Abstract
Small bowel perforation is a rare complication of ventriculoperitoneal (VP) shunt placement. When seen, it most commonly affects the stomach or colon. We describe a case and image findings of an 8-year-old female who presented with sepsis and erosion of the VP shunt into the small bowel. The imaging findings were confirmed surgically. We also provide an overview of the current literature discussing previously reported cases, clinical features, and treatment.
Keywords: VP shunt erosion into small bowel, pseudocyst, ventriculoperitoneal shunt, VP shunt, VP complications, hydrocephalus, bowel perforation, Gram-negative bacterial meningitis
CASE REPORT
Our patient is an 8-year-old female born at 29 weeks gestational age with a history of cerebral palsy and three prior VP shunt revisions who presents with a two-day history of nonbilious emesis, fever, cephalgia, and sepsis. The most recent shunt revision was at four years old. The computed tomography (CT) scan of the head at admission demonstrated ventriculomegaly, with interval increase in size of the ventricular system since the prior examination (Figure 1). No free intraventricular air was seen on the examination. A subsequent VP shunt patency scan verified the patency of the distal shunt tubing. However, there was central organization of radiotracer in the abdomen in a pattern commonly seen with pseudocyst formation (Figure 2). Faint serpiginous radiotracer uptake was observed surrounding the central collection (Figure 2). A CT of abdomen and pelvis was then obtained demonstrating that the shunt tubing was intraluminal within multiple small bowel loops (Figure 3). The central organization of radiotracer was likely related to the shunt tubing tightly coiled within several small bowel loops (Figure 3F).
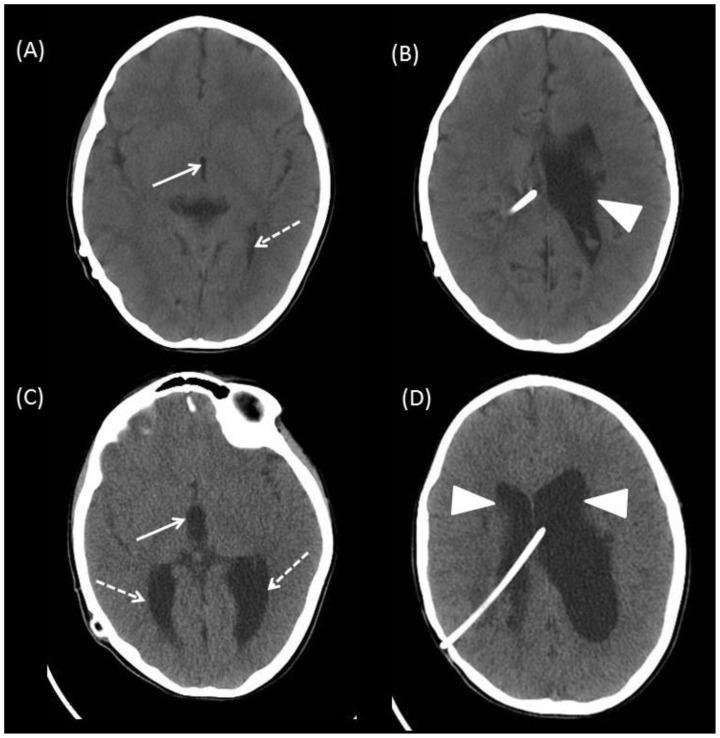
Figure 1.
8-year-old female with VP shunt erosion into the small bowel.
Findings: (A and B) Comparison CT head demonstrates a decompressed third ventricle (arrow) (measuring 2 mm in diameter) and occipital horn of the left lateral ventricle (dashed arrow). (B) The right lateral ventricle is decompressed and the left lateral ventricle is dilated (arrowhead). (C and D) CT head on admission demonstrates interval increase in the third ventricle (arrow), now measuring 9 mm in diameter. The occipital horns and bodies of the lateral ventricles are also dilated (dashed arrows and arrowheads). The right parietal approach VP shunt catheter terminates in the body of the left lateral ventricle. No air is seen within the ventricular system.
Technique: Axial CT of the head without contrast, 120kvp, 130 mA, 5 mm slice thickness.
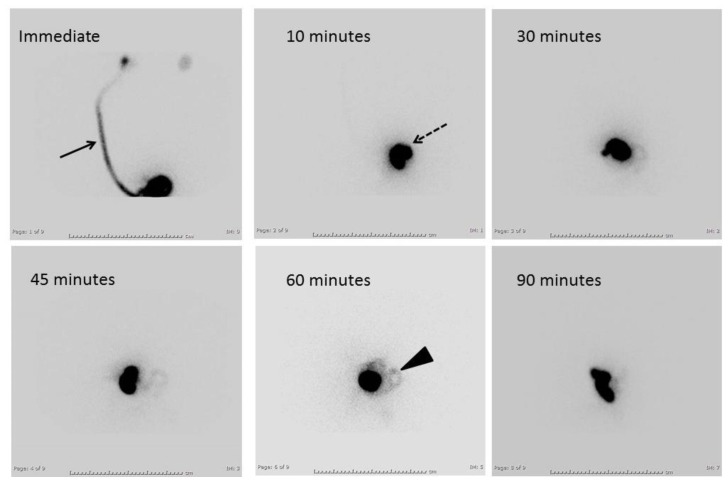
Figure 2.
8-year-old female with VP shunt erosion into the small bowel.
Findings: A Nuclear medicine VP shunt patency scan demonstrates a patent VP shunt (arrow) with central organization of radiotracer (dashed arrow). Faint serpiginous radiotracer uptake is seen adjacent to the central collection at 60 minutes (arrowhead). A CT abdomen/pelvis was recommended with concern for pseudocyst formation.
Technique: Technetium-99m DTPA 2.1 microcuries injected into shunt bubble followed by frontal images obtained immediately, 10 minutes, 30 minutes, 45 minutes, 60 minutes, and 90 minutes.
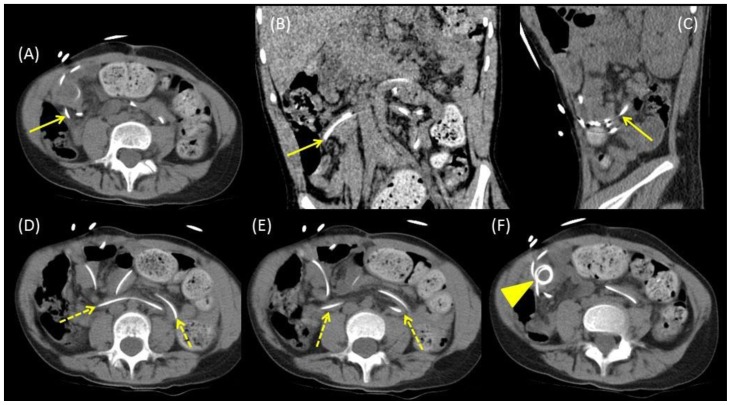
Figure 3.
8-year-old female with VP shunt erosion into the small bowel.
Findings: (A–C) CT of the abdomen and pelvis demonstrates the erosion site of the VP shunt catheter into the small bowel in axial (A), coronal (B), and sagittal (C) planes (arrows). (D and E) The VP shunt catheter is seen within several small bowel loops (dashed arrows) on axial CT images. (F) The VP shunt catheter is coiled outside of the bowel in the right lower quadrant (arrowhead), this likely corresponded to the central radiotracer organization in the abdomen seen on the VP shunt patency scan.
Technique: Axial CT of the abdomen/pelvis without contrast, 120kvp, 100 mA, 5 mm slice thickness. Coronal and sagittal thickness 1 mm.
The VP shunt fluid analysis revealed Gram-negative bacteria. The patient underwent exploratory laparoscopy confirming erosion of the VP shunt catheter into the small bowel and subsequent removal of the peritoneal portion of the shunt catheter. The patient received 14 days of antibiotics and the peritoneal portion of the shunt catheter was replaced on hospital day 14. A follow-up CT of the head prior to discharge demonstrated improved hydrocephalus.
DISCUSSION
Etiology & Demographics
VP shunt complications include pseudocyst formation, perforation of the gastrointestinal (GI) tract, penetration into solid organs/abdominal wall, protrusion outside the body, disconnection, and infection. Bowel perforation is a rare complication of VP shunt placement, with an incident rate ranging from 0.1–1% [1,2]. A review of 94 cases found that more than half of these occur from 0–10 years of age, with 34 males, 26 females, and the remaining 34 cases the gender was not reported [3]. When seen, it most commonly affects the stomach and colon. Thus, small bowel perforation by a VP shunt catheter is an exceedingly uncommon occurrence [4]. Risk factors include thin bowel wall in children, prior surgery, chronic irritation, infection, silicone allergy, and sharp/inflexible shunt catheter tip [3,5].
Clinical & Imaging Findings
Stomach and colon erosion of the VP shunt are commonly found on physical examination with either oral or rectal extrusion of the tubing. Otherwise, presentation can be variable and nonspecific. Patients may present with abdominal pain, leukocytosis, fever, diarrhea, or other symptoms of gastroenteritis. Other signs or symptoms include scalp necrosis, shunt dysfunction, meningitis, or seizures [6]. Many patients are asymptomatic and a low percentage (approximately 6%) of patients present with symptoms of meningitis, as in our patient. In the setting of meningitis and VP shunt with atypical pathogens recovered from cerebrospinal fluid (CSF), such as Gram-negative or anaerobic organisms, along with gastrointestinal symptoms, VP shunt erosion into the GI tract should be highly considered [6,7]. The most common organism isolated is Escherichia coli [6].
The most specific finding for VP shunt erosion seen on VP shunt patency scan includes radiotracer opacification of the bowel with associated peristalsis. Nonspecific findings include central organization of radiotracer in the abdomen. CT of the head or cerebral sonogram may demonstrate hydrocephalus, indicating a shunt malfunction. Air may ascend from the GI tract into the VP shunt resulting in intraventricular air [8]. As in our patient, a CT of the abdomen and pelvis will show the shunt in the bowel lumen [3].
Treatment & Prognosis
Management of VP shunt GI perforation is dependent upon multiple factors. If the patient presents with sepsis, perforation peritonitis, or intraperitoneal abscess, an exploratory laparotomy/laparoscopy should be emergently performed [2,3]. In an asymptomatic patient, the shunt tubing should be disconnected at the abdominal wall and removed through the orifice via endoscopy or colonoscopy [3,6]. If the shunt tubing cannot be reached via endoscopy or colonoscopy, an exploratory laparotomy/laparoscopy should be performed. The distal end should not be pulled back through the peritoneal cavity if at all possible, in order to prevent contamination [6]. Appropriate antibiotics should also be given.
The mortality related to VP shunt GI perforation ranges from 5.32 – 13.5 % [3,6]. A case review of 45 cases found that 80% recovered (36 patients), while 13.5% (6 patients) died from VP shunt-related causes [6]. 4.5% (2 patients) died of other unrelated causes and 2% (1 patient) the outcome was unknown.
Differential Diagnosis
This case also highlights differential considerations for the central organization of intra-abdominal radiotracer when seen on a VP shunt patency scan. The differential diagnosis for VP shunt perforation into the GI tract includes peritoneal CSF pseudocyst and peritoneal abscess. However, these imaging findings would demonstrate a fluid collection in the abdomen and fluid analysis should be obtained to confirm diagnosis. CT images of a peritoneal CSF pseudocyst will demonstrate a low-attenuating loculated fluid collection adjacent to the tip of the VP shunt. The peritoneal CSF pseudocyst is hypoechoic on ultrasound and may be septated, contain debris, or internal echoes. A peritoneal abscess will show similar findings as a peritoneal CSF pseudocyst. However, surrounding inflammatory changes can be seen on CT or hyperemia on color Doppler ultrasound images. Fluid analysis should be obtained to confirm diagnosis to differentiate between peritoneal CSF pseudocyst and peritoneal abscess. VP shunt tubing within the bowel seen on CT may mimic other GI tract tubes such as orogastric, nasogastric, Dobhoff tubes, or percutaneous feeding tubes. Careful attention should be made to follow each of the tubes to determine their individual paths.
TEACHING POINT
In a patient with a ventriculoperitoneal shunt catheter presenting with Gram-negative bacterial meningitis and gastrointestinal symptoms, VP shunt erosion into the gastrointestinal tract should be high on the differential.
Table 1.
Summary table of ventriculoperitoneal shunt erosion into the gastrointestinal tract.
| Etiology |
|
| Incidence |
|
| Gender Ratio |
|
| Age Predilection |
|
| Risk factors |
|
| Treatment |
|
| Prognosis |
|
| Imaging findings |
|
Table 2.
Differential diagnosis table for ventriculoperitoneal shunt erosion into the gastrointestinal tract.
| Diagnosis | VP shunt patency scan | CT | Ultrasound |
|---|---|---|---|
| VP shunt erosion into GI tract |
|
|
Cerebral sonogram: Hydrocephalus |
| Peritoneal CSF pseudocyst |
|
|
|
| Peritoneal abscess |
|
|
|
| Oral/Nasal or percutaneous GI tube (Nasogastric, Dobhoff, percutaneous feeding tubes) |
|
|
|
ABBREVIATIONS
- CSF
cerebrospinal fluid
- CT
computed tomography
- GI
gastrointestinal
- VP
ventriculoperitoneal
REFERENCES
- 1.Robert BS, Michael HL, Richard AR. Colonic perforation by ventriculoperitoneal shunt. Surgical Neurology. 1986;25:173–7. doi: 10.1016/0090-3019(86)90289-2. [DOI] [PubMed] [Google Scholar]
- 2.Vinchon M, Baroncini M, Laurent T, Patrick D. Bowel perforation caused by peritoneal shunt catheters: diagnosis and treatment. Neurosurgery. 2006 Feb;58(1 Supplement):ONS76–82. doi: 10.1227/01.NEU.0000192683.26584.34. discussion ONS76–82. [DOI] [PubMed] [Google Scholar]
- 3.Hai A, Rab AZ, Ghani I, Huda MF. Perforation into gut by ventriculoperitoneal shunts: A report of two cases and review of the literature. Journal of Indian Association of Pediatric Surgeons. 2011 Jan-Mar;16(1):31–33. doi: 10.4103/0971-9261.74521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Odebode TO. Jejunal perforation and peroral extrusion of a peritoneal shunt catheter. British Journal of Neurosurgery. 2007 Apr;21(2):235–6. doi: 10.1080/02688690701264346. [DOI] [PubMed] [Google Scholar]
- 5.John DB, Brodkey JS, Schaefer IK. Colonic Perforation by ventriculoperitoneal shunt tubing: A case of suspected silicone allergy. Surgical Neurology. 1998;49:21–4. doi: 10.1016/s0090-3019(97)00014-1. [DOI] [PubMed] [Google Scholar]
- 6.Sathyanarayana S, Wylen EL, Baskaya MK, Nanda A. Spontaneous bowel perforation after ventriculoperitoneal shunt surgery: case report and a review of 45 cases. Surgical Neurology. 2000 Nov;54(5):388–396. doi: 10.1016/s0090-3019(00)00334-7. [DOI] [PubMed] [Google Scholar]
- 7.Ibrahim AW. E. coli meningitis as an indicator of intestinal perforation by V-P shunt tube. Neurosurgery Rev. 1998;21(2–3):194–197. doi: 10.1007/BF02389332. [DOI] [PubMed] [Google Scholar]
- 8.Shetty PG, Fatterpekar GM, Sahani DV, Shroff MM. Pneumocephalus secondary to colonic perforation by VP shunt catheter. British Journal of Radiology. 1999;72:704–5. doi: 10.1259/bjr.72.859.10624329. [DOI] [PubMed] [Google Scholar]