Abstract
Background
Orem’s self-care model is a nursing model that was introduced with the purpose of improving the self-care of individuals, especially patients suffering from chronic diseases.
Objectives
To determining the effect of Orem’s self-care model on fatigue in multiple sclerosis patients.
Patients and Methods
This research involved a clinical trial. Sixty-three multiple sclerosis patients at the vice-chancellor in treatment affairs of Yasuj University of Medical Sciences were selected based on nonrandom sampling, but they were allocated to the two groups based on random allocation. In the intervention group, Orem’s model was applied during six sessions of 45 - 60 minutes in length, and the process continued for 1 month. The data were collected 1 week before and 7 weeks after the end of the intervention using the Orem’s self-care model-based assessment form and fatigue severity scale, the validity and reliability of which have been
Results
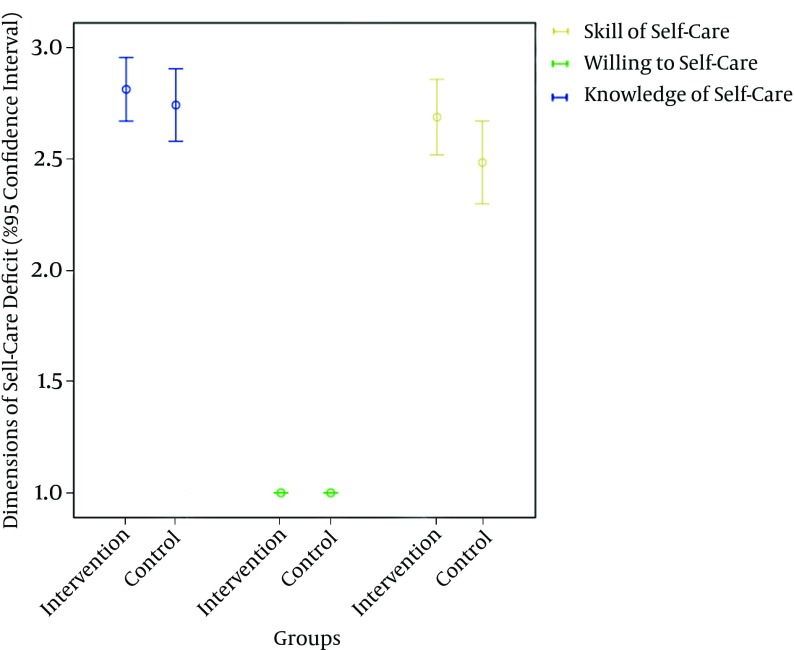
Before the intervention, 11.11% of the participants had a good knowledge of self-care. In addition, self-care willingness and skills were observed in 76.19% and 4.76% of participants, respectively. The mean difference in fatigue reduced significantly in the intervention group after the intervention (P < 0.05). After the intervention, a statistically significant difference was observed in the mean difference of fatigue between the two groups (P < 0.05).
Conclusions
Orem’s self-care model is significantly effective in reducing the fatigue of multiple sclerosis patients.
Keywords: Models, Nursing, Fatigue, Multiple Sclerosis
1. Background
Multiple sclerosis (MS) is a type of autoimmune nervous system disorder that causes impaired transmission of nervous impulses by progressive demyelinating and the accumulation of plaques on the cerebral and spinal cord axons. The disease is classified into four types, namely relapsing-remitting, progressive-relapsing, primary progressive, and secondary progressive (1). The prevalence of the disease in recent decades has shown a rising trend throughout the world, including Iran. Consequently, the number of MS patients has been reported to be about 2 million worldwide (2) and about 60,000 in Iran (3).
MS patients may experience a wide spectrum of symptoms, such as fatigue, motionlessness, numbness, weakness, tremors, pain, spasticity and incontinence, and visual and sexual disorders. Individual and family life depend on the clinical symptoms and complications (4). Fatigue, which has been defined as a subjective complaint involving a perceived feeling of physical and mental inability (5), is one of the most prevalent symptoms reported by the majority of MS patients (6). Therefore, Subira and de Castro (2000) reported that the prevalence of fatigue in these patients is 76.13% (7). The fatigue pattern in these patients may take the form of feeling severe fatigue due to excessive activity, or the feeling of fatigue may be irrelevant to activity (8). Moreover, fatigue affects individuals’ occupations, daily activities, leisure times, and social relations (6, 9).
So far, no decisive treatment method has been introduced for the disease, and the use of palliative and immunosuppressive medications (1) is not sufficiently effective in controlling the fatigue of these patients; furthermore, such medications themselves result in fatigue and other psychosomatic complications (10). In contrast, because of the high cost of treatment (11), the use of non-medicinal methods, such as rehabilitation, consultation, training, rest, relaxation exercises, and energy conservation (12), in addition to being welcomed and accepted by many MS patients, has also attracted the attention of researchers (13). In fact, a review of the available literature shows that interventions like aromatherapy massage (14), stress management (15), humor therapy (16), and designed feeding patterns (17) have been fruitful in remediating fatigue in MS patients.
Empowerment of patients in self-care is one of the many ways to deal with the complications of MS disease (18). Orem’s self-care model is an important nursing models that was introduced with the purpose of enabling patients or care agents to upgrade self-care skills (19). This theory has attracted the attention of many researchers and medical staff aiming to reduce disease complications and the costs of treatment (20). A review of the available studies shows that this model has been applied in the context of different diseases; for example, increased self-care agency has been reported in patients suffering from congestive heart failure (21), bronchial asthma (22), end-stage renal disease (23), cystic fibrosis (24), acquired immune deficiency syndrome (AIDS) (25), and diabetes (26) after applying Orem’s model.
Since, like any other chronic disease, MS necessitates long-term care, self-care skills and empowerment in these patients has become more and more visible. In particular, the motto of world health organization in 2014 was A healthy life with self-care, which shows that self-care is the highest priority in the medical and health services system. Nurses have a vital role in improving the knowledge of patients and increasing their self-care agency and skills in the field of the disease by applying exclusive models of nursing care, including Orem’s model, in clinical wards. In fact, Orem’s model emphasizes that the patients themselves should undertake the responsibility for self-care as the main agent and player; in case of their inability to do so, the skills of those providing care must be upgraded.
2. Objectives
The objective of this article is to examine the effect of Orem’s self-care model on fatigue in MS patients.
3. Patients and Methods
3.1. Design
This study was a single blind randomized clinical trial study where the analyzer was blinded to participants. This article was extracted from the MSc thesis written by the corresponding author with the number 904. The research was approved by the research ethics committee of Yasuj University of Medical Sciences (reference number 93.06.10.06, dated 09/01/2014) and was registered on the site of Iranian registry clinical trials (IRCT; number IRCT2015012020313N2). The conceptual framework for this study was based on the nursing model titled Orem’s self-care model (19).
3.2. Sampling
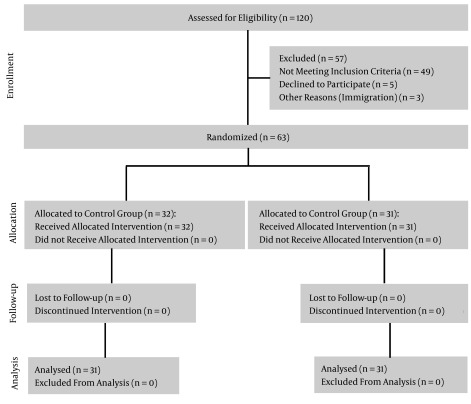
The population of this study consisted of MS patients under treatment who had medical records at the society of special diseases of the vice-chancellor in treatment affairs of Yasuj University of Medical Sciences, Iran, in 2014. Data were collected from health centers affiliated with the Yasuj University of Medical Sciences. Because of the limited population of the study, it was not possible to select the number of samples based on the calculation formula used to estimate the sample size. Among 120 available patients, 63 patients who met the inclusion criteria were selected using a nonrandom sampling method. Next, the samples were divided into two groups, namely an intervention group (32 subjects) and a control group (31 subjects; Figure 1) based on parallel and random allocation of block randomization. There were 16 blocks and four cases in each block. Recruitment began on 07/23/2014 and lasted for 2 months.
Figure 1. Consort Flow Diagram.
3.3. Inclusion and Exclusion Criteria
The inclusion criteria included confirmation of diagnosis of MS disease by a neurologist, being under treatment and having medical records at reliable medical centers, conscious willingness to participate in the research, and lack of known cognitive disorders. Unwillingness to continue participating in the research was the exclusion criterion. Written informed consent was obtained before the research. In addition, emphasis was placed on the confidentiality of information and patients’ ability to exit at will at any stage of the study.
3.4. Measures
The measures described below were used for collecting data related to primary and secondary outcomes (including Orem’s self-care model and fatigue) 1 week before and 2 months after the end of the intervention.
3.4.1. Demographic Information Questionnaire
The questionnaire comprised two parts, one on demographic data and one on disease information.
3.4.2. Orem’s Self-Care Model-Based Assessment Form
This form was organized into two parts. In the first part, items like self-care status, self-care changes, self-care agent, and dependent self-care agent were included. In the second part, self-care needs were assessed.
3.4.3. Exclusive Fatigue Severity Scale for Multiple Sclerosis (FSS)
The scale is a 9-item Likert scale. Responses range from 1 (strongly disagree) to 7 (strongly agree) (27, 28). The validity of the scale has been confirmed as adequate in foreign study (Cronbach’s α = 0.89) (29) and as adequate for the Persian language (α = 0.96) (30). In addition, reliability of this questionnaire has been reported as adequate in foreign study (interclass correlation coefficient [ICC] = 0.81) (29) and as adequate for the Persian language (ICC = 0.93) (30).
3.5. Interventions
The intervention was based on the nursing process of Orem’s self-care model, as follows (Tables 1, 2) (31):
Table 1. [Part 1]. Nursing System Design, Partially Compensatory and Supportive-Educative.
| Self-Care Needs | Self-Care Agency | Self-Care Deficit | Methods of Helping | Implementation |
|---|---|---|---|---|
| Air a | Adequate | No problem | -Guiding | -Air health |
| Water a | Adequate | No problem | -Guiding | -Fluid intake |
| Food a | Adequate | No problem | -Guiding | -Appropriate nutrition |
| Elimination a | Inadequate | Incontinence and constipation related to nervous system disorders | -Guiding; -Teaching | -Bladder training; -Pelvic floor muscle exercises; -Valsalva maneuver; -Availability of toilets; -Fluid intake; -Mobility |
| Activity/rest a | Inadequate | 1-Bathing, grooming, toileting, and rest disorder related to pain, spasticity, and fatigue; 2-Fatigue related to hyperthermia, disease, and drug complications | -Guiding; -Teaching; -Supporting; -Providing an environment | 1-Relief of pain; -Warm Showers; -Hot water bag; -Massage; 2-Planning for daily activities; -Prioritizing tasks; -Energy conservation; -Controlling body temperature; -Arranging ventilation set; -Taking a shower; -Rest; -Reducing level of activity; -Safe intake of vitamins A, D, and E |
| Solitude/social interaction a | Inadequate | Solitude and social interaction disorder related to physical limitations and depression | -Supporting; -Providing an environment | -Written emotional expression; -Humor therapy; -Emotional support |
| Prevention of hazards a | Inadequate | Prevention of hazards disorder related to visual disorders and falling | -Teaching; -Supporting | -Using eye shield for one eye; -Using books with large font; -Designing house environment; -Accessory tools |
| Promotion of normalcy a | Adequate | Patients desired to be normal but could not do something because of the disease. No problem | -Supporting | -Adaptation to disease |
aUniversal needs.
Table 2. [Part 2]. Nursing System Design, Partially Compensatory and Supportive-Educative (Continued).
| Self-Care Needs | Self-Care Agency | Self-Care Deficit | Methods of Helping | Implementation |
|---|---|---|---|---|
| Maintenance of developmental environment a | Inadequate | 1-Sexual disorders related to nervous system disorders, disease, and drug complications; 2-Dependent on significant others due to physical limitations | -Guiding; -Supporting-Providing an environment | -Energy conservation; -Pharmaceutical information; -Emotional support; 2-Accessory tools; -Designing house environment; -Rest; -Emotional support |
| Prevention of conditions threatening normal development a | Inadequate | Occupational deprivation related to disease complications | -Guiding; -Supporting -Providing an environment | -Accepting disease; -Accessory tools -Planning for daily activities; -Rest; -Emotional support |
| Seeking medical assistance b | Adequate | No problem | -Guiding; -Teaching | -Introduction of aspects of disease |
| Awareness of the effects of disease b | Inadequate | Insufficient awareness of disease process related to lack of access to resources and lack of medical staff training | -Teaching | -Introduction of symptoms and complications of disease |
| Effectively carrying out medical regimen b | Inadequate | Insufficient handling of medical regimen related to lack of knowledge and disbelief that their health could improve | -Guiding; -Teaching | -Introduction of medicinal and non-medicinal treatments |
| Awareness of the effects of medical care b | Inadequate | Insufficient awareness of the effects of medical care related to lack of knowledge | -Teaching; -Supporting | -Introduction of non-medicinal treatments and cares |
| Modifying the self-concept in a particular state of health b | Adequate | No problem | -Supporting | -Introduction of aspects of disease |
| Learning to live with effects of disease b | Adequate | No problem | -Guiding; -Supporting | -Introduction of disease complications |
aDevelopmental needs.
bHealth deviation needs.
a, Assessment of self-care needs (including universal, developmental, and health deviation needs) and self-care agency; b, nursing diagnosis or self-care deficit; c, goal setting; a, nursing system design (including wholly compensatory, partially compensatory, and supportive–educative nursing systems) and methods of helping (including acting, guiding, teaching, supporting, and providing an environment); b, planning; a, implementation; b, follow-up; and; c, evaluation.
In the intervention group, 4 cases were included in the partially compensatory and 28 cases in the supportive-educative nursing system. In the control group, 5 and 26 participants were included in the partially compensatory and supportive-educative nursing system, respectively. The intervention for the participants in the partially compensatory nursing system was implemented individually and at home. In the self-care plan for this group, the patients and significant others participated, but in view of the contents of the self-care plan, the process was implemented quite similarly to the group plan. In the intervention group, Orem’s self-care model was applied during six sessions of 45 - 60 minutes in length (3 weeks) by 09/23/2014. After the sessions were over, the self-care model was applied for 4 weeks at home, terminating on 12/13/2014. In the follow-up stage, participants in the intervention group completed the checklist of self-care self-reporting on a daily basis over 4 weeks; their level of obligation to Orem’s model was controlled. In the control group, no intervention was conducted, and the participants received only care and training routines; at the end of the research, nursing interventions were made available to them based on the supportive–educative nursing system.
3.6. Statistical Analysis
Data were analyzed using IBM SPSS statistical software 22. Descriptive statistics (mean, standard deviation, frequency, percentage, and graphs) were calculated for the demographic variables, the mean difference of fatigue severity, dimensions of self-care deficit, and sampling. All of the data were used for analysis and no participants were removed from the analysis due to missing data. The Fisher’s exact test calculated the type of MS disease (relapsing-remitting or primary/secondary progressive), number of admissions (once, more than once), background of other diseases (yes, no), sex, marriage status (single, married), and place of residence (city, village). The chi-square test was used to measure the level of education, occupation, and self-care deficit. With respect to the normal distribution of the fatigue scores, parametrical tests were used in data analysis. The independent samples T-test was used to evaluate age, duration and age of suffering from MS, and the mean difference of fatigue severity between the two groups in terms of the time of intervention. The paired samples T-test was used to calculate the mean difference of fatigue severity within each group before and after the intervention. All tests were two-sided and included a confidence interval of 95% and a significance of P < 0.05.
4. Results
Table 3 reports the demographic variables in the two groups. Based on the relevant statistical tests, no significant difference was observed between the two groups in terms of demographic variables (P > 0.05). The mean differences of fatigue severity were compared in terms of demographic variables; based on the results of independent samples T-test, no significant difference was observed in terms of sex, marital status, occupation, level of education, or type of MS disease (P > 0.05). Moreover, based on Pearson correlation, no significant correlation was observed between fatigue and the variables of age or duration and age of suffering from disease P > 0.05).
Table 3. Demographic Variables in the Intervention and Control Groups (N = 63)a.
| Variable | Intervention (32 Cases) | Control (31 Cases) | P Value |
|---|---|---|---|
| Age, mean ± SD | 6.5 ± 29 | 8.44 ± 30.7 | 0.37b |
| Duration of suffering from MS, mean ± SD | 31.9 ± 52.3 | 27.1 ± 42.8 | 0.20b |
| Age of suffering from MS, mean ± SD | 6.3 ± 24.6 | 8.5 ± 27.1 | 0.10b |
| Type of MS disease | 0.50c | ||
| Relapsing-remitting | 29 (90.6) | 29 (93.5) | |
| Primary and secondary progressive | 3 (9.4) | 2 (6.5) | |
| Number of admissions | 0.50c | ||
| Once | 23 (71.8) | 22 (70.9) | |
| More than once | 9 (28.2) | 9 (29.1) | |
| Background of other diseases | 0.50c | ||
| Yes | 4 (12.5) | 3 (9.6) | |
| No | 28 (87.5) | 28 (90.4) | |
| Sex | 0.17c | ||
| Male | 6 (18.7) | 10 (32.3) | |
| Female | 26 (81.3) | 21 (67.8) | |
| Marriage status | 0.36c | ||
| Single | 21 (65.6) | 18 (58) | |
| Married | 11 (34.4) | 13 (42) | |
| Place of residence | 0.50c | ||
| City | 26 (81.2) | 23 (74.2) | |
| Village | 6 (18.8) | 8 (25.8) | |
| Level of education | 0.38d | ||
| Primary-Guidance | 5 (15.6) | 9 (29) | |
| High school-Diploma | 8 (25) | 8 (25.8) | |
| Higher than diploma | 19 (59.4) | 14 (45.2) | |
| Occupation | 0.80d | ||
| Unemployed | 8 (25) | 7 (22.5) | |
| Schoolchildren and Student | 13 (40.6) | 11 (35.5) | |
| Housekeeper | 6 (18.7) | 5 (16.1) | |
| Others | 5 (15.7) | 8 (25.9) |
aValues are expressed as No. (%) unless otherwise indicated.
bIndependent Samples T-Test.
cFisher’s Exact Test.
dChi-Square Test.
The mean difference in fatigue severity between the two groups was assessed in terms of the time of intervention. With respect to similar studies that have used the FSS in MS patients, the mean difference or effect size of 4.56 was significant (32). In this study, a medium of statistical significant difference of 4 was considered. Before the intervention, the independent samples T-test did not show a significant difference between the two groups in terms of mean difference of fatigue (P > 0.05). After the intervention, however, a statistical significant difference was observed between the two groups (P < 0.05). The mean difference of fatigue within each group before and after intervention was investigated. In the intervention group, paired samples T-test showed a significant difference before and after the intervention (P < 0.05). However, in the control group, a significant difference was observed in the direction of increasing fatigue (P > 0.05; Tables 4, 5).
Table 4. Mean Difference in Fatigue Severity Between the two Groups in Terms of the Time of Intervention.
| Time | Intervention, Mean ± SD | Control, Mean ± SD | Mean Difference | 95% Confidence Interval for Difference | P Valuea | |
|---|---|---|---|---|---|---|
| Upper Bound | Lower Bound | |||||
| Before intervention | 0.37 ± 6.22 | 0.40 ± 6.04 | 0.18 | 0.37 | -0.01 | 0.70 |
| After intervention | 0.39 ± 1.68 | 0.26 ± 6.45 | -4.77 | -4.60 | -4.94 | 0.001b |
aIndependent samples T-Test.
bStatistical significant difference at P < 0.05.
Table 5. Mean Difference of Fatigue Severity Within Each Group, Before and After Intervention.
| Time | Before Intervention, Mean ± SD | After Intervention, Mean ± SD | Mean Difference | 95% Confidence Interval for Difference | P Valuea | |
|---|---|---|---|---|---|---|
| Upper Bound | Lower Bound | |||||
| Intervention | 0.37 ± 6.22 | 0.39 ± 1.68 | 5.45 ± 0.52 | 4.73 | 4.35 | 0.001b |
| Control | 0.40 ± 6.04 | 0.26 ± 6.45 | -0.41 ± 0.38 | -0.27 | -0.54 | 0.001b |
aPaired samples T-Test.
bStatistical significant difference at P < 0.05.
Before the intervention, three dimensions of self-care deficit (including knowledge, willingness, and skills) for the intervention and control groups were illustrated by error bars (Figure 2).
Figure 2. Summary Error Bars of Three Dimensions of Self-Care Deficit (95% Confidence Interval) for the Intervention and Control Groups before the Intervention.
5. Discussion
The present study, which was conducted with the aim of studying the effect of Orem’s self-care model on fatigue in MS patients, indicated that the application of Orem’s model was able to statistically reduce fatigue in the intervention group. An extensive review of the literature was performed regarding the effect of Orem’s self-care model on fatigue in patients with MS and other disorders, but except for a single study, no other research was found in this context. The results of a study by Masoudi et al. (2009), in which they reported a reduction of fatigue and improvement of daily activities in MS patients following the implementation of Orem’s model, are in accordance with the finding of the present research. However, it should be noted that in that study, the Piper Fatigue Scale was used for 70 patients; thus, the scale used and the sample size were different from the present study (33).
Improvement in self-concept (34) and quality of life (35) in MS patients have been reported following the implementation of Orem’s model. In addition, research carried out on individuals with other medical issues, such as diabetic foot ulcers (36) and hypothyroid goiters (37), reported an increase in self-care agent and improvement in quality of life of the patients.
In justifying the effectiveness of this model, it could be said that study of knowledge, willingness, and the self-care skills of the participants showed that patients were facing self-care deficit in relation to MS disease, fatigue, and its complications. It is undeniable that although 92.06% of the patients had reported their willingness to self-care, unawareness of the creating factors and the ways of adjusting fatigue, as well as a lack of skills in this field, illustrated the patients’ self-care deficit. Correspondingly, applying the decreasing guidelines of fatigue in the framework of Orem’s model indicated that the patients’ fatigue had significantly reduced. In addition, using the supportive–educative system for bronchial asthma patients, Kaur et al. (2009) found that the intervention had been significantly fruitful in increasing the self-care knowledge of the intervention group (22). Moreover, by applying Orem’s self-care deficit theory in a diabetes patient, Kumar et al. (2007) reached the nursing diagnosis of knowledge deficit in relation to diabetes management, but the interventions were effective in promoting the knowledge of the patient (26).
Other findings have shown no significant difference in the mean difference of fatigue and the variables of sex, marital status, occupation, level of education, or type of MS disease. Hartelius et al. (2004) did not observe a significant correlation between fatigue and sex, marital status, type of MS disease, or type of medicine (38). The results of that study are lend support to the results of the present research. A significant correlation was demonstrated between fatigue and education level in MS patients in a study by Lerdal et al. (2003), which exclusively assessed the correlation of fatigue and demographic variables (39). This contradiction may have arisen from the difference of cultural conditions, field of education, and level of education of the patients.
By fostering awareness of the self-care needs of MS patients and empowering these individuals, Orem’s self-care model could be significantly effective in reducing the fatigue of these patients. In addition to eliciting awareness of the self-care needs and fatigue in MS patients, the results of this research could be used in all nursing roles, such as teaching, research, management, caring, supporting, consultation, and rehabilitation of patients. Although numerous treatments have so far been applied to improve the fatigue, Orem’s model has various benefits, including its low cost, accessibility, ease of learning, lack of complications, and non-invasiveness; as a result, it has been well accepted by patients. Hence, patients and their families could take a great step towards eliminating different self-care needs by applying the model in their daily life. Since most MS patients are in the age of adolescence and youth, habituation of self-care habits would be more convenient than in the case of other chronic diseases that emerge later in life. When patients’ abilities are restricted, this model can be used by both the patient and significant others. Actually, after recognizing the factors affecting self-care in relation to fatigue, these patients will try to promote their self-care deficit by increasing their knowledge, willingness, and skills related to self-care. By holding training workshops on Orem’s self-care model for nurses and applying it in cases of MS disease, a great step can take towards publicizing the culture of self-care. A nursing process based on Orem’s self-care model can be useful for improving diseases complications.
Although the findings of this research show a reduction of fatigue in MS patients after applying Orem’s self-care model, the research also had some limitations which should be considered in generalization of the results. These are identified as follows:
In terms of the extremely limited population of MS patients in this research, it is proposed that the same study should be carried out on a wider population with a longer duration; another limitation of the present research was that most of the participating patients were in need of a supportive-educative system based on the Orem’s self-care model. It is proposed to study the effect of this model on patients who are in need of a partially compensatory or wholly compensatory system in other studies; most patients in this study exhibited relapsing–remitting MS, and a study on the other types of the disease is recommended; and although the name of the exclusive fatigue severity scale for MS patients (FSS) includes the word severity, the scale chiefly considers the impact of fatigue on daily activities (40). In addition, since the researcher did not have access to other scales to assess fatigue severity in these patients where their validity and reliability had been confirmed in the Persian language except the exclusive fatigue severity scale for MS patients, it is proposed to study the clinical dimensions and fatigue severity with other scales of assessment of fatigue in MS patients, such as fatigue descriptive scale (FDS), neurological fatigue index (NFI-MS), fatigue questionnaire (FQ), checklist for individual strength (CIS), and the fatigue questionnaire and sleep questionnaire.
Acknowledgments
We express our thanks to the MS patients and their families, vice-chancellors for therapeutics and research of Yasuj University of Medical Sciences, and those who assisted in this study. Our sincere gratitude is also extended to her excellency Dr. Robabeh Memarian, scientific faculty member of Tehran Tarbiat Modares University, who paved the way for our research through her consultations.
Footnotes
Authors’ Contribution:Ardashir Afrasiabifar monitoring of intervention, analysis of data, and compiling the article; Zahra Mehri designing the research, sampling, allocating samples to the study groups, implementation of the intervention, collecting data, and compiling the article; Saied Javad Sadat, collecting data; Hamid Reza Ghaffarian Shirazi, analysis of data.
Conflict of Interest:None declared.
Funding/Support:We received a grant from the deputy of research and technology of Yasuj University of Medical Sciences, Iran.
References
- 1.Anderson M. Management of patients with neurologic infections, autoimmune disorders, and neuropathies. In: Smeltzer SCOC, Bare BG, Hinkle JL, Cheever KH, editors. Nursing and health. 2005. pp. 1956–9. [Google Scholar]
- 2.Stuifbergen AK, Blozis SA, Harrison TC, Becker HA. Exercise, functional limitations, and quality of life: A longitudinal study of persons with multiple sclerosis. Arch Phys Med Rehabil. 2006;87(7):935–43. doi: 10.1016/j.apmr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Yavari A. Designing and testing a model of neuropsychopathological, emotional and behavioral variables as precedents of depression in multiple sclerosis patients. Shiraz University,: 2012. [Google Scholar]
- 4.Halper J. The Evolution of Nursing Care in Multiple Sclerosis. Int J MS Care. 2000;2(1):14–22. doi: 10.7224/1537-2073-2.1.14. [DOI] [Google Scholar]
- 5.Krupp LB. Fatigue in multiple sclerosis: a guide to diagnosis and management. Demos Medical Publishing; 2004. [Google Scholar]
- 6.Zifko UA. [Therapy of day time fatigue in patients with multiple sclerosis]. Wien Med Wochenschr. 2003;153(3-4):65–72. doi: 10.1046/j.1563-258x.2003.02014.x. [DOI] [PubMed] [Google Scholar]
- 7.Subira ML, de Castro P. Modalities of fatigue in multiple sclerosis: correlation with clinical and biological factors. Multiple Sclerosis. 2000;6(2):124–30. doi: 10.1177/135245850000600212. [DOI] [PubMed] [Google Scholar]
- 8.Holland NJ, Murray TJ, Reingold S. Multiple sclerosis: a guide for the newly diagnosed. Demos Medical Publishing; 2002. [Google Scholar]
- 9.Lisak D. Overview of symptomatic management of multiple sclerosis. J Neurosci Nurs. 2001;33(5):224–30. doi: 10.1097/01376517-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Hernandez Reif M, Field T, Field T, Theakston H. Multiple sclerosis patients benefit from massage therapy. Bodywork Movement therapies. 1998;2(3):168–74. [Google Scholar]
- 11.McIlveen B, Robertson VJ. A randomised controlled study of the outcome of hydrotherapy for subjects with low back or back and leg pain. Physiotherapy. 1998;84(1):17–26. doi: 10.1016/s0031-9406(05)65898-1. [DOI] [Google Scholar]
- 12.Neill J, Belan I, Ried K. Effectiveness of non-pharmacological interventions for fatigue in adults with multiple sclerosis, rheumatoid arthritis, or systemic lupus erythematosus: a systematic review. J Adv Nurs. 2006;56(6):617–35. doi: 10.1111/j.1365-2648.2006.04054.x. [DOI] [PubMed] [Google Scholar]
- 13.Mallik M, Hall C, Howard D. Nursing Knowledge and Practice. Elsevier Health Sciences; 2009. [Google Scholar]
- 14.Bahraini S, Mannani R, Bekhradi R, Naji SA. The effect of aromatherapy massage on the fatigue severity in women with multiple sclerosis. QJSUMS. 2011;18(3):172–8. [Google Scholar]
- 15.Bassak-Nejad S, Rahimi H, Zargar Y, Majdinasab N. Effects of stress management training based on cognitive-behavioral therapy on chronic fatigue and coping strategies in multiple sclerosis patients. Modern Care J. 2014;10(3):165–72. [Google Scholar]
- 16.Eshgh ZM, Naghavi B, Rashvand F, Majd HA, Derakhshan HB. Effects of humor therapy on fatigue and depression of multiple sclerosis (MS) patients. sbmu. 2011;20(70) [Google Scholar]
- 17.Rashvand F, Moshtagh EZ, Soleimani MA, Abtahi M, Nasiri M, Madani H. Effects of designed feeding patterns on fatigue in multiple sclerosis patients. 2013 [Google Scholar]
- 18.Acton GJ, Malathum P. Basic Need Status and Health-Promoting Self-Care Behavior in Adults. Western J Nur Res. 2000;22(7):796–811. doi: 10.1177/01939450022044764. [DOI] [PubMed] [Google Scholar]
- 19.Meleis AI. Theoretical nursing: Development and progress. Lippincott Williams and Wilkins; 2011. [Google Scholar]
- 20.Strauser DR, Ketz K, Keim J. The relationship between self-efficacy, locus of control and work personality. Rehabilitation. 2002;68(1):20. [Google Scholar]
- 21.21. Jahanbin I HK, Rasti M, Soltani F, Keshavarzi S. The effect of cardiac rehabilitation on performing self-care activities based on orem's self-care model among elderly people suffering from congestive heart failure; A randomized double-blind control. Int J Develop Res. 2014;4(3):784–8. [Google Scholar]
- 22.Kaur S, Behera D, Gupta D, Verma S. Evaluation of a supportive educative Intervention'on self care in patients with bronchial asthma. Nur Mid Res J. 2009;5(2):124–32. [Google Scholar]
- 23.Simmons L. Dorthea Orem's self care theory as related to nursing practice in hemodialysis. Nephrol Nur J. 2009;36(4):419. [PubMed] [Google Scholar]
- 24.Baker LK, Denyes MJ. Predictors of self-care in adolescents with cystic fibrosis: a test of Orem's theories of self-care and self-care deficit. J Pediatr Nurs. 2008;23(1):37–48. doi: 10.1016/j.pedn.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 25.da Luz Sampaio Filho FJ, do Amaral Gubert F, da Costa Pinheiro PN, Martins AK, Vieira NFC, Nóbrega MFB. The life of the adolescent with hiv/Aids and self-care: a descriptive study. objnursing. 2013;12(1):89–105. [Google Scholar]
- 26.Kumar CP. Application of Orem's self-care deficit theory and standardized nursing languages in a case study of a woman with diabetes. Int J Nurs Terminol Classif. 2007;18(3):103–10. doi: 10.1111/j.1744-618X.2007.00058.x. [DOI] [PubMed] [Google Scholar]
- 27.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 28.Schwid SR, Covington M, Segal BM, Goodman AD. Fatigue in multiple sclerosis: current understanding and future directions. J Rehabil Res Dev. 2002;39(2):211–24. [PubMed] [Google Scholar]
- 29.Armutlu K, Korkmaz NC, Keser I, Sumbuloglu V, Akbiyik DI, Guney Z, et al. The validity and reliability of the Fatigue Severity Scale in Turkish multiple sclerosis patients. Int J Rehabil Res. 2007;30(1):81–5. doi: 10.1097/MRR.0b013e3280146ec4. [DOI] [PubMed] [Google Scholar]
- 30.Shahvarughi Farahani A, Azimian M, Fallahpour M, Karimlou M. Evaluation of Reliability and Validity of the Persian Version of Fatigue Severity Scale (FSS) among Persons with Multiple Sclerosis. Rehabilitation. 2013;13(4):84–91. [Google Scholar]
- 31.Alligood MR. Nursing theorists and their work. Elsevier Health Sciences; 2013. [Google Scholar]
- 32.Ghotbi N, Nakhostin Ansari N, Fetrosi S, Shamili A, Choobsaz H. Fatigue in iranian patients with neurological conditions. 2014 [Google Scholar]
- 33.Masoudi R, Kheyri F, Ahmadi F, Mohammadi IT. The effect of Orem's self care model on fatigue and activity daily of living of patients with Multiple Sclerosis. Rehabilitation. 2009;10(3):43–52. [Google Scholar]
- 34.Masoodi R, Khayeri F, Safdari A. Effect of self-care program based on the Orem frame work on self concept in multiple sclerosis patients. goums. 2010;12(3):37–44. [Google Scholar]
- 35.Sahebalzamani M, Zamiri M, Rashvand F. The effects of self-care training on quality of life in patients with multiple sclerosis. Iran J Nurs Midwifery Res. 2012;17(1):7–11. [PMC free article] [PubMed] [Google Scholar]
- 36.Chiang HC, Liu YF, Chang SH. Applying Orem's theory to the care of a diabetes patient with a foot ulcer. Tzu Chi Nur J. 2007;6(6):127–35. [Google Scholar]
- 37.Rahimi A, Salehi SH, Afrasiabifar A. The effect of orem’s self-care model on quality of life of patients with hypothyroid goiter. Armaghane danesh. 2012;17(5) [Google Scholar]
- 38.Hartelius L, Burge A, Johansson A, Ljungsfors A, Mattsson A, Winkworth A, et al. How Does Fatigue Affect Communication? Int J MS Care. 2004;6(2):39–51. doi: 10.7224/1537-2073-6.2.39. [DOI] [Google Scholar]
- 39.Lerdal A, Celius EG, Moum T. Fatigue and its association with sociodemographic variables among multiple sclerosis patients. Mult Scler. 2003;9(5):509–14. doi: 10.1191/1352458503ms943oa. [DOI] [PubMed] [Google Scholar]
- 40.Taylor RR, Jason LA, Torres A. Fatigue rating scales: an empirical comparison. Psychol Med. 2000;30(4):849–56. doi: 10.1017/s0033291799002500. [DOI] [PubMed] [Google Scholar]