Abstract
Purpose
Both pediatric urologists and pediatric surgeons perform hernia repairs, hydrocelectomies and orchiopexies. We hypothesized that surgeons perform more incarcerated and female hernia repairs while urologists perform more orchiopexies and hydrocelectomies.
Methods
The Vizient-AAMC Faculty Practice Solutions Center® database was queried from January 2009 to December 2014 to identify patients 10 years or younger who underwent the above procedures performed by pediatric specialists. Age, gender, race, insurance, geographic region and surgeon volume were examined.
Results
In the study 55,893 surgeries were identified; 26,073 primary hernia repairs, 462 recurrent hernia repairs, 3,399 laparoscopic hernia repairs, 9,414 hydrocele repairs and 16,545 orchiopexies. Pediatric surgeons performed 89% of primary hernia repairs with an annual median surgeon volume of 4 cases/year. Pediatric urologists performed 62% of hydrocelectomies and 83% of orchiopexies with annual median surgeon volumes of 6 and 24, respectively. Pediatric surgeons performed all procedures in younger patients and performed more female and incarcerated hernia repairs.
Conclusions
Pediatric surgeons operated on younger patients and treat more patients with inguinal hernias while pediatric urologists care for more boys with undescended testes and hydroceles. This knowledge of referral patterns and care between specialties with overlapping expertise will allow improvements in training and access.
LEVELS OF EVIDENCE
Cost Effectiveness Study, Level of Evidence III
Keywords: hernia repair, hydrocele, undescended testicle, practice pattern, epidemiology
1.0 INTRODUCTION
Pediatric hernia repairs, hydrocelectomies and orchiopexies are common procedures performed by both pediatric surgeons and pediatric urologists. Using the Taiwan National Health Insurance database, Chang et al. estimated the cumulative incidence of pediatric hernias to be 6.62% in boys and 0.74% in girls aged 15 years and younger.[1] Using the same database, Pan et al. estimated the incidence of inguinal hernia repairs to be 4.2% in children aged 6 years and younger over a 7 year period.[2] The incidence of congenital undescended testicles in full term boys is estimated to be 2–4% at birth and 1% by age 1 with cumulative incidences of orchiopexy to be 2–4%.[3] Despite numerous outcome analyses and these being the most common procedures in children, there are no studies evaluating who are in fact performing these surgeries, pediatric urologists or pediatric surgeons.[4–6]
In the United States, adults with hernias are almost universally referred to general surgeons. Similarly, men with hydroceles are referred to urologists. On the other hand, for children, both procedures are performed by pediatric urologists and surgeons. This study has aimed to evaluate the practice patterns of pediatric hernia, hydrocele and undescended testicle repair in the United States academic centers. This type of data is very important when analyzing surgical training, volume-based outcomes, quality of care and access. We hypothesized that pediatric surgeons perform more female and incarcerated hernia repairs and pediatric urologists perform more hydrocelectomies and orchiopexies.
2.0 METHODS AND MATERIALS
2.1 Data Source
The Vizient-AAMC Faculty Practice Solutions Center (FPSC) database was developed by the Vizient, Inc. and the Association of American Medical Colleges to characterize physician productivity.[7] The database includes data from more than 90 faculty practice plans from across the country and has been used to study patterns of surgical practice at academic institutions.[8–10]
Within the database, surgery is subclassified into general, trauma, burn, thoracic, cardiac, plastic, oncology, vascular, pediatric and transplant surgery. Urology currently has no subcategorizations. To specifically identify pediatric surgeons and pediatric urologists, the FPSC database was queried from January 2009 to December 2014 to find any physician performing inguinal hernia repair, hydrocele repair or orchiopexy in patients under 10 years of age based on each respective CPT code (Supplemental Table 1). The number of new patient visits was determined for each identified physician and only cases performed by physicians whose practices consisted of 50% or greater patients age 18 or less were included in analyses. The primary scrotal/inguinal pathology for which the patient was treated was identified based on ICD9 codes for each respective condition (Supplemental Table 2).
2.2 Statistical Analysis
For each procedure, patient characteristics of age, gender, race, insurance and geographic region were examined. For hernia repair, subset analyses were performed for primary repair in preterm infants, incarcerated hernia, female hernia, laparoscopic hernia repair and recurrent hernia repair. For hydrocele repair, subset analyses were performed for repair by scrotal approach and inguinal approach. For orchiopexy, subset analyses were performed for inguinal, open abdominal and laparoscopic assisted approaches. The laparoscopic approach was included as this still includes scrotal or inguinal incisions and we did not want to bias the analysis by excluding abdominal testes.
Categorical patient characteristics such as gender, race (non-white vs. white for subjects with known race) and insurance (commercial vs. non-commercial) were compared between pediatric urologists and pediatric surgeons using logistic regression models with standard errors adjusted for within-hospital correlation using generalized estimating equations (GEE). Mean patient age was compared between pediatric urologists and surgeons using a linear mixed effects model including a random effect for hospital. Geographic regions were compared between pediatric urologists and surgeons using chi-square tests. As the FPSC database has surgeon specific identifiers, the annual case volume for each surgeon for each procedure was calculated. Concurrent bilateral procedures in a single patient were considered a single case. Surgeon volume was compared between pediatric urologists and surgeons using negative binomial regression models with standard errors adjusted for within-hospital correlation using GEE. Analyses were conducted using SAS software for Windows, version 9.4 (SAS Institute, Cary, NC).
3.0 RESULTS
During the 6-year period, 55,893 cases were performed by 632 doctors, 443 pediatric surgeons and 189 pediatric urologists at 73 hospitals.
3.1 Hernia Repair
3.1.1 Primary Hernia Repair
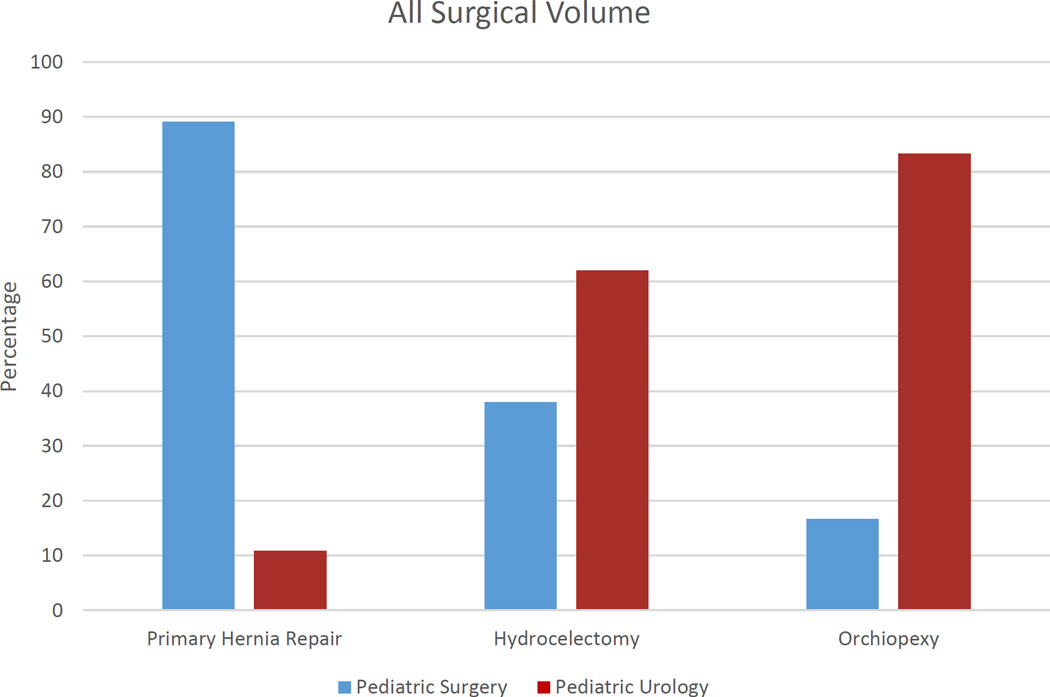
A total of 26,073 primary hernia repairs were performed by both specialties and 89% were performed by pediatric surgeons (Figure 1). For all primary repairs, pediatric surgeons treated younger patients than pediatric urologists (p<0.001) with patients 2 years and younger accounting for greater than 50% of the general surgery cases. Pediatric surgeons also treated a higher proportion of non-white patients than pediatric urologists (p=0.008) (Table 1, Figure 1).
Figure 1.
Comparison of Case Volumes between Pediatric Surgeons and Urologists
Table 1.
Primary Hernia Repair
| Patient Characteristic | General Surgery (23,247 Cases 425 Surgeons) |
Urology (2,826 Cases 146 Surgeons) |
All Cases (26,073 Cases 571 Surgeons) |
P-Value |
|---|---|---|---|---|
| Age (Years) | <0.001a | |||
| 0—1 | 6969 (30%) | 413 (15%) | 7382 (28%) | |
| 1—2 | 5475 (24%) | 617 (22%) | 6092 (23%) | |
| 2—3 | 3253 (14%) | 581 (21%) | 3834 (15%) | |
| 3—4 | 2335 (10%) | 386 (14%) | 2721 (10%) | |
| 4—5 | 2199 (9%) | 353 (12%) | 2552 (10%) | |
| 5--6 | 1717 (7%) | 291 (10%) | 2008 (8%) | |
| 6--10 | 1299 (6%) | 185 (7%) | 1484 (6%) | |
| Gender | <0.001 | |||
| Female | 5753 (25%) | 243 (9%) | 5996 (23%) | |
| Male | 17494 (75%) | 2583 (91%) | 20077 (77%) | |
| Race | 0.008b | |||
| Asian | 403 (2%) | 37 (1%) | 440 (2%) | |
| Black | 3507 (15%) | 257 (9%) | 3764 (14%) | |
| Hispanic | 800 (3%) | 78 (3%) | 878 (3%) | |
| White | 6946 (30%) | 909 (32%) | 7855 (30%) | |
| Other | 1154 (5%) | 116 (4%) | 1270 (5%) | |
| Unknown | 10437 (45%) | 1429 (51%) | 11866 (46%) | |
| Insurance | 0.149c | |||
| Commercial | 10298 (44%) | 1345 (48%) | 11643 (45%) | |
| Medicaid | 10685 (46%) | 1170 (41%) | 11855 (45%) | |
| Self Pay/Other | 2264 (10%) | 311 (11%) | 2575 (10%) |
For test comparing mean patient age between specialties
For test comparing proportions of white vs. nonwhite subjects, in subjects with known race.
For test comparing proportion of subjects with commercial vs. non-commercial insurance.
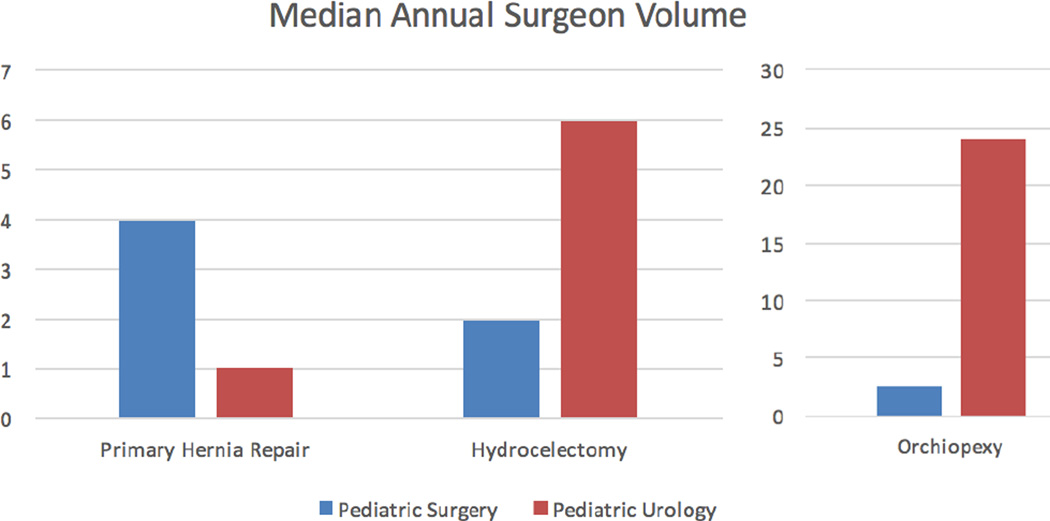
The distribution of surgeons by specialty and region was evaluated to see if the differences were secondary to availability of urologists in the region. The proportions of urologists did not differ significantly between regions (data not shown). Surgeon volume was higher for pediatric surgeons than pediatric urologists for all hernia surgery types (Supplemental Table 3). For primary hernia repairs, pediatric surgeons had a median surgeon volume of 4 cases/year (range 0–36) compared to that of urologists of 1 case/year (range 0–20) (Supplemental Table 3, Figure 2).
Figure 2.
Comparison of Median Case Volumes between Pediatric Surgeons and Urologists
3.1.2 Incarcerated Hernia Repair
There were 1,460 cases of incarcerated hernia repair and 94% were performed by pediatric surgeons. Pediatric surgeons performed repairs of incarcerated hernias in younger patients (p<0.001); patients aged 1 and less accounted for 40% of these cases. Pediatric surgeons also performed incarcerated hernia repairs in a higher proportion of patients with non-commercial insurance (p<0.001) (Supplemental Table 4).
3.1.3 Hernia Repair in Preterm Infants
Of the 26,073 cases, 5,375 cases were performed in pre-term infants and 97% of these cases were performed by pediatric surgeons. Pediatric surgeons performed more primary open repairs in non-white preterm infants than pediatric urologists (Supplemental Table 5).
3.1.4 Recurrent Hernia Repair
There were 462 recurrent hernia repairs and 92% were performed by pediatric surgeons. Pediatric surgeons performed more recurrent hernia repairs in female patients than urologists with female patients accounting for 24% of their recurrent hernia cases (p=0.01) (Supplemental Table 6).
3.1.5 Female Hernia Repair
Female hernias accounted for 5,996 cases and 96% of these cases were performed by pediatric surgeons. In the primary repair group, female patients accounted for 25% of the general surgery cases as compared to 9% of the urologic cases. Overall, pediatric surgeons repaired female hernias in younger patients (p<0.001), in more non-white patients (p=0.003) and in a higher proportion of patients with non-commercial insurance (p=0.002) (Supplemental Table 7).
3.1.6 Laparoscopic Hernia Repair
There were 3,399 laparoscopic hernia repairs and 96% of these cases were performed by pediatric surgeons. Pediatric surgeons performed laparoscopic repairs in younger patients (p<0.001), primarily under the age of 3, and in more non-white patients (p=0.04) (Supplemental Table 8). Gender differences were not found to be significant.
3.2 Hydrocelectomy
A total of 9,414 hydrocelectomies were performed by both specialties and 38% were performed by pediatric surgeons (Figure 1). The distribution of surgeon specialties was evaluated by region and the relative proportions of pediatric urologists and general surgeons did not differ by region (data not shown). Surgeon volume was significantly higher for pediatric urologists than pediatric surgeons (p<0.001) (median 6.0 vs. 2.0 cases per year) (Table 2, Figure 2). Patients treated by pediatric urologists were older than those treated by general surgeons (p<0.001) with a mean age of 3.5 years compared to 2.7 (Table 2).
Table 2.
Hydrocele Repair
| General Surgery (3,579 Cases 337 Surgeons) |
Urology (5,835 Cases 168 Surgeons) |
All Cases (9,414 Cases 505 Surgeons) |
P-Value | |
|---|---|---|---|---|
| Age (Years) | <0.001a | |||
| N | 3,579 | 5,835 | 9,414 | |
| Mean (SD) | 2.7 (2.2) | 3.5 (2.3) | 3.2 (2.3) | |
| Median (Range) | 2.0 (0.0--10.0 ) | 3.0 (0.0--10.0) | 3.0 (0.0--10.0) | |
| Surgeon Volume | ||||
| All Hydrocele Repairs | 3,579 | 5,835 | 9,414 | |
| Participating Surgeons | 337 | 168 | 505 | |
| Median (Range) Annual Surgeon Volume |
2.0 (0.4--18.3) | 6.0 (0.8--34) | <0.001 | |
| Scrotal Approach | 1,597 | 3,605 | 5,202 | |
| Participating Surgeons | 257 | 154 | 411 | |
| Median (Range) Annual Surgeon Volume |
0.8 (0--11.4) | 2 (0--33.6) | <0.001 | |
| Inguinal Approach | 2,142 | 2,951 | 5,093 | |
| Participating Surgeons | 294 | 151 | 445 | |
| Median (Range) Annual Surgeon Volume |
1.2 (0--17.8) | 2 (0—27.3) | <0.001 | |
For test comparing mean patient age between specialties
3.3 Orchiopexy
Within the study period, 16,545 orchiopexies were performed and pediatric surgeons performed 17% of the cases (Figure 1). Surgeon volume was higher for pediatric urologists than general surgeons (p<0.001) (median 24 vs. 2.5 cases per year) (Table 3, Figure 2). Patients treated by pediatric urologists were older (p=<0.001) with mean age of 3.4 years compared to 2.9 years (Table 3). Patients treated by pediatric urologists were more likely to have commercial insurance (p=0.006) (Table 3).
Table 3.
Orchiopexy
| General Surgery (2,763 Cases 252 Surgeons) |
Urology (13,782 Cases 159 Surgeons) |
All Cases (16,545 Cases 411 Surgeons) |
P- Value |
|
|---|---|---|---|---|
| Age (Years) | <0.001a | |||
| N | 2,763 | 13,782 | 16,545 | |
| Mean (SD) | 2.9 (2.8) | 3.4 (2.9) | 3.3 (2.9) | |
| Median (Range) | 1.7 (0.0--10.0) | 2.2 (0.0--10.0) | 2.1 (0.0--10.0) | |
| Surgeon Volume | ||||
| All Orchiopexies | 2,763 | 13,782 | 16,545 | <0.001 |
| Participating Surgeons | 252 | 159 | 411 | |
| Median (Range) Annual Surgeon Volume |
2.5 (0.8--36.0) | 24.0 (0.7--81.2) | ||
| Open Inguinal Approach | 2,501 | 12,404 | 14,905 | <0.001 |
| Participating Surgeons | 244 | 159 | 403 | |
| Median (Range) Annual Surgeon Volume |
2.1 (0 --31.0 ) | 20.7 (0.7--70.0) | ||
| Open abdominal Approach | 78 | 704 | 782 | <0.001 |
| Participating Surgeons | 52 | 104 | 156 | |
| Median (Range) Annual Surgeon Volume |
0 (0--2.0) | 0.4 (0--13.0) | ||
| Laparoscopic Approach | 223 | 957 | 1,180 | <0.001 |
| Participating Surgeons | 92 | 112 | 204 | |
| Median (Range) Annual Surgeon Volume |
0 (0--5.0) | 1.0 (0--11.5) | ||
For test comparing mean patient age between specialties
4.0 DISCUSSION
Understanding practice patterns may yield important information regarding patient access to care. Hernia repair is common in the pediatric population. In 2013, Somme et al. published data on the frequency of pediatric inpatient surgical procedures using the 2009 Kids’ Inpatient Database (KID). Pediatric inguinal hernia was listed as the 9th most common pediatric procedure with a weighted estimated national frequency of 4,507, which is certainly a gross underestimate since the annual volume is almost identical to the 73 hospitals in our study.[11] Despite being a common procedure, hernia repair wait times have been found to be prolonged. In 2008, Zamakhashary et al. found that the median wait time for elective hernia repair in children less than 2 years of age was 35 days, and wait time of greater than 14 days was associated with doubling the risk of incarceration.[12] In 2014, Gawad et al. found in a single center study that the wait time from referral to surgeon to surgical repair was 79 days and patient prematurity and comoribities were associated with longer wait time.[13] These and other similar studies however often do not distinguish between surgical intervention by pediatric surgeons or urologists. The KID estimate is limited by only inclusion of inpatient data. Furthermore, the lack of provider specific data precluded identification of pediatric trained surgeons.[14] The FPSC database includes inpatient and outpatient encounters, yielding a much greater volume of data and allows the user to identify specialists and pediatric providers to show variation between individual providers and specialties.
While referral patterns may account for the variations in surgeon volume, exposure during training may also affect treatment patterns. Even though the inguinal dissection for hernia repair, hydrocele repair and orchiopexy are very similar, general surgery and urology residents have varying levels of exposure and comfort with these procedures. Gustafson and MacNeily evaluated case logs of 48 urology residents and found an average of 7 hernia repairs, 7 hydrocelectomies and 30 orchiopexies per year.[15] Survey of 41 senior urology residents revealed that approximately 75% felt technically competent with hernia repair, hydrocelectomy and orchiopexy of palpable testes.[16] In comparison, survey of 19 general surgery residents revealed that approximately 30% felt “somewhat competent” with orchiopexy, and 70% felt uncomfortable with orchiopexy. All felt “fully” or “somewhat” competent with inguinal hernia repairs in children and 75% felt competent with inguinal hernia repair in infants.[17] Trainee comfort with these procedures may impact post-training practice patterns.
Timing of hernia repair in preterm infants remains a topic of discussion given the need to weigh the benefits of preventing incarceration against the risks of anesthesia and technical challenges of the preterm canal.[18] Age at time of surgery was a significant factor differentiating patients treated by pediatric urologists and surgeons. In a recent survey of the members of the American Academy of Pediatrics, 63% of surgeons indicated that they would perform hernia repair in preterm patients prior to NICU discharge.[19] Infants with urological conditions such as hypospadias, undescended testes, vesicoureteral reflux and renal obstruction are almost always referred to urology after discharge from the NICU. On the other hand, pediatric surgeons are called to the NICU to urgently care for infants with imperforate anus, pyloric stenosis, diaphragmatic hernia, omphalocele and gastroschisis. The very strong presence of pediatric surgeons in the NICU, hence treatment of neonates, is likely a major factor explaining the much younger age of patients treated by pediatric surgeons.
As is for most large database studies, accuracy of the data is subject to coding error. The FPSC database is based on billing data for which CPT coding is done by professional abstractors at each academic institution that submits data. We are unable to determine whether other factors exist that limit access to pediatric specialists or affect referral patterns. Our median annual surgeon volume for pediatric surgeons performing primary hernia repair may also be lower compared to other studies, specifically a recent study of recertification case numbers.[20] One reason for this difference is that we analyzed practice and referral patterns, thus concurrent, bilateral procedures in one patient were counted as a single case. Another possible reason for the lower median volume may be that our study was limited to academic centers, whereas the recertification data includes approximately 50% private practice surgeons.
Although outcomes were not studied in this analysis, previous studies have demonstrated that surgeon volume correlates positively with patient outcomes. We previously showed for ureteral reimplantation that patients treated by low-volume surgeons (<13 cases per year) had longer length of stay, higher odds of ICU admission, longer ICU stays and higher rate of surgical complications than those treated by high-volume surgeons.[21] Higher surgeon volume was also associated with fewer complications in pyloromyotomies.[22] Understanding the practice patterns of inguinal and scrotal surgeries may facilitate future studies of volume-based outcomes.
5.0 CONCLUSIONS
This large multi-center analysis demonstrates that age is a key factor differentiating patient referral and care for children with inguinal or scrotal disorders. Pediatric surgeons operated on younger patients than pediatric urologists. Though hernia repairs, hydrocelectomies and orchiopexies are common procedures for both specialties, pediatric surgeons treat more boys and girls with inguinal hernias while pediatric urologists care for more boys with undescended testes and hydroceles. Knowledge of referral patterns and care between specialties with overlapping expertise will allow improvements in training and access.
Supplementary Material
Acknowledgments
David Troland, Manager-Physician Services Analytics, Vizient, Inc., provided assistance with data acquisition and management.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Chang SJ, Chen JY, Hsu CK, Chuang FC, Yang SS. The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia. 2015 doi: 10.1007/s10029-015-1450-x. [DOI] [PubMed] [Google Scholar]
- 2.Pan ML, Chang WP, Lee HC, Tsai HL, Liu CS, Liou DM, et al. A longitudinal cohort study of incidence rates of inguinal hernia repair in 0- to 6-year-old children. J Pediatr Surg. 2013;48:2327–2331. doi: 10.1016/j.jpedsurg.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Barthold JS, Gonzalez R. The epidemiology of congenital cryptorchidism, testicular ascent and orchiopexy. J Urol. 2003;170:2396–2401. doi: 10.1097/01.ju.0000095793.04232.d8. [DOI] [PubMed] [Google Scholar]
- 4.Manoharan S, Samarakkody U, Kulkarni M, Blakelock R, Brown S. Evidence-based change of practice in the management of unilateral inguinal hernia. J Pediatr Surg. 2005;40:1163–1166. doi: 10.1016/j.jpedsurg.2005.03.044. [DOI] [PubMed] [Google Scholar]
- 5.Chin TW, Pan ML, Lee HC, Tsai HL, Liu CS. Second hernia repairs in children-a nationwide study. J Pediatr Surg. 2015;50:2056–2059. doi: 10.1016/j.jpedsurg.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 6.Shalaby R, Ismail M, Gouda S, Yehya AA, Gamaan I, Ibrahim R, et al. Laparoscopic management of recurrent inguinal hernia in childhood. J Pediatr Surg. 2015;50:1903–1908. doi: 10.1016/j.jpedsurg.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Vizient-AAMC Faculty Practice Solutions Center Irving, TX: Vizient, Inc. 2016 [Google Scholar]
- 8.Mostaedi R, Ali MR, Pierce JL, Scherer LA, Galante JM. Bariatric surgery and the changing current scope of general surgery practice: implications for general surgery residency training. JAMA Surg. 2015;150:144–151. doi: 10.1001/jamasurg.2014.2242. [DOI] [PubMed] [Google Scholar]
- 9.Sturm RM, Durbin-Johnson B, Kurzrock EA. Congenital adrenal hyperplasia: current surgical management at academic medical centers in the United States. J Urol. 2015;193:1796–1801. doi: 10.1016/j.juro.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cooke DT, Wisner DH. Who performs complex noncardiac thoracic surgery in United States academic medical centers? Ann Thorac Surg. 2012;94:1060–1064. doi: 10.1016/j.athoracsur.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 11.Somme S, Bronsert M, Morrato E, Ziegler M. Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics. 2013;132:e1466–e1472. doi: 10.1542/peds.2013-1243. [DOI] [PubMed] [Google Scholar]
- 12.Zamakhshary M, To T, Guan J, Langer JC. Risk of incarceration of inguinal hernia among infants and young children awaiting elective surgery. CMAJ. 2008;179:1001–1005. doi: 10.1503/cmaj.070923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gawad N, Davies DA, Langer JC. Determinants of wait time for infant inguinal hernia repair in a Canadian children's hospital. J Pediatr Surg. 2014;49:766–769. doi: 10.1016/j.jpedsurg.2014.02.064. [DOI] [PubMed] [Google Scholar]
- 14.Barnhart DC, Oldham K, Meyers RL. Time to get on the bus: children's surgery and where we need to go. Pediatrics. 2013;132:e1659–e1660. doi: 10.1542/peds.2013-3154. [DOI] [PubMed] [Google Scholar]
- 15.Gustafson P, MacNeily A. Pediatric procedures in urology residency training: An analysis of the experience of Canadian urology residents. Can Urol Assoc J. 2014;8:317–320. doi: 10.5489/cuaj.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mickelson JJ, Macneily AE, Samarasekera D, Beiko D, Afshar K. Competence in pediatric urology upon graduation from residency: perceptions of residents, program directors and pediatric urologists. Can Urol Assoc J. 2008;2:205–210. doi: 10.5489/cuaj.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poenaru D, Fitzgerald P Education Committee of the Canadian Association of Paediatric S. Training general surgery residents in pediatric surgery: A Canadian survey. J Pediatr Surg. 2001;36:706–710. doi: 10.1053/jpsu.2001.22941. [DOI] [PubMed] [Google Scholar]
- 18.Lee SL, Gleason JM, Sydorak RM. A critical review of premature infants with inguinal hernias: optimal timing of repair, incarceration risk, and postoperative apnea. J Pediatr Surg. 2011;46:217–220. doi: 10.1016/j.jpedsurg.2010.09.094. [DOI] [PubMed] [Google Scholar]
- 19.Antonoff MB, Kreykes NS, Saltzman DA, Acton RD. American Academy of Pediatrics Section on Surgery hernia survey revisited. J Pediatr Surg. 2005;40:1009–1014. doi: 10.1016/j.jpedsurg.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 20.Abdullah F, Salazar JH, Gause CD, Gadepalli S, Biester TW, Azarow KS, et al. Understanding the Operative Experience of the Practicing Pediatric Surgeon: Implications for Training and Maintaining Competency. JAMA Surg. 2016 doi: 10.1001/jamasurg.2016.0261. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen HG, Chamie K, Nguyen KG, Durbin-Johnson B, Kurzrock EA. Outcomes after pediatric ureteral reimplantation: a population based analysis. J Urol. 2011;185:2292–2297. doi: 10.1016/j.juro.2011.02.055. [DOI] [PubMed] [Google Scholar]
- 22.Ly DP, Liao JG, Burd RS. Effect of surgeon and hospital characteristics on outcome after pyloromyotomy. Arch Surg. 2005;140:1191–1197. doi: 10.1001/archsurg.140.12.1191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.