Highlights
-
•
The diagnosis of epiploic appendagitis is crucial; CT scan imaging is necessary for an accurate diagnosis.
-
•
CT scan findings are an ovoid mass lesion of fat density, surrounded by a dense rim in all cases.
-
•
Non-surgical management is preferred with CT controls.
Keywords: Acute abdomen, Diagnosis, Computed tomography, Ultrasonography, Management
Abstract
Purpose
The aim of this work is to explain the clinical features and the imaging findings of primitive epiploic appendagitis in 12 patients.
Materials and methods
Twelve patients were examined in 2 University hospitals between January 2011 and June 2016. Their medical charts have been reviewed. Nine patients have undergone enhanced CT examination and only two among them, have had at first an abdominal ultrasound.
Results
The age ranged between 36 and 65 years old. All the patients consulted for an acute abdominal pain in most of the cases in the left iliac fossa with no elevated body temperature nor a significant elevation of the inflammation markers. Ultrasound features showed a hyper-echoic mass surrounded by a hypo-echoic peripheral ring. CT scan images showed a fat ovoid lesion that corresponds to the inflamed Appendix epiploica with a peripheral hyper-attenuating rim and in some cases the central “dot sign” referring to the thrombosed vessel. Only 4 patients underwent surgery.
Conclusion
For its non-specific clinical presentation, that can mimic other surgical affections, and its rather non-operative treatment, the diagnosis of epiploic appendagitis is crucial. Ultrasound and especially CT scan imaging are necessary for an accurate diagnosis.
1. Introduction
The primitive epiploic appendagitis is caused by the inflammation, torsion or ischemia of an epiploic appendage, which is a small adipose protrusion arising from the serosal surface of the colon. It is a relatively rare cause of acute abdominal pain. Depending on its localization, it is frequently misdiagnosed as acute appendicitis or colon diverticulitis. Diagnosis confirmation can be obtained through ultrasound and computed tomography findings and thus additional unnecessary investigation or intervention can be avoided.
2. Patients and methods
Clinical records and CT pictures of 12 consecutive patients who have consulted in 2 University hospitals in Tunisia from January 2011 to June 2016 were reviewed.
The patients consulted the emergency department for an acute abdominal pain. Their complete history was obtained, a full clinical examination was obtained and a routine laboratory investigation was demanded for each.
Two patients have had abdominal ultrasonography and the whole group has undergone a CT examination.
The study was performed according to the World Medical Association Declaration of Helsinki. No informed consent was obtained from research subjects.
3. Results
The study includes 12 patients: 8 females and 4 males. The age ranges between 36 and 65 years old. The clinical examination and laboratory investigations findings are shown in the table (Table 1).
Table 1.
Clinical and biological carachteristics of the 12 patients.
| patient | sex | Age | temperature | Nausea or vomiting | Site of pain | WBC count elements/mm3 | CRP mg/l | surgery | clinical resolution delay (days) |
|---|---|---|---|---|---|---|---|---|---|
| P1 | F | 51 | 37.8 | absent | Left iliac fossa | 10 300 | 26 | 2 | |
| P 2 | F | 58 | 37.5 | absent | Left iliac fossa | 11 800 | 15 | 1 | |
| P 3 | F | 61 | 37 | nausea | Right iliac fossa | 9500 | 30 | 3 | |
| P 4 | F | 38 | 38 | absent | Right iliac fossa | 15000 | 25 | 5 | |
| P 5 | M | 47 | 37.5 | absent | Left iliacfossa | 12000 | 10 | 10 | |
| P 6 | M | 36 | 37 | nausea | Left iliac fossa | 10000 | 5 | 12 | |
| P7 | F | 46 | 37.5 | vomiting | Right upper quadrant | 7500 | 5 | 20 | |
| P 8 | F | 64 | 38.2 | absent | hypogastric and right iliac fosa | 10600 | 20 | laparoscopic resection and appendicectomy | |
| P 9 | F | 65 | 37 | absent | Left iliac fossa | 10280 | 38.4 | 3 | |
| P 10 | M | 54 | 38 | nausea | right flank | 140230 | 18 | laparoscopic resection and appendicectomy | |
| p 11 | M | 53 | 37 | absent | Right iliac fossa | 10100 | Mc burney epiploic resection and appendicectomy | ||
| p 12 | F | 47 | 37 | absent | Right iliac fossa | 7000 | laparoscopic resection and appendicectomy |
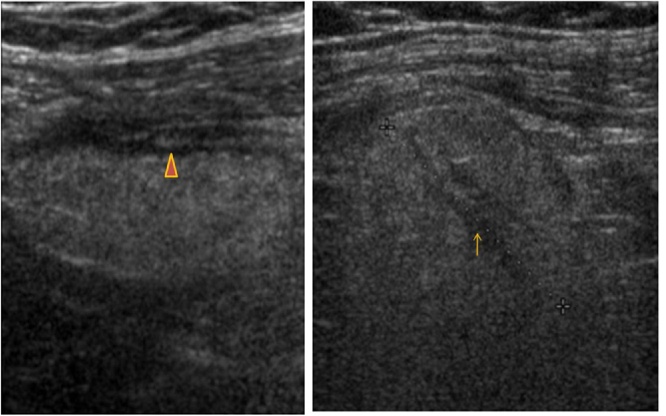
Abdominal ultrasound was performed in two patients. It showed in both cases an ovoid hyperechoic mass surrounded by a hypoechoic halo, hypovascular and incompressible under the probe (Fig. 1).
Fig. 1.
Ultrasoud images (using a high frequency probe): A hyperechoic mass surrounded by a hypoechoic rim (head arrow) with a hypoechoic central element “the dot sign” (arrow).
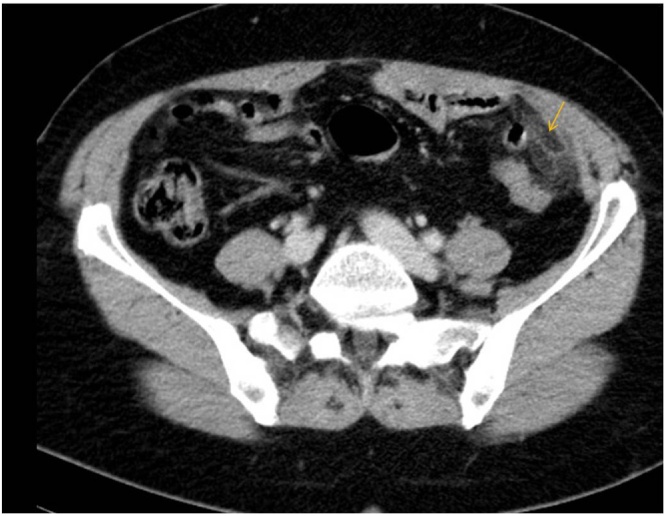
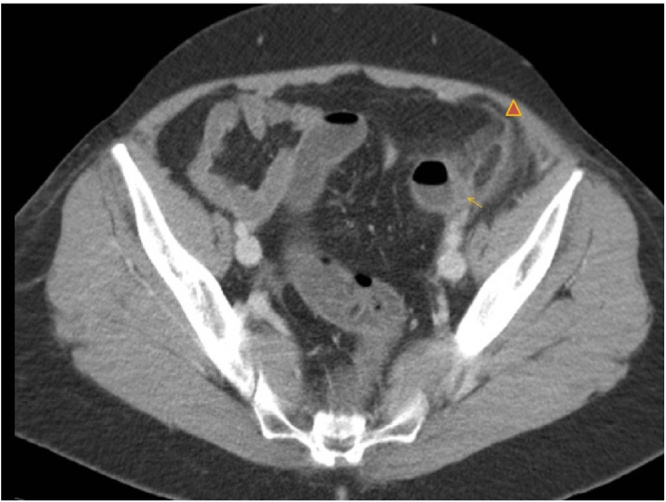
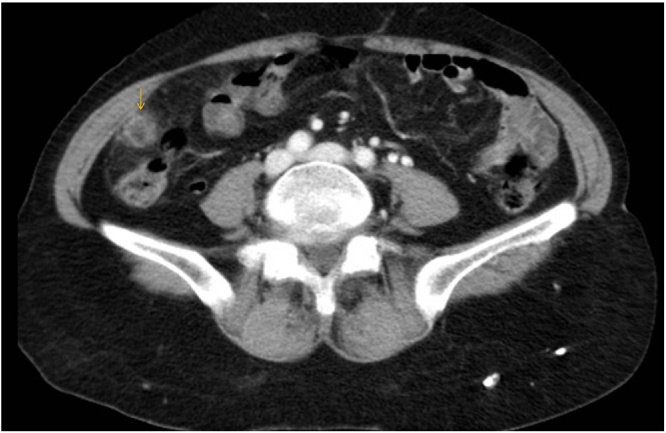
CT scan findings showed an ovoid mass lesion of fat density, surrounded by a dense rim in all cases (Fig. 2, Fig. 3, Fig. 4 ) .It was associated with a thickened peritoneal lining (Fig. 3) and a peri-appendageal fat stranding in cases(Fig. 2, Fig. 3, Fig. 4). In two cases, was noted a high attenuated central dot within the inflamed appendage (Fig. 1, Fig. 2).The localization of the abnormalities corresponded to the site of pain in all cases: attached to the sigmoid colon (n = 6), to the caecum (n = 5) and to the right hepatic flexure (n = 1).
Fig. 2.
Axial CT scan showing an ovoid fat density mass surrounded by a hyper-attenuating ring (arrow) situated on the anti-mesenteric side of the descendant colon with adjacent fat stranding.
Fig. 3.
axial CT Image showing the ovoid fat lesion with the hyper-attenuating peripheral rim. Note the associated localized colon wall thickening (arrow). There is an associated localized peritoneum thickening (head arrow).
Fig. 4.
CT scan image showing a mass that abuts the caecum with an ill defined hyperattenuting surrounding ring (arrow).
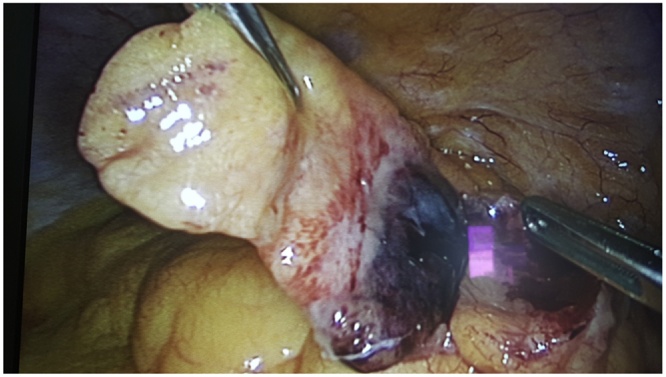
Only 4 patients underwent surgery with a laparoscopic approach in three of them. Intraoperative findings were a central fatty core surrounded by inflammation with an average size 5, 3 cm in length (limits: 4–7 cm). Resection of the infarcted epiploic appendage was performed (Fig. 5).
Fig. 5.
intraoperative laparoscopic view: dissecion of the infarcted epiploic appendage.
In non surgical treatment, complete resolution was observed within 4–20 days (average = 7 days) and without any complication.
4. Discussion
Epiploic appendices are defined as small pouches of peritoneum filled with adipose tissue, arranged along the colon, more frequently on the left colon and the caecum. They have a length that varies between 0.5 and 5 cm. Due to their mobility and low blood supply they have an increased potential of, respectively, torsion or ischemia resulting in their inflammation.
Acute appendagitis is a rare inflammatory affection, which can be either primary or secondary. It occurs mostly in obese patients in the second to fifth decades of life [1]. Heavy exercise is also known to be a contributing factor.
Patients usually describe a strong, non-migrating, sharp pain, localized mostly in the left or right lower abdominal quadrant. Localized tenderness over the site is common and often associated with rebound tenderness without rigidity. These symptoms mimic appendicitis, cholecystitis, and diverticulitis [2].
Fever, nausea, vomiting, decreased appetite and altered bowel function are usually absent [3] however a slightly elevated body temperature might be seen.
Laboratory tests results are non-specific. Although a slight elevation of white blood cells count and serum levels of CRP might be noted, most studies indicate that the inflammation markers are usually normal.
The imaging appearance of acute epiploic appendagitis in ultrasound corresponds to an oval non compressible, hyperechoic mass at the site of maximum tenderness, adjacent to the colon, usually surrounded by a hypoechoic border, with no central blood flow depicted on Doppler ultrasound images [4]. The most common CT feature is a 1.5–3.5-diameter fat-density lesion, that abuts the anterior colonic wall, and that is surrounded by inflammatory changes [5]. The presence of a high attenuation central focus, believed to represent the thrombosed vessel in the Appendix epiploica, although not constant, can be helpful to the diagnosis. We can observe a thickening of the parietal peritoneum, due to the inflammatory process, while the colonic wall remains often normal in thickness.
Differential diagnosis includes omental infarction, appendicitis, and acute diverticulitis. The absence of the hyper-attenuating ring is rather in favor of omental infarction, while in acute diverticulitis, the typical CT findings are the presence of colonic diverticula with inflammation or abscess in the mesocolon with adjacent colonic wall thickening that extends more than 5 cm [4].
If performed, a follow up CT can show at a variable degree the persistence of the imaging abnormalities within the month of evolution and a complete resolution of the signs within six months [1]. In our study only a follow up examination was performed resulting in the amendment of the symptoms and thus no follow up CT was performed for any of the patients. This case series reinforces the findings of the literature about the strong role of CT in the positive diagnosis of acute primitive appendagitis [1], [4], [5].
The treatment of acute primitive appendagitis is a source of debate. Although the non-surgical, conservative method based on oral anti-inflammatory medication is preferred, it is associated with a high rate of recurrence. Laparoscopic removal of the involved appendage is occasionally required and consists of simple ligation and excision of the inflamed appendage [6]. Only four patients have undergone surgery in our case series. Three of them were originally from the regional hospital where there is a CT disponibility problem. In this hospital, primitive epiploic appendagitis with persistence of symptoms was initially misdiagnosed as a surgical emergency (appendicitis).
5. Conclusion
For its treatment to be conservative, the diagnosis of epiploic appendagitis is crucial and supposes the knowledge of its imaging features. The typical presentation on ultrasonography and CT of appendagitis helps discard other differential diagnoses and avoid patients’ unnecessary surgery.
The work has been reported in line with the CARE criteria compliant with the CARE guidelines: http://www.care-statement.org/.
Conflicts of interest
All authors declare there is no conflict of interest
Funding
No source have funded our case series.
Ethical approval
All the figures are anonymized for the case series. Our work is in accordance with medical ethics This study was approved by the ethical committee of the medical school of Tunis.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
We certify that we have participated sufficiently in the intellectual content, conception and design of this work or the analysis and interpretation of the data, as well as the writing of the manuscript, to take public responsibility for it and have agreed to have our name listed as a contributor.
-
1.
Nadida Dali—analysis and interpretation of the data,
-
2.
Amal Ali—study concept and design,
-
3.
I. Marzouk-Mouss—drafting of the manuscript. Acquisition of the data, submitting.
-
4.
Makram Moussa—acquisition of the data (surgery).
-
5.
A. Manamani—study supervision.
-
6.
L. Charrada-Ben Farhat—critical revision of the manuscript for important intellectual content.
-
7.
L. hendaoui—critical revision of the manuscript for important intellectual content.
Guarantor
Pr hendaoui.
References
- 1.Saad J., Mustafa H.A., Elsani A.M., Alharbi F., Alghamdi S. Primary epiploic appendagitis: reconciling CT and clinical challenges. Indian J. Gastroenterol. 2014;33(5):420–426. doi: 10.1007/s12664-014-0466-y. [DOI] [PubMed] [Google Scholar]
- 2.Cho M.S., Hwang-Bo S., Choi U.Y., Kim H.S. A case of epiploic appendagitis with acute gastroenteritis. Pediatr. Gastroenterol. Hepatol. Nutr. 2014;17(4):263. doi: 10.5223/pghn.2014.17.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akinosoglou K., Kraniotis P., Thomopoulos K., Assimakopoulos S.F. Epiploic appendagitis: a non-surgical cause of acute abdomen. Ann. Gastroenterol. 2015;28(2):296. [PMC free article] [PubMed] [Google Scholar]
- 4.Singh A.K., Gervais D.A., Hahn P.F., Sagar P., Mueller P.R., Novelline R.A. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25(6):1521–1534. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
- 5.Singh A.K., Gervais D.A., Hahn P.F., Rhea J., Mueller P.R. CT appearance of acute appendagitis. Am. J. Roentgenol. 2004;183(5):1303–1307. doi: 10.2214/ajr.183.5.1831303. [DOI] [PubMed] [Google Scholar]
- 6.Vázquez-Frias J.A., Castañeda P., Valencia S., Cueto J. Laparoscopic diagnosis and treatment of an acute epiploic appendagitis with torsion and necrosis causing an acute abdomen. JSLS. 2000;4(3):247. [PMC free article] [PubMed] [Google Scholar]