Abstract
Background
Little is known about the reach and impact of collaborative care for depression outside of clinical trials.
Objectives
To examine the effect of a collaborative care intervention for depression on the rates of depression diagnosis, use of specific depression codes, and treatment intensification.
Research Design
Evaluation of a staggered, multiple baseline implementation initiative
Subjects
Patients receiving depression care in primary care clinics throughout Minnesota from February 2008 through March 2011
Measures
Data regarding depression diagnosis rates and codes, and measures of antidepressant intensification were provided by health insurers
Results
DIAMOND affected neither rates of depression recognition nor use of depression diagnostic codes, and the overall reach of DIAMOND was disappointingly small. Patients in DIAMOND had more episodes of treatment intensification than non-DIAMOND patients, but we were unable to account for depression severity in our analysis.
Conclusions
DIAMOND did not affect depression recognition or diagnostic coding, but may have affected treatment intensification. Our results suggest that even strongly evidence-based interventions may have little contamination effects on patients not enrolled in the new care model.
Keywords: Depression, Primary Care, Collaborative Care, Implementation
INTRODUCTION
All too often, what looks promising in randomized clinical trials with highly selected patient populations, additional resources, and substantial control of the intervention may not be feasible or as effective when implemented in the real clinical world. While healthcare delivery and insurance leaders in Minnesota knew that collaborative care for depression was effective in randomized trials, they also recognized it was rarely being used.1 A primary reason for this seemed to be that its key services, particularly encounters with care managers, were not reimbursable. Given this, healthcare delivery and insurance leaders worked together with the Institute for Clinical Systems Improvement (ICSI), a regional quality improvement organization, to provide a new payment model for clinics trained to provide collaborative depression care. These efforts resulted in an initiative called DIAMOND (Depression Improvement Across Minnesota: Offering a New Direction).
The DIAMOND Initiative provided a unique opportunity to study the implementation of the collaborative care model for depression and examine its reach and impact on unenrolled patients. This examination is important because a growing emphasis on implementation of evidence-based treatment brings a responsibility to examine the degree of implementation and its intended and unintended effects. Additionally, real-world implementation may involve sacrificing some fidelity to the model, leading to additional learnings about how implementation differs from previous randomized clinical trials and informing future endeavors to spread this treatment.
Because collaborating healthcare payers provided claims data for all insured patients receiving antidepressant medications, we had the opportunity to examine important questions about implementation, specifically: (1) Did DIAMOND affect the percentage of patients receiving depression codes? (2) Since DIAMOND insurance payments were only for patients with certain depression codes, did DIAMOND influence the use of those codes? (3) As a key feature of the collaborative care model is to intensify treatment when needed, were DIAMOND patients more likely to receive treatment intensification than others with depression?
METHODS
Participants
Participants were patients with depression insured by a participating healthcare insurance plan and receiving antidepressant medications for depression in a primary care clinic. Nearly all of the large healthcare payers in Minnesota (Blue Cross Blue Shield, HealthPartners, Medica, Preferred One and UCare) sent de-identified data to the study team for insured members with a new prescription for an antidepressant (identified via national drug codes and/or generic product identifiers) during the period of the initiative’s implementation, February 2008 through March 2011. Payer data indicated which patients had diagnoses of major depression (ICD9 codes 296.2 and 296.3), dysthymia (300.4) or depressive disorder, not elsewhere classified (311).
Design
The DIAMOND Initiative has been described previously,2–4 but its key features were adopted from the largest study of the collaborative care model for depression to date, the IMPACT study.5 As such, the DIAMOND care model specified systematic patient follow-up and monitoring by trained on-site care managers who reviewed cases weekly with a consultant psychiatrist, consistent use of the PHQ96,7 to monitor depression severity, treatment intensification for patients not improving, and depression relapse prevention for patients achieving remission. In order to study this complex initiative, both initiative and research leaders agreed on an implementation design that was minimally disruptive for participants yet vigorous enough to allow study of its effectiveness, resulting in a staggered implementation design. Over 2.5 years, the initiative was implemented in 75 clinics in five sequences that were six months apart.
Training was facilitated by ICSI and conducted for 6 months prior to implementation for each site. The involved staff at each clinic, including physicians, care managers, and care manager supervisors, met with ICSI for four face-to-face training sessions and two webinars that covered each component of the DIAMOND care model, such as PHQ9 use, depression management, registry development and use, and the new roles of the care manager and consulting psychiatrist. In addition, care managers attended a 1.5-day training session just prior to implementation that focused on their role, workflow, and skill-building for motivational interviewing, behavioral activation, and handling difficult cases. Training materials included checklists for implementation, example clinical workflows, evidence-based guidelines, patient materials and brochures, and tools and scripts for each team member. Monthly care manager calls were conducted throughout DIAMOND implementation to facilitate sharing and discussing tools and processes that were working well, as well as challenges and frustrations. Each site was given ongoing feedback about their enrollment and outcomes for their own quality improvement work.
Payment for DIAMOND services was a flat monthly per-participant amount which was limited to patients who had major depression (ICD9 codes 296.2, 296.3) or dysthymia (300.4) and were seen in participating clinics. Depression NOS (311) was excluded from reimbursement because guidelines for treating this diagnosis were lacking, and because the DIAMOND initiative wanted to encourage more precise depression diagnoses. Payment was independently negotiated between participating health plans and medical groups but billed using a common DIAMOND-specific code that allowed tracking of patients recruited into DIAMOND care. Accordingly, patients were defined as having received DIAMOND care if there was a DIAMOND-specific billing code associated with their care in any given month.
Analysis
To be included in the main analyses, patients needed a diagnostic code for depression at least once during the observation period. Patients with prescriptions for antidepressants but without a depression diagnosis code were not included.
To determine whether DIAMOND influenced the percentage of patients diagnosed with depression, we calculated the proportion of all primary care patients who received depression diagnoses in each month in each sequence. We then tested for statistically significant differences pre- versus post-implementation by including a timexDIAMOND interaction term in a mixed linear regression model weighted by clinic size.
To determine whether the use of depression diagnostic codes was affected by DIAMOND, we restricted the analysis to patients with depression. We then counted the number of patients with ICD9 codes of 296.2, 296.3, or 300.4 in a given month divided by the total number of patients seen in all clinics that month.
To determine whether DIAMOND patients were more likely to receive treatment intensification, only patients seen in clinics after DIAMOND was implemented in one of these clinics were included. Since our claims data did not provide information about dosage or days’ supply, we defined treatment intensification as the dispensing of any new antidepressant medication observed in a 3-month period. This included either changing from one antidepressant to another or adding another antidepressant to the current regimen. The number of unique antidepressants dispensed for a patient in a 3-month period was counted, and treatment intensification occurred each time the number of unique antidepressants per patient increased relative to the previous 3-month period. A chi square test was used to test for differences in having treatment intensification by receipt of DIAMOND care as indicated by a DIAMOND-specific billing code.
RESULTS
A total of 106,931 patients with a prescription for an antidepressant had 1,114,207 primary care visits at 75 clinics with 973 providers. Of these, 37,859 patients with antidepressant prescriptions without diagnoses of depression were excluded; the largest excluded group was 19,933 patients with generalized anxiety disorder but not depression. Our final sample included 854,293 visits for 69,072 patients with depression, including 757,570 person-months of observation and a median person-month follow-up of 8 months (interquartile range 3–16 months) (Table 1).
Table 1.
Number of medical groups, clinics, clinicians and patients by sequence.
| Sequence | Medical groups N |
Clinics N (%) |
Clinicians N (%) |
Patients N (%) |
Patients per Clinician |
|---|---|---|---|---|---|
| 1 | 5 | 10 (13%) | 98 (10%) | 8675 (13%) | 88.5 |
| 2 | 8 | 20 (27%) | 433 (45%) | 26660 (39%) | 61.6 |
| 3 | 6 | 15 (20%) | 114 (12%) | 9658 (14%) | 84.7 |
| 4 | 7 | 12 (16%) | 148 (15%) | 10996 (16%) | 74.3 |
| 5 | 6 | 18 (24%) | 180 (18%) | 13083 (19%) | 72.7 |
| Total | 75 | 973 | 69,072 |
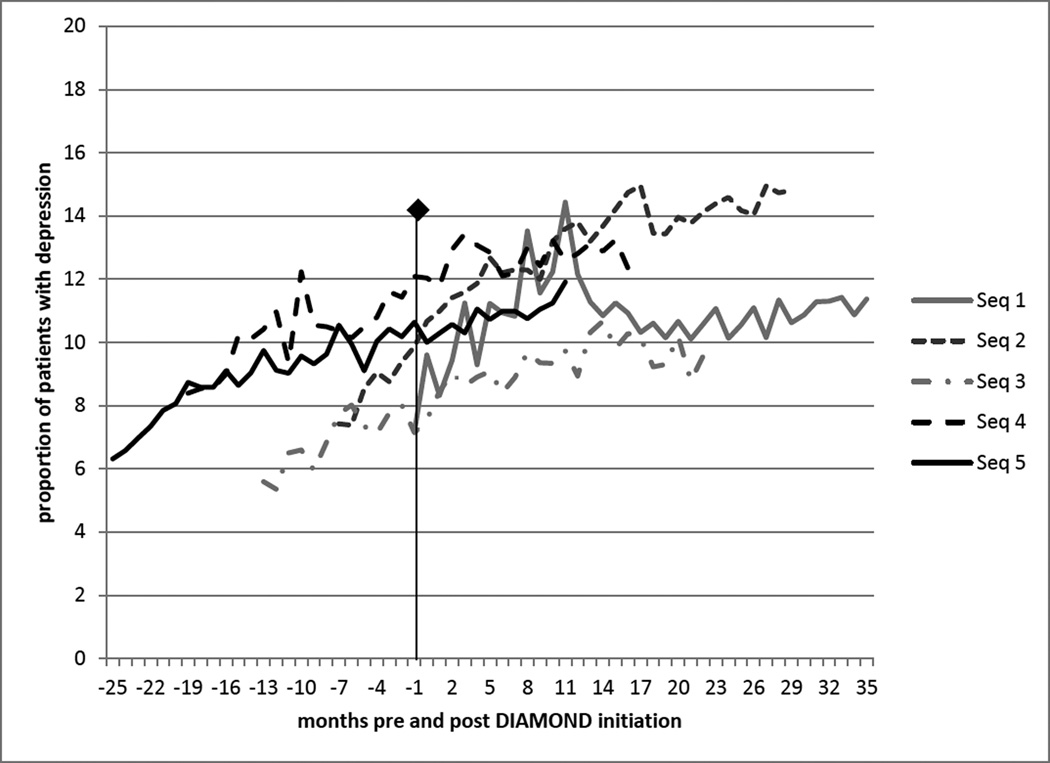
DIAMOND did not influence the percentage of patients receiving depression codes in primary care clinics (Figure 1). While there was a general increase in depression diagnoses over time, there was no additional observed increase following DIAMOND implementation. In fact, for all DIAMOND sequences combined, the slope of depression diagnoses was higher before DIAMOND implementation than following it (0.153 versus 0.013, p<0.001).
Figure 1.
Frequency of Diagnosis of Depression Pre- and Post-DIAMOND Implementation in Each Sequence.
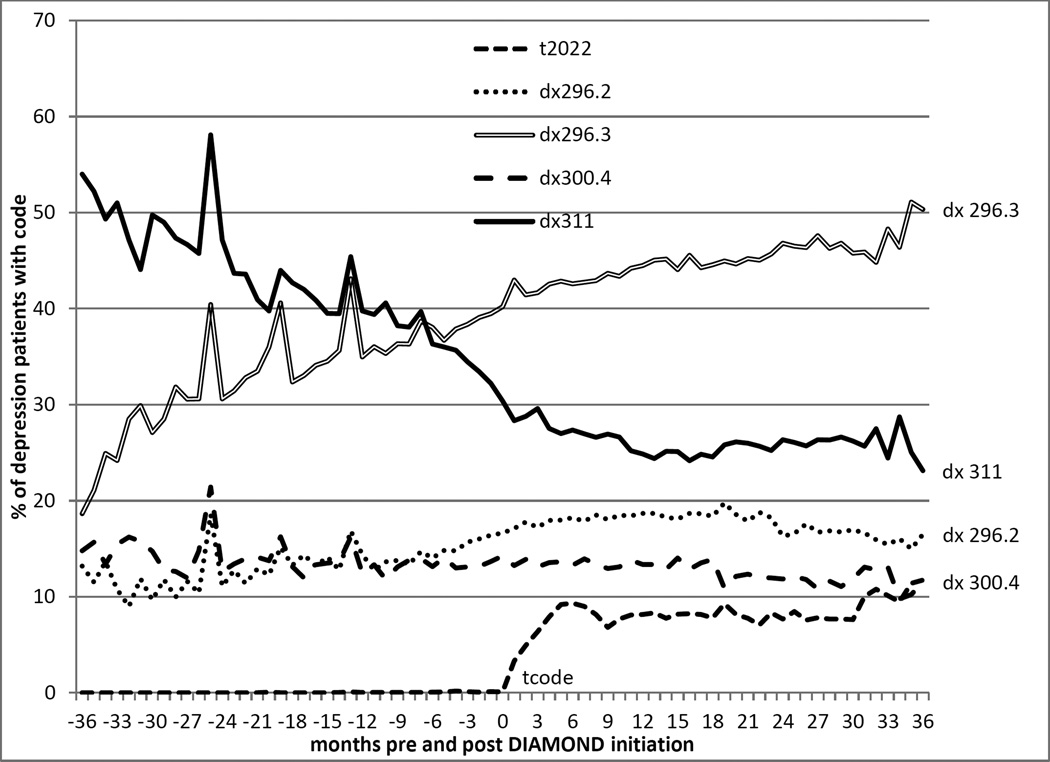
DIAMOND also did not influence providers’ use of specific diagnostic codes for depression. As seen in Figure 2, there was an increase in the use of the single episode major depression code (296.2), and a decrease in the use of depression not otherwise specified (311), but these changes were present before DIAMOND and continued afterward without apparent influence by DIAMOND implementation. There were no significant changes in the use of codes for recurrent major depression (296.3) or dysthymia (300.4).
Figure 2.
Frequency of Use of Various Depression Diagnostic Codes Pre- and Post-DIAMOND Implementation.
DIAMOND patients were more likely to receive treatment intensification (Table 2). While 15.2% of the 2976 patients receiving DIAMOND care had at least one treatment intensification, 10.9% of the 44,347 non-DIAMOND patients seen after DIAMOND implementation had evidence of treatment intensification, a significant difference (p<0.0001). Of those patients with any treatment intensification in either group, the vast majority of patients (78–79%) had only one.
Table 2.
Treatment Intensification.
| Number of Treatment Intensifications |
Non-DIAMOND Patients N (%) |
DIAMOND Patients N (%) |
P-Value |
|---|---|---|---|
| Any treatment intensification |
4820 (10.9%) | 451 (15.2%) | P<0.0001 |
| 1 | 3830 (8.6%) | 352 (11.8%) | P<0.0001 |
| 2 | 804 (2%) | 82 (2.8%) | |
| 3 | 156 (0.4%) | 13 (0.4%) | |
| 4 | 27 (0.1%) | 4 (0.1%) | |
| 5 | 3 (0.01%) | 0 (0%) |
DISCUSSION
Despite significant changes in care delivery and reimbursement for patients with specific depression codes, DIAMOND did not appear to affect either rates of depression recognition or use of diagnostic codes, and the overall reach of DIAMOND was disappointingly small. Patients in DIAMOND did have more measurable episodes of treatment intensification than patients with depression treated outside of this collaborative care initiative, but this may have been an appropriate difference, as claims data do not include any measures of depression severity.
DIAMOND implementation did not affect how often depression was diagnosed. This finding is likely related to DIAMOND recruitment rates being much lower than anticipated, peaking at only 2.4% of potentially eligible patients, and resulting in low spread of the initiative. The reasons for this are likely multi-factorial, and speak to the daunting task of effectively translating clinical research into practice. Despite the experience and support of ICSI, including significant training for clinical staff and payment changes to make collaborative care more financially feasible for clinics, patients were ultimately recruited into DIAMOND at very low rates. Ultimately, the weak penetration of this intervention may have been related to the low reimbursement level from commercial payers and the absence of coverage for DIAMOND care for those insured by Medicare or Medicaid. Additionally, DIAMOND was not a clinical trial, and as such did not have research assistants to actively identify and recruit subjects, often an arduous task in research that takes significant resources, a factor that may have also contributed to its small reach. Further, participating clinics consistently indicated that many physicians did not refer patients to DIAMOND because of clinical inertia for a nontraditional care model, disagreement with the idea that DIAMOND was needed or that it provided care better care than their existing care, or a sentiment that many patients did not want or need the extra care. Moreover, most clinics were unwilling to implement an automatic opt-in process for patient participation, something that might have significantly improved recruitment. Finally, while ICSI provided clinics with feedback about their recruitment rates, feedback alone likely wasn’t enough to change provider behaviors and workflows.
Another potential reason DIAMOND did not affect depression diagnosis rates had to do with economic changes at the time. National and global data indicate an increase in depression and suicide in western countries that began with the onset of the Great Recession in December 2007, two months before the first sequence of DIAMOND was initiated.8–10 The depression rate increased particularly for men and people of racial and ethnic minorities, and was at least partially related to increased unemployment and decreased housing wealth related to the recession.11–13 These time trends may have overwhelmed any effects of DIAMOND. However, we should note that diagnoses of major depression were increasing in our data as early as February 2006 and continued for at least four years, without a noticeable change in the rate of depression diagnoses with the onset of the Great Recession (or with the implementation of DIAMOND).
While we had expected that DIAMOND implementation would affect diagnostic coding for all patients with depression, this did not happen. Rates of coding for single episodes of depression (ICD9 code 296.2) increased throughout the study period, and rates of coding for depression not otherwise specified (ICD9 code 311) decreased, but these trends were occurring before DIAMOND and were unchanged by DIAMOND implementation. Some of these coding changes may have been related to multiple efforts by led ICSI to change depression care at least four years prior to DIAMOND implementation. ICSI was conducting action groups with a large share of the primary care and behavioral health providers in Minnesota for approximately four years before DIAMOND started, with a primary focus on gaining acceptance of the use of the PHQ9 and diagnosing depression more accurately. This included efforts to educate primary care providers that all health plans were paying for their care of depression and to encourage clinicians to avoid using depression NOS diagnoses unless clinically appropriate. ICSI action group members felt that depression NOS represented a heterogeneous group of depression diagnoses that no one approach would likely work to improve. Instead, action groups focused on working with patients with major depression and dysthymia, where they more confident of what to recommend. Simultaneously, the health plans in MN made their own efforts to improve depression care, largely through increased services for patients with depression. Ultimately, all of these efforts may have had some effects on diagnosis and coding practices. However, DIAMOND’s lack of effect on specific depression codes is likely primarily a consequence of the low rates of penetration of the intervention itself. Ultimately, it is likely that the time trend for these changes was already so strong that any effect on coding DIAMOND implementation may have had was comparably insignificant. In the end, this finding speaks to how difficult it can be to successfully influence care.
Of note, patients in DIAMOND appeared to have had more episodes of treatment intensification, at least as measured by changes between antidepressants or augmentation with a second antidepressant, suggesting that once patients were recruited into DIAMOND, there was a difference in how their depression was treated. Approximately 80% of patients receiving treatment intensification had only one round of such intensification, potentially indicating that these were successful treatment modifications. However, these findings should be interpreted with caution. A limitation of our data is that we do not have information on depression severity, and there was likely selection bias present, with clinicians more likely to recruit patients with more severe or treatment-resistant depression into DIAMOND. If this was the case, the higher level of treatment intensification in DIAMOND patients would have been appropriate. On the other hand, it is also possible that the majority of DIAMOND patients had only one treatment intensification because their treatment team failed to make further needed adjustments despite ongoing depression; again, these data do not let us assess depression response or remission.
Of note, the DIAMOND main results paper reported that remission rates for DIAMOND patients were no different than three comparison groups, despite patients being more satisfied with their care, suggesting that treatment intensification may not have been pursued as often as might have been warranted.14,15 Our finding that apparently higher rates of treatment intensification did not seem to translate into improved depression outcomes is similar to that of a study examining implementation of depression collaborative care in primary care clinics in the Veterans Administration (VA).16 The VA study found that patients who received collaborative care were more likely to receive adequate doses of antidepressants (66% versus 43%, p=0.01), but this did not translate into differences in depression outcomes.
We recognize several limitations of our data. Given the way these data were collected, we do not have patient-level data, including patient characteristics, previous episodes of depression, or comorbid conditions, all of which can affect patient outcomes. Another important limitation is an inability to capture psychotherapy episodes, resulting in patients participating in therapy but not taking antidepressants misclassified as untreated. Our ability to measure depression treatment intensification was somewhat rudimentary, as we were unable to ascertain changes in antidepressant doses or the addition of psychotherapy. Additionally, our cohort was dynamic, with members able to leave or be added over time. However, a strength of this study was our ability to examine a large cohort of patients with a reasonable duration of follow-up during a real-world implementation of the collaborative care model for depression. Additionally, the staggered design of DIAMOND implementation minimized any impact of secular trends during the observation period, and the use of a DIAMOND-specific billing code allowed us to ascertain a patient’s exposure to the intervention.
In conclusion, DIAMOND did not affect the overall depression recognition rates or patterns of diagnostic coding in outpatients with depression. While DIAMOND may have had some effect on treatment intensification, we cannot rule out the possibility of selection bias influencing this finding. Our results suggest that even strongly evidence-based interventions with wide local publicity may have little contamination effects on patients not enrolled in the new care model.
Acknowledgments
Funding/Support: This research was funded by grant #5R01MH080692 from the National Institute of Mental Health.
Footnotes
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 2.Solberg LI, Glasgow RE, Unutzer J, et al. Partnership research: a practical trial design for evaluation of a natural experiment to improve depression care. Med Care. 2010;48(7):576–582. doi: 10.1097/MLR.0b013e3181dbea62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crain AL, Solberg LI, Unutzer J, et al. Designing and implementing research on a statewide quality improvement initiative: the DIAMOND study and initiative. Med Care. 2013;51(9):e58–e66. doi: 10.1097/MLR.0b013e318249d8a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solberg LI, Crain AL, Jaeckels N, et al. The DIAMOND initiative: implementing collaborative care for depression in 75 primary care clinics. Implement Sci. 2013;8:135. doi: 10.1186/1748-5908-8-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 6.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) J Affect Disord. 2004;81(1):61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- 8. [Accessed March 9, 2016];US Business Cycle Expansions and Contractions. http://www.nber.org/cycles.html.
- 9.Chang SS, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013;347:f5239. doi: 10.1136/bmj.f5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehta K, Kramer H, Durazo-Arvizu R, Cao G, Tong L, Rao M. Depression in the US population during the time periods surrounding the great recession. J Clin Psychiatry. 2015;76(4):e499–e504. doi: 10.4088/JCP.14m09637. [DOI] [PubMed] [Google Scholar]
- 11.Kendrick T, Stuart B, Newell C, Geraghty AW, Moore M. Changes in rates of recorded depression in English primary care 2003–2013: Time trend analyses of effects of the economic recession, and the GP contract quality outcomes framework (QOF) J Affect Disord. 2015;180:68–78. doi: 10.1016/j.jad.2015.03.040. [DOI] [PubMed] [Google Scholar]
- 12.Yilmazer T, Babiarz P, Liu F. The impact of diminished housing wealth on health in the United States: evidence from the Great Recession. Soc Sci Med. 2015;130:234–241. doi: 10.1016/j.socscimed.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 13.Riumallo-Herl C, Basu S, Stuckler D, Courtin E, Avendano M. Job loss, wealth and depression during the Great Recession in the USA and Europe. Int J Epidemiol. 2014;43(5):1508–1517. doi: 10.1093/ije/dyu048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solberg LIC, AL, Maciosek M, Unutzer J, Ohnsorg K, Beck A, Rubenstein L, Whitebird RR, Rossom RC, Pietruszewski PB, Crabtree BF, Joslyn K, Van de Ven A, Glasgow RE. A Stepped Wedge Evaluation of an Initiative to Spread the Collaborative Care Model for Depression in Primary Care. Annals of Family Medicine. doi: 10.1370/afm.1842. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solberg LI, Crain AL, Maciosek MV, et al. A Stepped-Wedge Evaluation of an Initiative to Spread the Collaborative Care Model for Depression in Primary Care. Ann Fam Med. 2015;13(5):412–420. doi: 10.1370/afm.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaney EF, Rubenstein LV, Liu CF, et al. Implementing collaborative care for depression treatment in primary care: a cluster randomized evaluation of a quality improvement practice redesign. Implement Sci. 2011;6:121. doi: 10.1186/1748-5908-6-121. [DOI] [PMC free article] [PubMed] [Google Scholar]