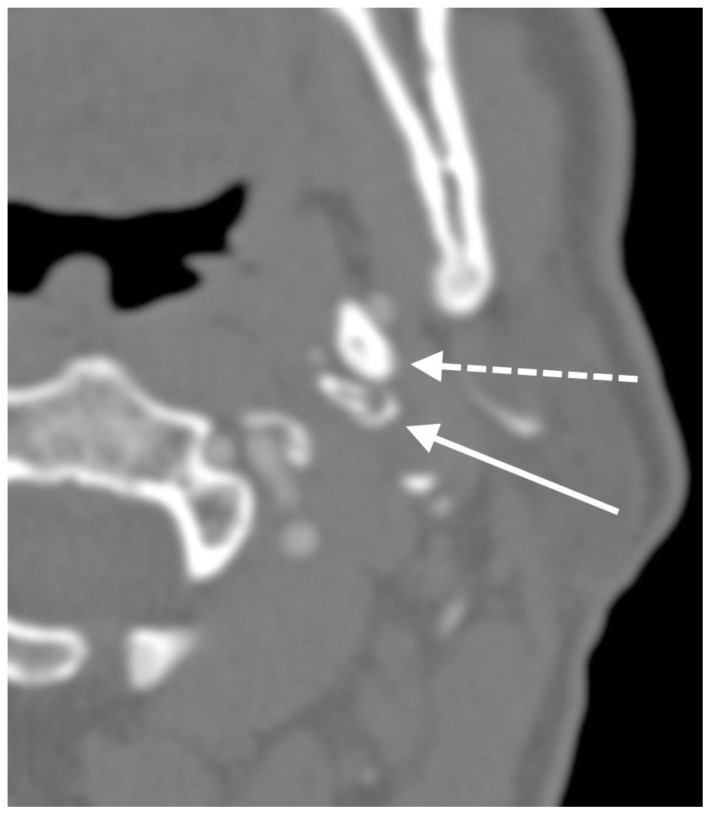
Figure 8.
64-year-old male with elongated styloid processes and fractured, occluded left internal carotid artery stent presumed to be due to stylocarotid syndrome.
FINDINGS: Fractured, severely stenotic left internal carotid artery stent (solid arrow) adjacent to the elongated left styloid process (dashed arrow). Nonopacification of the stent consistent with thrombus. The elongated styloid process measured approximately 8 cm.
TECHNIQUE: Axial image from CTA of the head and neck, slice thickness 0.75mm, 120 kVp, 531 mAs, 512×512 matrix, FOV 20.6 cm, with 75mL intravenous ioversal (Optiray 320).
Table 1.
Summary table for Eagle syndrome.
| Etiology | Uncertain. Possible causes include congenital abnormality, prior tonsillectomy, trauma, or hypercalcemia. |
| Incidence | Although an elongated styloid process can be found in approximately 4% of the population, only 4–10% are symptomatic. |
| Gender ratio | Symptoms are more commonly seen in women, although there does not appear to be a gender predilection for elongation of the styloid process. |
| Age predilection | Can be seen at any age. Symptoms are more common after age 40. |
| Risk factors | Prior tonsillectomy, trauma, hypercalcemia. |
| Treatment | Nonsurgical: local steroid injection, NSAIDS, observation Surgical: transoral or transcervical styloidectomy |
| Prognosis | Overall success rate of treatment is high (80%). |
| Imaging findings | Elongation of the styloid process and/or ossification of the stylohyoid ligament. |
Table 2.
Differential diagnosis table for Eagle syndrome.
| X-ray | CT | |
|---|---|---|
| Eagle syndrome | Elongated styloid process (>3 cm) | Elongated styloid process (>3 cm) Normal carotid vasculature |
| Stylocarotid syndrome | Elongated styloid process (>3 cm) | Elongated styloid process (>3 cm) Carotid stenosis, occlusion, dissection, or pseudoaneurysm adjacent to the styloid process |
ABBREVIATIONS
- CCAD
cervical carotid artery dissection
- ECA
external carotid artery
- ICA
internal carotid artery
REFERENCES
- 1.Mupparapu M, Robinson MD. The mineralized and elongated styloid process: a review of current diagnostic criteria and evaluation strategies. Gen Dent. 2005;53(1):54–59. [PubMed] [Google Scholar]
- 2.Eagle WW. Elongated styloid process: Report of two cases. Arch Otolaryngol. 1937;25:584–587. doi: 10.1001/archotol.1949.03760110046003. [DOI] [PubMed] [Google Scholar]
- 3.Martin TJ, Friedland DR, Merati AL. Transcervical resection of the styloid process in Eagle syndrome. Ear Nose Throat J. 2008;87(7):399–401. [PubMed] [Google Scholar]
- 4.Dao A, Karnezis S, Lane J, III, Fujitani RM, Saremi F. Eagle syndrome presenting with external carotid artery pseudoaneurysm. Emerg Radiol. 2011;18(3):263–265. doi: 10.1007/s10140-010-0930-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beder E, Ozgursoy OB, Ozgursoy SK, Anadolu Y. Three-dimensional computed tomography and surgical treatment for Eagle’s syndrome. Ear Nose Throat J. 2006;85(7):443–445. [PubMed] [Google Scholar]
- 6.Raina D, Gothi R, Rajan S. Eagle syndrome. Indian J Radiol Imaging. 2009;19(2):107–108. doi: 10.4103/0971-3026.50826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ling AJ, Mwipatayi P, Gandhi T, Seiunarine K. Stenting for carotid artery stenosis: Fractures, proposed etiology and the need for surveillance. J Vasc Surg. 2008;47(6):1220–1226. doi: 10.1016/j.jvs.2008.01.043. [DOI] [PubMed] [Google Scholar]
- 8.Gokce C, Sisman Y, Ertas ET, Akgunlu F, Ozturk A. Prevalence of Styloid Process Elongation on Panoramic Radiography in the Turkey Population from Cappadocia Region. Eur J Dent. 2008;2:18–22. [PMC free article] [PubMed] [Google Scholar]
- 9.Boscainos PJ, Papagelopoulos PJ, Goudelis G, et al. Eagle’s syndrome. Orthopedics. 2004;27(4):423–425. doi: 10.3928/0147-7447-20040401-23. [DOI] [PubMed] [Google Scholar]
- 10.Kim E, Hansen D, Frizzi J. Eagle syndrome: case report and review of the literature. Ear Nose Throat J. 2008;87(11):631–633. [PubMed] [Google Scholar]
- 11.Miller DB. Eagle’s syndrome and the Trauma patient. Significance of an elongated styloid process and/or ossified stylohyoid ligament. Funct Ortho. 1997;2264:916–925. [PubMed] [Google Scholar]
- 12.Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol. 2001;22:1401–1402. [PMC free article] [PubMed] [Google Scholar]
- 13.Balbuena L, Hayes D, Ramirez SG, Johnson R. Eagle’s syndrome (elongated styloid process) South Med J. 1997;90:331–334. doi: 10.1097/00007611-199703000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Naik SM, Naik SS. Tonsillo-Styloidectomy for Eagle’s Syndrome: A Review of 15 Cases in KVG Medical College Sullia. Oman Med J. 2011;26(2):122–126. doi: 10.5001/omj.2011.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim JE, Min JH, Park HR, Choi BR, Choi JW, Huh KH. Severe calcified stylohyoid complex in twins: a case report. Imaging Sci Dent. 2012;42(2):95–97. doi: 10.5624/isd.2012.42.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okabe S, Morimoto Y, Ansai T, et al. Clinical significance and variation of the advanced calcified stylohyoid complex detected by panoramic radiographs among 80-year-old subjects. Dentomaxillofac Radiol. 2006;35(3):191–199. doi: 10.1259/dmfr/12056500. [DOI] [PubMed] [Google Scholar]
- 17.Guo B, Jaovisidha S, Sartoris DJ, et al. Correlation between ossification of the stylohyoid ligament and osteophytes of the cervical spine. J Rheumatol. 1997;24(8):1575–1581. [PubMed] [Google Scholar]
- 18.Chuanga WC, Shorta JH, McKinneya AM, Ankera L, Knolla B, McKinneya ZJ. Reversible Left Hemispheric Ischemia Secondary to Carotid Compression in Eagle Syndrome: Surgical and CT Angiographic Correlation. AJNR Am J Neuroradiol. 2007;28:143–145. [PMC free article] [PubMed] [Google Scholar]
- 19.Ohara N, Sakaguchi M, Okazaki S, Nagano K, Kitagawa K. Internal Carotid Artery Dissection Caused by an Elongated Styloid Process: Usefulness of Transoral Ultrasonography. J Stroke Cerebrovasc Dis. 2012;21(8):918.e7–918.e8. doi: 10.1016/j.jstrokecerebrovasdis.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Farhat HI, Elhammady MS, Ziayee H, Aziz-Sultan MA, Heros RC. Eagle syndrome as a cause of transient ischemic attacks. J Neurosurg. 2009;110(1):90–93. doi: 10.3171/2008.3.17435. [DOI] [PubMed] [Google Scholar]
- 21.Raser JM, Mullen MT, Kasner SE, Cucchiara BL, Messé SR. Cervical carotid artery dissection is associated with styloid process length. JAMA Neurol. 2011;77(23):2061–2066. doi: 10.1212/WNL.0b013e31823b4729. [DOI] [PubMed] [Google Scholar]
- 22.Volker W, Besselmann M, Dittrich R, et al. Generalized arteriopathy in patients with cervical artery dissection. JAMA Neurol. 2005;64:1508–1513. doi: 10.1212/01.WNL.0000159739.24607.98. [DOI] [PubMed] [Google Scholar]