Abstract
Purpose
Cytochrome P450 1A1 (CYP1A1) polymorphisms were implicated in endometriosis risk, but individual published studies showed inconclusive results. Thus, a meta-analysis was performed to clarify the effect of CYP1A1 polymorphisms on endometriosis risk.
Methods
PubMed, Embase, and CNKI databases were searched to identify the eligible studies focusing on the associations between CYP1A1 MspI and Ile462Val polymorphisms and susceptibility to endometriosis. Summary odds ratios (ORs) and 95 % confidence intervals (95 % CIs) for CYP1A1 polymorphisms and endometriosis were calculated.
Results
Pooled analysis of 12 studies involved a total of 1555 cases and 2868 controls showed that in all genetic models, no significant association between CYP1A1 MspI polymorphism and endometriosis risk was observed in the overall, Asians and Caucasians population, respectively. Interestingly, increased endometriosis risk was associated with carrying the C allele of CYP1A1 combined with GSTM1 null genotypes. For CYP1A1 Ile462Val polymorphism, eight studies were available (878 cases and 1991 controls). In the overall analysis, CYP1A1 Ile462Val polymorphism had a statistically significant association with increased endometriosis risk in allele contrast and all genetic models except the model of Val/Ile vs. Ile/Ile. In the subgroup analysis by ethnicity, significant elevated endometriosis risk was associated with CYP1A1 Ile462Val polymorphism in Asians but not in Caucasians under all genetic models. No publication bias was found in the present studies.
Conclusions
This meta-analysis suggested that CYP1A1 Ile462Val polymorphism was associated with an increased risk of endometriosis, particularly in Asians. CYP1A1 MspI polymorphism may not be associated with endometriosis risk, but GSTM1 and CYP1A1 MspI polymorphism may have a joint effect on endometriosis risk.
Keywords: Endometriosis, Cytochrome P450 1A1, Polymorphism, Meta-analysis
Introduction
Endometriosis is one of the most common gynecological disorders in women that is defined as the presence of endometrial glands and stroma outside the uterine cavity. It is associated with a spectrum of symptoms of which chronic pelvic pain and infertility are the most common [1]. The disease affects 5 to 15 % of women in reproductive age, while the prevalence in infertile women is 30 to 50 % [2]. Although endometriosis has been intensively studied, the exact cause of the disorder is still unclear. Endometriosis is considered as a multifactor disease affected by hormonal, immunological, environmental, and genetic factors. Numerous studies have shown that the genetic factors were importantly involved in the susceptibility to endometriosis [3].
Cytochrome P450 1A1 (CYP1A1) enzyme is a member of the CYP superfamily and prone to mutation [4]. Multiple polymorphic sites within the CYP1A1 gene have been reported, while MspI (rs4646903 T>C) and Ile462Val (rs1048943 A>G) are the two most common polymorphisms. Several studies have investigated the relationships between CYP1A1 MspI and Ile462Val polymorphisms and endometriosis risk [5–8] However, the results were inconclusive. Hence, to acquire a more precise estimation of these associations, a meta-analysis of all eligible case–control studies was needed. A previous meta-analysis (based on only 480 cases and 475 controls from three studies in 2001, 2002, 2003, respectively) investigating the relationship of CYP1A1 MspI polymorphism and endometriosis was conducted in 2006 [9]. It was suggested that women with CYP1A1 MspI +/− and +/+ genotype have about 40 % of increased risk of endometriosis as compared with women of MspI −/− genotype, but the relationship of CYP1A1 Ile462Val polymorphism and endometriosis was not mentioned. In the past 10 years, several more replication studies which were performed to reevaluate the effect of CYP1A1 MspI polymorphisms on endometriosis offered some new data and diverse conclusions. In order to perform a more comprehensive estimation of the associations between CYP1A1 gene polymorphisms and endometriosis susceptibility, we conducted the meta-analysis to assess the associations between CYP1A1 MspI and Ile462Val polymorphisms and the risk of endometriosis.
Materials and methods
Literature search
All eligible studies were identified by searching the PubMed, Embase, and China National Knowledge Infrastructure (CNKI) (last update Jan 10, 2016) using the terms as follows: (‘polymorphism’ or ‘mutation’ or ‘variant’ or ‘variation’ or ‘genotype’ or ‘genetic’) and (‘CYP1A1’ or ‘cytochrome P450 1A1’) and (endometriosis). No language restriction was applied. Manual search of reference lists from potentially relevant articles was also performed to identify other potential studies.
Inclusion and exclusion criteria
The following criteria were used to select the eligible studies: (1) the studies evaluated the associations between CYP1A1 MspI and Ile462Val polymorphisms and the risk of endometriosis, (2) case-control studies, (3) the studies provided sufficient data to estimate an odds ratio (OR) and 95 % confidence interval (95 % CI). Only published studies with full text articles were included. If more than one article from the same group occurred, we only included the most recent or complete article to avoid overlapping.
The following exclusion criteria were applied for excluding studies: (1) no control population; (2) studies contained duplicate data; (3) no available genotype or allele frequency; (4) publication only as an abstract or as conference proceedings, (5) case reports or reviews; (6) unpublished study.
Data extraction
The following information were extracted: the first author, year of publication, ethnicity, country, number of subjects, diagnostic criteria of cases, genotyping methods, the minor allele frequency and genotypes, sites of mutation and Hardy-Weinberg equilibrium (HWE) in controls. Data were extracted independently by two investigators and discrepancies were resolved by consensus including a third author.
Statistical analysis
The STATA version 10.0 (Stata Corp, College Station, TX) software was used for meta-analysis. The HWE of genotypes in the control group was assessed by using a χ 2 test. The possible associations between CYP1A1 MspI and Ile462Val polymorphisms and endometriosis risk were evaluated by ORs and 95 % CI under allele contrast (MspI: C vs. T; Ile462Val: Val vs. Ile), homozygote (MspI:CC vs. TT; Ile462Val: Val/Val vs. Ile/Ile), heterozygote (MspI: CT vs. TT; Ile462Val: Val/Ile vs. Ile/Ile), recessive (MspI: CC vs. CT + TT; Ile462Val: Val/Val vs. Val/Ile + Ile/Ile), and dominant (MspI: CC + CT vs. TT; Ile462Val: Val/Val + Val/Ile vs. Ile/Ile) models. Studies providing the combined genotypes (CC + CT; Val/Val + Val/Ile) rather than the separate ones were only included in the dominant model evaluation.
The Q-statistic and I 2 test were used to evaluate potential heterogeneity between studies. I 2 < 25 % represents no heterogeneity, I 2 = 25–50 % represents moderate heterogeneity, I 2 = 50–75 % represents large heterogeneity, and I 2 > 75 % represents extreme heterogeneity [10]. If the result of the Q test was P < 0.10, suggesting the existence of between-study heterogeneity, ORs were pooled by random-effects model (DerSimonian and Laird method). Otherwise, the fixed-effects model (the Mantel-Haenszel method) was used. Subgroup analyses were utilized to explore the potential sources of heterogeneity across studies. Potential publication bias was estimated by the Begg rank correlation test and Egger weighted regression test. P < 0.05 was considered to represent statistically significant publication bias.
Results
Literature search and study selection
According to the search criteria, a total of 70 articles relevant to the searched keywords were initially identified, of which 48 irrelevant papers were excluded after reading the title and abstract. After the full-text evaluation, five articles were excluded with reasons for no available data (n = 1) [11], irrelevance to endometriosis (n = 1) [12], duplicate publications (n = 3) [13–15]. An article providing data for two different subgroups (Caucasian and Asian) was counted as two separate studies [6]. Finally, 18 studies (12 articles in English [5, 7, 16–25] and others in Chinese [6, 8, 26–28]) were included in this meta-analysis. For the CYP1A1 MspI polymorphism, 12 studies involved a total of 1555 cases and 2868 controls. For the CYP1A1 Ile462Val polymorphism, eight studies were available, including a total of 878 cases and 1991 controls. There were four articles (including five studies) about the association between combinations of CYP1A1 MspI polymorphism and the glutathione S-transferases M1 (GSTM1) null mutation and the risk of endometriosis [5, 6, 22, 24].
Study characteristics were summarized in Tables 1 and 2 (Table 1 for MspI, Table 2 for Ile462Val). Among these publications about the CYP1A1 MspI polymorphism, seven studies involved Asian subjects, four studies involved Caucasian subjects, and one study involved unknown subjects (Table 1). A total of eight separate comparisons (five Asian and three Caucasian) were considered for CYP1A1 Ile462Val polymorphism (Table 2). Four genotype methods were used among these studies, including DNA sequencing, TaqMan, polymerase chain reaction–restriction fragment length polymorphism (PCR–RFLP), and allele-specific PCR (AS-PCR). Only three studies were confirmed as endometriosis by surgery [7, 18, 22], and other studies were confirmed as endometriosis by histological study.
Table 1.
Characteristics of studies about MspI included in the present meta-analysis
| Study | Year | Ethnicity (country) | Numbers | Diagnosis method | Genotype method | Minor allele frequency | Cases | Controls | P value (HWE test) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Control | Case | Control | TT | TC | CC | TT | TC | CC | ||||||
| Wu CH et al. | 2012 | Asian (China) | 121 | 171 | Laparoscopy and histological examination | TaqMan | Cannot calculate | TT | TC + CC | TT | TC + CC | Cannot calculate | |||
| 60 | 61 | 84 | 87 | ||||||||||||
| Trabert B et al. | 2011 | Caucasian (USA) | 255 | 567 | Surgical examination | PCR-RFLP | 0.118 | 0.138 | 202 | 46 | 7 | 423 | 132 | 12 | 0.65 |
| Rozati R et al. | 2008 | Asian (India) | 97 | 102 | Laparoscopy examination | PCR-RFLP | 0.232 | 0.230 | 56 | 37 | 4 | 61 | 35 | 6 | 0.74 |
| Juo SH et al. | 2006 | Asian (China) | 104 | 299 | Laparoscopy and histological examination | PCR-RFLP | 0.346 | 0.401 | 42 | 52 | 10 | 107 | 144 | 48 | 0.97 |
| Huber A et al. | 2005 | Caucasian (Austria) | 32 | 790 | Surgical and histological examination | PCR-sequencing | Cannot calculate | TT | TC + CC | TT | TC + CC | Cannot calculate | |||
| 28 | 4 | 650 | 140 | ||||||||||||
| Babu KA et al. | 2005 | Asian (India) | 310 | 215 | Laparoscopy examination | PCR-RFLP | 0.311 | 0.356 | 145 | 137 | 28 | 93 | 91 | 31 | 0.26 |
| Arvanitis DA et al. | 2003 | Caucasian (Greece) | 275 | 346 | Surgical or laparoscopy, histological examination | PCR-RFLP | 0.202 | 0.143 | 173 | 93 | 9 | 253 | 87 | 6 | 0.64 |
| Iizuka S et al. | 2003 | Asian (Japan) | 35 | 37 | Histological examination | PCR-RFLP | 0.371 | 0.405 | 17 | 10 | 8 | 15 | 14 | 8 | 0.19 |
| Hadfield RM et al. | 2001 | Unknown (UK) | 129 | 49 | Surgical and histological examination | PCR-RFLP | Cannot calculate | TT | TC + CC | TT | TC + CC | Cannot calculate | |||
| 102 | 27 | 37 | 12 | ||||||||||||
| Chen ZF et al. | 2005 | Caucasian (China) | 41 | 107 | Surgical or laparoscopy, histological examination | PCR-RFLP | Caucasian | Caucasian | Caucasian 0.79 | ||||||
| 0.378 | 0.299 | 16 | 19 | 6 | 52 | 46 | 9 | Asian 0.77 | |||||||
| Asian (China) | 80 | 105 | Asian | ||||||||||||
| 34 | 41 | 5 | 44 | 49 | 12 | ||||||||||
| Asian | |||||||||||||||
| 0.319 | 0.348 | ||||||||||||||
| Peng DX et al. | 2002 | Asian (China) | 76 | 80 | Surgical or laparoscopy, histological examination | PCR-RFLP | 0.447 | 0.35 | 23 | 38 | 15 | 34 | 36 | 10 | 0.92 |
Table 2.
Characteristics of studies about Ile/Val included in the present meta-analysis
| Study | Year | Ethnicity (country) | Numbers | Diagnosis method | Genotype method | Minor allele frequency | Cases | Controls | P value (HWE test) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Control | Case | Control | Ile/Ile | Ile/Val | Val/Val | Ile/Ile | Ile/Val | Val/Val | ||||||||
| Matsuzaka Y et al. | 2012 | Asian (Japan) | 95 | 137 | Laparoscopy and histological examination | PCR-sequencing | 0.242 | 0.223 | Ile | Val | Ile | Val | Cannot calculate | ||||
| 144 | 46 | 213 | 61 | ||||||||||||||
| Trabert B et al. | 2011 | Caucasian (USA) | 255 | 567 | Surgical examination | PCR-RFLP | 0.053 | 0.053 | 231 | 21 | 3 | 510 | 54 | 3 | Ile/Val 0.24 | ||
| Tsuchiya M et al. | 2007 | Asian (Japan) | 79 | 59 | Laparoscopy and histological examination | PCR-RFLP | Cannot calculate | Ile/Ilel | Ile/Val + Val/Va | Ile/Ile | Ile/Val + Val/Val | Cannot calculate | |||||
| 50 | 29 | 40 | 19 | ||||||||||||||
| Huber A et al. | 2005 | Caucasian (Austria) | 32 | 790 | Surgical and histological examination | PCR-sequencing | Cannot calculate | Ile/Ile | Ile/Val + Val/Val | Ile/Ile | Ile/Val + Val/Val | Cannot calculate | |||||
| 32 | 0 | 735 | 52 | ||||||||||||||
| Ivashchenko TE et al. | 2003 | Caucasian (Russia) | 74 | 40 | Laparoscopy and histological examination | PCR-RFLP | 0.034 | 0.05 | 69 | 5 | 0 | 36 | 4 | 0 | 0.74 | ||
| An XF et al. | 2011 | Asian (China) | 216 | 216 | Surgical and histological examination | AS-PCR | 0.407 | 0.282 | 72 | 112 | 32 | 110 | 90 | 16 | 0.68 | ||
| Cao YH et al. | 2008 | Asian (China) | 51 | 102 | Surgical or laparoscopy, histological examination | AS-PCR | 0.431 | 0.255 | 16 | 26 | 9 | 58 | 36 | 8 | 0.47 | ||
| Peng DX et lal. | 2003 | Asian (China) | 76 | 80 | Surgical or laparoscopy, histological examination | AS-PCR | 0.395 | 0.25 | 29 | 34 | 13 | 46 | 28 | 6 | 0.55 | ||
CYP1A1 MspI polymorphism and endometriosis risk
For CYP1A1 MspI polymorphism, no significant difference in risk was seen between endometriosis and controls in the overall meta-analysis (C vs. T: OR = 1.02, 95 % CI 0.84–1.24, I 2 = 56.1 %, P heterogeneity = 0.02; CC vs. TT: OR = 0.98, 95 % CI 0.64–1.49, I 2 = 41.5 %, P heterogeneity = 0.09; CT vs. TT: OR = 1.06, 95 % CI 0.90–1.25, I 2 = 31.2 %, P heterogeneity = 0.17; dominant model: OR = 1.02, 95 % CI 0.88–1.17, I 2 = 29.8 %, P heterogeneity = 0.15; and recessive model: OR = 0.87, 95 % CI 0.65–1.16, I 2 = 31.6 %, P heterogeneity = 0.17). Stratification analysis by ethnicity also showed neither significant association between the CYP1A1 MspI polymorphism and endometriosis in the population of Asian nor in that of Caucasian origin under allele contrast and all genetic models (Table 3). In the subgroup analysis by HWE in controls, no obvious association was found yet (data not shown).
Table 3.
Analyses of the association between CYP1A1 MspI polymorphism with endometriosis
| Comparisons | No. of studies | Subgroup | OR (95 % CI) | Test of heterogeneity | Publication bias | ||
|---|---|---|---|---|---|---|---|
| P value | I 2 (%) | Begg’s test | Egger’s test | ||||
| C vs. T | 9 | All | 1.02 (0.84, 1.24) | 0.02 | 56.1 | 0.35 | 0.56 |
| Ethnicity | |||||||
| 6 | Asian | 0.90 (0.77, 1.06) | 0.28 | 19.8 | |||
| 3 | Caucasian | 1.20 (0.79, 1.82) | 0.02 | 74.0 | |||
| CC vs. TT | 9 | All | 0.98 (0.64, 1.49) | 0.09 | 41.5 | 0.60 | 0.16 |
| Ethnicity | |||||||
| 6 | Asian | 0.72 (0.51, 1.02) | 0.24 | 26.4 | |||
| 3 | Caucasian | 1.72 (0.95, 3.13) | 0.65 | 0 | |||
| CT vs. TT | 9 | All | 1.06 (0.90, 1.25) | 0.17 | 31.2 | 1.00 | 0.99 |
| Ethnicity | |||||||
| 6 | Asian | 1.03 (0.82, 1.28) | 0.75 | 0 | |||
| 3 | Caucasian | 1.13 (0.65, 1.97) | 0.01 | 77.0 | |||
| Dominant model | 12 | All | 1.02 (0.88, 1.74) | 0.15 | 29.8 | 0.95 | 0.80 |
| Ethnicity | |||||||
| 7 | Asian | 0.96 (0.79, 1.16) | 0.65 | 0 | |||
| 4 | Caucasian | 1.10 (0.68, 1.78) | 0.02 | 69.9 | |||
| 1 | unknown | ||||||
| Recessive model | 9 | All | 0.87 (0.65, 1.16) | 0.17 | 31.6 | 0.75 | 0.14 |
| Ethnicity | |||||||
| 6 | Asian | 0.72 (0.52, 1.00) | 0.33 | 12.6 | |||
| 3 | Caucasian | 1.13 (0.66, 1.93) | 0.23 | 32.9 | |||
CYP1A1 Ile462Val polymorphism and endometriosis risk
In the overall population, meta-analysis revealed significant association between the CYP1A1 Ile462Val polymorphism and endometriosis in allele contrast and all genetic models except the model of Val/Ile vs. Ile/Ile (Table 4). In the subgroup analysis by ethnicity, significant association between the CYP1A1 Ile462Val polymorphism and endometriosis was found in the population of Asian origin under allele contrast and all genetic models (Table 4). We did not observe significant association between the Ile462Val polymorphism and endometriosis in Caucasian population (Table 3). For the studies within HWE in controls, there was still significant association between the Ile462Val polymorphism and endometriosis susceptibility (data not shown).
Table 4.
Analyses of the association between CYP1A1 Ile462Val polymorphism with endometriosis
| Comparisons | No. of studies | Subgroup | OR (95 % CI) | Test of heterogeneity | Publication bias | ||
|---|---|---|---|---|---|---|---|
| P value | I 2 (%) | Begg’s test | Egger’s test | ||||
| Val vs. Ile | 6 | All | 1.48 (1.12, 1.97) | 0.06 | 52.8 | 1.00 | 0.43 |
| Ethnicity | |||||||
| 4 | Asian | 1.68 (1.38, 2.05) | 0.17 | 39.9 | |||
| 2 | Caucasian | 0.96 (0.62, 1.49) | 0.57 | 0 | |||
| Val/Val vs. Ile/Ile | 4 | All | 3.20 (1.98, 5.19) | 0.94 | 0 | 1.00 | 0.87 |
| Ethnicity | |||||||
| 3 | Asian | 3.32 (2.00, 5.50) | 0.91 | 0 | |||
| 1 | Caucasian | 2.21 (0.44, 11.02) | |||||
| Val/Ile vs. Ile/Ile | 5 | All | 1.52 (0.97, 2.39) | 0.05 | 58.3 | 1.00 | 0.73 |
| Ethnicity | |||||||
| 3 | Asian | 2.02 (1.47, 2.77) | 0.75 | 0 | |||
| 2 | Caucasian | 0.83 (0.51, 1.36) | 0.71 | 0 | |||
| Dominant model | 7 | All | 1.52 (1.01, 2.30) | 0.03 | 57.0 | 0.37 | 0.31 |
| Ethnicity | |||||||
| 4 | Asian | 2.04 (1.54, 2.68) | 0.40 | 0 | |||
| 3 | Caucasian | 0.83 (0.52, 1.31) | 0.55 | 0 | |||
| Recessive model | 4 | All | 2.31 (1.46, 3.65) | 0.99 | 0 | 0.73 | 0.47 |
| Ethnicity | |||||||
| 3 | Asian | 2.32 (1.44, 3.74) | 0.95 | 0 | |||
| 1 | Caucasian | 2.24 (0.45,11.17) | |||||
Association of genotypes of CYP1A1-GSTM1 with endometriosis risk
Taking the genotype of TT for CYP1A1 MspI and GSTM1 present as the reference, genotypes of TC or TC + CC for CYP1A1 and GSTM1 null deletion were significantly associated with endometriosis risk (TC/GSTM− vs. TT/GSTM+: OR = 1.44, 95 % CI 1.06–1.96, I 2 = 36.1 %, P heterogeneity = 0.18; TC + CC/GSTM− vs. TT/GSTM+: OR = 1.45, 95 % CI 1.08–1.94, I 2 = 38.1 %, P heterogeneity = 0.17) (Table 5). Hadfield et al. also reported a similar finding [25] to ours, which was not included in our meta-analysis because of lack of data about the interaction of CYP1A1 MspI polymorphism and GSTM1 null mutation on the endometriosis risk.
Table 5.
Analyses of the association between combinations of CYP1A1 MspI polymorphism and the GSTM1 null mutation and the risk of endometriosis
| Comparisons | No. of studies | OR (95 % CI) | Test of heterogeneity | |
|---|---|---|---|---|
| P value | I 2 (%) | |||
| TT GSTM− vs. TT GSTM+ | 5 | 1.02 (0.77, 1.35) | 0.13 | 44.6 |
| TC GSTM− vs. TT GSTM+ | 5 | 1.44 (1.06, 1.96) | 0.18 | 36.1 |
| CC GSTM− vs. TT GSTM+ | 5 | 1.35 (0.75, 2.43) | 0.53 | 0 |
| CC + TC GSTM− vs. TT GSTM+ | 5 | 1.45 (1.08, 1.94) | 0.17 | 38.1 |
Gene–gene interaction cannot be assessed for combinations of CYP1A1 Ile462Val polymorphism and GSTM1 null mutation on the risk of endometriosis in the pooled analysis because there was only one study about the interaction [27], in which taking the subjects with the genotype of Ile/Ile for CYP1A1 and GSTM1 present as the reference, the OR was 4.40 (95 % CI, 1.55–12.45) for subjects with genotype of Ile/Val for CYP1A1 and GSTM1 null, and 9.90 (95 % CI, 1.80–54.45) for subjects with genotype of Val/Val for CYP1A1 and GSTM1 null.
Heterogeneity analysis
For the CYP1A1 MspI polymorphism, there was moderate or large heterogeneity among studies in overall comparisons. To explore sources of heterogeneity across studies, subgroup analyses by ethnicity (Asian or Caucasian) and Hardy-Weinberg equilibrium (HWE) in controls (yes or not) were conducted. There was no heterogeneity in the studies of Asian in most comparisons; however, there was still large heterogeneity in the studies of Caucasian in most comparisons (Table 3). HWE in controls could not explain the heterogeneity (data not shown).
For the CYP1A1 Ile462Val polymorphism, there was large heterogeneity among studies in most comparisons. To explore sources of heterogeneity across studies, subgroup analyses by ethnicity (Asian or Caucasian) and HWE in controls (yes or not) were conducted. There was no heterogeneity in the studies of Asian or Caucasian in most comparisons (Table 4). HWE in controls still could not explain the heterogeneity (data not shown).
There were two studies about the relationship between the CYP1A1 MspI polymorphism and endometriosis risk in Indians, and no study on the relationship between CYP1A1 Ile462Val polymorphism and endometriosis risk in Indians. It was really one problem that Indians are counted as Asians or Caucasians in stratified analysis. In stratified analysis, there was no difference between the results no matter Indians were counted as Asians or not. Thus, we only showed the results of stratified analysis in which Indians are counted as Asians, while the results of stratified analysis in which Indians are counted as Caucasians are not showed in the article.
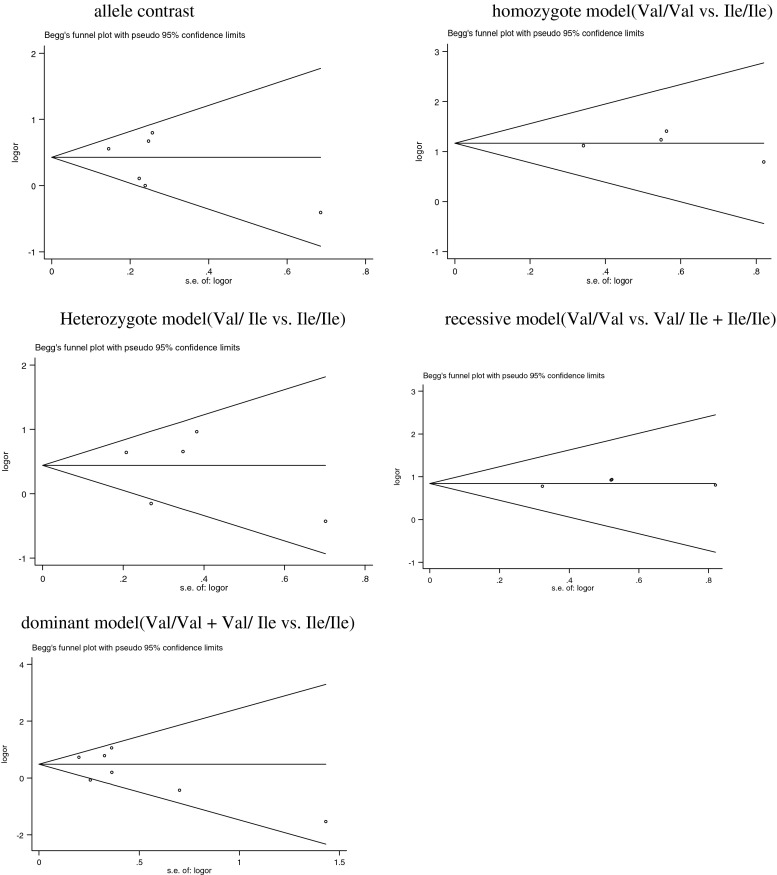
Publication bias
Begg’s funnel plot and Egger’s test were performed to assess possible publication bias (Tables 2, 3, and 4; Figs. 1 and 2), which showed no publication bias for studies published on the CYP1A1 MspI and Ile462Val polymorphisms.
Fig. 1.
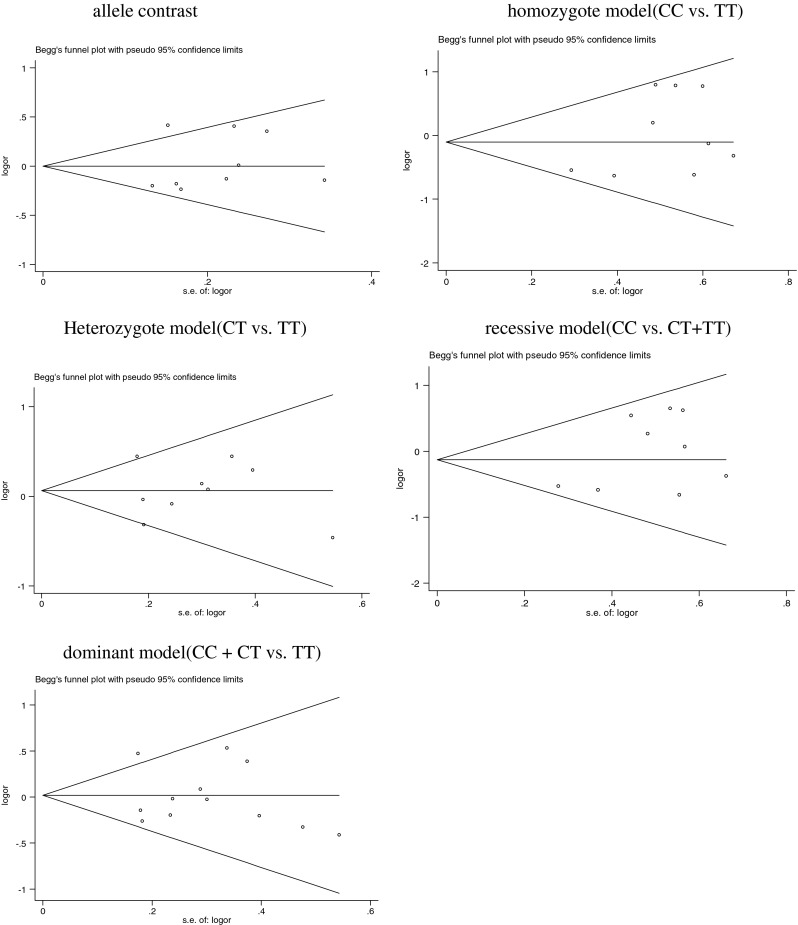
Begg’s funnel plot of publication bias test on the relationship between CYP1A1 MspI polymorphism and endometriosis risk. Each point represents a separate study for the indicated association
Fig. 2.
Begg’s funnel plot of publication bias test on the relationship between CYP1A1 Ile462Val polymorphism and endometriosis risk. Each point represents a separate study for the indicated association
Discussion
Environmental toxins, including dioxin, have been implicated as risk factors of endometriosis [29]. It was stated that phase I drug-metabolizing enzymes (DMEs) metabolized toxic compounds to genotoxic electrophilic intermediates, and phase II DMEs conjugate the intermediates to water-soluble derivatives, completing the detoxification cycle [30]. Cytochrome P450s are the most important phase I enzymes. The products of CYP1A1 are involved in estrogen and PAH metabolism. It was shown that CYP1A1 was involved in metabolism of dioxin, which may increase the incidence and severity of endometriosis in monkeys [29]. Moreover, CYP1A1 is also involved in estrogen metabolism, catalyzing the hydroxylation of 17β-estradiol at the C-2 position [31]. Considering that estrogenic components play key roles in endometriosis [32], CYP1A1 may be associated with endometriosis. The CYP1A1 MspI polymorphism can alter the level of gene expression or mRNA stability, resulting in a highly inducible activity of the enzyme [33]. For the Ile462Val polymorphism, it was found that mean mRNA (induced/basal) levels of CYP1A1 increased with number of Val variants [34]. Heterozygotes for both 3801C and Val variants had twofold increased basal CYP1A1 expression compared with homozygotes for the 3801T and Ile alleles [35]. Hence, certain variant genotypes of the CYP1A1 gene which may cause enhanced enzymatic activity appear to play a role in susceptibility to endometriosis in theory. To date, several studies reported the role of CYP1A1 polymorphisms in endometriosis. However, the results were inconclusive. Therefore, we performed a meta-analysis to acquire a more precise estimation of these associations.
In the meta-analysis, we investigated the associations between CYP1A1 MspI and Ile462Val polymorphisms and endometriosis risk. To the best of our knowledge, this is the first meta-analysis of the assessment for the relationships between both the two CYP1A1 gene polymorphisms and the risk of endometriosis (the previous meta-analysis (2006) assessed the association between only CYP1A1 MspI polymorphism and endometriosis risk). Meta-analysis of the CYP1A1 MspI polymorphism showed no association with endometriosis in all genetic models and allele contrast in the overall, Asians and Caucasians population, respectively. Interestingly, when gene–gene interaction was taken into account, increased endometriosis risk was associated with carrying the C allele of CYP1A1 combined with GSTM1 null genotypes. It was speculated that GSTM1 and CYP1A1 MspI polymorphism may have a joint effect on endometriosis risk.
Meta-analysis of the CYP1A1 Ile462Val polymorphism showed a significantly increased risk of endometriosis in the overall population. In the stratified analysis by ethnicity, the significant association of Ile462Val polymorphism and endometriosis was observed in Asians but not in Caucasians. However, there were only small number of studies on Caucasians for this polymorphism, and it was suggested that Val variant occurred more frequently in Asian than in Caucasians [36]. Therefore, it was possible that the observed ethnic difference in the association of Ile462Val polymorphism and endometriosis might be the result of small samples. More studies with the Caucasians population are needed to validate the effect of the CYP1A1 Ile462Val polymorphism on endometriosis risk in Caucasians.
Heterogeneity is one of the important issues, which may affect the interpretation of the results. In our meta-analysis, between-study heterogeneity was significant in most comparisons. It was suggested that genetic associations for complex diseases may be spurious if the distribution of genotypes in the healthy control groups in genetic case-control studies deviates from HWE [37]. So it was important to utilize the sub-group analysis by HWE in controls to explore the potential genetic associations for complex diseases. However, HWE in controls was unable to identify the sources of heterogeneity. For CYP1A1 MspI polymorphism, in the subgroup analyses by ethnicity, although there was still large heterogeneity in the studies of Caucasian in most comparisons, there was no heterogeneity in the studies of Asian in most comparisons. For CYP1A1 Ile462Val polymorphism, in the subgroup analyses by ethnicity, there was no heterogeneity in the studies of Asian or Caucasian in most comparisons. Therefore, it was possible that the ethnic difference might partly be the source of heterogeneity. Furthermore, endometriosis was a complex disease. Both environmental and genetic factors could affect the endometriosis risk in different populations. Wherefore, contributors to heterogeneity in this meta-analysis may also be related to the gene–environment interactions.
Some limitations of our study should be considered. Firstly, the included studies were carried out mainly in Asians and Caucasians. Further studies in other ethnic groups are needed to confirm the results of this meta-analysis. Secondly, the meta-analysis was based primarily on unadjusted ORs as the result of the lack of available information, and confounding factors might influence the precision of effect estimates. Thirdly, endometriosis is a complex disorder influenced by both genetic and environmental factors. CYP1A1 polymorphisms may be only one risk of endometriosis, and there are many other genetic and environmental factors that participate in the development of endometriosis [38–40]. Gene–gene interaction may influence the results of endometriosis risk. It was suggested that increased risk of developing endometriosis was not found in women with GSTM1 null genotype when compared with women with other genotypes in a meta-analysis of the association between GSTM1 polymorphism and endometriosis risk [41]. In our meta-analysis, CYP1A1 MspI polymorphism may not be associated with endometriosis risk, but GSTM1 null genotypes combined with the C allele of CYP1A1 were associated with increased risk for endometriosis. Thus, there is synergy between GSTM1 and CYP1A1 MspI polymorphism on endometriosis risk. So more studies were needed to confirm whether other gene polymorphisms combined with CYP1A1 polymorphisms were associated with the endometriosis risk or not. Gene–environment interactions were not addressed in this meta-analysis, since no related data were provided in the included studies. Fourthly, although Begg’s test and Egger’s test did not show any conspicuous publication bias, selection bias may have occurred because we only included published articles in this meta-analysis. Finally, some significant heterogeneity across studies was detected in the meta-analysis. Nevertheless, this may not be a principal issue because our results showed that the related summarized ORs were not substantially altered after subgroup analyses by ethnicity which may be the main source of heterogeneity, especially in Asians, and this indicated obvious statistical robustness of our results.
In conclusion, this study suggested that CYP1A1 Ile462Val polymorphism was associated with an increased risk of endometriosis, particularly in Asians. CYP1A1 MspI polymorphism may not be associated with endometriosis risk; however, genotypes combined of the C allele of CYP1A1 and GSTM1 null were associated with increased risk for endometriosis. Considering the small number of studies included, more studies are needed to validate these findings, especially in different populations.
Footnotes
Capsule This meta-analysis suggested that CYP1A1 Ile462Val polymorphism was associated with an increased risk of endometriosis, particularly in Asians.
References
- 1.Bulun SE. Endometriosis. N Engl J Med. 2009;360:268–279. doi: 10.1056/NEJMra0804690. [DOI] [PubMed] [Google Scholar]
- 2.Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364:1789–1799. doi: 10.1016/S0140-6736(04)17403-5. [DOI] [PubMed] [Google Scholar]
- 3.Dun EC, Taylor RN, Wieser F. Advances in the genetics of endometriosis. Genome Med. 2010;2:75. doi: 10.1186/gm196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agundez JA. Cytochrome P450 gene polymorphism and cancer. Curr Drug Metab. 2004;5:211–224. doi: 10.2174/1389200043335621. [DOI] [PubMed] [Google Scholar]
- 5.Arvanitis DA, Koumantakis GE, Goumenou AG, Matalliotakis IM, Koumantakis EE, Spandidos DA. CYP1A1, CYP19, and GSTM1 polymorphisms increase the risk of endometriosis. Fertil Steril. 2003;79:702–709. doi: 10.1016/S0015-0282(02)04817-3. [DOI] [PubMed] [Google Scholar]
- 6.Chen ZF, Ding Y, Lin RY, Wang XF, Ding JB. Relationship between endometriosis and MspI polymorphisms of cytochrome P4501A1(CYP1A1) gene or CYP1A1 MspI GSTM1 null genotypes combined. Prog Obstet Gynecol. 2005;14:285–288. [Google Scholar]
- 7.Trabert B, Schwartz SM, Peters U, De Roos AJ, Chen C, Scholes D, et al. Genetic variation in the sex hormone metabolic pathway and endometriosis risk: an evaluation of candidate genes. Fertil Steril. 2011;96:1401–1406. doi: 10.1016/j.fertnstert.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An XF, Yang LP, Liu SJ. Study on the relationship between polymorphisms of CYP1A1 gene Exon7 and susceptibility of endometriosis in women of Han Nationality in Jilin City. Matern Child Health Care China. 2011;26:2174–2176. [Google Scholar]
- 9.Guo SW. The association of endometriosis risk and genetic polymorphisms involving dioxin detoxification enzymes: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2006;124:134–143. doi: 10.1016/j.ejogrb.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Ioannidis JP, Boffetta P, Little J, O’Brien TR, Uitterlinden AG, Vineis P, et al. Assessment of cumulative evidence on genetic associations: interim guidelines. Int J Epidemiol. 2008;37:120–132. doi: 10.1093/ije/dym159. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe T, Imoto I, Kosugi Y, Fukuda Y, Mimura J, Fujii Y, et al. Human arylhydrocarbon receptor repressor (AHRR) gene: genomic structure and analysis of polymorphism in endometriosis. J Hum Genet. 2001;46:342–346. doi: 10.1007/s100380170070. [DOI] [PubMed] [Google Scholar]
- 12.Parveen F, Faridi RM, Das V, Tripathi G, Agrawal S. Genetic association of phase I and phase II detoxification genes with recurrent miscarriages among North Indian women. Mol Hum Reprod. 2010;16:207–214. doi: 10.1093/molehr/gap096. [DOI] [PubMed] [Google Scholar]
- 13.Arvanitis DA, Goumenou AG, Matalliotakis IM, Koumantakis EE, Spandidos DA. Low-penetrance genes are associated with increased susceptibility to endometriosis. Fertil Steril. 2001;76:1202–1206. doi: 10.1016/S0015-0282(01)02865-5. [DOI] [PubMed] [Google Scholar]
- 14.Peng DX, He YL, Qiu LW, Yang F, Lin JM. Association between gene mutation of cytochrome P450A1 in exon 7 A4889G locus and susceptibility to endometriosis. Chin J Med Genet. 2003;20:284–286. [PubMed] [Google Scholar]
- 15.Yang LP, An XF. Analysis on the relationship between polymorphism of Exon 7 situs in CYP1A1 gene, GSTM1 gene and susceptibility of endometriosis in women of Han nationality in Jilin city. Matern Child Health Care China. 2009;24:2556–2559. [Google Scholar]
- 16.Matsuzaka Y, Kikuti YY, Goya K, Suzuki T, Cai LY, Oka A, et al. Lack of an association human dioxin detoxification gene polymorphisms with endometriosis in Japanese women: results of a pilot study. Environ Health Prev Med. 2012;17:512–517. doi: 10.1007/s12199-012-0281-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu CH, Guo CY, Yang JG, Tsai HD, Chang YJ, Tsai PC, et al. Polymorphisms of dioxin receptor complex components and detoxification-related genes jointly confer susceptibility to advanced-stage endometriosis in the taiwanese han population. Am J Reprod Immunol. 2012;67:160–168. doi: 10.1111/j.1600-0897.2011.01077.x. [DOI] [PubMed] [Google Scholar]
- 18.Rozati R, Giragalla SB, Bakshi H, Doddamaneni S, Khaja N, Sharma RS. The CYP1A1 and GSTM1 genetic polymorphisms and susceptibility to endometriosis in women from South India. Int J Fertil Steril. 2008;2:105–112. [Google Scholar]
- 19.Tsuchiya M, Tsukino H, Iwasaki M, Sasaki H, Tanaka T, Katoh T, et al. Interaction between cytochrome P450 gene polymorphisms and serum organochlorine TEQ levels in the risk of endometriosis. Mol Hum Reprod. 2007;13:399–404. doi: 10.1093/molehr/gam018. [DOI] [PubMed] [Google Scholar]
- 20.Juo SH, Wang TN, Lee JN, Wu MT, Long CY, Tsai EM. CYP17, CYP1A1 and COMT polymorphisms and the risk of adenomyosis and endometriosis in Taiwanese women. Hum Reprod. 2006;21:1498–1502. doi: 10.1093/humrep/del033. [DOI] [PubMed] [Google Scholar]
- 21.Huber A, Keck CC, Hefler LA, Schneeberger C, Huber JC, Bentz EK, et al. Ten estrogen-related polymorphisms and endometriosis: a study of multiple gene-gene interactions. Obstet Gynecol. 2005;106:1025–1031. doi: 10.1097/01.AOG.0000185259.01648.41. [DOI] [PubMed] [Google Scholar]
- 22.Babu KA, Reddy NG, Deendayal M, Kennedy S, Shivaji S. GSTM1, GSTT1 and CYP1A1 detoxification gene polymorphisms and their relationship with advanced stages of endometriosis in South Indian women. Pharmacogenet Genomics. 2005;15:167–172. doi: 10.1097/01213011-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Ivashchenko TE, Shved NI, Kramareva NA, Aĭlamazian EK, Baranov VS. Analysis of the polymorphic alleles of genes encoding phase 1 and phase 2 detoxication enzymes in patients with endometriosis. Genetika. 2003;39:525–529. [PubMed] [Google Scholar]
- 24.Iizuka S, Kosugi Y, Isaka K, Takayama M. Could polymorphisms of N-acetyltransferase 2 (NAT2), glutathione S-transferase M1 (GSTM1), and cytochrome P450 (CYP1A1) be responsible for genetic predisposition to endometriosis among Japanese? J Tokyo Med Univ. 2003;61:59–66. [Google Scholar]
- 25.Hadfield RM, Manek S, Weeks DE, Mardon HJ, Barlow DH, Kennedy SH, et al. Linkage and association studies of the relationship between endometriosis and genes encoding the detoxification enzymes GSTM1, GSTT1 and CYP1A1. Mol Hum Reprod. 2001;7:1073–1078. doi: 10.1093/molehr/7.11.1073. [DOI] [PubMed] [Google Scholar]
- 26.Cao YH, Yao L, Wang D, Han P. Relationship between endometriosis and cytochrome P4501A1 genetic polymorphism of the Hans Tangshan Heibei province. Chinese J Coal Ind Med. 2008;11:810–812. [Google Scholar]
- 27.Peng DX, He YL, Qiu LW, Lin JM. The influence of gene mutation of CYP1A1 and GSTM1 on the endometriosis susceptibility. Guangdong Med J. 2004;25:923–924. [Google Scholar]
- 28.Peng DX, He YL, Qiu LW, Yang F, Lin JM. Susceptibility to endometriosis in women of Han Nationality in Guangdong Province associated with Msp I polymorphisms of cytochrome P450 1A1 gene. J First Mil Med Univ. 2002;22:814–816. [PubMed] [Google Scholar]
- 29.Birnbaum LS, Cummings AM. Dioxins and endometriosis: a plausible hypothesis. Environ Health Perspect. 2002;110:15–21. doi: 10.1289/ehp.0211015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nebert DW, McKinnon RA, Puga A. Human drug-metabolizing enzyme polymorphisms: effects on risk of toxicity and cancer. DNA Cell Biol. 1996;15:273–280. doi: 10.1089/dna.1996.15.273. [DOI] [PubMed] [Google Scholar]
- 31.Spink DC, Eugster HP, Lincoln DW, 2nd, Schuetz JD, Schuetz EG, Johnson JA, et al. 17 beta-estradiol hydroxylation catalyzed by human cytochrome P450 1A1: a comparison of the activities induced by 2,3,7,8-tetrachlorodibenzo-p-dioxin in MCF-7 cells with those from heterologous expression of the cDNA. Arch Biochem Biophys. 1992;293:342–348. doi: 10.1016/0003-9861(92)90404-K. [DOI] [PubMed] [Google Scholar]
- 32.Zhao YC, Gong P, Chen YR, Nwachukwu JC, Srinivasan S, Ko CM, et al. Dual suppression of estrogenic and inflammatory activities for targeting of endometriosis. Sci Transl Med. 2015;7:271ra9. doi: 10.1126/scitranslmed.3010626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah PP, Saurabh K, Pant MC, Mathur N, Parmar D. Evidence for increased cytochrome P450 1A1 expression in blood lymphocytes of lung cancer patients. Mutat Res. 2009;670:74–78. doi: 10.1016/j.mrfmmm.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 34.Crofts F, Taioli E, Trachman J, Cosma GN, Currie D, Toniolo P, et al. Functional significance of different human CYP1A1 genotypes. Carcinogenesis. 1994;15:2961–2963. doi: 10.1093/carcin/15.12.2961. [DOI] [PubMed] [Google Scholar]
- 35.Taioli E, Bradlow HL, Garbers SV, Sepkovic DW, Osborne MP, Trachman J, et al. Role of estradiol metabolism and CYP1A1 polymorphisms in breast cancer risk. Cancer Detect Prev. 1999;23:232–237. doi: 10.1046/j.1525-1500.1999.09912.x. [DOI] [PubMed] [Google Scholar]
- 36.Masson LF, Sharp L, Cotton SC, Little J. Cytochrome P-450 1A1 gene polymorphisms and risk of breast cancer: a HuGE review. Am J Epidemiol. 2005;161:901–915. doi: 10.1093/aje/kwi121. [DOI] [PubMed] [Google Scholar]
- 37.Trikalinos TA, Salanti G, Khoury MJ, Ioannidis JP. Impact of violations and deviations in Hardy-Weinberg equilibrium on postulated gene-disease associations. Am J Epidemiol. 2006;163:300–309. doi: 10.1093/aje/kwj046. [DOI] [PubMed] [Google Scholar]
- 38.Fan W, Li S, Chen Q, Huang Z, Ma Q, Xiao Z. Association between interleukin-10 promoter polymorphisms and endometriosis: a meta-analysis. Gene. 2013;515:49–55. doi: 10.1016/j.gene.2012.11.037. [DOI] [PubMed] [Google Scholar]
- 39.Sapkota Y, Low SK, Attia J, Gordon SD, Henders AK, Holliday EG, et al. Association between endometriosis and the interleukin 1A (IL1A) locus. Hum Reprod. 2015;30:239–248. doi: 10.1093/humrep/deu267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang QY, Guan Q, Wang Y, Feng X, Sun W, Kong FY, et al. BDNF Val66Met polymorphism is associated with Stage III-IV endometriosis and poor in vitro fertilization outcome. Hum Reprod. 2012;27:1668–1675. doi: 10.1093/humrep/des094. [DOI] [PubMed] [Google Scholar]
- 41.Guo SW. Glutathione S-transferases M1/T1 gene polymorphisms and endometriosis: a meta-analysis of genetic association studies. Mol Hum Reprod. 2005;11:729–743. doi: 10.1093/molehr/gah206. [DOI] [PubMed] [Google Scholar]