Abstract
Introduction
Chronic conditions are among the most common and costly of all health problems. Addressing tobacco use among adults with chronic conditions is a public health priority due to high prevalence as well as greater potential harm from continued use.
Methods
Data were drawn from 9 years (2005–2013) of the U.S. National Survey on Drug Use and Health. Adult (≥18 years) tobacco use included any past 30-day use of cigarettes, cigars, pipes, or smokeless tobacco. Chronic conditions examined included anxiety, asthma, coronary heart disease, depression, diabetes, hepatitis, HIV, hypertension, lung cancer, stroke, and substance abuse. Controlling for sociodemographics, trends in product use for most conditions and a composite of any condition among those with chronic conditions were compared to respondents with no condition in weighted logistic regression analyses.
Results
Cigarette smoking declined significantly over time among adults with no chronic condition. Adults with one or more chronic condition showed no comparable decrease, with cigarette smoking remaining especially high among those reporting anxiety, depression, and substance abuse. Cigar and pipe use remained stable and more prevalent among those with any chronic condition, with the exception of pipe use declining among those with heart disease. Smokeless tobacco use increased over time, with higher prevalence among those with asthma, mental health, and substance abuse conditions.
Conclusions
These findings have tobacco control and regulatory implications for addressing higher tobacco use among adults with chronic conditions. Provider advice and cessation resources targeting tobacco use among those with chronic conditions are recommended.
Keywords: Medical comorbidity, Tobacco, Nicotine, Cigarettes, Cigars, Pipes, Smokeless tobacco, Chronic conditions
1. Introduction
Chronic conditions, such as cancer, heart disease, stroke, type 2 diabetes, and depression, are among the most common and costly of all health problems. For example, in 2012, 117 million (49.8%) civilian, non-institutionalized US adults had at least 1 of 10 selected chronic conditions, and more than half of these adults had multiple chronic conditions (Ward et al., 2014). Seven of the top 10 causes of deaths in 2010 were related to chronic diseases (Centers for Disease Control and Prevention, 2013). Two of these chronic diseases together, cancer and heart disease, account for nearly 48% of all deaths (Centers for Disease Control and Prevention, 2013). Cigarette smoking has been causally linked to many chronic health conditions including cancers and heart diseases (U.S. Department of Health and Human Services, 2014).
In addition to cigarette smoking's causal link to much of chronic disease, many chronic conditions are exacerbated by continued tobacco use. The diagnosis of a chronic condition can be a catalyst for quitting smoking (Keenan, 2009) although these quit attempts may not translate into long-term tobacco cessation (Patel et al., 2009). For a specific example, tobacco use is a known major contributor to cardiovascular disease. While cardiac patients who use tobacco would benefit from quitting smoking, most cardiac patients who smoke resume smoking within 6 months of diagnosis (Barth et al., 2015). Additionally, smoking cessation rates following a cardiac event have not increased over time as they have in the general population (Sochor et al., 2015). Despite the importance of being tobacco-free among patients with medical conditions, coping with withdrawal symptoms while managing the stress associated with having chronic health problems may create additional barriers to cessation.
The challenging relationship between chronic conditions and tobacco use has been relatively well characterized among those with mental health problems. Those with past year mental health problems are well known to have higher smoking rates than adults without mental health issues (Gfroerer et al., 2013). Using data from the National Survey on Drug Use and Health (NSDUH) during 2009–2011, for example, Gfroerer et al. (2013) reported that nearly 20% of adults were diagnosed with some form of mental illness in the past year, 36% of those individuals smoked, and those with mental illness smoke 3 in 10 of all cigarettes smoked by adults. Individuals with substance abuse disorders are also well documented to have higher cigarette smoking prevalence, poorer quit rates, and to be more likely to die from smoking than other substance-related causes (Guydish et al., 2011; Hurt et al., 1996; Schroeder and Morris, 2010; Sobell, 2002). Considered together, the existing literature suggests that individuals with chronic health conditions continue to use tobacco at relatively high rates and bear a disproportionate burden of tobacco-related illness (U.S. Department of Health and Human Services, 2014).
Cigarette smoking in the general population has declined significantly since the first Surgeon General's report in 1964 (U.S. Department of Health and Human Services, 2014) and has continued to decrease steadily over the last decade (Substance Abuse and Mental Health Services Administration, 2014). Smoking rates from NSDUH indicate past month cigarette use declined from 26.0% to 21.3% between 2002 and 2013. However, this decline may not extend to those with chronic conditions. For example, smoking rates declined much more rapidly from 2009 to 2012 among adults without compared to those with mental health conditions (Cook et al., 2014). Much less is known about use among those with other chronic conditions or use of other tobacco products in these populations.
The U.S. Center for Tobacco Products has identified people with “mental health or medical co-morbidities” as a research priority due to high tobacco use prevalence and greater potential harm from use. The primary aim of the present study is to compare trends in adult tobacco use among adults with versus without chronic health conditions. Moreover, to better inform policy and clinical recommendations across the changing tobacco landscape, this study goes beyond examining cigarette smoking and examines trends in the use of non-cigarette tobacco products (i.e., cigars, pipes, and smokeless tobacco products) within each chronic condition subgroup.
2. Method
2.1. Data source
NSDUH, the data source for this report, is a nationally representative survey of the civilian, non-institutionalized U.S. population 12 years of age and older (Substance Abuse and Mental Health Services Administration, 2013) that has been conducted periodically since 1971 and annually since 1990. Due to differences in the survey methodology and design, as well as changes to items assessing the presence of chronic conditions, this report is limited to data obtained from the 2005 through 2013 survey years. Detailed descriptions of survey procedures have been provided for each of the survey years (e.g., Substance Abuse and Mental Health Services Administration, 2007, 2013). Weights are used so that data reflect the US population. The current report is limited to the 335,080 respondents who were 18 years of age or older and provided information regarding the presence of the chronic conditions of interest.
2.2. Measures
The dependent variables were past 30-day use of cigarettes, cigars, pipes, or smokeless tobacco. Respondents were coded as current cigarette smokers if they reported smoking all or part of a cigarette in the 30 days prior to the interview. Similarly, respondents were coded as current users of cigars or pipes if they reported smoking part of or all of a cigar or pipe in the past 30 days. Use of snuff and chewing tobacco in the previous 30 days were combined to form a single variable assessing current use of smokeless tobacco. To ensure comparability of the tobacco use definitions across products, thresholds for lifetime use were not used. Tobacco products were considered independently and use of multiple forms of tobacco was not examined. Thus, those who reported not using cigarettes in the previous 30 days, for example, could potentially have been using another form of tobacco.
The definition of chronic health condition was based on a set of 20 conditions cited by the United States Department of Health and Human Services (Goodman et al., 2013). Because not all of those chronic conditions were assessed as part of NSDUH, the list of chronic conditions examined in this report is limited to heart disease, hypertension, stroke, diabetes, asthma, lung cancer, hepatitis, human immunodeficiency virus (HIV) infection, anxiety, depression, and substance abuse. In addition, items addressing communicable diseases or chronic conditions not on this list of 20 were excluded from this report. With the exception of substance abuse, the respondents were asked “which, if any, of these conditions did a doctor or medical professional tell you that you had in the past 12 months?” Substance abuse was assessed based on questions regarding alcohol and drug use according to an algorithm developed by NSDUH investigators in accordance with the abuse and dependence criteria in the Diagnostic and Statistical Manual of Mental Disorder, Fourth Edition (American Psychiatric Association, 2000).
2.3. Statistical methods
Multiple logistic regression models were developed to examine trends in cigarette, cigar, pipe and smokeless tobacco use over time. The main independent variables of interest were the presence of a chronic condition, time, and the condition-by-time interaction. In the event that the condition-by-time interaction was not statistically significant, the analyses were repeated, eliminating the interaction term in order to assess the main effects of the presence of a chronic condition and time. Analyses examined the effect of having at least one chronic condition as well as each of the separate conditions, provided there was at least one person with that condition in each of the 60 strata at each time point. To allow for comparability across all analyses, the presence or absence of any chronic condition was first determined. Respondents who reported having none of the chronic conditions of interest served as the reference groups for all analyses. This resulted in unequal sample sizes across analyses, with subjects having a chronic condition other than the one under examination in that analysis being removed. All models included respondent age, gender, race/ethnicity, and level of educational attainment as covariates. Conditional proportions of tobacco users were computed for those with and without any chronic disease/specific chronic condition, with the age set to 35 to 49 years, race/ethnicity as Non-Hispanic White, education fixed at “Some College” and assuming equal proportions of men and women. All analyses were conducted using the survey logistic procedure of STATA, version 13.1.
3. Results
3.1. Participant characteristics
A total of 335,080 individuals provided information on both tobacco use and comorbid chronic conditions (Table 1). Of these, 123,089 (29.6%) used tobacco in the previous 30 days, with cigarettes being the product used most frequently (n = 105,392 (24.8%)). Among tobacco users, 25,165 respondents (4.5% of the sample, 15.2% of tobacco users) used multiple tobacco products. A total of 123,353 individuals (41.4%) reported either having been told by a health care professional in the previous year that they had one of the medical or mental health chronic conditions being examined, or met criteria for having a past-year substance abuse disorder, with 33,529 (12.5%) reporting more than one chronic condition. The most prevalent conditions overall were hypertension and substance abuse, comprising 19.0% and 8.9% of the sample, respectively. The distribution of demographic characteristics differs somewhat across the tobacco use groups, which is reflected in the adjusted odds ratios (AOR) describing the relationship between these characteristics and use of specific forms of tobacco (Table 2).
Table 1.
Demographic and chronic condition characteristics of cigarette, cigar, and pipe smokers, users of smokeless tobacco and non-tobacco users. National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
| Characteristic | Current cigarette smokers (n = 105,392) |
Current cigar smokers (n = 26,827) |
Current pipe smokers (n = 3887) |
Current smokeless tobacco users (n = 16,093) |
Current non-tobacco users (n = 211,991) |
Total (n = 335,080) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Adjusted % | N | Adjusted % | N | Adjusted % | N | Adjusted % | N | Adjusted % | N | Adjusted % | |
| Age | ||||||||||||
| 65 + | 1974 | 6.5% | 317 | 4.9% | 172 | 16.7% | 329 | 8.1% | 17,031 | 21.1% | 19,634 | 17.0% |
| 50–64 | 7483 | 21.6% | 1233 | 1.8% | 261 | 21.2% | 700 | 14.4% | 23,250 | 26.0% | 31,982 | 24.7% |
| 35–49 | 19,974 | 30.2% | 3392 | 25.7% | 441 | 19.0% | 3006 | 33.2% | 45,992 | 26.8% | 69,589 | 27.8% |
| 30–34 | 8461 | 10.7% | 1585 | 10.1% | 211 | 8.5% | 1295 | 11.4% | 16,348 | 7.7% | 25,925 | 8.5% |
| 26–29 | 8631 | 10.4% | 1858 | 11.2% | 197 | 7.1% | 1137 | 9.6% | 13,901 | 6.2% | 23,717 | 7.3% |
| 18–25 | 58,869 | 20.6% | 18,442 | 30.7% | 2605 | 27.5% | 9626 | 23.5% | 95,680 | 12.3% | 164,233 | 14.7% |
| Gender | ||||||||||||
| Female | 51,049 | 46.4% | 6520 | 18.4% | 914 | 15.1% | 959 | 5.8% | 125,930 | 56.7% | 179,722 | 51.9% |
| Male | 54,343 | 53.7% | 20,307 | 81.6% | 2973 | 84.9% | 15,134 | 94.2% | 86,061 | 43.3% | 155,358 | 48.1% |
| Race | ||||||||||||
| Non-Hispanic White | 72,302 | 71.3% | 17,590 | 68.9% | 2770 | 75.4% | 13,833 | 86.8% | 129,269 | 66.5% | 214,780 | 68.3% |
| African American | 11,390 | 11.9% | 4141 | 15.9% | 286 | 9.5% | 421 | 5.2% | 27,610 | 11.4% | 41,077 | 11.5% |
| Native American | 2422 | 0.8% | 414 | 0.7% | 109 | 1.2% | 5 | 1.0% | 2145 | 0.4% | 4854 | 0.5% |
| Hawaiian/PI | 503 | 0.3% | 83 | 0.2% | 14 | 0.6% | 77 | 0.3% | 998 | 0.3% | 1565 | 0.3% |
| Asian | 2180 | 2.2% | 389 | 1.3% | 95 | 2.0% | 121 | 0.8% | 10,059 | 5.5% | 12,480 | 4.5% |
| Hispanic | 12,926 | 11.9% | 3197 | 11.3% | 429 | 9.5% | 735 | 4.5% | 37,047 | 14.9% | 51,311 | 13.8% |
| Other | 3669 | 1.6% | 1013 | 1.7% | 184 | 1.8% | 438 | 1.4% | 4863 | 1.0% | 9013 | 1.2% |
| Education | ||||||||||||
| Less than High School Grad | 23,919 | 20.5% | 5472 | 16.7% | 810 | 21.6% | 2863 | 17.0% | 29,337 | 13.2% | 55,535 | 15.0% |
| High School Grad | 40,013 | 37.2% | 9554 | 31.6% | 1352 | 30.4% | 6381 | 38.5% | 63,411 | 28.2% | 109,396 | 30.5% |
| Some College | 29,681 | 27.3% | 8054 | 28.7% | 1136 | 25.0% | 4690 | 26.4% | 62,874 | 25.3% | 98,253 | 25.9% |
| College Grad | 11,779 | 15.0% | 3747 | 23.0% | 589 | 23.1% | 2159 | 18.1% | 56,369 | 33.3% | 71,896 | 28.6% |
| Chronic conditions | ||||||||||||
| No chronic condition | 56,468 | 54.2% | 13,680 | 52.3% | 1868 | 48.2% | 8728 | 54.5% | 144,502 | 60.2% | 211,727 | 58.6% |
| Any chronic condition | 48,924 | 45.8% | 13,147 | 47.7% | 2019 | 51.8% | 7365 | 45.5% | 67,489 | 39.8% | 123,353 | 41.4% |
| One condition | 34,548 | 31.1% | 9654 | 34.0% | 1458 | 36.4% | 5696 | 33.6% | 49,914 | 28.0% | 89,824 | 28.9% |
| More than one condition | 14,376 | 14.8% | 3493 | 13.7% | 561 | 15.4% | 1669 | 11.9% | 17,575 | 11.8% | 33,529 | 12.5% |
| Anxiety | 9256 | 8.5% | 1735 | 6.1% | 292 | 6.5% | 798 | 4.7% | 9515 | 4.2% | 19,470 | 5.3% |
| Depression | 11,218 | 10.5% | 2204 | 7.9% | 351 | 8.3% | 852 | 5.0% | 13,454 | 6.4% | 25,458 | 7.3% |
| Substance abuse | 28,157 | 19.4% | 9259 | 26.3% | 1349 | 23.2% | 4955 | 21.4% | 15,308 | 4.8% | 47,251 | 8.9% |
| Asthma | 7445 | 6.0% | 1911 | 5.7% | 289 | 6.8% | 924 | 5.4% | 13,716 | 5.9% | 22,230 | 5.9% |
| Diabetes | 2631 | 4.6% | 527 | 3.8% | 119 | 7.6% | 375 | 5.1% | 9005 | 8.0% | 12,175 | 7.1% |
| Heart disease | 1335 | 2.7% | 256 | 2.4% | 73 | 5.6% | 173 | 2.5% | 4607 | 4.8% | 6209 | 4.2% |
| Hypertension | 7945 | 13.8% | 1808 | 13.5% | 295 | 16.3% | 1413 | 16.3% | 24,010 | 20.9% | 33,707 | 19.0% |
| Hepatitis | 569 | 0.8% | 78 | 0.4% | 17 | 0.6% | 41 | 0.4% | 444 | 0.3% | 1041 | 0.5% |
| HIV | 165 | 0.2% | 31 | 0.1% | 5 | 0.1% | 10 | 0.1% | 153 | 0.1% | 328 | 0.1% |
| Lung cancer | 56 | 0.1% | 10 | 0.0% | 4 | 0.3% | 7 | 0.1% | 108 | 0.1% | 166 | 0.1% |
| Stroke | 239 | 0.5% | 36 | 0.2% | 8 | 0.3% | 26 | 0.5% | 546 | 0.6% | 808 | 0.5% |
Table 2.
Logistic regressions of sociodemographic characteristics predicting various tobacco product use among US adults (aged ≥18 years). National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
| Cigarettes |
Cigar |
Pipe |
Smokeless Tobacco |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age | <0.01 | <0.01 | <0.01 | <0.01 | ||||||||
| 65 + | Reference | Reference | Reference | Reference | ||||||||
| 50–64 | 3.34 | (3.08, 3.63) | 2.47 | (2.00, 3.04) | 0.91 | (0.70, 1.19) | 1.52 | (1.13, 2.03) | ||||
| 35–49 | 5.06 | (4.72, 5.41) | 2.93 | (2.37, 3.62) | 0.79 | (0.61, 1.04) | 3.21 | (2.43, 4.24) | ||||
| 30–34 | 6.99 | (6.43, 7.59) | 3.83 | (3.05, 4.82) | 1.23 | (0.88, 0.17) | 4.06 | (3.12, 5.29) | ||||
| 26–29 | 8.29 | (7.64, 8.99) | 4.66 | (3.75, 5.80) | 1.17 | (0.85, 1.61) | 3.67 | (2.79, 4.83) | ||||
| 18–25 | 6.48 | (5.99, 7.00) | 6.07 | (4.93, 7.49) | 2.13 | (1.67, 2.72) | 4.06 | (3.09, 5.33) | ||||
| Gender | <0.01 | <0.01 | <0.01 | <0.01 | ||||||||
| Female | Reference | Reference | Reference | Reference | ||||||||
| Male | 1.30 | (1.27, 1.33) | 5.78 | (5.38, 6.22) | 6.07 | (5.43, 6.79) | 19.92 | (16.82, 23.60) | ||||
| Race | <0.01 | <0.01 | <0.01 | <0.01 | ||||||||
| White/Non-Hispanic | Reference | Reference | Reference | Reference | ||||||||
| African American | 0.72 | (0.69, 0.75) | 1.21 | (1.12, 1.30) | 0.77 | (0.55, 0.90) | 0.21 | (0.17, 0.26) | ||||
| Native American | 1.26 | (1.08, 1.46) | 1.15 | (0.85, 1.54) | 1.92 | (1.30, 2.84) | 1.37 | (1.01, 1.86) | ||||
| Hawaiian/PI | 0.66 | (0.51, 0.85) | 0.53 | (0.31, 0.92) | 1.55 | (0.59, 4.07) | 0.73 | (0.49, 1.11) | ||||
| Asian | 0.45 | (0.41, 0.49) | 0.25 | (0.19, 0.32) | 0.45 | (0.32, 0.64) | 0.15 | (0.10, 0.22) | ||||
| Hispanic | 0.46 | (0.44, 0.49) | 0.56 | (0.51, 0.62) | 0.51 | (0.42, 0.62) | 0.16 | (0.14, 0.19) | ||||
| Other | 1.28 | (1.17, 1.40) | 1.29 | (1.04, 1.61) | 1.22 | (0.93, 1.60) | 0.70 | (0.58, 0.85) | ||||
| Education | <0.01 | <0.01 | ||||||||||
| <High School | Reference | <0.01 | Reference | Reference | <0.01 | Reference | ||||||
| High School Grad | 0.69 | (0.66, 0.71) | 0.95 | (0.85, 1.05) | 0.66 | (0.57, 0.78) | 1.11 | (1.00, 1.23) | ||||
| Some College | 0.50 | (0.48, 0.53) | 1.01 | (0.91, 1.13) | 0.65 | (0.55, 0.77) | 0.85 | (0.77, 0.93) | ||||
| College Grad | 0.22 | (0.21, 0.23) | 0.88 | (0.78, 0.99) | 0.59 | (0.49, 0.71) | 0.51 | (0.43, 0.57) | ||||
3.2. Trends in cigarette smoking
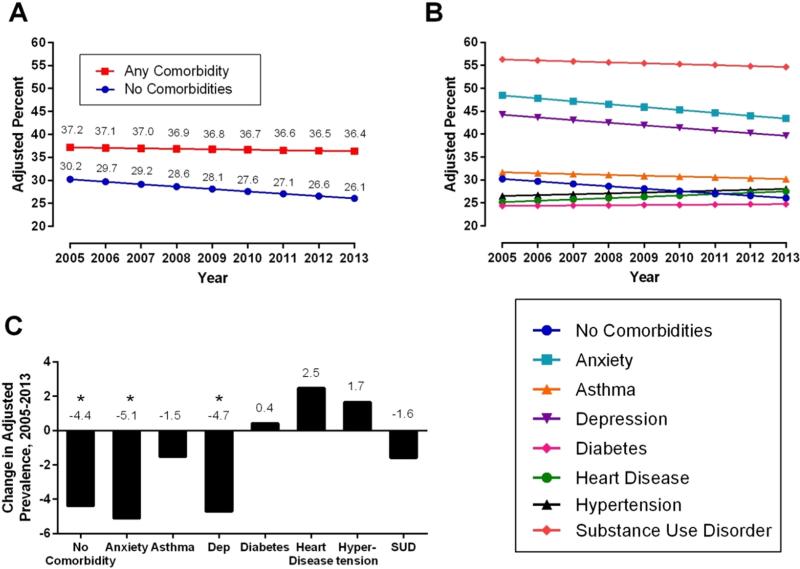
Changes over time in the likelihood of cigarette smoking depended upon whether the respondent had been diagnosed with at least one of the chronic conditions of interest in the past year (Table 3; AOR for interaction (95% CI) = 1.02 (1.01, 1.03), p < 0.01). Among adults who did not endorse a chronic condition, the predicted probability of cigarette smoking declined from 30.2% to 26.1% between 2005 and 2013 (Fig. 1A; p < 0. 01). In contrast, cigarette smoking remained stable among adults with at least one of the 11 chronic conditions examined (2005: 37.2%; 2013: 36.4% p = 0.33). These contrasting trends over time contributed to an increasing disparity in the likelihood of smoking between the two groups, with the difference in the level of smoking between the two groups in 2005 of 6.9% rising to 10.3% by 2013.
Table 3.
Relationship between chronic health conditions and trends over time of tobacco product use among US adults (aged ≥ 18 years). National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
| Cigarettes |
Cigars |
Pipes |
Smokeless Tobacco |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| At least one condition | ||||||||||||
| Interaction | 1.02 | (1.01, 1.03) | <0.01 | Not significant | Not significant | Not significant | ||||||
| Condition | 1.34 | (1.25, 1.43) | <0.01 | 1.57 | (1.49, 1.65) | <0.01 | 1.53 | (1.35, 1.73) | <0.01 | 1.32 | (1.24, 1.41) | <0.01 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1a | 1.00 | (0.99, 1.00) | 0.33 | 0.99 | (0.98, 1.00) | 0.07 | 1.00 | (0.98, 1.03) | 0.88 | 1.02 | (1.00, 1.03) | 0.02 |
| Time trend 2b | 0.97 | (0.97, 0.98) | <0.01 | |||||||||
| Anxiety | ||||||||||||
| Interaction | Not significant | Not significant | Not significant | Not significant | ||||||||
| Condition | 2.18 | (2.07, 2.29) | <0.01 | 1.69 | (1.55, 1.85) | <0.01 | 1.87 | (1.41, 2.49) | <0.01 | 1.17 | (1.04, 1.32) | 0.01 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 0.97 | (0.97, 0.98) | <0.01 | 0.99 | (0.98, 1.00) | 0.21 | 1.00 | (0.96, 1.04) | 0.96 | 1.02 | (1.00, 1.03) | 0.03 |
| Time trend 2 | ||||||||||||
| Depression | ||||||||||||
| Interaction | Not significant | Not significant | Not significant | Not significant | ||||||||
| Condition | 1.85 | (1.76, 1.94) | <0.01 | 1.67 | (1.53, 1.82) | <0.01 | 1.79 | (1.37, 2.33) | <0.01 | 0.94 | (0.82, 1.08) | 0.40 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 0.98 | (0.97, 0.98) | <0.01 | 0.99 | (0.98, 1.01) | 0.31 | 1.01 | (0.97, 1.04) | 0.72 | 1.02 | (1.01, 1.04) | 0.01 |
| Time trend 2 | ||||||||||||
| Substance abuse | ||||||||||||
| Interaction | 1.02 | (1.00, 1.03) | 0.02 | Not significant | Not significant | Not significant | ||||||
| Condition | 3.05 | (2.81, 3.32) | <0.01 | 2.52 | (2.39, 2.65) | <0.01 | 2.22 | (1.93, 2.56) | <0.01 | 1.70 | (1.58, 1.84) | <0.01 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 0.99 | (0.98, 1.00) | 0.19 | 0.99 | (0.98, 1.00) | 0.12 | 1.02 | (0.99, 1.05) | 0.24 | 1.02 | (1.00, 1.03) | 0.01 |
| Time trend 2 | 0.97 | (0.97, 0.98) | <0.01 | |||||||||
| Asthma | ||||||||||||
| Interaction | 1.02 | (1.00, 1.03) | 0.05 | Not significant | Not significant | Not significant | ||||||
| Condition | 1.05 | (0.96, 1.15) | 0.25 | 1.27 | (1.15, 1.40) | 0.01 | 1.58 | (1.22, 2.04) | <0.01 | 1.28 | (1.13, 1.45) | <0.01 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 0.99 | (0.98, 1.01) | 0.28 | 0.99 | (0.98, 1.00) | 0.14 | 1.02 | (0.98, 1.05) | 0.37 | 1.02 | (1.00, 1.04) | 0.02 |
| Time trend 2 | 0.98 | (0.97, 0.98) | <0.01 | |||||||||
| Diabetes | ||||||||||||
| Interaction | 1.03 | (1.00, 1.06) | 0.05 | Not significant | Not significant | Not significant | ||||||
| Condition | 0.71 | (0.60, 0.84) | <0.01 | 0.91 | (0.76, 1.08) | 0.28 | 1.37 | (0.97, 1.94) | 0.07 | 1.11 | (0.93, 1.33) | 0.22 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 1.00 | (0.98, 1.03) | 0.83 | 0.99 | (0.98, 1.00) | 0.12 | 1.00 | (0.97, 1.03) | 1.00 | 1.02 | (1.00, 1.03) | 0.03 |
| Time trend 2 | 0.97 | (0.97, 0.98) | <0.01 | |||||||||
| Heart disease | ||||||||||||
| Interaction | 1.04 | (1.01, 1.08) | 0.02 | Not significant | 0.83 | (0.74, 0.94) | <0.01 | Not significant | ||||
| Condition | 0.75 | (0.61, 0.91) | <0.01 | 0.98 | (0.79, 1.22) | 0.85 | 3.10 | (1.55, 6.22) | <0.01 | 0.81 | (0.66, 0.98) | 0.03 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 1.02 | (0.98, 1.05) | 0.36 | 0.99 | (0.98, 1.01) | 0.22 | 0.84 | (0.75, 0.94) | <0.01 | 1.02 | (1.00, 1.04) | 0.01 |
| Time trend 2 | 0.97 | (0.97, 0.98) | <0.01 | 1.01 | (0.98, 1.05) | 0.51 | ||||||
| Hypertension | ||||||||||||
| Interaction | 1.04 | (1.02, 1.05) | <0.01 | Not significant | Not significant | Not significant | ||||||
| Condition | 0.79 | (0.71, 0.87) | <0.01 | 1.15 | (1.05, 1.25) | <0.01 | 1.12 | (0.87, 1.44) | 0.38 | 1.24 | (1.11, 1.39) | <0.01 |
| No condition | Reference | Reference | Reference | Reference | ||||||||
| Time trend 1 | 1.01 | (0.99, 1.03) | 0.20 | 0.99 | (0.98, 1.00) | 0.18 | 0.99 | (0.96, 1.03) | 0.76 | 1.02 | (1.00, 1.03) | 0.01 |
| Time trend 2 | 0.97 | (0.97, 0.98) | <0.01 | |||||||||
If the interaction term is statistically significant, Time Trend 1 describes changes over time for those with the condition of interest. Otherwise it describes the main effect of time over the nine year period.
If the interaction term is statistically significant, Time Trend 2 describes changes over time for those with the no chronic condition.
Fig. 1.
Trends in cigarette smoking from 2005 to 2013 comparing A) adults with any chronic condition to those with none, B) adults with no chronic condition to each of 7 individual chronic conditions, and C) change in adjusted prevalence from 2005 to 2013 for each chronic condition. National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
When cigarette smoking was examined by chronic condition separately (Fig. 1B and Table 3), stark differences were observed in the likelihood of smoking, but the time trend described above was similar for the majority of chronic conditions examined. The predicted probability of smoking in adults reporting mental health problems or substance abuse disorders ranged between 39.6% and 56.3%, all significantly greater than those for individuals without a chronic condition (all p < 0.01). Compared to those without a chronic health condition, adults with asthma had similar smoking rates (AOR = 1.05 (0.96, 1.15), p = 0.25) and those with diabetes, heart disease, and hypertension had lower smoking rates (AOR = 0.71 (0.60, 0.84), p = 0.01; 0.75 (0.61, 0.91, p < 0.01; 0.79 (0.71, 0.87), p < 0.01, respectively). Smoking among those with anxiety and depression decreased by 5.1% and 4.7%, respectively, between 2005 and 2013 (Fig. 1C), similar to the decrease seen among those without any chronic condition (See Table 3 for the full results).
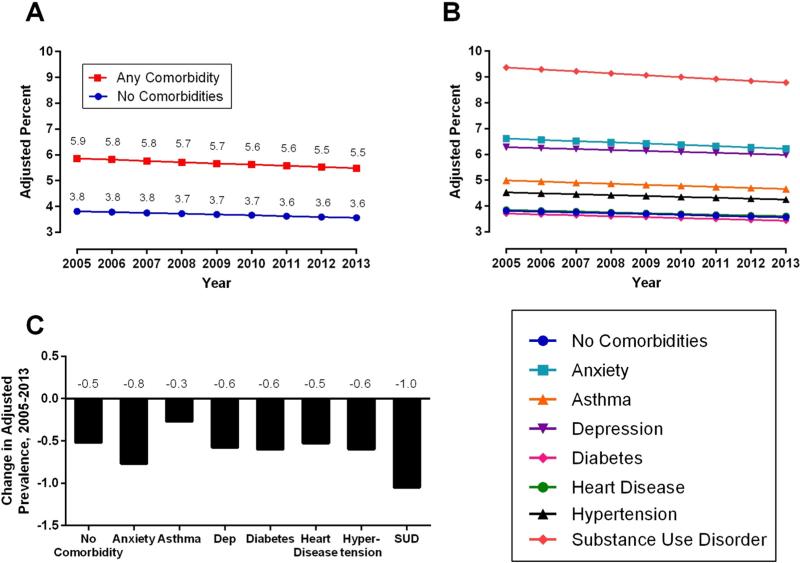
3.3. Trends in cigar smoking
Cigar smoking was higher across all years among adults with at least one chronic condition (Fig. 2A; 2005: 5.9%, 2013: 5.5%; AOR = 1.57 (1.49, 1.65), p < 0.01) compared to those without a chronic condition (2005: 3.8%; 2013: 3.6%,). However, no significant change over time was observed (AOR = 0.99 (0.98, 1.00), p = 0.07).
Fig. 2.
Trends in cigar smoking from 2005 to 2013 comparing A) adults with any chronic condition to those with none, B) adults with no chronic condition to each of 7 individual chronic conditions, and C) change in adjusted prevalence from 2005 to 2013 for each chronic condition. National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
As with cigarettes, those with anxiety, depression and substance abuse disorders exhibited the highest rates of cigar use, with prevalence ranging between 6.0% and 9.4% (Fig. 2B). These rates were significantly greater than among those without a chronic condition (AORs = 1.69 (1.55, 1.85), p < 0.01; 1.67 (1.53, 1.82), p < 0.01; 2.52 (2.39, 2.65, < 0.01, respectively). Cigar smoking among those with hypertension or asthma was also significantly elevated (AOR = 1.15, (1.05, 1.25), p < 0.01 and 1.27 (1.15, 1.40), p < 0.01, respectively). There were no significant differences in cigar use among those with diabetes and heart disease compared to those who did not report a chronic condition (AOR = 0.91, (0.76, 1.08), p = 0.28 and 0.98 (0.79, 1.22), p = 0.85, respectively).
As with the results for any chronic condition, there were no significant changes over time in cigar smoking among people reporting each of the specific chronic conditions examined (Fig. 2C).
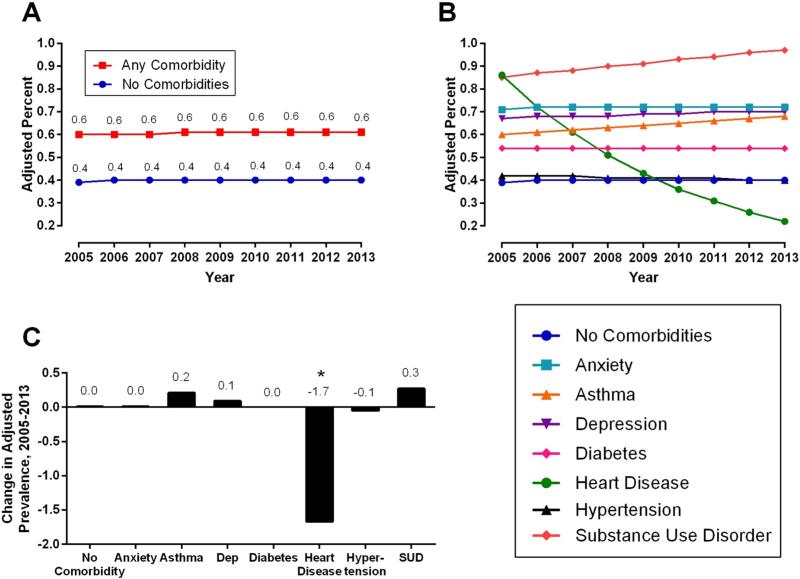
3.4. Trends in pipe smoking
Pipe smoking was significantly higher among individuals reporting at least one chronic condition (AOR = 1.53 (1.35, 1.73), p < 0.01; 2005: 0.60%, 2013: 0.61%; Fig. 3A) than among those with none (2005:0.39%, 2013: 0.40%). Overall trends in pipe smoking remained stable over time (AOR = 1.00 (0.98, 1.03), p = 0.88).
Fig. 3.
Trends in pipe smoking from 2005 to 2013 comparing A) adults with any chronic condition to those with none, B) adults with no chronic condition to each of 7 individual chronic conditions, and C) change in adjusted prevalence from 2005 to 2013 for each chronic condition. National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
Pipe smoking among those with anxiety, depression, substance abuse disorders, and asthma ranged between 0.60% and 0.97% (Fig. 3B), significantly higher compared to those without a chronic condition (AOR = 1.87 (1.41, 2.49), p < 0.01; 1.79 (1.37, 2.33), p < 0.01; 2.22 (1.93, 2.56), p < 0.01; 1.58 (1.22, 2.04), p < 0.01, respectively).
Few with chronic conditions showed significant changes in the probability of smoking pipes over time (Fig. 3C). The notable exception was among those with heart disease, where pipe smoking decreased from a high of 2.3% to 0.6% between 2005 and 2013 (AOR for interaction = 0.83 (0.74, 0.94), p < 0.01; AOR for those with heart disease = 0.84 (0.75, 0.94), p < 0.01, AOR for those with no chronic condition = 1.00 (0.98, 1.03), p = 088).
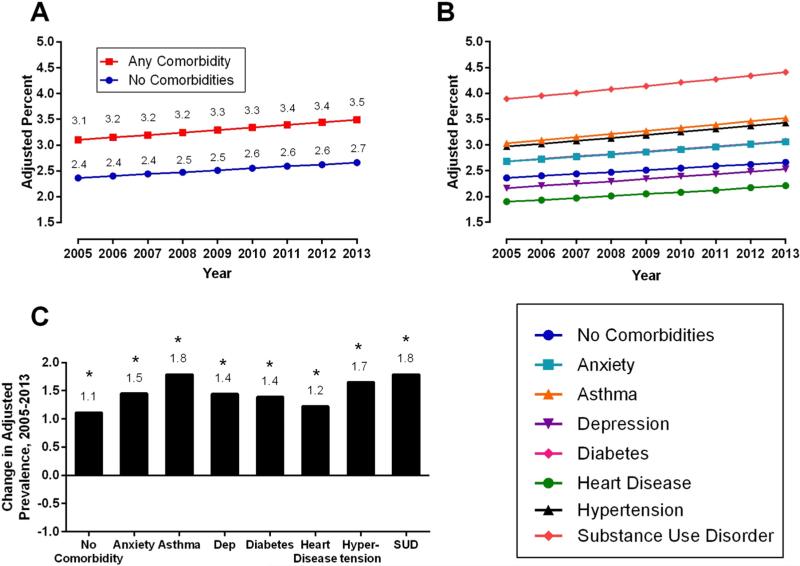
3.5. Trends in smokeless tobacco use
Rates of smokeless tobacco use were higher among adults reporting at least one chronic condition (3.10%–3.49%) compared to those with none (2.36%–2.66%; AOR = 1.32 (1.24, 1.41), p < 0. 01; Fig. 4A). There was also a significant increase in smokeless tobacco use over time among those with and without chronic conditions (AOR = 1.02 (1.00, 1.03), p = 0.02).
Fig. 4.
Trends in smokeless tobacco use from 2005 to 2013 comparing A) adults with any chronic condition to those with none, B) adults with no chronic condition to each of 7 individual chronic conditions, and C) change in adjusted prevalence from 2005 to 2013 for each chronic condition. National Survey on Drug Use and Health (NSDUH), United States, 2005–2013.
Smokeless tobacco use among those with anxiety, substance abuse disorders, asthma, and hypertension (Fig. 4B, Table 3), was significantly higher across years compared to those without a chronic condition (AORs = 1.17 (1.04, 1.32), p = 0.01; 1.70 (1.58, 1.84), p < 0.01; 1.28 (1.13, 1.45), p < 0.01; 1.24 (1.11, 1.39), p < 0.01, respectively), while those with heart disease exhibited decreases in smokeless tobacco use (AOR = 0.81 (0.66, 0.98), p = .03).
Smokeless tobacco use among individuals with any of the chronic health conditions examined increased between 2005 and 2013 (Fig. 4C; see Table 3 for the complete set of AORs).
4. Discussion
Overall, current cigarette smoking was more common among US adults who reported at least one chronic condition and these higher rates did not decline from 2005 to 2013 as they did for adults without a chronic condition. When disentangled, there were significant differences in cigarette smoking for each of the chronic conditions compared to adults without a chronic condition examined in this study. Adults with mental health and substance abuse conditions were more likely to be current smokers compared to those with the other chronic conditions. These results are consistent with other reports (Cook et al., 2014) in suggesting that tobacco control policies targeting the general population have not worked as effectively within subpopulations of those with mental illnesses and substance abuse disorders. Cigarette smoking among those with anxiety and depression declined slightly between 2005 and 2013; however smoking rates in these groups remained significantly higher than rates among adults without a chronic condition across all years. Adults with other chronic health conditions such as asthma, diabetes, heart disease, hypertension and substance abuse did not see declines in smoking over time compared to adults without chronic conditions. To our knowledge, this latter observation has not been previously reported.
The relatively stable cigarette smoking rates among adults with chronic health conditions is concerning given that smoking is linked to these chronic conditions and continued tobacco use is likely to worsen them. For example, our analyses indicate that 1 in 4 adults who had been told that they had heart disease in the past 12 months were still smoking. In fact, multisite studies in the US report smoking prevalence of 27 to 36% in those hospitalized for an acute cardiac condition (Agaku et al., 2014; LaBresh et al., 2007; Leifheit-Limson et al., 2013). This signifies that greater public health efforts are needed to reduce smoking in populations already suffering from tobacco-related diseases.
While cigarette smoking has declined over time in the US among those without chronic conditions, non-cigarette tobacco use has not declined over time for any group. Cigar and pipe smoking remained steady over the 9-year time span and use of each product was higher among adults with at least one chronic condition compared to those without a chronic condition. Of note, pipe smoking among adults with heart disease was the only chronic condition to show a significant decline in use of non-cigarette tobacco products. It may be that those who have been told that they have heart disease are a unique group who have successfully reduced their pipe smoking but may not have been able to quit other tobacco products. This requires further study of the health messages and provider warnings that have potentially motivated cessation of some tobacco products to inform how to better support individuals using other products to quit and stay tobacco-free.
In contrast to declines in cigarette smoking, use of smokeless tobacco products increased over time for those with chronic conditions as it did among those without chronic conditions. The National Health Interview Surveys (Pleis et al., 2003; Pleis and Lethbridge-Çejku, 2006; Schiller et al., 2012) reported similar findings in the general population such that adult smokeless tobacco use, mainly snuff, increased in the US in the past decade. Smokeless tobacco use in our study was higher among those with substance abuse disorders and those with asthma, anxiety and depression. With use of various smokeless products on the rise, particularly among vulnerable groups with chronic health conditions, a better understanding is needed of issues regarding patterns of use and the potential for reduced harm (e.g. using smokeless products along with cigarettes or to replace cigarettes).
This study has several limitations that merit mention. First, all measures were self-report and respondents were asked to identify whether a physician told them that they had the condition in the past 12-months and it was therefore not possible to ascertain the timing of when they were initially diagnosed. Second, this report was limited to studying only the chronic conditions measured in the NSDUH surveys. Additionally, although diseases such as stroke, HIV, and lung cancer are among the chronic conditions included in NSDUH, low sample sizes in these lower prevalence conditions prohibited separate examination in our analyses. Third, our findings are limited to 2005–2013 as not all of the smoking and chronic condition questions were administered in previous waves. Fourth, NSDUH is a cross-sectional population based survey that does not allow for causal inferences about whether smoking was influenced by the chronic conditions, whether diagnosis of a chronic condition facilitated smoking cessation, or a third variable influenced both. It was also outside the scope of this study to examine interactions between the individual chronic conditions. How these chronic conditions may interact with each other is an area in need of further investigation. Despite these limitations, our findings provide evidence of diverging trends in cigarette smoking rates among individuals with and without chronic conditions, and report for the first time prevalence rates across cigarette and non-cigarette products for a variety of chronic health conditions.
5. Conclusion and implications
The Family Smoking Prevention and Tobacco Control Act (TCA) gives the Food and Drug Administration (FDA) broad authority to regulate tobacco product manufacturing, distribution and marketing to reduce the public health toll from tobacco products in the US. While various tobacco control and prevention policies have contributed to reduced prevalence of cigarette smoking in the US (U.S. Department of Health and Human Services, 2014), these declines are not being realized among groups coping with chronic conditions. Declines have also not been observed for non-cigarette tobacco products that do not currently have the same restrictions on flavoring and marketing as those imposed on cigarettes. In addition to regulatory implications, there are clear clinical implications. Physician advice and public health communications must continue to be developed to reduce the high prevalence of tobacco use among people with mental health and substance abuse conditions, as well as the continued use of tobacco among groups currently suffering from tobacco-related diseases. Disparities in who is most likely to receive advice to quit smoking from health care providers have been reported in other national datasets, with only half of all smokers reporting receipt of advice to quit (Danesh et al., 2014). It remains to be explicitly studied if certain groups such as those who are diagnosed with heart disease are more likely to receive cessation advice and support compared to other chronic condition groups such as those with mental health and substance abuse issues. Accumulating data support the need for targeted communication and more accessible cessation support for uniquely vulnerable groups coping with chronic conditions to reduce the disparate burden of tobacco-related disease and death in the United States.
Supplementary Material
Acknowledgments
Funding
This project was supported in part by Tobacco Centers of Regulatory Science (TCORS) award P50DA036114 from the National Institute on Drug Abuse (NIDA) and Food and Drug Administration (FDA), TCORS award P50CA180908 from the National Cancer Institute (NCI) and FDA, Center for Evaluation and Coordination of Training and Research (CECTR) in Tobacco Regulatory Science award U54CA189222 from NCI and FDA, Institutional Training Grant award T32DA07242 from NIDA, and Centers of Biomedical Research Excellence P20GM103644 award from the National Institute on General Medical Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Footnotes
Competing interests
The authors have no conflicts of interest to report.
Transparency document
The Transparency document associated with this article can be found, in the online version.
References
- Agaku IT, King BA, Husten CG, Bunnell R, Ambrose BK, Hu SS, Holder-Hayes E, Day HR, Centers for Disease, C., Prevention Tobacco product use among adults–United States, 2012-2013. MMWR Morb. Mortal. Wkly Rep. 2014;63:542–547. [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Author; Washington, DC.: 2000. [Google Scholar]
- Barth J, Jacob T, Daha I, Critchley JA. Psychosocial interventions for smoking cessation in patients with coronary heart disease. Cochrane Database Syst. Rev. 2015;7:CD006886. doi: 10.1002/14651858.CD006886.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Deaths and Mortality. NCHS FastStats Centers for Disease Control and Prevention; Atlanta, GA: 2013. [Google Scholar]
- Cook B, Wayne G, Kafali E, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311:172–182. doi: 10.1001/jama.2013.284985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danesh D, Paskett ED, Ferketich AK. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev. Chronic Dis. 2014;11:E131. doi: 10.5888/pcd11.140053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gfroerer J, Dube S, King B, Garrett B, Babb S, McAfee T. Vital signs: current cigarette smoking among adults aged ≥18 years with mental illness — United States. Morb. Mortal. Wkly Rep. (MMWR) Cent. Dis. Control. Prev. 2013;2009–2011:81–87. [Google Scholar]
- Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev. Chronic Dis. 2013;10:E66. doi: 10.5888/pcd10.120239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guydish J, Passalacqua E, Tajima B, Chan M, Chun J, Bostrom A. Smoking prevalence in addiction treatment: a review. Nicotine Tob. Res. 2011;13:401–411. doi: 10.1093/ntr/ntr048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurt RD, Offord KP, Croghan IT, et al. Mortality following inpatient addictions treatment: role of tobacco use in a community-based cohort. JAMA. 1996;275:1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- Keenan PS. Smoking and weight change after new health diagnoses in older adults. Arch. Intern. Med. 2009;169:237–242. doi: 10.1001/archinternmed.2008.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBresh KA, Fonarow GC, Smith SC, Jr., Bonow RO, Smaha LC, Tyler PA, Hong Y, Albright D, Ellrodt AG, Get With The Guidelines Steering, C. Improved treatment of hospitalized coronary artery disease patients with the get with the guidelines program. Crit. Pathw. Cardiol. 2007;6:98–105. doi: 10.1097/HPC.0b013e31812da7ed. [DOI] [PubMed] [Google Scholar]
- Leifheit-Limson EC, Spertus JA, Reid KJ, Jones SB, Vaccarino V, Krumholz HM, Lichtman JH. Prevalence of traditional cardiac risk factors and secondary prevention among patients hospitalized for acute myocardial infarction (AMI): variation by age, sex, and race. J. Women's Health. 2013;22:659–666. doi: 10.1089/jwh.2012.3962. [DOI] [PubMed] [Google Scholar]
- Patel K, Schlundt D, Larson C, Wang H, Brown A, Hargreaves M. Chronic illness and smoking cessation. Nicotine Tob. Res. 2009;11:933–939. doi: 10.1093/ntr/ntp088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleis J, Benson V, Schiller J. Summary health statistics for U.S. adults: National Health Interview Survey, 2000. Vital Health Stat. 2003 [PubMed] [Google Scholar]
- Pleis J, Lethbridge-Çejku M. Summary health statistics for U.S. adults: National Health Interview Survey, 2005. Vital Health Stat. 2006;10 [PubMed] [Google Scholar]
- Schiller J, Lucas J, Ward B, Peregoy J. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat. 2012;10 [PubMed] [Google Scholar]
- Schroeder SA, Morris CD. Confronting a neglected epidemic: tobacco cessation for persons with mental illnesses and substance abuse problems. Annu. Rev. Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. 291p following 314. [DOI] [PubMed] [Google Scholar]
- Sobell MB. Alcohol and tobacco: clinical and treatment issues. Alcohol. Clin. Exp. Res. 2002;26:1954–1955. doi: 10.1097/01.ALC.0000041008.52475.C5. [DOI] [PubMed] [Google Scholar]
- Sochor O, Lennon RJ, Rodriguez-Escudero JP, Bresnahan JF, Croghan I, Somers VK, Lopez-Jimenez F, Pack Q, Thomas RJ. Trends and predictors of smoking cessation after percutaneous coronary intervention (from Olmsted County, Minnesota, 1999 to 2010). Am. J. Cardiol. 2015;115:405–410. doi: 10.1016/j.amjcard.2014.11.020. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results From the 2006 National Survey on Drug Use and Health: National Findings Series H-32. Office of Applied Studies; Rockville, MD: 2007. NSDUH. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results From the 2012 National Survey on Drug Use and Health: Summary of the National Findings. Rockville, MD: 2013. NSDUH Series H-46 NSDUH. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . In: Results From the 2013 National Survey on Drug Use and Health: Summary of National Findings. NSDUH, editor. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. Series H-48. [Google Scholar]
- U.S. Department of Health and Human Services . The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health. Atlanta, GA: 2014. [Google Scholar]
- Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev. Chronic Dis. 2014;11:E62. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.