Abstract
Neighborhood effects on health research has grown over the past 20 years. While the substantive findings of this literature have been published in systematic reviews, meta-analyses, and commentaries, operational details of the research have been understudied. We identified 7,140 multi-level neighborhoods and health papers published on US populations between 1995–2014, and present data on the study characteristics of the 259 papers that met our inclusion criteria. Our results reveal rapid growth in neighborhoods and health research in the mid-2000s, illustrate the dominance of observational cross-sectional study designs, and show a heavy reliance on single-level, census-based neighborhood definitions. Socioeconomic indicators were the most commonly analyzed neighborhood variables and body mass was the most commonly studied health outcome. Well-known challenges associated with neighborhood effects research were infrequently acknowledged. We discuss how these results move the agenda forward for neighborhoods and health research.
Keywords: Neighborhoods, study design, multi-level, social epidemiology, USA
Interest in “neighborhood effects on health,” or the independent effect of neighborhood context on health over and above individual factors, has been growing over the past 20 years (Oakes et al., 2015). This trend has been motivated by epidemiological studies seeking to explain patterns of disease and health across geographic areas and populations, and by the recognition that individual health is influenced by not only individual characteristics, but also by contexts to which individuals belong (Berkman and Kawachi, 2000; Macintyre, 2000). For example, researchers have conceptualized a wide range of neighborhood characteristics, including area-level poverty, walkability, food environment, air pollution, social cohesion, and crime, among others, as drivers of an equally broad range of individual health outcomes (Diez Roux and Mair, 2010). Recognizing that contextual exposures influence health, and can interact with individual-level characteristics and systems at other levels, is a crucial component of social epidemiological theories of disease distribution, particularly ecosocial theory, that have been explicated and refined in the latter part of the 20th century, and have been gaining strength in the past 20 years or so (Krieger, 2011, 1994). Growth in neighborhoods and health research reflects, in part, the influence of these contextualized perspectives on health as an alternative to dominant biomedical and lifestyle models that focus on proximate, individual-level risk factors for disease (Krieger, 2011). Examining neighborhood effects on health has also taken on new practical importance as the public health community increasingly looks to place-based interventions to promote population health and health equity (Frieden, 2010; Marmot et al., 2008).
Attempts to synthesize neighborhoods and health research conducted to date have included summaries of methodological advances in recent neighborhoods and health research (Oakes & Andrade, 2014), and a review and commentary on the contribution that “neighborhood effects” papers have made to our understanding of health since 1990 (Oakes et al., 2015). In addition, we count over 20 systematic reviews of neighborhoods and health studies that focus on various health outcomes or behaviors (Table 1). Previous reviews have found moderate to strong evidence of neighborhood effects on depression (Kim, 2008; Mair et al., 2008), mental health (Truong & Ma, 2006), early child health outcomes (Christian et al., 2015; Sellstrom & Bremberg, 2006), birth outcomes (Vos et al., 2014), intimate partner violence (Beyer et al., 2015), all-cause mortality (Meijer et al., 2012), and other general health outcomes (Pickett & Pearl, 2001; I. H. Yen et al., 2009), over and above individual-level risk factors. However, other work looking at weight-related health behaviors among African Americans (Casagrande et al., 2009) and alcohol use (Jackson et al., 2014) have reported mixed findings. Similarly, reviews on obesity (Black & Macinko, 2008; Corral et al., 2015; Feng et al., 2010) and physical activity (Bancroft et al., 2015; Ding et al., 2011; Foster & Giles-Corti, 2008; Koohsari et al., 2015; Owen et al., 2004) found largely inconsistent results across various neighborhood-level measures and health outcomes.
Table 1.
Summary of Systematic Reviews and Meta-Analyses on the Associations Between Neighborhoods and Health
| Author | Review/Meta | Exposure definition | Outcome definition | Country | Participants | # of studies | Conclusion |
|---|---|---|---|---|---|---|---|
| Ding et al, 2011 (Ding et al., 2011) | Review | Environmental attributes | Physical activity | Global | Youth (3–18 years) | 103 | - The strongest correlates for children were walkability, traffic speed/volume, access/proximity to recreation facilities, land-use mix, and residential density. - The most supported correlates for adolescents were land-use mix and residential density. - Observed associations varied by the mode of measurement (perceived, objective or combination) |
| Foster & Giles-Corti, 2008 (Foster & Giles-Corti, 2008) | Review | Real and perceived neighborhood safety | Physical activity | Global | Adults | 41 | - Results are inconsistent because much of the research relies on inadequate conceptualization and operationalization of safety. Many neighborhood characteristics may not directly affect PA. |
| Koohsari, et al 2015 (Koohsari et al., 2015) | Review | Neighborhood environmental attributes: walkability-related, urban/regional, social/crime, aesthetics, destination-related, route-related | Sedentary behaviors | Global | Adults | 17 | - There is modest, but mixed evidence: 28% of the analyses found significant associations between neighborhoods environmental attributes with adults’ sedentary behaviors, whereas 56% found nonsignificant associations. - The most consistent association was for lower levels of sedentary behavior among residents of urban compared to regional areas. |
| Bancroft et al 2015 (Bancroft et al., 2015) | Review | Parks or trails | Objectively measured physical activity | USA | No restriction | 20 | - There is inconsistency even among studies with objectively measured physical activity: 5 out of 20 articles reported a significant positive association between parks and physical activity; 9 found no association; and 6 had mixed findings. |
| Owen et al 2004 (Owen et al., 2004) | Review | Objectively assessed and perceived environmental attributes | Walking | Global | No restriction | 18 | - Aesthetic attributes, convenience of facilities for walking (sidewalks, trails); accessibility of destinations (stores, park, beach); and perceptions about traffic and busy roads were found to be associated with walking for particular purposes. |
| Feng et al, 2010 (Feng et al., 2010) | Review | Built environment: physical activity environment; land use/transportation environment; food environment | Obesity | Global | No restriction | 63 | - Of the 22 contextual papers (defined place based on contextual effects derived from shared pre-determined administrative units) that have evaluated 80 relations, 38 relations did not achieve statistical significance. - Of the 15 buffer papers (defined place based on individually unique geographic buffers) that have evaluated 40 relations, 24 relations did not achieve statistical significance. |
| Corral et al, 2015 (Corral et al., 2015) | Review | Residential segregation | Overweight/obesity | USA | African American adults | 11 | - Only 4 of the 11 studies used valid measures of both segregation and overweight/obesity and also controlled for area-poverty. Though not without methodological limitations, those 4 studies suggested that segregation contributes to overweight and obesity among African American adults. |
| Black & Macinko 2006 (Black & Macinko, 2008) | Review | Neighborhood level factors | Obesity | Global | No restriction | 37 | - In 15 studies, neighborhood-level measures of economic resources were associated with obesity. Also, neighborhood features that discourage physical activity were consistently associated with increased body mass index. - Inconsistent results for neighborhood income inequality, racial composition, and availability of healthy food. |
| de Vet et al 2011 (de Vet et al., 2011) | Umbrella review | Environmental factors | Physical activity and dietary behaviors | Global | Children and adolescents | 18 reviews (671 studies) | - Consistent evidence supporting the associations between school and neighborhood characteristics and physical activity, but not for dietary behaviors. |
| Safron et al, 2011 (Safron et al., 2011) | Umbrella review | Social and physical micro-environmental (neighborhood, school) characteristics | Diet, physical activity, and body weight | Global | Children and adolescents | 8 reviews (132 studies) | - Stronger support for several neighborhood and school characteristics (e.g., community opportunities to exercise, lower costs of physical activity facilities, physical activity built environment, low crime level) and adolescent physical activity. |
| Kramer and Hogue, 2009 (Kramer & Hogue, 2009) | Review | Black-white residential segregation | Health outcomes | USA | African Americans | 39 | - The health effects of segregation are relatively consistent: isolation segregation is associated with poor pregnancy outcomes and increased mortality, but clustered segregation (black neighborhoods) seemed to have health-protective effects. |
| Papas et al., 2007 (Papas et al., 2007) | Review | Objective measure of the build environment | Overweight/obesity | USA, Australia, Europe | No restriction | 20 | -Most (17/20) studies reported associations between the built environment and BMI, though the direction of the association was mixed. Most (18/20) studies were cross-sectional. One of the two longitudinal studies found a negative association between produce prices and weight gain; the other (sprawl and BMI) was null. |
| Pickett and Pearl, 2001 (Pickett & Pearl, 2001) | Review | Local area social characteristics | Health outcomes | Developed countries | No restriction | 25 ML studies | - Consistent evidence to support modest neighborhood effects on health. |
| Casagrande et al. 2009 (Casagrande et al., 2009) | Review | Built environment | Health behaviors | USA | African American adults | 17 | - Inconsistent relationships found between physical activity and light traffic, presence of sidewalks, and safety from crime. - Perceived barriers to physical activity were associated with obesity. |
| Yen et al 2009 (I. H. Yen et al., 2009) | Review | Objective and perceived neighborhood environment | Health outcomes | Global | Older adults | 33 | - Among different categories of neighborhood characteristics (socioeconomic composition, racial composition, demographics, perceived resources and/or problems, physical environment, and social environment), neighborhood level socioeconomic status was the strongest and most consistent predictor for elderly’s mortality and morbidity, self-reported health or quality of life, mental health, cognition, disability, and physical activity/body mass index. |
| Kim, 2008 (Kim, 2008) | Review | Neighborhood characteristics | Depression | Global | Adults | 28 | - In general, studies support for harmful effects of social disorder and, to a lesser extent, protective effects for neighborhood socioeconomic status. |
| Mair et al, 2008 (Mair et al., 2008) | Review | Neighborhood characteristics | Depression/depressive symptoms | Global | No restriction | 45 | - 37 studies reported associations of at least one neighborhood characteristic with depression/depressive symptoms. - The associations of depressive symptoms/depression with structural features (socioeconomic and racial composition, stability and built environment) were less consistent, smaller in number of studies, than with social processes (disorder, social interactions, violence). |
| Truong & Ma 2006 (Truong & Ma, 2006) | Review | Neighborhood characteristics | Mental health | Developed countries | Adults | 29 | - 27studies found statistically significant associations between mental health and at least one measure of neighborhood characteristics (sociodemographic characteristics, physical environment). Though the effect estimates attenuated after adjusting for individual-level characteristics, they still remained significant. |
| Christian et al, 2015 (Christian et al., 2015) | Review | Neighborhood built environment, green spaces, and the home outdoor area | Child health outcomes | Global | Children | 32 | - The presence of child relevant neighborhood destinations and services and parents’ perceptions of neighborhood safety were positively associated with general health and social-emotional development during early developmental periods. |
| Sellstrom & Bremberg 2006 (Sellstrom & Bremberg, 2006) | Review | Neighborhood context | Child health outcomes | High-income countries | Children and adolescent | 13 ML studies | - Neighborhood socioeconomic status and social climate were shown to have small to moderate effects on birth weight, injuries, behavioral problems, and child maltreatment. - On average, 10% of variation in health outcomes was explained by neighborhood determinants, after controlling for important individual and family variables. |
| Vos et al 2014 (Vos et al., 2014) | Review and meta-analysis | Neighborhood deprivation | Birth outcomes | Global | Birth outcomes | 24 in review; 7 in meta-analysis | - Living in a deprived neighborhood was consistently associated with increased odds for preterm delivery (OR: 1.23, 95% CI: 1.18–1.28), small-for-gestational age (OR: 1.31, 95% CI: 1.28–1.34), and stillbirth (OR: 1.33, 95% CI: 1.21–1.45). |
| Meijer et al, 2012 (Meijer et al., 2012) | Review and meta-analysis | Area-level socioeconomic status | All-cause mortality | Global | No restriction | 40 in review; 18 in meta-analysis | - No clear evidence to support the associations for area-level income inequality or social capital and all-cause mortality. - There was a significantly higher risk of mortality for individuals living in neighborhoods with low socioeconomic status. |
| Jackson et al, 2014 (Jackson et al., 2014) | Review | Neighborhood environment | Alcohol use | Global | Adolescents | 23 | - The majority of studies found no associations with residential mobility, neighborhood disorder or crime, employment or job availability, neighborhood attitudes to drinking, social capital and collective efficacy. - There were mixed results in studies examining neighborhood-level socio-economic disadvantage and alcohol use. |
| Beyer et al, 2015 (Beyer et al., 2015) | Review | Neighborhood environment | Intimate partner violence | Global | Adults | 36 | - 30 studies reported a positive association between one or more neighborhood characteristics and intimate partner violence. This was true for majority of the 17 studies that adequately adjusted for individual and neighborhood variables. |
Authors of the reviews commonly criticized the underlying studies for poor measurement of neighborhood environments, a reliance on administrative neighborhood definitions, weak study designs, and underdeveloped or absent conceptual models, all of which may contribute to inconsistent results. Such critiques align with narrative reviews published over the past decade, which reflect on the direction of neighborhoods and health research (e.g., Chaix, 2009; Diez Roux, 2007; Diez Roux and Mair, 2010). These papers have articulated conceptual models describing how multiple aspects of neighborhood environments may affect health, and have offered suggestions for future research directions that emphasize causal inference and a richer theoretical understanding of place. Calls for stronger study designs, more theoretically relevant spatial scales (e.g., Diez Roux and Mair, 2010), and better measures of a broader range of neighborhood-level exposures, mediators and confounders (e.g., Chaix, 2009) highlight the importance of methodological details for understanding the state of the science examining neighborhood effects on health.
However, there is little empirical information on the operational details of recent neighborhoods and health research. While previous reviews, included many of those cited above, provide such details for papers on specific health outcomes or neighborhood characteristics, this is the first systematic review of neighborhood and health literature published over the past 20 years that spans multiple health outcomes and neighborhood factors, and catalogues information on indicators important for assessing the neighborhood health effects literature. To this end, we describe how neighborhoods and health research has been focused and carried out between 1995–2014 by summarizing study characteristics of multi-level neighborhoods and health papers published during those years. Multi-level analyses are those that rely on data indexed at more than one level, for example, using data collected on individuals, at level 1, residing in neighborhoods, at level 2. Multi-level models provide estimates of both average relationships between exposures and outcomes, as well as of variation around these averages, at each level. By accounting for statistical dependence in data that is generated by shared contexts, and modeling realistically complex population heterogeneity, multi-level models are methodologically and substantively well-suited for studying neighborhood effects on health (Subramanian, 2004; Subramanian et al., 2003).
The multi-level analysis criterion helped us narrow a broad literature that investigates the health of individuals situated within neighborhoods to those studies whose target of inference was shared neighborhood environment (Subramanian and O’Malley, 2010). Limiting our search to multi-level analyses screened out papers that may have viewed clustering within neighborhoods as a nuisance, and those that conceptualized neighborhood environments as “activity spaces” unique to each individual. As such, studies that used a population average approach to account for shared environments, and those that used spatial buffers to construct individually-varying environmental measures, for example, were deliberately excluded from this review.
We report metrics on the neighborhood definitions used, health outcomes studied, neighborhood attributes measured, study designs employed, and multi-level sample sizes analyzed in papers that met our inclusion criteria. We also examine the extent to which researchers acknowledge common pitfalls in neighborhood effects research, including the fact that different neighborhood boundaries and sizes will produce different estimates. More specifically, we noted whether each study explicitly cited the frameworks of Modifiable Area Unit Problem (MAUP) and/or the Uncertain Geographic Problem (UGCoP), which highlight the fact that areal units are usually arbitrarily determined and, therefore, “modifiable” or “uncertain”, in the sense that they can be aggregated to form units of different sizes or spatial arrangements leading to different results (Openshaw and Openshaw, 1984).
The goals for this manuscript are twofold. First, we provide new data on the characteristics of a broad set of neighborhoods and health studies over the past 20 years as a resource to better understand the state of the “neighborhood effects on health” science. Primary objectives include characterizing the size, scope, and trajectory of growth in the literature over the past 20 years. Secondly, we reflect on previous agendas to advance neighborhoods and health research, highlighting goals that have not yet been met by the existing literature.
METHODS
Search strategy
To identify empirical multi-level studies that examine associations between neighborhood environment and health outcomes published between January 1, 1995 and December 1, 2014, we performed a literature search in four electronic databases: PubMed, Embase, PsycInfo, and Sociological Abstracts. Searches were conducted using the following title, abstract, keyword and Medical Subject Headings (MeSH) terms: multilevel, multi-level, residence characteristics, neighborhood, and built environment. No search terms were included that restricted articles based on specific outcomes (see Appendix 1 for search strategies). The reference lists of previous reviews and meta-analyses on neighborhood effects on specific health outcomes and papers deemed seminal by the investigators were reviewed. We did not perform a meta-analysis on included studies because of the diversity of the health outcomes and incomparable statistical approaches employed across the studies reviewed.
Inclusion/exclusion criteria
To be included, studies had to be 1) multi-level (i.e., at least two levels of analysis), where at least one of the higher levels was a neighborhood context, and 2) focused on exploring how neighborhoods affect health. We did not restrict how the neighborhood was defined or measured given our explicit interest in exploring this issue. We included studies with diverse outcomes related to health and health behaviors, ranging from mental health, body anthropometric measures, cancer and cardiovascular health, physical activity, and diet, for example, but excluded outcomes that measured well-being, such as quality of life and happiness. We also excluded papers focused on natural environmental exposures (e.g., particulate matter, radiation), which are generally, although not always, conceptualized as individual-level risks for which the neighborhood is not the theoretically appropriate level of measurement. We limited our search to English language articles with US study populations due to diverse methodological considerations for administrative units in other countries. Only empirical studies published in peer-reviewed journals were included in the study; abstracts, posters, book chapters, dissertations, methodological studies, reviews, and commentaries were excluded.
Study selection
Three reviewers (ASM, MS, RK) conducted the literature search, study selection, and data extraction. Once all identified bibliographic records from the four electronic databases were compiled and duplicates were removed, the list of studies was divided equally among three reviewers (ASM, MS, RK) to independently screen the titles and abstracts using the above-mentioned eligibility criteria. The same researchers then reviewed and cross-checked the included abstracts and full papers to verify inclusion criteria were met. Lastly, previous reviews and seminal papers were manually retrieved to identify additional studies. Each included article was reviewed three times to ensure it met eligibility criteria; reviewers iteratively discussed any items of confusion, and disagreement in the process was resolved through discussion with all study authors.
Data extraction
For each study, we extracted the following information: author(s), title, year, journal (volume, issue). In addition to indexing the studies, these variables allowed us to assess growth in the literature over time, and to examine if and how the field’s substantive focus has shifted since 1995. To understand how neighborhoods have been conceptualized, we inventoried neighborhood definitions and the ways in which neighborhood-level predictor variables were constructed. To gauge the substantive focus of neighborhood effects research, we also organized predictor and outcome variables into broad substantive categories. We extracted data on each study’s basic design and multi-level sample sizes, which are critical elements of study strength and allow us to comment on the ability of the research to produce individual- versus neighborhood-level estimates. As part of this effort, we also extracted information on individual level covariates, level 2 covariates, level 3 covariates, how levels 2 and 3 were measured, sample description, and noted whether neighborhood exposure variables relied on spatial information. Neighborhood predictors operationalized in terms of distance to specific exposures (e.g., mean distance to the closest park) were classified as proximity-based. Finally, we documented whether each paper included an explicit acknowledgement of the Modifiable Area Unit Problem (MAUP) or the Uncertain Geographic Problem (UGCoP). The MAUP refers to the sensitivity of spatial patterns to the choice of area level units in the analysis (Gehlke & Biehl, 1934; Openshaw & Taylor, 1979) such that the same measure takes on different values at different geographic scales. The UGCoP refers to circumstances when our knowledge is limited about which geographic scales are causally relevant for health (Kwan, 2012).
Analytic approach
All studies that met the inclusion criteria were entered into a data base, and basic descriptive statistics were generated in SAS 9.3. The reporting of this review conforms to recommendations from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (Moher et al., 2009).
RESULTS
Of 7,140 publications retrieved from initial search, a total of 259 papers met our inclusion criteria (Figure 1). The majority of these studies were published after 2003 (Figure 2); only 10% of them (26 studies) were published between 1995 and 2003, while at least this many have been published annually since 2011, with the exception for year 2012. The mid-2000s accounted for the fastest rate of growth in the literature across the 20 year time frame.
Figure 1.
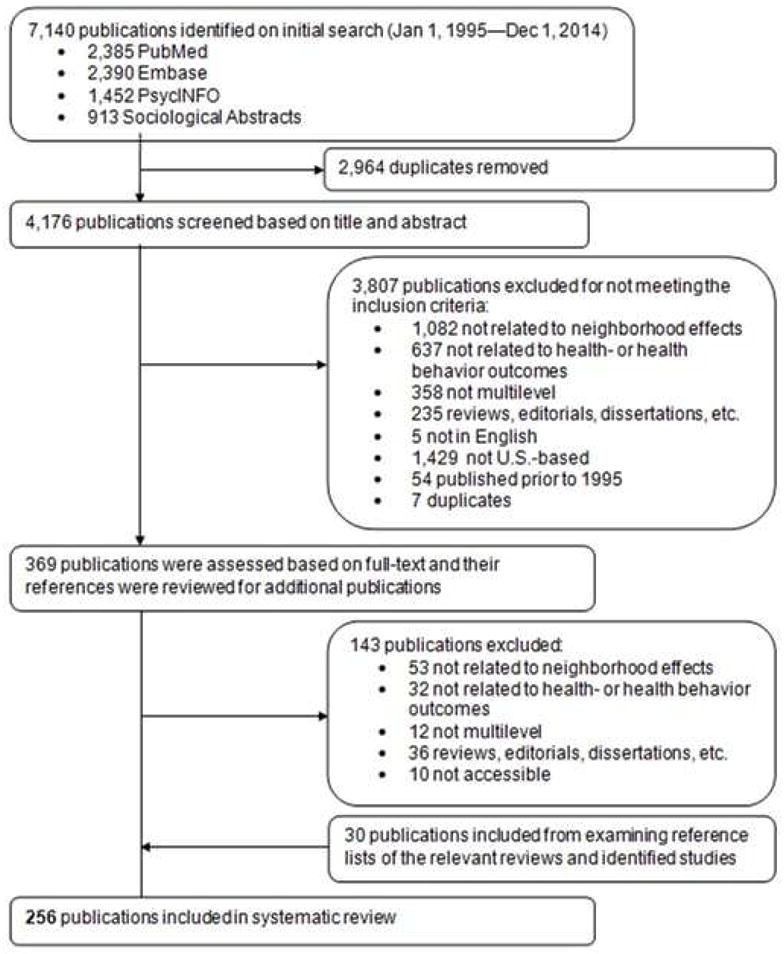
Flowchart for Study Selection
Figure 2.
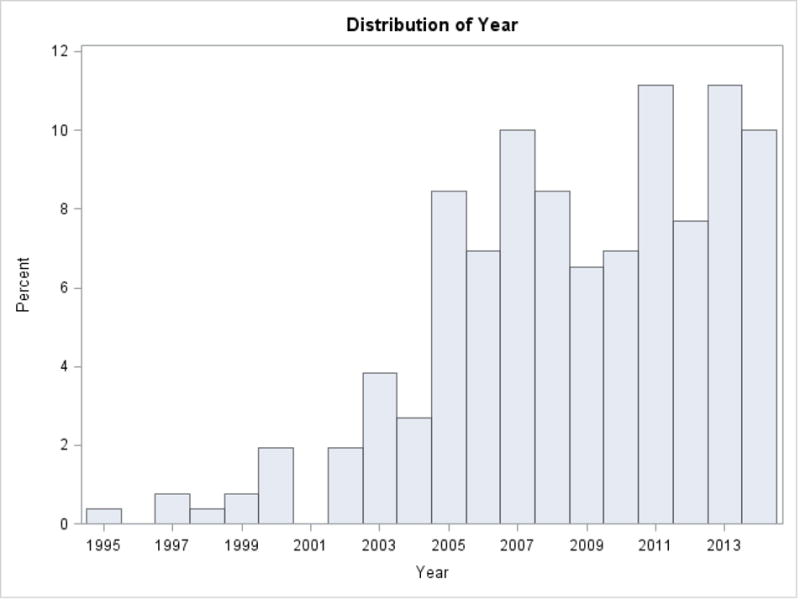
Trend of number of neighborhoods effect studies published by year (1995–2014)
Study design
Most of the included studies featured a cross-sectional design (70.7%), while just under 20% were longitudinal (Table 2). Investigations of the built environments and disability from 1986–2001 (Clarke et al., 2009), neighborhood walkability and changes in body mass index from 1990–2004 (Michael et al., 2013), and overall neighborhood social environment and risk of death from 1983–1994 (Irene H Yen & Kaplan, 1999) were among the longest-running longitudinal studies we found. Case-control (3.9%) and prospective cohort (3.9%) designs were used infrequently. Studies drawing on fully experimental data were rare (1.5%), and although these papers included data on individuals enrolled in trials, none of the trials aimed to modify the neighborhood environment. As such, neighborhood effect estimates were produced from observational analyses of trial participant data. We reviewed one study with a natural experimental design in which variation in neighborhood environment was reported to be exogenous (Arcaya et al., 2014).
Table 2.
Characteristics of 259 Empirical Quantitative Studies of Neighborhood Effects and Health
| No. of Studies | % of total studies | |
|---|---|---|
| Study design | ||
| Cross-sectional | 183 | 70.66 |
| Longitudinal | 50 | 19.31 |
| Case-control | 10 | 3.86 |
| Prospective cohort | 10 | 3.86 |
| Experimental | 4 | 1.54 |
| Others | 2 | 0.77 |
| Neighborhood level sample size | ||
| N<10 | 2 | 0.77 |
| 10≤N<25 | 12 | 4.63 |
| 25≤N<50 | 36 | 13.90 |
| 50≤N<100 | 62 | 23.94 |
| 100≤N | 117 | 45.17 |
| Not reported | 30 | 11.58 |
| Individual level sample size | ||
| 0<n<1,000 | 50 | 19.31 |
| 1,000≤n<5,000 | 92 | 35.52 |
| 5,000≤n<10,000 | 27 | 10.42 |
| 10,000≤n<20,000 | 37 | 14.29 |
| 20,000≤n | 53 | 20.46 |
| Average number of individuals per neighborhood | ||
| 0<avg<5 | 38 | 14.67 |
| 5≤avg<10 | 26 | 10.04 |
| 10≤avg<20 | 43 | 16.60 |
| 20≤avg<50 | 52 | 20.08 |
| 50≤avg<75 | 12 | 4.63 |
| 75≤avg<100 | 11 | 4.25 |
| 100≤avg | 47 | 18.15 |
| Neighborhood N not reported | 30 | 11.58 |
Sample size
About half of the papers we reviewed produced neighborhood effects estimates from data on more than 100 neighborhoods. Analyses of fewer than 50 neighborhoods represented about a fifth of the papers (19.7%). Surprisingly, neighborhood sample size was not reported in 11.6% of studies.
Individual-level samples sizes were frequently large, with more than 80% based on at least 1,000 people, and more than one fifth of papers based on more than 20,000 people. When we examined individual sample sizes by neighborhood, we found that a quarter of studies relied on data on fewer than 10 individuals per neighborhood. Roughly a fifth of papers had data on 100 or more individuals per neighborhood. Plotting individual versus neighborhood sample sizes (Figure 3) illustrates the fact that most studies’ samples averaged fewer than 50 individuals per neighborhood.
Figure 3.
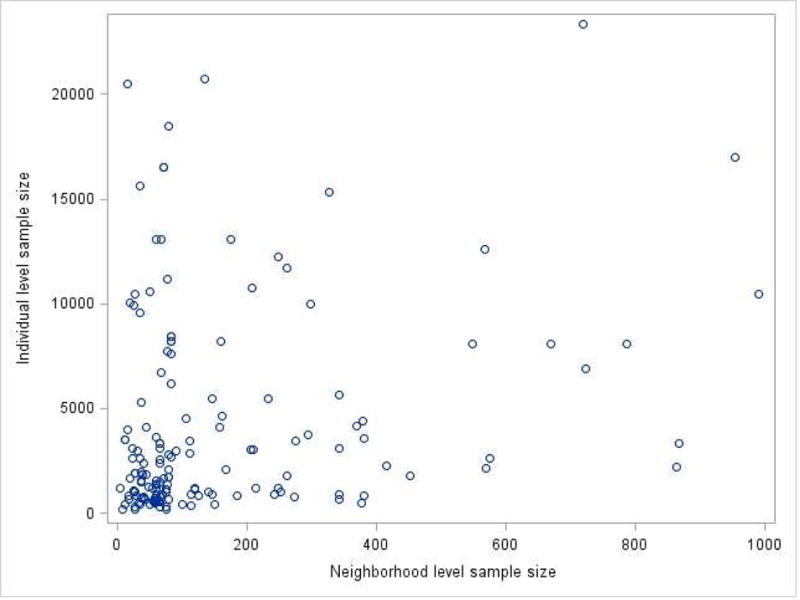
Correlation between neighborhood-level sample size and individual-level sample size
Measures
Neighborhood-level variables that dominated the literature spanned several categories (Table 3). Census-based aggregate variables, a category that comprises all descriptors derived from census data, including, for example, poverty rate, racial/ethnic composition, an d percent of the population lacking a college education, were the most common neighborhood-level predictors (43.2%). A smaller share of studies examined neighborhood variables as survey-based aggregate variables (12.0%) and even fewer used non-aggregated, contextual variables (5.4%). Survey-based aggregate variables are those derived from data collected at individual-level but expressed as a summary measure at the neighborhood-level. For instance, measures of neighborhood cohesion frequently come from individual responses to the Sense of Community Scale, and neighborhood stress scores can be derived from resident responses to the City Stress Index (Andrews et al., 2014). Finally, non-aggregated, contextual variables refer to predictors capturing truly contextual features of the neighborhood environment that are not based on census data or individual respondents. For instance, studies using measures such as density of convenience stores, proximity to food establishments, distance to public transit and other observable neighborhood conditions were classified in this category. It was not uncommon for studies (38.2%) to use a combination of these different types of neighborhood predictors.
Table 3.
Neighborhood Level Characteristics in 259 Empirical Quantitative Studies of Neighborhood Effects and Health
| No. of Studies | % of total studies | |
|---|---|---|
| Multiple level of geographies | ||
| 1 level | 243 | 89.58 |
| 2 or more levels | 15 | 9.65 |
| Neighborhood definition | ||
| Census tracts | 135 | 52.12 |
| Block groups | 57 | 22.01 |
| Neighborhood clustersa | 21 | 8.11 |
| ZIP codes | 15 | 5.79 |
| Othersb | 20 | 7.72 |
| More than one definitionc | 8 | 3.09 |
| No description | 3 | 1.16 |
| Is neighborhood geographic vs spatial | ||
| Geographic | 208 | 80.31 |
| Spatial | 14 | 5.41 |
| Both | 37 | 14.29 |
| Is neighborhood variable proximity vs prevalence | ||
| Prevalence | 234 | 90.35 |
| Proximity | 5 | 1.93 |
| Both | 20 | 7.72 |
| Neighborhood level variables | ||
| Census-based aggregated | 112 | 43.24 |
| Survey-based aggregated | 31 | 11.97 |
| Non-aggregatedd | 14 | 5.41 |
| Combinatione | 99 | 38.22 |
| Not reported | 3 | 1.16 |
| Explicit mention of MAUP/UGP | ||
| None | 249 | 96.14 |
| UGP | 2 | 0.77 |
| MAUP | 8 | 3.09 |
Abbreviations: MAUP= modifiable areal unit problem as originally described in Gehlke & Biehl (1934) ; UGP=uncertain geographic context problem as originally described in Kwan (2012); only explicit reference to these terms was acknowledged.
All 21 studies using neighborhood clusters (NCs) as neighborhood definition were analyzing data from Project on Human Development in Chicago Neighborhoods (PHDCN). 847 census tracts in the city of Chicago were collapsed to form 343 NCs that were “ecologically meaningful” (http://www.icpsr.umich.edu/icpsrweb/PHDCN/sampling.jsp).
Other definitions of neighborhoods included primary care service areas, “buffers” or “radius circle”, geopolitical units, and minor civil division.
Studies that used more than one definition of neighborhood tested their main effects models using multiple definitions. 6 studies used census tracts and block groups; 2 studies used census tracts and ZIP codes.
Non-aggregated neighborhood variable refers to truly contextual features of the environment, including number of convenience stores, availability of recreational centers, and air quality.
Combination refers to any mix of census-/survey-based aggregated variables and non-aggregated variables used in the studies as neighborhood level predictors and/or covariates.
In a substantial majority of cases (90.4%), the neighborhood exposure variables were a-spatial (e.g., percent poverty). Less than 2% of studies used proximity to neighborhood exposures (e.g., average distance to the nearest grocery store) as the sole predictor variable. Nearly 8% used a combination of spatial and a-spatial neighborhood exposures.
Neighborhood definitions
Approximately half (52.1%) of studies used census tracts to define neighborhood boundaries. An additional 22% also used census definitions at a smaller scale, employing block groups instead. The influence of the Project on Human Development in Chicago Neighborhoods (PHDCN) on the field is apparent in our analysis, with 8.1% of papers defining neighborhoods according to that study’s neighborhood clusters. Zip codes (5.8%) or the use of multiple definitions (3.1%) were less common, and very few papers did not have a clear neighborhood definition (1.2%). Analytically, authors overwhelmingly used neighborhoods as the second and final level in their multi-level models (89.6% of papers). Only one-tenth of studies analyzed neighborhood effects using three level models, and just two papers (0.8% of our sample) conducted analyses beyond three levels. For three-level analyses, counties were most often chosen as the third level (Major et al., 2012; Major et al., 2014; Markossian et al., 2014; Robert & Ruel, 2006; Xiao et al., 2007; Xiao et al., 2011), while census tracts (Subramanian et al., 2005) and states (Subramanian et al., 2008) were less commonly used. One study investigating the relationship among neighborhood stressors, stress-buffering mechanisms, and likelihood of alcohol, drug, and mental health disorder analyzed four-levels (level-1 individuals, level-2 households, level-3 census tracts, and level-4 county) (Stockdale et al., 2007). Another example of a four-level study nested children (level-1) in block groups (level-2) in zip codes (level-3) in counties (level-4) (Zhang et al., 2013).
Substantive focal areas
The most commonly studied neighborhood characteristics (Table 5) included socioeconomic status (28.2%), the built environment (9.3%), and poverty (6.95%). We distinguished neighborhood socioeconomic status from poverty because the former encompasses a broader construct pertaining to resource allocation, social exclusion, and power relations (Zhang et al., 2013). For instance, studies analyzing neighborhood-wide owner-occupied housing units, unemployment rates, proportion of female-headed households, average educational attainment, and occupational professions were all classified as exploring neighborhood socioeconomic status. Built environment included exposures such as neighborhood walkability, land use mix, aesthetic quality, physical incivilities, street connectivity, and public transportation. Of note, 23.6% of studies reviewed did not describe any primary predictor, instead conceptualizing neighborhoods themselves as sources of variance in health. Finally, 9.7% of studies reviewed included unique primary predictors that were uncommon in most other studies, such as service density, concentration of widowed individuals, neighborhood stability, and linguistic isolation.
Table 5.
Primary Neighborhood Predictors in Studies of Neighborhood Effects and Health (N=259)
| Neighborhood Exposure/Predictor | No. of studies | % of total Studies |
|---|---|---|
| No primary predictor a | 61 | 23.55 |
| Socioeconomic Status (SES) b | 73 | 28.18 |
| Built environment | 24 | 9.27 |
| Poverty | 18 | 6.95 |
| Food environment | 17 | 6.56 |
| Racial composition | 16 | 6.18 |
| Social environment | 15 | 5.79 |
| Violence/crime | 6 | 6.18 |
| Health care access | 4 | 1.54 |
| Others | 25 | 9.65 |
Studies testing for multiple neighborhood predictors or assessing variations by neighborhoods were classified as not having a primary neighborhood predictor.
SES includes area level income and deprivation index as well.
In terms of health outcomes, obesity/BMI (Table 4) were most frequently assessed, representing roughly a fifth of the extant literature (19.7%). Other commonly explored health outcomes included mental health-related outcomes (13.5%), pregnancy and birth outcomes (7.7%), cancer-related behaviors including screening, diagnosis, and survival (7.7%), and self-rated health (7.3%). Outcomes of interest have changed over time (Figure 4), with obesity/BMI overtaking mental health in 2010 as the most popular health dimension examined.
Table 4.
Ranking of Common Health Outcomes Explored in Studies of Neighborhood Effects and Health (N=259)
| Health outcome | No. of Studies | % of total studies |
|---|---|---|
| BMI/obesity | 51 | 19.69 |
| Mental health | 35 | 13.51 |
| Pregnancy and birth outcomes | 20 | 7.72 |
| Cancer screening, diagnosis, and survival | 20 | 7.72 |
| Self-rated health | 19 | 7.34 |
| Physical activity | 18 | 6.95 |
| Alcohol and substance use | 16 | 6.18 |
| Mortality | 15 | 5.79 |
| Sexual health/STIs | 14 | 5.41 |
| Respiratory disease and asthma | 7 | 2.70 |
| Coronary heart disease | 6 | 2.32 |
| Smoking | 5 | 1.93 |
| Fruit and vegetable intake | 5 | 1.93 |
| Stress | 4 | 1.54 |
| Hospitalization | 3 | 1.16 |
| Tuberculosis | 2 | 0.77 |
| Diabetes | 2 | 0.77 |
| Medication adherence | 2 | 0.77 |
| Stroke | 1 | 0.39 |
| Violence | 1 | 0.39 |
| Others | 13 | 5.02 |
Figure 4.
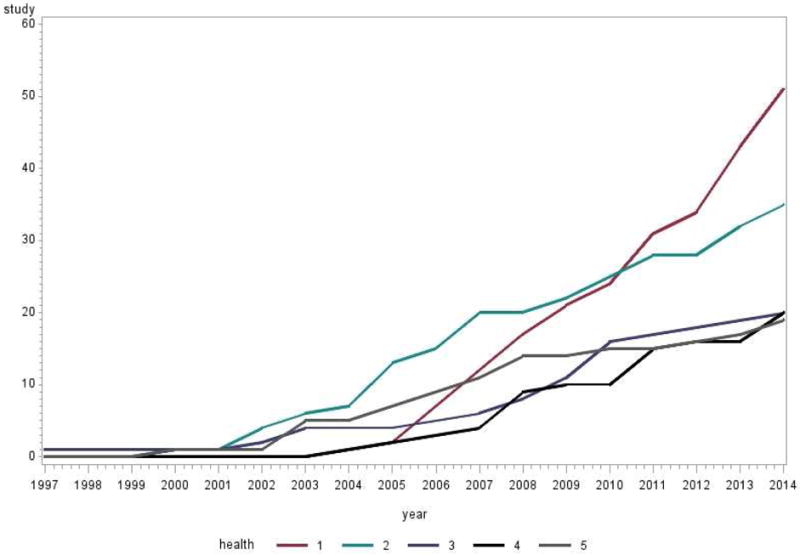
Cumulative trend of neighborhood effects publications for the top five most common health outcomes over time (1997–2014)
Acknowledgement of limitations of multilevel neighborhood effects research
We noted how frequently authors explicitly acknowledged challenges associated with the Modifiable Areal Unit Problem (MAUP) or the Uncertain Geographic Context Problem (UGCoP). While it was not uncommon for authors to note limitations of their chosen neighborhood boundaries and sizes, very few studies have included an explicit mention of either of these problems (96.1% omitted discussion of these problems). When either was mentioned, the MAUP was addressed more frequently than the UGCoP (3.1% and 0.8%, respectively).
DISCUSSION
This review provides an account of how multi-level neighborhoods and health research, the subset of the broader place and health literature that is most focused on exploring how shared neighborhood environments matter for health (Subramanian and O’Malley, 2010) has grown and been operationalized in the past 20 years. Our results reveal a rapid expansion of the multi-level neighborhoods and health literature between 1995–2014, illustrate the dominance of observational cross-sectional study designs, and show a heavy reliance on single-level, census-based neighborhood definitions. Substantively, we found that socioeconomic indicators were the most commonly analyzed neighborhood variables. The most frequently explored health outcome was body mass as measured by BMI, and/or obesity, which overtook mental health as the most commonly studied outcome around 2010. We note that complex factors well-known to influence the design and interpretation of neighborhood effects research, including the MAUP and UGCoP, are rarely explicitly discussed in the literature.
One goal of this review was to provide new data on neighborhoods and health studies over the past 20 years as a resource to better understand the state of the “neighborhood effects on health” science. To this end, we hope that our results will provide useful points of reference in a range of settings. For example, these findings could help funders understand how outcomes studied by neighborhood and health researchers relate to overall burdens of morbidity and mortality, and could allow a comparison between the neighborhood-level interests of health researchers and those of other disciplines.
The second goal was to highlight the areas that warrant more attention in the research literature and to reflect on priorities for future neighborhoods and health research. We discuss our findings vis-a-vis previously articulated research agendas below, and highlight promising approaches to advance the field.
Causal Inference
Over 70% of the papers we reviewed were observational and cross-sectional in their design. Previous published work has noted the challenges associated with using observational cross-sectional data to understanding neighborhood effects on health, including confounding by unobserved covariates, structural confounding and the related threat of generating off-support estimates, and reverse causation (Diez Roux, 2007; Oakes, 2006, 2004). As such, the seemingly large literature on neighborhoods and health may actually provide a much smaller body of work from which to draw causal inferences. This has not precluded researchers from producing valuable insights into how neighborhoods affect health; a small number of well-designed studies can, and in some cases does, provide convincing causal evidence on neighborhood effects on health. Clear articulation of the conditions that must be met in order to identify neighborhood effects (Vanderweele, 2008) is helpful in assessing when data can support a causal interpretation of multilevel effect estimates. However, leaders in the field have long noted that investigating relationships between neighborhoods and health requires a range of study types (e.g.,(Diez-Roux, 2001)), including longitudinal designs that follow people as they transition between neighborhoods and as neighborhoods evolve around them, and intervention studies designed to inform place-based efforts to improve health. Although calls for increased diversity in how we approach neighborhoods effects on health research have been made for over 15 years, our findings suggest that there is still a paucity of longitudinal and quasi, natural, or fully experimental research in this area. We note efforts to prospectively measure changes in health associated with relocations spurred by exogenous events. For example, researchers tracked changes in depressive symptoms among African American public housing residents relocated from distressed public housing to voucher-subsidized, private market rental units that were in less economically disadvantaged areas, on average (Cooper et al., 2014). Analyzing four waves of data on depressive symptoms and Census tract-level economic conditions spanning pre- to post-relocation, the authors found that improvements in neighborhood economic conditions predicted reductions in depressive symptoms and that perceptions of community violence mediated the relationship. In contrast, an earlier study found that census tract affluence, not disadvantage, predicted depressive disorders among African Americans (Alegría et al., 2014). While there are many explanations for why these results may have differed, including drawing on different African American populations, slightly different time periods, different geographic extents and different measures, crucial differences in study design may contribute to the discrepancy.
Of the well-known challenges associated with making inferences using cross-sectional observational data, confounding is perhaps the most commonly acknowledged but we note that efforts to better understand ‘reverse causation’ have been on the rise. While health selection into neighborhoods has been highlighted in previous reviews and commentaries (e.g., (Chaix, 2009; Diez Roux and Mair, 2010), empirical evidence on this process has been scant until relatively recently. This is, in part, because observational cross-sectional studies cannot answer whether neighborhoods influence health, health drives neighborhood attainment, or health and neighborhood outcomes are both governed by prior common causes. However, with longitudinal data, frameworks that conceptualize health as an outcome and place as an exposure can be reversed to ask if health sorts individuals into neighborhoods. Earlier studies that adjusted for stated neighborhood preferences (Frank et al., 2007) to assess health-related selection effects are now joined by new empirical evidence supporting (M. C. Arcaya et al., 2014; Dunn et al., 2014) (Arcaya et al., 2015) and disputing (James et al., 2015) the idea that health is a meaningful neighborhood selection factor. Clarifying the casual role of health status in determining residential outcomes is important for both generating unbiased neighborhood effects on health estimates and for understanding the substantively important process that determine residential mobility.
Testing complex and dynamic relationships
Beyond improved testing of directed hypotheses about how places affect health or health sorts people into places, our findings support calls for more holistic efforts to understand the complexity of reciprocal neighborhood-health interactions (e.g., Auchincloss and Roux, 2008). Our inventory of commonly studied health outcomes revealed that BMI/obesity and mental health served as outcomes in nearly one third of the literature we reviewed. Because both BMI and mental health function as trajectories over time (Araújo et al., 2015; Merikangas et al., 2003), the timing of relevant neighborhood exposures may be distal in some cases, and/or may accumulate over various life stages. Further complicating matters, many of the dominant neighborhood exposures identified in this review, including socioeconomic status, poverty, and racial composition, are correlated across the life course and even between generations (Sharkey, 2008, 2013). This type of dependency makes it difficult to interpret whether associations detected between contemporaneously measured neighborhood and health variables in fact reflect correlations between early life environment and current outcomes, or even between early environment and early life outcomes, which themselves function as starting points for correlated or mutually-reinforcing trajectories throughout the life course. Because the most frequently studied exposures and outcomes in the field have important life course components, it is essential that researchers exploring the effects of neighborhood on health base their analytic plans around knowledge of disease etiology, a priori hypotheses about the most important timing of neighborhood exposures for each outcome, and the ways in which individuals interact with neighborhoods over time. The complex systems paradigm has been proposed to address these methodological challenges (Galea et al., 2010). In the complex systems paradigm (Diez Roux, 2011), the system (e.g. neighborhoods) contains individual elements (e.g. people) that interact locally with feedback across elements and multiple levels to create global patterns. Methods in this paradigm that have been proposed to complement our current analytic strategies include agent-based modeling (Auchincloss and Roux, 2008), which entails running computer simulations of how micro-level entities behave and interact with each other and with the environment over time in order to understand macro-level systems. Such models have been used by urban planning researchers to understand how people move through the city (Schelhorn et al., 1999); to explore the role of segregation in shaping the dietary patterns of neighborhood residents (Auchincloss et al., 2011); and to better understand the interaction between physical activity behavior and the neighborhood context (Gao, 2013).
Identifying interventions that work
A crucial challenge associated with using observational study designs to assess the dominant focal areas tackled by the literature can be summarized by the central question: so what’s the intervention? With respect to neighborhood socioeconomic status and deprivation, for example, different ways of increasing neighborhood income are likely to have distinct health impacts. Knowing that neighborhood poverty threatens health could spur recommendations to increase local incomes through minimum wage increases, to gentrify poor neighborhoods by moving wealthy residents in, or to help poor people relocate from poor to affluent neighborhoods. The effects of each intervention in these cases could benefit, or even harm, health to different degrees, even if they all decreased neighborhood poverty by the same amount, but observational studies on such neighborhood attributes rarely provide insight into the ramifications of different intervention approaches. We echo other calls from within the public health community to increase the number of experimental studies (Oakes et al., 2015) so that we can begin to tackle the central question of what interventions have the potential to actually improve health outcomes and health equity. Community-based collaborations designed to understand neighborhood change, intervention studies, and evaluations of natural experiments do not always conform to traditional funding models, institutional review board processes or research timelines (Brown et al., 2010; Nyden, 2003), introducing increased time costs and risks for researchers. Initiatives that explicitly support cross-sector partnerships between academic and community leaders (e.g., (Robert Wood Johnson Foundation, 2016) may help to incentivize work that can directly inform neighborhood-level interventions that improve health.
Defining neighborhoods
Nearly 75% of the studies we reviewed relied on U.S. Census Bureau tracts or block groups to define neighborhoods. While we have some evidence that these geographies perform well with respect to certain types of public health research (Krieger et al., 2003), the field’s overwhelming preference for census boundaries raises questions about whether these definitions are driven by strong a priori hypotheses about how contexts affect health, or whether neighborhood boundaries are selected for convenience. It seems unlikely that for three quarters of the interesting questions in the field, relevant process occurs at the scale of census tracts or block groups. Compounding the problem, about 90% of papers we reviewed used only two levels of analysis, with individuals at level 1 and neighborhoods at level 2. This means that in the vast majority of papers, spatial relationships among neighborhood units were not considered, nor were neighborhoods situated within larger geographies. To the first point, ignoring distance among neighborhood units can be quite problematic from a technical perspective, for example when spatial clustering of level-2 residuals occurs (M. Arcaya et al., 2012). Omitting information about spatial relationships may also cost researchers in terms of their substantive findings. For example, evidence suggests that poor neighborhood surrounded by other poor neighborhoods affect people differently than do poor neighborhoods surrounded by less disadvantaged areas (Graif, 2015). In addition to modeling relationships among level 2 neighborhood units, researchers should consider whether higher-level geographies should also be incorporated into their models. Supra-neighborhood characteristics may be crucial to health, including the municipal policy environment, which shapes neighborhoods (Thornton et al., 2013) through services, policies, and programs (Vlahov et al., 2007). The share of the local budget allocated to public health has been recognized as both an indicator of fiscal resources for, and of attitudes towards, health (Hillemeier et al., 2003). This and other readily accessible municipal-level variables could help explain not only individual variation in health outcomes, but also variance that typically partitions to the neighborhood level. In short, the importance of extended environments, whether modeled by including spatial relationships among neighborhood units, or situating neighborhoods in higher-level geographies, is lost under the typical approach to modeling local contexts that is seen in the literature. Future studies should carefully consider mechanisms, theory, and disease etiology to craft neighborhood definitions, establish relevant scales, and consider the interaction of neighborhoods with their larger geographic contexts. Because these decisions should be specifically tailored for each study, there is no “right” way of defining geographic contexts that we would expect to account for 75% of analyses. A systematic review that explores evidence on neighborhoods and health at both higher and lower levels would be informative on this point. Although studies that construct individually-varying activity spaces to measure neighborhood exposures are on the rise and may avoid some challenges associated with choosing neighborhood boundaries, investigating how membership in neighborhoods impacts health requires grappling with these issues. A wider range of neighborhood definitions would be a welcome addition to the neighborhoods and health literature moving forward. On a distinct but related point, despite frequently testing the sensitivity of their results to changes in scale and boundaries, authors rarely explicitly acknowledge the MUAP or UGCoP. While there are other ways of discussing limitations in neighborhood definitions, we used this as a crude indicator of whether the field was explicitly addressing this issue. Considerations stemming from issues of boundaries and scale should be surfaced to aid readers in interpreting results, even if data limitations prevent testing alternative neighborhood models.
Limitations
Our analysis is necessarily limited by our choice of search terms and review protocol. For example, we could have retrieved a somewhat different sample of papers with modified, yet reasonable, search terms. Likewise, it is possible that nuances in manuscript text that implied -but did not explicitly state - that research considered the MAUP/UGCoP could arguable be misrepresented by our classifications. However, any other specific choice of protocol is vulnerable to similar challenges. Given our goal of providing a broad overview and synthesis of research conducted to date, small changes in review procedures would likely produce similar findings. A second limitation is that our search was restricted to US studies.
Taken together, our findings prompt a series of questions that should be asked as part of planning future neighborhood effects on health studies, and to advance of this line if inquiry in the population health field: what is the added value of another observational cross-sectional study? Is there a way to answer the focal research question that allows for the consideration both “reverse causation” and confounding? Does the analysis require a life course perspective in order to test for the theoretically most important neighborhood effects on health? Can we explore the relationships of interest with quasi-experimental data in order to inform community-level interventions? Do we have a strong a priori hypothesis about the relevant spatial scales or hierarchical memberships that matter for the health outcome at hand? How can we construct a model of the environment that best represents our understanding of how contexts affect health? Considering these questions, where relevant, has the potential to diversify and advance the type of knowledge generated by neighborhoods and health researchers and move us closer to identifying policy levers for interventions.
Supplementary Material
Figure 5.
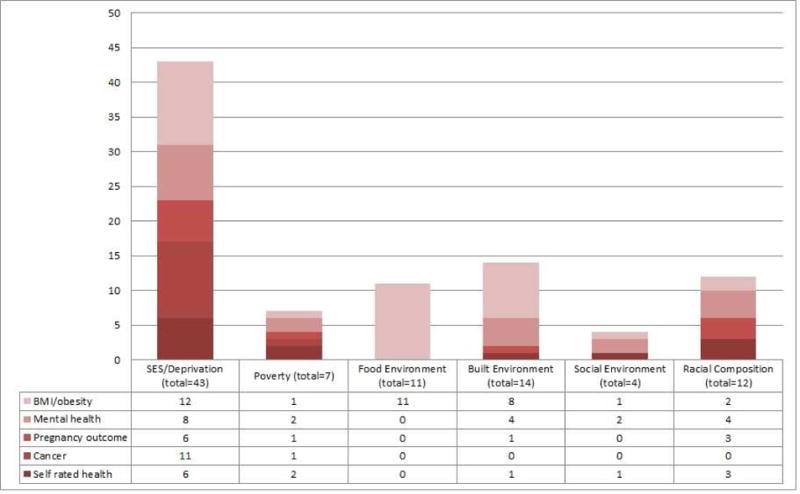
Neighborhood predictors and health outcomes commonly studied together
Highlights.
Multi-level neighborhoods and health literature has grown over the past 20 years
Observational cross-sections, census-based boundaries, and two-level designs were dominant
BMI/obesity and neighborhood SES were the most common outcomes and exposures, respectively.
Making causal inferences and modeling complex and dynamic relationships are future priorities.
Future research should inform interventions that improve health and reduce disparities.
Acknowledgments
SVS, RTS and MA conceptualized the study. RK, ASM, and MS conducted the review and entered the data. RK created the graphics and tables. MA wrote the first draft of the manuscript. RK, RTS, and SVS provided critical edits, and contributed to the writing. RTS and SVS provided overall supervision to the study. The authors would like to thank Galina Gheihman for her research assistance in conducting the review. RTS is funded by an NCI Career Development Grant (K01 CA16904101). SVS was supported, in part, by a Robert Wood Johnson Foundation Investigator Award in Health Policy Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mariana Arcaya, Massachusetts Institute of Technology.
Reginald Tucker-Seeley, Harvard Chan School of Public Health.
Rockli Kim, Harvard Chan School of Public Health.
Alina Schnake-Mahl, Harvard Chan School of Public Health.
Marvin So, Harvard Chan School of Public Health.
SV Subramanian, Harvard Chan School of Public Health.
References
- Andrews JO, Mueller M, Newman SD, Magwood G, Ahluwalia JS, White K, et al. The association of individual and neighborhood social cohesion, stressors, and crime on smoking status among African-American women in southeastern US subsidized housing neighborhoods. Journal of Urban Health. 2014;91:1158–1174. doi: 10.1007/s11524-014-9911-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araújo J, Severo M, Barros H, Mishra G, Guimarães J, Ramos E. Developmental trajectories of adiposity from birth until early adulthood and association with cardiometabolic risk factors. International Journal of Obesity. 2015;39:1443–1449. doi: 10.1038/ijo.2015.128. [DOI] [PubMed] [Google Scholar]
- Arcaya MC, Graif C, Waters MC, Subramanian SV. Health Selection into Neighborhoods Among Families in the Moving to Opportunity Program. Am J Epidemiol. 2015 doi: 10.1093/aje/kwv189. kwv189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcaya M, Brewster M, Zigler CM, Subramanian S. Area variations in health: A spatial multilevel modeling approach. Health Place. 2012;18:824–831. doi: 10.1016/j.healthplace.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcaya MC, Subramanian S, Rhodes JE, Waters MC. Role of health in predicting moves to poor neighborhoods among Hurricane Katrina survivors. Proceedings of the National Academy of Sciences. 2014;111:16246–16253. doi: 10.1073/pnas.1416950111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auchincloss AH, Roux AVD. A New Tool for Epidemiology: The Usefulness of Dynamic-Agent Models in Understanding Place Effects on Health. Am J Epidemiol. 2008;168:1–8. doi: 10.1093/aje/kwn118. [DOI] [PubMed] [Google Scholar]
- Bancroft C, Joshi S, Rundle A, Hutson M, Chong C, Weiss CC, et al. Association of proximity and density of parks and objectively measured physical activity in the United States: A systematic review. Soc Sci Med. 2015;138:22–30. doi: 10.1016/j.socscimed.2015.05.034. [DOI] [PubMed] [Google Scholar]
- Beyer K, Wallis AB, Hamberger LK. Neighborhood environment and intimate partner violence: a systematic review. Trauma Violence Abuse. 2015;16:16–47. doi: 10.1177/1524838013515758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black JL, Macinko J. Neighborhoods and obesity. Nutr Rev. 2008;66:2–20. doi: 10.1111/j.1753-4887.2007.00001.x. [DOI] [PubMed] [Google Scholar]
- Brown P, Morello-Frosch R, Brody JG, Altman RG, Rudel RA, Senier L, Pérez C, Simpson R. Institutional review board challenges related to community-based participatory research on human exposure to environmental toxins: A case study. Environ Health. 2010;9:39. doi: 10.1186/1476-069X-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande SS, Whitt-Glover MC, Lancaster KJ, Odoms-Young AM, Gary TL. Built environment and health behaviors among African Americans: a systematic review. Am J Prev Med. 2009;36:174–181. doi: 10.1016/j.amepre.2008.09.037. [DOI] [PubMed] [Google Scholar]
- Chaix B. Geographic life environments and coronary heart disease: a literature review, theoretical contributions, methodological updates, and a research agenda. Annu Rev Public Health. 2009;30:81–105. doi: 10.1146/annurev.publhealth.031308.100158. [DOI] [PubMed] [Google Scholar]
- Christian H, Zubrick SR, Foster S, Giles-Corti B, Bull F, Wood L, et al. The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health Place. 2015;33:25–36. doi: 10.1016/j.healthplace.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Lantz P. Urban built environments and trajectories of mobility disability: findings from a national sample of community-dwelling American adults (1986–2001) Social science & medicine. 2009;69:964–970. doi: 10.1016/j.socscimed.2009.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corral I, Landrine H, Hall MB, Bess JJ, Mills KR, Efird JT. Residential Segregation and Overweight/Obesity Among African-American Adults: A Critical Review. Front Public Health. 2015;3:169. doi: 10.3389/fpubh.2015.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vet E, de Ridder DT, de Wit JB. Environmental correlates of physical activity and dietary behaviours among young people: a systematic review of reviews. Obes Rev. 2011;12:e130–142. doi: 10.1111/j.1467-789X.2010.00784.x. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV. Neighborhoods and health: where are we and were do we go from here? Rev Dépidémiologie Santé Publique. 2007;55:13–21. doi: 10.1016/j.respe.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Diez-Roux AV. Investigating Neighborhood and Area Effects on Health. Am J Public Health. 2001;91:1783–1789. doi: 10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE. Neighborhood environment and physical activity among youth a review. Am J Prev Med. 2011;41:442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- Dunn EC, Winning A, Zaika N, Subramanian S. Does poor health predict moving, move quality, and desire to move?: A study examining neighborhood selection in US adolescents and adults. Health Place. 2014;30:154–164. doi: 10.1016/j.healthplace.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16:175–190. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Foster S, Giles-Corti B. The built environment, neighborhood crime and constrained physical activity: an exploration of inconsistent findings. Prev Med. 2008;47:241–251. doi: 10.1016/j.ypmed.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Frank LD, Saelens BE, Powell KE, Chapman JE. Stepping towards causation: Do built environments or neighborhood and travel preferences explain physical activity, driving, and obesity? Soc Sci Med. 2007;65:1898–1914. doi: 10.1016/j.socscimed.2007.05.053. [DOI] [PubMed] [Google Scholar]
- Gehlke CE, Biehl K. Certain effects of grouping upon the size of the correlation coefficient in census tract material. Journal of the American Statistical Association. 1934;29:169–170. [Google Scholar]
- Graif C. Delinquency and gender moderation in the moving to opportunity intervention: The role of extended neighborhoods. Criminology. 2015;53:366–398. [Google Scholar]
- Jackson N, Denny S, Ameratunga S. Social and socio-demographic neighborhood effects on adolescent alcohol use: a systematic review of multi-level studies. Soc Sci Med. 2014;115:10–20. doi: 10.1016/j.socscimed.2014.06.004. [DOI] [PubMed] [Google Scholar]
- James P, Hart JE, Arcaya MC, Feskanich D, Laden F, Subramanian SV. Neighborhood Self-Selection: The Role of Pre-Move Health Factors on the Built and Socioeconomic Environment. Int J Environ Res Public Health. 2015;12:12489–12504. doi: 10.3390/ijerph121012489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiol Rev. 2008;30:101–117. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- Koohsari MJ, Sugiyama T, Sahlqvist S, Mavoa S, Hadgraft N, Owen N. Neighborhood environmental attributes and adults’ sedentary behaviors: Review and research agenda. Prev Med. 2015;77:141–149. doi: 10.1016/j.ypmed.2015.05.027. [DOI] [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian S, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) J Epidemiol Community Health. 2003;57:186–199. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan MP. The uncertain geographic context problem. Annals of the Association of American Geographers. 2012;102:958–968. [Google Scholar]
- Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62:940–946. doi: 10.1136/jech.2007.066605. 948 p following 946. [DOI] [PubMed] [Google Scholar]
- Major JM, Oliver MN, Doubeni CA, Hollenbeck AR, Graubard BI, Sinha R. Socioeconomic status, healthcare density, and risk of prostate cancer among African American and Caucasian men in a large prospective study. Cancer Causes & Control. 2012;23:1185–1191. doi: 10.1007/s10552-012-9988-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major JM, Sargent JD, Graubard BI, Carlos HA, Hollenbeck AR, Altekruse SF, et al. Local geographic variation in chronic liver disease and hepatocellular carcinoma: contributions of socioeconomic deprivation, alcohol retail outlets, and lifestyle. Annals of epidemiology. 2014;24:104–110. doi: 10.1016/j.annepidem.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markossian TW, Hines RB, Bayakly R. Geographic and Racial Disparities in Breast Cancer–Related Outcomes in Georgia. Health services research. 2014;49:481–501. doi: 10.1111/1475-6773.12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer M, Rohl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74:1204–1212. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Archives of general psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Michael YL, Gold R, Perrin N, Hillier TA. Built environment and change in body mass index in older women. Health & place. 2013;22:7–10. doi: 10.1016/j.healthplace.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Nyden P. Academic incentives for faculty participation in community-based participatory research. J Gen Intern Med. 2003;18:576–585. doi: 10.1046/j.1525-1497.2003.20350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes JM. Commentary: advancing neighbourhood-effects research—selection, inferential support, and structural confounding. Int J Epidemiol. 2006;35:643–647. doi: 10.1093/ije/dyl054. [DOI] [PubMed] [Google Scholar]
- Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58:1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Oakes JM, Andrade KE, Biyoow IM, Cowan LT. Twenty years of neighborhood effect research: an assessment. Current Epidemiology Reports. 2015;2:80–87. doi: 10.1007/s40471-015-0035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes JM, Andrade KN. Methodologic innovations and advances in social epidemiology. Current Epidemiology Reports. 2014;1:38–44. [Google Scholar]
- Openshaw S, Taylor PJ. A million or so correlation coefficients: three experiments on the modifiable areal unit problem. Statistical applications in the spatial sciences. 1979;21:127–144. [Google Scholar]
- Owen N, Humpel N, Leslie E, Bauman A, Sallis JF. Understanding environmental influences on walking; Review and research agenda. Am J Prev Med. 2004;27:67–76. doi: 10.1016/j.amepre.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The Built Environment and Obesity. Epidemiol Rev. 2007;29:129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert SA, Ruel E. Racial segregation and health disparities between black and white older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61:S203–S211. doi: 10.1093/geronb/61.4.s203. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation. Interdisciplinary Research Leaders [WWW Document] RWJF; 2016. URL http://www.rwjf.org/en/library/funding-opportunities/2016/interdisciplinary-research-leaders.html (accessed 5.6.16) [Google Scholar]
- Safron M, Cislak A, Gaspar T, Luszczynska A. Micro-environmental characteristics related to body weight, diet, and physical activity of children and adolescents: a systematic umbrella review. Int J Environ Health Res. 2011;21:317–330. doi: 10.1080/09603123.2011.552713. [DOI] [PubMed] [Google Scholar]
- Sellstrom E, Bremberg S. The significance of neighbourhood context to child and adolescent health and well-being: a systematic review of multilevel studies. Scand J Public Health. 2006;34:544–554. doi: 10.1080/14034940600551251. [DOI] [PubMed] [Google Scholar]
- Sharkey P. The Intergenerational Transmission of Context1. American Journal of Sociology. 2008;113:931–969. [Google Scholar]
- Sharkey P. Stuck in place: Urban neighborhoods and the end of progress toward racial equality. University of Chicago Press; 2013. [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, Sherbourne CD. The importance of social context: neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Social science & medicine. 2007;65:1867–1881. doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian SV, O’Malley AJ. Modeling neighborhood effects: the futility of comparing mixed and marginal approaches. Epidemiol Camb Mass. 2010;21 doi: 10.1097/EDE.0b013e3181d74a71. 475-478-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S, Chen JT, Rehkopf DH, Waterman PD, Krieger N. Racial disparities in context: a multilevel analysis of neighborhood variations in poverty and excess mortality among black populations in Massachusetts. American Journal of Public Health. 2005;95:260–265. doi: 10.2105/AJPH.2003.034132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S, Elwert F, Christakis N. Widowhood and mortality among the elderly: The modifying role of neighborhood concentration of widowed individuals. Social science & medicine. 2008;66:873–884. doi: 10.1016/j.socscimed.2007.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton RLJ, Greiner A, Fichtenberg CM, Feingold BJ, Ellen JM, Jennings JM. Achieving a Healthy Zoning Policy in Baltimore: Results of a Health Impact Assessment of the TransForm Baltimore Zoning Code Rewrite. Public Health Rep. 2013;128:87. doi: 10.1177/00333549131286s313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. J Ment Health Policy Econ. 2006;9:137–154. [PubMed] [Google Scholar]
- Vos AA, Posthumus AG, Bonsel GJ, Steegers EA, Denktas S. Deprived neighborhoods and adverse perinatal outcome: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2014;93:727–740. doi: 10.1111/aogs.12430. [DOI] [PubMed] [Google Scholar]
- Xiao H, Gwede CK, Kiros G, Milla K. Analysis of prostate cancer incidence using geographic information system and multilevel modeling. Journal of the National Medical Association. 2007;99:218. [PMC free article] [PubMed] [Google Scholar]
- Xiao H, Tan F, Goovaerts P. Racial and geographic disparities in late-stage prostate cancer diagnosis in Florida. Journal of health care for the poor and underserved. 2011;22:187. doi: 10.1353/hpu.2011.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. American Journal of Epidemiology. 1999;149:898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37:455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Onufrak S, Holt JB, Croft JB. A multilevel approach to estimating small area childhood obesity prevalence at the census block-group level. Prev Chronic Dis. 2013;10:E68. doi: 10.5888/pcd10.120252. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


