Abstract
A 66-year-old woman was referred to our hospital for investigation of interstitial lung disease. She had spent most of her time in a shrine, and had always been exposed to vaporized paraffin from burning candles. Chest High-resolution computed tomography (HRCT)showed ground-glass attenuation with thickening of septal lines, wh create the so-called “crazy-paving appearance”. Although bronchoalveolar lavage(BAL) and transbronchial biopsy were performed to aid in diagnosis, the findings did not reveal any conclusive information. Improvements on chest radiographs and in the patient's symptoms were observed without any therapeutic intervention; however, one year later, her chest X-ray showed deteriorative changes. Surgical lung biopsy was performed, and the pathological findings were consistent with those of lipoid pneumonia. The patient showed spontaneous remission of the disease. The cause of exogenous lipoid pneumonia was attributed to inhalation of vaporized paraffin from burning candles in the shrine.
This is the first case of lipoid pneumonia that was found to develop from exposure to vaporized paraffin.
Keywords: Exogenous lipoid pneumonia, Paraffin, Candle
1. Introduction
Lipoid pneumonia is a very rare disease and its exposure history remains unclear. The development of exogenous lipoid pneumonia in the present case may be attributed to inhalation of vaporized paraffin from burnt candles.
2. Case report
A 66-year-old woman had been experiencing shortness of breath one year prior to consult. She had no relevant medical history nor was she taking any prescribed medications. She had been living in a shrine ever since she was born. She went to a hospital because she felt a sudden pain in her right shoulder. Her chest X-ray and HRCT images revealed right pneumothorax and interstitial shadow in both lower lungs (Fig. 1). Although the pneumothorax was improved by chest tube drainage, the interstitial lung shadow showed no change. She was referred to our hospital for a detailed investigation for interstitial lung disease. The following clinical observations were recorded at initial examination: respiratory rate, 14 breaths/min; blood pressure, 100/50 mmHg; body temperature, 36.8 °C; oxygen saturation, 91%.
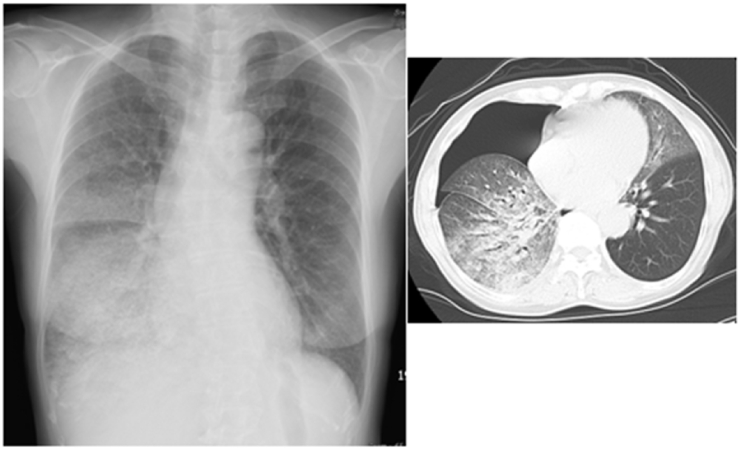
Fig. 1.
Chest X-ray and CT revealed right pneumothorax and interstitial shadow in both lower lungs on first visited to a hospital.
The physical examination showed no abnormal findings except for inspiratory fine crackles in the right lower lung field on auscultation. The laboratory data, including complete blood count, C-reactive protein level, and blood biochemistry, showed no abnormality. Only the serum Krebs Von Den Lungen-6 (KL-6) level was high at 1116 IU/L, and PaO2 was deteriorating at 67.4 mmHg. Chest X-ray and CT showed ground-glass attenuation in the lower field of the right lung (Fig. 2). Differential diagnosis indicated alveolar proteinosis, eosinophilic pneumonia, lipoid pneumonia, and mucinous adenocarcinoma. BAL and transbronchial lung biopsy were performed to facilitate diagnosis. The total cell count of the BAL fluid was 2.1 × 105/ml, and the cellularity differential revealed increased lymphocytes (61%). Both bacterial and fast-acid cultures showed negative results, and non-specific inflammation was observed in the biopsied specimen. In addition, extracellular oily droplets were absent in the cytological examination.
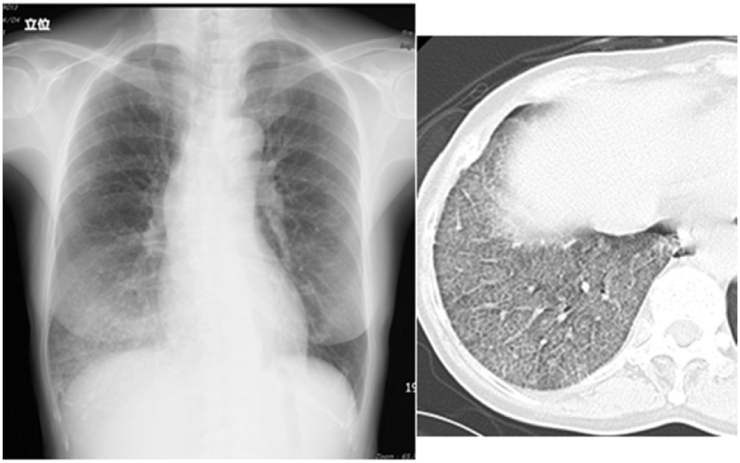
Fig. 2.
After chest tube drainage, interstitial shadow in lower field of the right lung showed no change. Ground-glass attenuation was seen on chest CT.
We advised the patient to wear a mask while she worked in the shrine. Although no treatment was provided, radiological findings improved and dyspnea decreased; furthermore, the serum KL-6 level also decreased with time. However, approximately one year later, chest radiographic findings deteriorated without suspicious trigger, and surgical lung biopsy by video-assisted thoracoscopy was performed to diagnose the condition. Histologically, intra-alveolar fibrosis was observed in a small area (Fig. 3a) and abundant cholesterol cleft granulomas (Fig. 3b), fibrin deposition (Fig. 3c), and aggregating lymphocytes along the alveolar walls were observed. These findings were consistent with the findings of exogenous lipoid pneumonia. Subsequently, improvement in the chest radiograph findings without additional therapy was observed again, and the patient remained in remission.
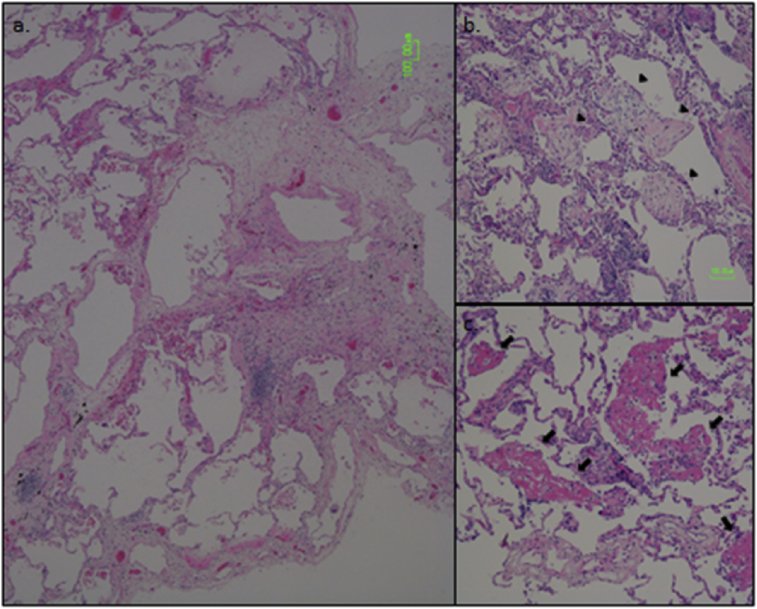
Fig. 3.
Lung biopsy specimens showed on hematoxylin and eosin staining X200, a. intra-alveolar fibrosis was observed in a small area. b. Abundant cholesterol cleft granulomas were seen.(arrow head). c. Fibrin deposition and aggregating lymphocytes along the alveolar walls were observed(arrow).
3. Discussion
Lipoid pneumonia is an uncommon non-infectious, inflammatory disease resulting from aspiration or inhalation of fat-like compounds from animal, vegetable, or mineral oil [1], [2]. It is caused by the accumulation of macrophages that phagocytize the lipids in the intra-alveolar spaces. It is classified into two major categories: exogenous type and endogenous type. The endogenous type occurs because of obstruction by a carcinoma or foreign material. On the other hand, the exogenous type results from recurrent exposure to or inhalation of various types of lipids and oil. Some patients had received a mineral oil nasal instillation, taken laxatives, or aspirated mineral oil [3]. Most of them had predisposing risk factors for aspiration such as swallowing disturbances or episodes of loss of consciousness, or belonged to extremes of age groups. Mineral oils inhibit the cough reflex; therefore, exogenous lipoid pneumonia is frequently asymptomatic and is often detected incidentally on radiographic imaging [3], [4].
Chest radiographic examination shows various characteristic features such as airspace consolidation, ground-glass attenuation, and mass-like shadow [5]. Our case showed right lower lobe dominant ground-glass attenuation that was consistent with lipoid pneumonia. Franquet et al. found that multiple aspirations may result in pulmonary fibrosis [6]. In fact, our case showed intra-alveolar fibrosis in a small area, and we think that the rupture of this area led to pneumothorax. Even though an abundance of cholesterol clefts was observed in the alveolar spaces, lipid vacuoles were not present. It is possible that prevention of exposure to vaporized paraffin from burning candles for one year had caused the accumulation of lipid to disappear. However, a focal fibrin deposition that showed an acute reactive change was observed. It was suggested that deterioration was caused by viral or bacterial infection or re-activation of lipoid pneumonia without inhalation of vaporized paraffin.
Initially, exogenous lipoid pneumonia was not considered in the differential diagnosis because we were not aware of any history of exposure to causative materials. However, we noticed that the patient had been living in a shrine and had a high likelihood of being exposed to candle soot. Japanese traditional candles are made of vegetable oil gathered from Toxicodendron succedaneum (wax tree). Recently, imported candles made of paraffin have been used increasingly because of the reasonable cost. Notably, after burning, the Japanese traditional candle emits soot, whereas the imported candle releases vaporized paraffin. Glynn reported a patient who acquired lipoid pneumonia as a result of using a spray lubricant as a liniment [7]. As this case had a similar clinical situation to ours, we inferred that our case was caused by inhalation of vaporized paraffin from a burnt candle.
Nonetheless, many people are regularly exposed to burned paraffin, e.g., in candle shops or in candle-making jobs; no exogenous lipoid pneumonia case has been reported in these people because they had no symptoms. They might have been diagnosed with other interstitial lung diseases. We believe that exposure to vaporized paraffin is closely associated with the pathogenesis of the disease. We must consider the possibility of exogenous lipoid pneumonia when the characteristic findings of ground-glass attenuation with septal thickening are observed on CT.
Fortunately, our patient showed spontaneous remission. Previous reviews had reported that prevention is the best treatment for lipoid pneumonia. Most of the cases show spontaneous remission after discontinuation of the causative stimuli and appropriate conservative management. However, we believe that wearing masks may provide protection from exposure to paraffin vapors from candles. This is the first case of exogenous lipoid pneumonia that was probably caused by inhalation of vaporized paraffin from burning candles.
References
- 1.Kuroyama M., Kagawa H., Kitada S., Maekura R., Mori M., Hirano H. Exogenous lipoid pneumonia caused by repeated sesame oil pulling: a report of two cases. BMC Pulm. Med. 2015;30 doi: 10.1186/s12890-015-0134-8. 15 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asnis D.S., Saltzman H.P., Melchert A. Shark oil pneumonia. An overlooked entity. Chest. 1993;103:976–977. doi: 10.1378/chest.103.3.976. [DOI] [PubMed] [Google Scholar]
- 3.Gondouin A., Manzoni P., Ranfaing E., Brun J., Cadranel J., Sadoun D. Exogenous lipid pneumonia: a retrospective multicenter study of 44 cases in France. Eur. Respir. J. 1996;9:1463–1469. doi: 10.1183/09031936.96.09071463. [DOI] [PubMed] [Google Scholar]
- 4.Marchiori E., Zanetti G., Mano C.M., Hochhegger B. Exogenous lipoid pneumonia. Clinical and radiological manifestations. Respir. Med. 2011;105:659–666. doi: 10.1016/j.rmed.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Betancourt S.L., Martinez-Jimenez S., Rossi S.E., Truong M.T., Carrillo J., Erasmus J.J. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. Am. J. Roentgenol. 2010;194:103–109. doi: 10.2214/AJR.09.3040. [DOI] [PubMed] [Google Scholar]
- 6.Franquet T., Giménez A., Bordes R., Rodríguez-Arias J.M., Castella J. The crazy-paving pattern in exogenous lipoid pneumonia: CT-pathologic correlation. Am. J. Roentgenol. 1998;170:315–317. doi: 10.2214/ajr.170.2.9456935. [DOI] [PubMed] [Google Scholar]
- 7.Glynn K.P., Gale N. Exogenous lipoid pneumonia due to inhalation of spray lubricant (DW-40 lung) Chest. 1990;97:1265–1266. doi: 10.1378/chest.97.5.1265. [DOI] [PubMed] [Google Scholar]