Abstract
Parkinson's disease (PD) is a chronic and complex neurodegenerative disorder resulting in a mixture of motor and nonmotor symptoms. Psychosis develops in around 60% of PD patients during and can be one of the most challenging nonmotor symptoms. PD psychosis is considered the single greatest precipitant for nursing home placement. PD psychosis is an independent predictor of increased mortality, and there is no ‘ideal’ or universal treatment strategy. The treatment approach to PD psychosis should be tailored and individualized for each patient. In this review, we will discuss PD psychosis and provide practical treatment considerations for neurologists, psychiatrists and other healthcare professionals. We stress the importance of real-time communication between members of the healthcare team.
KEYWORDS : antipsychotics, hallucinations, parkinsonism, pimavanserin, psychosis
Practice points.
Up to 60% of Parkinson's disease (PD) patients will develop psychosis at some point in the course of their illness.
PD-psychosis (PDP) commonly present as illusions, a false sense of presence, hallucinations or delusions.
The recommended approach to PDP is to identify any possible trigger(s), reduce or stop any non-PD or PD medications, and if symptoms still persist, try antipsychotics.
Communicating in real-time between a neurologist, psychiatrist and other health care professionals caring for a PD patient with psychosis is important to achieve the best outcome.
Clozapine is currently considered the most efficacious drug for the treatment of psychosis in PD; however, the monitoring and risk of side effects seems to have limited its widespread use.
Quetiapine is commonly used due to a low reported incidence of side effects and the possible benefit in improving sleep, though many studies have shown no benefit in treatment of PD psychosis.
Pimavanserin, a 5-HT2A receptor inverse agonist may possibly provide a new and different pharmacologic approach to PDP, however, at the current time it is not approved for use in the USA.
Background
Parkinson's disease (PD) is a common neurodegenerative disorder affecting an estimated 6 million people worldwide. Population studies have revealed a rising rate of PD prevalence with age, from 428 per 100,000 in persons 60–69 years to 1087 per 100,000 in those 70–79 years [1]. As the population ages and life expectancy increases, the number of affected persons with PD will be expected to increase to 9 million by 2030 [2].
PD can be described as a complicated neurological disorder, where different neurotransmitters (e.g., dopamine, serotonin, acetylcholine) and basal ganglia circuits (e.g., motor, limbic) are altered, resulting in a mixture of motor and nonmotor symptoms [3,4]. The classical motor symptoms include bradykinesia, rigidity and rest tremor, with postural instability often occurring in later stages of the disease [5]. Nonmotor symptoms include cognitive impairment, psychiatric manifestations, autonomic dysfunction (e.g., orthostatic hypotension, gastrointestinal, urogenital), sleep disorders, and other symptoms such as fatigue and pain [6].
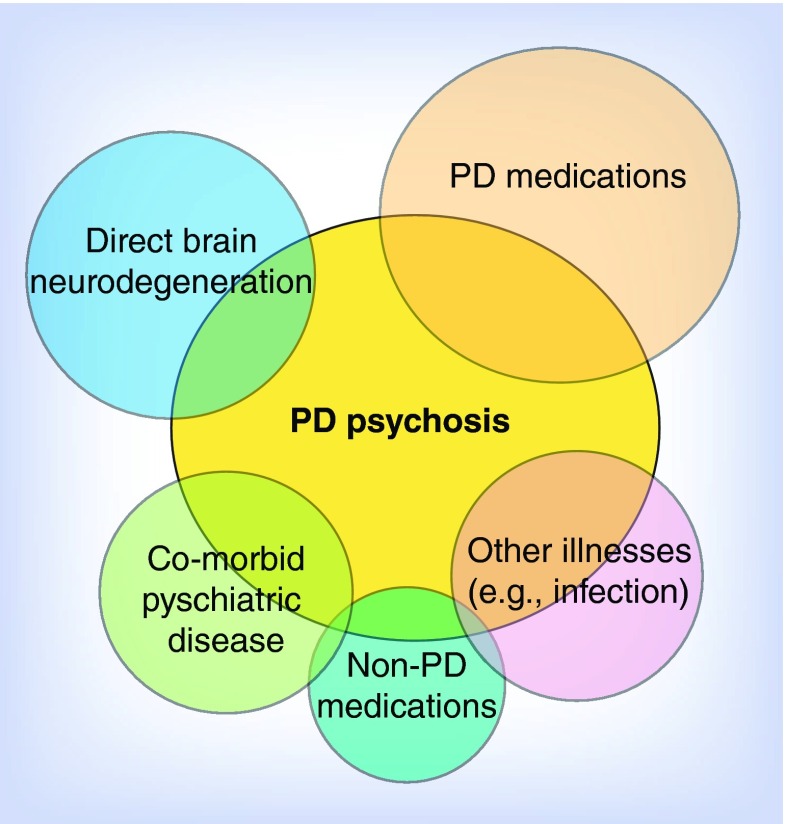
Psychiatric symptoms, such as depression, anxiety, apathy, impulse control disorders or psychosis can present early in the course of the illness and progress to become a clinical challenge at more advanced stages [7,8]. These symptoms may be related to the disease progression itself, to PD dopaminergic or nondopaminergic therapy, or related to nonmotor fluctuations [9]. However, it is difficult to relate psychosis to a specific cause. A combination of all possible triggers is probably occurring altogether (Figure 1). In this perspective article, we will focus our discussion on the psychotic symptoms that can present in PD, how psychosis is currently managed and what we can expect for near future management. We will offer tips for treatment for neurologists, psychiatrists and other health care professionals, and we stress the importance of real-time communication.
Figure 1. . Possible triggers of psychosis in Parkinson's disease.
PD: Parkinson's disease.
Definition, risk factors & clinical course of psychosis
PD-psychosis (PDP) is defined as the presence of at least one of the following: illusions, false sense of presence, hallucinations or delusions; that occurred after PD onset; have been recurrent or continuous for 1 month; and are not more reasonably accounted for by another cause [10]. In clinical practice, anticipating patients who will develop psychosis is a challenge. Clinical characteristics that have been reported as risk factors for developing psychosis in PD include: other medical conditions (e.g., infections, dehydration, metabolic causes), long-term dopaminergic therapy, longer disease duration and development of cognitive impairment, specifically executive dysfunctions. Memory deficits and frontal lobe atrophy have been associated with hallucinations [11]. Genetic factors should also be considered as an associated risk factor for developing psychosis in PD. Recently, genetic polymorphisms (e.g., cholecystokinin system) have shown a significant association with the presence of hallucinations [12] and PD patients with glucocerebrosidase gene mutations have been shown to develop psychosis earlier than patients without mutations [13]. Premorbid psychiatric symptoms and/or neuropsychological symptoms such as vivid dreams [14] and anxiety [15] also have been associated with development of psychosis. A recent neuropsychological PD study showed that hallucinations with loss of insight were associated with impairment in cognitive tasks localized to posterior cortical dysfunction (e.g., clock copying), suggesting a progression from frontal (executive functions) to posterior (visual associative functions) cortical areas as psychosis progresses [16].
PDP follows a progressive evolution presenting with hallucinations, illusions and finally developing hallucinations without insight and/or delusions. Table 1 summarizes the psychiatric syndromes encountered in PD. Hallucinations are the most common manifestation, observed in up to 70% of patients after 20 years of diagnosis [17]. They are defined as false sensory perceptions without the presence of a physical stimulus. These hallucinations can be classified as: false sense of presence, passage, visual and nonvisual hallucinations. False sense of presence (FP) is the vivid sensation that a person is present nearby, and is usually experienced to be beside and/or behind the patient. FP is sometimes referred as a social or an extracampine hallucination [18]. Passage hallucinations consist of a brief sensation of movement (person or animal) in the periphery or passing sideways [19]. FP and passage are sometimes referred to as ‘minor’ phenomena, and were recently reported as a prodromal symptom in 33% of ‘de novo’ PD patients [20]. Visual hallucinations have been described as well-formed images taking the form of people, animals or objects. The images tend to be friendly and familiar, appear briefly, are nonthreatening, and mostly occur in dim lighting conditions [21]. Most patients report to retain insight initially. Nonvisual hallucinations, such as auditory, sensory, tactile, olfactory and gustatory, may emerge over time, occur less frequently and less likely in isolation [22]. Early visual hallucinations and nonvisual hallucinations may suggest another parkinsonian syndrome such as Lewy body dementia or another co-morbid neurological condition [23].
Table 1. . Common psychiatric syndromes reported in Parkinson's disease.
| Type | Syndrome |
|---|---|
| Hallucinations (with or without insight) | False sense of presence |
| Passage hallucination | |
| Visual | |
| Auditory | |
| Tactile | |
| Olfactory | |
| |
Gustatory |
| Illusions |
Optical |
| Delusions | Paranoid: spouse infidelity, abandonment, stealing, persecutory, fear of being injured or poisoned |
| Grandiose | |
| Somatic | |
| Religious | |
| Delusional misidentification syndrome: | |
| – Capgras syndrome | |
| – Fregoli syndrome | |
| – Cotards syndrome | |
| – Ekbom syndrome | |
| – Diogenes syndrome | |
| – Intermetamorphosis | |
| – Subjective doubles | |
| – Misidentification of mirror image | |
| – Misidentification of television | |
| – Phantom boarder syndrome | |
| – Reduplicative paramnesia | |
| – Delusional hermaphroditism | |
| – Nurturing syndrome | |
| – Olfactory reference syndrome |
Illusions are defined as a misperception of real external stimuli, a mismatch between the objective and perceived properties of an object present in the environment. Illusions can present in up to 60% of PD patients with patients having reported a variety of objects such as a dark stain on the floor instead of areal insect or seeing animals or persons instead of trees or a coat rack [17,24].
Delusions are false beliefs that are maintained despite evidence to the contrary and have been reported in around 5–10% of PD patients [10]. Paranoid delusions are the most common type of delusions, consisting of spouse infidelity, abandonment or stealing. Other types, such as persecutory, fear of being injured, poisoned, grandiose, somatic and religious, can also occur. These psychotic symptoms develop when an initially retained insight is compromised and are often associated with cognitive impairment. Delusions are more challenging for the patient and caregiver, carrying a high risk of injury, hospitalization and suicide. A more severe type of delusion has been referred to as the delusional misidentification syndromes (DMS), which are phenomena characterized by the misidentification or reduplication of persons, places, objects or events. DMS have been reported in around 17% of PD patients with dementia [25]. Some of the reported DMS have been briefly described. Capgras syndrome is the belief that an identical appearing impostor has replaced a family member or friend. In Fregoli syndrome, a sufferer believes that a familiar person is able to disguise himself or herself into a stranger. Cotards syndrome is the belief that the person does not exist or that the person is dead. Ekbom syndrome is the belief of being infected by a parasite. In Diogenes syndrome there is a severe self-neglect with domestic squalor and social withdrawal [26,27]. Other more rare DMS are intermetamorphosis (belief that others have been transformed both physically and psychologically into another person), subjective doubles or Doppelganger syndrome (belief that he or she has a double), misidentification of mirror image (belief that one's reflection in the mirror is another person), phantom boarder syndrome (a belief that strangers are living in the patient's house), reduplicative paramnesia (belief that oneself has been replaced into an identical or near identical duplicated place), nurturing syndrome (belief their significant other's existence despite a considerable passage of time after their deaths) and an olfactory reference syndrome (excessive, irrational fear that one is emitting a foul unpleasant odor).
Epidemiological background
The estimated prevalence of PDP ranges from 4 to 45 per 1000 patients, meaning that up to 45,000 PD patients in the USA have developed psychotic symptoms. The incidence rate of PDP was reported as 79.7 per 1000 person-years, with symptoms occurring in up to 60% of PD patients at some point in the course of their illness [28]. Furthermore, PDP is considered a risk factor for hospitalization and the single greatest precipitant for nursing home placement [29]. In population studies, PDP also has been reported as an independent predictor of increased morbidity and mortality [30]. Since PDP has a negative impact on patients and caregivers, early identification and management of psychiatric symptoms is crucial to maintain a good quality of life [31]. The main problem in the management of PDP has been the lack of an ‘ideal’ medication for PDP, an effective and safe therapy targeting the psychosis while not worsening motor symptoms of PD. Here, we summarize the current approach with the available treatment options.
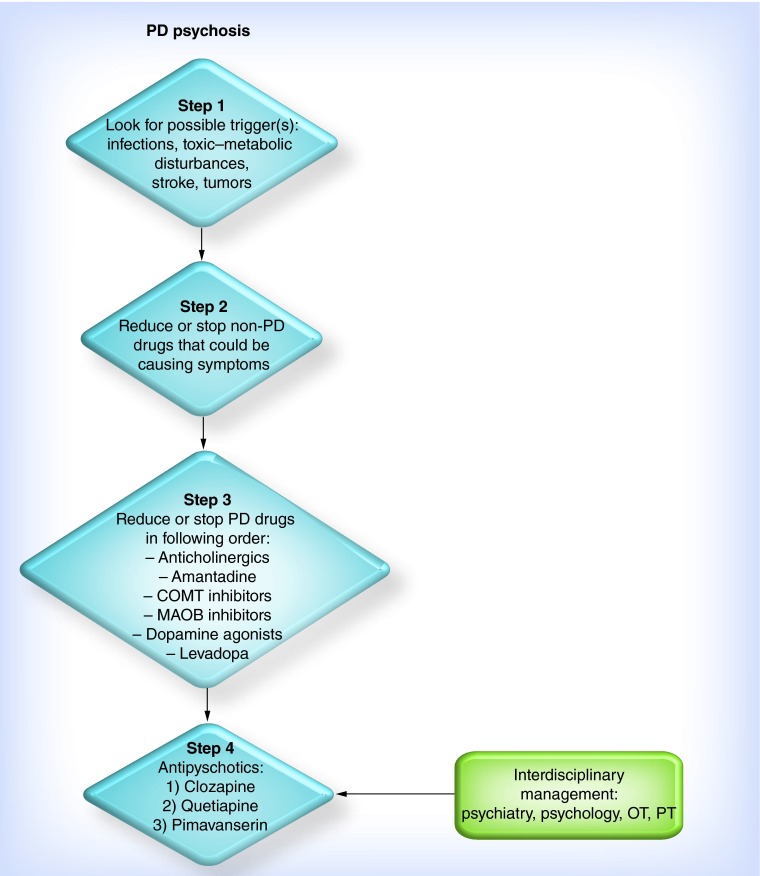
Current expert approach
The approach of psychosis in PD is similar to that of a patient in delirium [32]. The first step is to identify any possible trigger(s). We should rule out any possible source of infections (e.g., pulmonary, urinary), toxic-metabolic disturbances (e.g., electrolytes and TSH, among others), stroke or tumors. The second step is to look at patient's current non-PD drugs for possible drug-induced side effects and try to reduce or stop any of these medications, such as phenylpropanolamine, ephedrine, benzodiazepines, narcotics, digoxine, β-blockers, steroids, cimetidine, ranitidine, sildenafil and clarithromycin. In addition, there should be appropriate consideration of any recreational drug intoxications including LSD, cocaine, amphetamines and withdrawal syndrome such as can be seen with alcohol. Since PD drugs could be exacerbating or directly causing psychosis in PD patients, the third step would be to reduce or stop any of these drugs. A recommended approach is to start eliminating drugs with less potential for clinical (motor) benefit, such as anticholinergics, amantadine, MAO-B inhibitors, and then, if symptoms persist, even dopamine agonists and COMT inhibitors. Most experts will leave levodopa as the last drug and if a patient persists with psychosis changes in doses and intervals may be appropriate but may impact PD symptoms. This point of management is challenging and requires considerable expertise and close follow-up. A rare adverse effect from abrupt discontinuation of dopaminergic agents may be the development of neuroleptic malignant syndrome [33]. Most experts will also check for lingering infection (urinary or other) and treat aggressively if discovered, as this could impact psychosis outcome by prolonging symptoms. The trickiness in management of psychosis in PD is to achieve reduction of psychosis without worsening parkinsonism. If PD symptoms persist after all of the above strategies, antipsychotics could be carefully added. Figure 2 summarizes a general approach to PDP, though most experts will concede that there is no standardized approach or guideline. It is very important that an individual patient not be caught in the middle between a neurologist, a psychiatrist and other health care professionals. It is not uncommon in treatment for each specialty to make changes in a drug regimen without communicating in real-time with the other physician's participating in the care of the patient. This can lead to negative consequences for an individual patient, and therefore we stress that communication between multiple health care providers is critical to achieve a successful treatment outcome.
Figure 2. . One recommended approach to the management of Parkinson's disease psychosis.
OT: Occupational therapy; PD: Parkinson's disease; PT: Physical therapy.
Pathophysiology of PDP
Psychosis in PD was initially thought to be related only to the chronic use of dopaminergic or nondopaminergic drugs [34]. The influence was thought to be a result of limbic system dysfunction associated to an overstimulation of mesolimbic dopamine receptors. While studies have highlighted the contribution of long-term use of these agents as triggers or worsening psychosis, other mechanisms seem to contribute. Follow-up studies failed to find a clear association with levodopa dose and occurrence of hallucinations [35]. Structural imaging studies on PD patients with visual hallucinations have reported gray matter atrophy in the primary visual cortex, visual association cortex, limbic regions and cholinergic structures, where functional imaging studies have reported alterations in both dorsal and ventral visual pathways [36]. Studies have also suggested a marked desynchronization occurring between anterior and posterior cortical areas involved in visual processing during a visual hallucination [37]. Recent evidence has shown that serotonin also contributes to the pathogenesis of hallucinations. A functional imaging study reported abnormalities in the serotonin 2A receptor neurotransmission of PD patients with hallucinations [38]. Therefore the evidence collectively shows that the pathogenesis of psychosis in PD may be influenced by an interaction of multiple intrinsic and extrinsic factors.
Clinical evidence
First-generation antipsychotics were primarily post-synaptic antagonists of the dopamine type 2 (D2) receptor. Because of the predilection for post-synaptic dopamine blockade, the higher potency first-generation antipsychotics had significant risk of extrapyramidal effects such as parkinsonism and dystonic reactions. These agents have been supplanted by second-generation or atypical antipsychotics. The two most commonly used atypical antipsychotics for the treatment of PDP are clozapine and quetiapine. Mechanisms of action and randomized controlled trials of the antipsychotics studied for use in PDP are reviewed here. Clozapine is a dibenzodiazepine antipsychotic with its therapeutic efficacy thought to be mediated primarily through antagonism of D2 receptors and serotonin type 2A (5-HT2A) receptors. Clozapine also act as an antagonist of adrenergic (alpha1A, alpha 2A), histamine type 1 (H1), cholinergic (M1), and other dopaminergic (D1, D2, D3, D5) and serotonergic receptors (5-HT1A, 5-HT2C, 5-HT3, 5-HT6, 5-HT7).
The first major trial with clozapine was a small placebo-controlled double-blind study that evaluated the effects on neuropsychiatric symptoms that were induced by dopaminergic therapy [39]. Of the four PD patients who initially presented with psychosis (hallucinations, delusions and thought disorder), two showed improvement of symptoms (SAPS and BPRS) at a mean dose 137.5 mg/d, but were withdrawn prematurely due to delirium and somnolence. The other two showed worsening of psychosis at a mean dose of 250 mg/d. The authors concluded that clozapine's propensity to induce delirium and somnolence at high doses could have overshadowed the clinical benefits and recommended a target dose between 25 and 50 mg per day.
The Parkinson Study Group conducted the PSYCLOPS study. This was a multicenter, placebo-controlled, double-blind trial of clozapine for drug-induced psychosis (hallucinations or delusions) in 60 PD patients [40]. At the end of the 4-week trial, all measures of psychosis significantly improved compared with placebo (BPRS, CGIS, SAPS) with no worsening of motor symptoms in either group. In the clozapine group, the mean daily dose was 24.7 mg (range: 6.25–50 mg) and three withdrew due to leukopenia, myocardial infarction and sedation. The authors summarized their findings that clozapine at low doses reduced the severity of drug-induced psychosis in PD patients. A significant beneficial effect on tremor was also observed. Leukopenia developed in one patient, but resolved after discontinuing medication. There was also a significant gain in weight observed. The benefit of clozapine was maintained without worsening of PD motor features in the open-label extension study [41].
Following publication of that paper, the French Clozapine Parkinson Study Group reported a trial with similar study design (4-week, multicenter, placebo-controlled, double-blind, n = 60) [42]. Significant changes on psychiatric measurements (CGI and PANSS) were observed from the first week of therapy. At the end of the study, similar results to the Parkinson Study Group trial were observed. The mean daily dose of clozapine was 36 mg, seven of 32 patients on clozapine reported worsening of parkinsonism without the necessity of discontinuing treatment, and no cases of agranulocytosis were reported. These results were maintained during the open-label follow-up study [43].
After clozapine's proven efficacy on placebo-controlled trials several small comparative trials against other PDP drugs were published. Risperidone is a benzisoxazole atypical antipsychotic also with mixed strong antagonist activity on 5-HT2A and D2 receptors. Risperidone along with other agents in the family of ‘dones’ has weaker affinity to other serotonin and dopamine receptors than the family of ‘pines’ such as clozapine or olanzapine. The efficacy and safety of risperidone was compared with clozapine for the treatment of levodopa-induced psychosis in a 12-week, double-blind trial of ten PD patients [44]. The improvements observed on a psychosis measurement (BPRS) were not significant between groups. The mean clozapine daily dose was 62.5 mg (range: 25–100 mg per day). One subject on clozapine terminated the study early due to leukopenia, which resolved after stopping treatment and worsening of parkinsonism was observed in the risperidone group.
Olanzapine is a second-generation thienobenzodiazepine atypical antipsychotic with potent antagonism on serotonin (5-HT2A and 5-HT2C), dopamine (D1–4), histamine (H1) and adrenergic (alpha1) receptors, and moderate to weak affinity to 5-HT3, cholinergic (M1–5), GABAergic, BZD and β-adrenergic receptors. Olanzapine was compared with clozapine in a 2-month, double-blind trial in 15 hallucinating PD patients [45]. Patients on clozapine showed significant improvement on SAPS and BPRS scores from baseline. The mean clozapine daily dose was 25.8 mg. Deterioration of motor symptoms was observed in six of seven patients on olanzapine.
Quetiapine is a dibenzothiazepine atypical antipsychotic with activity similar to clozapine, and mediated through antagonism of D2 receptors and serotonin type 2 (5-HT2) receptors. It also has binding affinity to other serotonin (5-HT1A), dopamine (D1), histamine (H1) and adrenergic (alpha 1, alpha 2) receptors. After the promising results of open label studies, quetiapine gained popularity. There were, however, two comparative and five placebo-controlled randomized trials published in a period of 7 years, and most had disappointing findings.
The first randomized trial compared quetiapine and clozapine in a 12-week open-label, blinded-rater study, which included 23 PD patients with dopaminergic-induced psychosis [46]. The preliminary results revealed significant improvements (25–30%) on the psychosis measurements (BPRS and CGI) in both groups. Worsening of UPDRS III was significant only in the clozapine group. Mild improvements in dyskinesias were also observed in both groups. In their final report, which included 45 patients, the results remained positive and authors concluded that quetiapine might be an effective and well-tolerated drug in PD patients with psychosis [47]. In a second comparative randomized trial, 27 PD patients with psychosis were studied in a randomized, blinded-rater, 22-week trial [48]. While the clozapine group reported a significant reduction in hallucinations and delusion scores (NPI), the reduction in scores was not significant in the quetiapine group. Leukopenia was observed in three patients on clozapine, and no worsening of parkinsonian symptoms was observed in any of the arms.
The first placebo-controlled study included 31 PD patients with visual hallucinations while on dopaminergics and they were studied in a double-blind 12-week trial [49]. Improvements on the Baylor PD Hallucination Questionnaire and the BPRS were not significant compared with placebo. The medication was generally well-tolerated with no reported changes of PD motor symptoms. The authors reported that quetiapine at doses up to 200 mg/day failed to suppress hallucinations.
The second study reported a 3-month, double-blind trial evaluating 58 PD patients with severe visual or auditory hallucinations and/or delusions, all of which significantly affected quality of life [50]. No significant changes were observed on the BPRS, CGIS and UPDRS part III in either group. 26 patients required termination of treatment with quetiapine or placebo due to a lack of response. The trial showed no beneficial effect of quetiapine for psychosis.
The third placebo-controlled trial was a multicenter double-blind study assessing the effects and tolerability of quetiapine and donepezil (cholinesterase inhibitor), alone or in combination, for psychosis or agitation in patients with both dementia and parkinsonism [51]. Only nine patients had PD with dementia, 23 had dementia with Lewy bodies, and eight had Alzheimer disease. No significant changes were reported in the BPRS at 10 weeks of therapy and quetiapine was well tolerated.
A 12-week, randomized, placebo-controlled, double-blind trial of 24 PD patients with hallucinations or delusions assessed quetiapine's efficacy and indirectly by measuring the time remaining in the trial as primary outcome [52]. The differences in dropout times were not significant between groups. Since only 1/3 of patients completed the trial, secondary outcomes were analyzed at 6 weeks with no significant differences in the Baylor PD hallucination scale, NPI, BPRS and UPDRS between groups. Again, quetiapine did not show significant improvement on psychosis compared with placebo.
The last double-blind, placebo-controlled trial investigated the effects of quetiapine on sleep architecture and hallucinations in PD patients [53]. Sixteen patients experiencing visual hallucinations were included. No significant differences were observed on sleep architecture and total BPRS between arms. However, the mean improvement on the hallucination item of the BPRS and on the CGIS was significantly better in the quetiapine arm and there was not worsening parkinsonism. Five terminated the study early due to lack of efficacy, drowsiness and loss to follow-up. This was the only study that had clearly positive results for quetiapine.
Clozapine is currently considered the most efficacious drug for the treatment of psychosis in PD [54]. However, the need for continuous blood count monitoring due to the risk of severe neutropenia has limited its use. The evidence has been insufficient to conclude that quetiapine suppresses PD psychosis, however, larger well-designed trials are needed before confirming its inefficacy. In the meantime, because of quetiapine's low reported incidence of side effects and the potential to improve sleep, the use of this atypical antipsychotic has become part of routine use.
From our group's 8-year clinical experience using clozapine for PDP, we observed that 66% of the 36 patients (32 PD and 4 atypical PD) reported complete or partial clinical benefit [55]. The most common reason for discontinuation of clozapine was frequent blood testing (28%), nursing home placement (16%) and neutropenia (8%), which resolved after stopping therapy. Our results highlights the challenges associated with clozapine in PDP patients.
Other antipsychotics, such as aripirapzole, a quinolinone atypical antipsychotic with partial agonist activity on D2 and 5-HT1A, and antagonist at 5-HT2A receptors, or melperone, a butyrophenone atypical antipsychotic with low activity on D2 receptors, have been to date in general ineffective in reducing psychotic symptoms and the worry is that these agents may worsen PD motor symptoms [56,57]. Ziprasidone is a next generation benzylisothiazolylpiperazine atypical antipsychotic with antagonist activity at D2, 5-HT2A, 5-HT1D, agonist at 5-HT1A, and moderate inhibition to serotonin and norepinephrine reuptake. Ziprasidone was studied in a 4-week, randomized, single-blind, open-label comparative trial with clozapine in 16 PD patients with psychotic symptoms. Psychotic symptoms were significantly reduced in both groups, without worsening of motor symptoms. The results suggest a beneficial effect, however, better clinical trials will be necessary before recommending its use and understanding whether it will worsen PD motor symptoms [58].
Should clinicians be doing more to address PDP?
In the following paragraphs, we will discuss three controversial aspects regarding the management of psychosis in PD patients in addition to the approach discussed above. A risk-benefit approach is required for this population given that management with antipsychotics may have adverse effects. A recent study reported increased mortality in elderly PD patients with dementia managed with antipsychotic medication, however, this analysis did not compare the risk and outcomes of PDP patients who were not treated with antipsychotics [59].
Clinicians should identify PD patients that will most likely develop psychosis. We have learned from previous studies that there are important clinical characteristics that may place patients at risk for development of PDP: older age, disease severity, cognitive impairment or dementia, high doses of dopaminergics, longer disease duration, sleep disturbances, such as REM behavioral sleep disorder (RBD), and visual processing deficits. Imaging, physiological and neuropsychological studies have suggested common neurobiological processes leading to RBD, hallucinations and cognitive impairment. PD patients with the presence of RBD or psychosis will possibly progress to dementia [60]. As mentioned earlier, neuropsychological traits such as anxiety or executive functioning or verbal fluency impairment have been also associated with development of psychosis. Identifying this potentially more aggressive subtype of PD (one that may progress to psychosis) early in the course of the illness will help the clinician provide a better approach for PDP. We as clinicians need an accurate current and premorbid neuropsychiatric assessment including caregiver's point of view. This information is essential for the clinician to identify and treat this population. Clinicians are advised to remain vigilant in asking both patients and caregivers about possible psychotic symptoms;
Should we treat ‘minor’ psychotic symptoms? Historically many neurologists have withheld treatment with antipsychotics until the symptoms affect a patient's quality of life or become troublesome after attempting the initial strategies described above. Psychiatric symptoms in PD usually begin in milder forms and progress to more complex hallucinations and/or delusions [61]. Should we treat the ‘minor’ phenomena or benign hallucinations as soon as detected? All the randomized controlled trials described above included patients with hallucinations or delusions affecting patient's quality of life. Many experts ask the question, why wait until these symptoms progress to ‘major’ hallucinations or delusions? Recently, a longitudinal observational study of 64 patients showed that treatment of benign hallucinations strongly reduced progression to more complex hallucinations compared with those who did not receive antipsychotic medication [62], supporting the use of antipsychotics for the treatment of hallucinations with retained insight. However, there is no evidence regarding the treatment of ‘minor’ hallucinations and how this could affect their progression;
Does clozapine-phobia exist? Clozapine is not a first-line antipsychotic considered for PDP due to its well-known serious adverse effects, such as neutropenia, sedation, hypotension, bradycardia, seizure, and possible myocarditis and cardiomyopathy. How often do these issues clinically present? Is it better to withhold the most efficacious drugs instead of closely monitoring these drugs’ side effects? In a retrospective study of 35 PDP patients, the mean serum concentration of clozapine was much lower in PD patients than the mean concentration reported in schizophrenic patients (77.9 vs 350–600 ng/ml) with no serious adverse events were documented related to clozapine [63]. Are frequent blood tests or the side effect profile the main barrier for a clozapine prescription? Studies have shown that agranulocytosis usually improves if monitored appropriately and there is prompt discontinuation if encountered. The frequency of agranulocytosis decreased from 1 to 2% to less than 0.4% after close monitoring guidelines were implemented [64]. The US FDA has been addressing safety concerns and current knowledge about severe neutropenia [65]. Current recommendations for monitoring vary according to the patient's absolute neutrophil count level and the highest risk of neutropenia is in the initial 18 weeks of therapy. Prescribers are required to register in the Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program. Strengthening safety measures when prescribing clozapine will help clinicians to make treatment decisions. This recently introduced registry centralizes previous monitoring efforts across all drug manufacturers and providers. There is a risk-benefit to any atypical in the elderly population due to the FDA black box warning regarding increased risk of mortality.
Future perspective
New pharmacologic and nonpharmacologic therapies have been recently studied in PDP. The 5-HT2A receptor inverse agonists are a group of drugs that have shown reasonable clinical benefits in initial studies without the same level of reported side effects encountered with typical and atypical antipsychotics. Two randomized controlled trials have reported that pimavanserin, a 5-HT2A receptor inverse agonist, was effective in reducing psychotic symptoms in PD without worsening parkinsonism [66,67]. A recent meta-analysis of four randomized controlled trials of this 5-HT2A confirmed the potential for this approach [68]. Pimavanserin is a promising drug approach and is currently under FDA review, but is not currently approved for use. Pimavanserin recently showed a greater therapeutic window when compared with quetiapine and clozapine in animal models of PDP [69]. If this approach becomes available for PDP, it will be interesting to see if the efficacy exceeds that of quetiapine, and if in some cases it may allow patients to avoid the monitoring necessary for clozapine. So far, studies suggest that this new drug will be more effective than quetiapine.
Cholinergic dysfunction is common in PD. Drugs used for dementia, such as cholinesterase inhibitors, are also a promising therapy for psychosis in those PD patients with dementia. There are some studies suggesting that there is mild evidence of improvement of psychotic features from rivastigmine studies, but the effects seem to be mild and similar to quetiapine [70]. Other pharmacological approaches such as memantine (NMDA antagonist), ondansetron (5-HT3 antagonist), and even some antidepressants (citalopram) for those with concomitant psychosis and depression may be used for the treatment of PD psychosis, and there are some published findings in small trials [71], but these will need to be studied in larger trials.
• Nonpharmacological approaches to PDP
Recent small retrospective and open-label studies have revealed significant improvements on psychiatric measurements and short-term improvements on motor symptoms of PD with the use of Electroconvulsive Therapy for PDP [72–74]. Although it could be used as a last resource, larger prospective clinical trials will be needed to confirm these results before widely recommending this therapy for cases of PDP. There are several anecdotal observations from expert groups for the use of Electroconvulsive Therapy in very severe PDP cases where all pharmacological approaches have failed.
Psychotherapeutic treatments (e.g., comprehensive behavioral intervention therapy) and educational approaches have been emerging as potential adjunctive methods for the treatment of PD psychosis. Although studies have not confirmed results, these approaches should not prevent the clinician providing psychosocial care [75,76]. These neuropsychological approaches include educating the patient and caregiver with information on psychiatric symptoms with a special emphasis on training sessions, which focus on medication management and more specific coping strategies (e.g., visual, cognitive and interactive strategies) [77].
Conclusion
The development of psychosis is one of the most challenging symptoms in a subset of patients with PD. PDP is a risk factor for nursing home placement and is a predictor of future mortality. One issue in the treatment of PDP has been the lack of the ‘ideal’ drug, a drug that improves psychosis but does not worsen parkinsonism. Clozapine, the only drug established with clear efficacy in PDP, is underused due to its potential side effects and need for frequent blood testing. In most expert centers utilization of the clozapine registry and monitoring techniques has led to improvements in symptoms even in the most severe cases. Quetiapine and cholinesterase inhibitors may be useful in mild cases though the data support only mild beneficial effects. There is a renewed hope that new 5-HT2A receptor inverse agonists (pimavanserin) and other approaches may be a potential future avenue. Advances in knowledge of the pathophysiology of psychosis will potentially assist in improving the current pharmacologic and nonpharmacologic approaches. It is very important that an individual patient not be caught in the middle between a neurologist, a psychiatrist and other health care professionals. It is not uncommon in treatment for each specialty to make changes in a drug regimen without communicating in real-time with the other physician's participating in the care of the patient. These types of changes without proper communication can lead to negative consequences for an individual patient, and therefore we stress that communication between multiple health care providers will be critical to achieve a successful treatment outcome in PD related psychosis.
Acknowledgements
The authors would like to acknowledge the support of the National Parkinson Foundation, Tyler's Hope and the Bachmann-Strauss Foundation. The authors also acknowledge the UF Foundation and the UF INFORM database.
Footnotes
Financial & competing interests disclosure
D Martinez-Ramirez and MS Jaffee report no disclosures. MS Okun serves as a consultant for the National Parkinson Foundation, and has received research grants from NIH, NPF, the Michael J. Fox Foundation, the Parkinson Alliance, Smallwood Foundation, the Bachmann-Strauss Foundation, the Tourette Syndrome Association, and the UF Foundation. MS Okun has previously received honoraria, but in the past >48 months has received no support from industry. MS Okun has received royalties for publications with Demos, Manson, Amazon, Smashwords and Cambridge (movement disorders books). MS Okun is an associate editor for New England Journal of Medicine Journal Watch Neurology. MS Okun has participated in CME activities on movement disorders (in the last 36 months) sponsored by PeerView, Prime and by Vanderbilt University. The institution and not MS Okun receives grants from Medtronic and ANS/St. Jude, and the PI has no financial interest in these grants. MS Okun has participated as a site PI and/or co-I for several NIH, foundation, and industry sponsored trials over the years but has not received honoraria. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Disclaimer
This manuscript was run through the iThenticate system provided by the University of Florida and the first author takes all responsibility for ensuring originality.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: a systematic review and meta-analysis. Mov. Disord. 2014;29(13):1583–1590. doi: 10.1002/mds.25945. [DOI] [PubMed] [Google Scholar]
- 2.Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68(5):384–386. doi: 10.1212/01.wnl.0000247740.47667.03. [DOI] [PubMed] [Google Scholar]
- 3.Kalia LV, Lang AE. Parkinson's disease. Lancet. 2015;386(9996):896–912. doi: 10.1016/S0140-6736(14)61393-3. [DOI] [PubMed] [Google Scholar]; • An excellent review with cutting-edge approach and management of the motor and nonmotor symptoms in Parkinson's disease (PD).
- 4.Obeso JA, Rodriguez-Oroz MC, Stamelou M, Bhatia KP, Burn DJ. The expanding universe of disorders of the basal ganglia. Lancet. 2014;384(9942):523–531. doi: 10.1016/S0140-6736(13)62418-6. [DOI] [PubMed] [Google Scholar]
- 5.Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson's disease. Mov. Disord. 2015;30(12):1591–1601. doi: 10.1002/mds.26424. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Martin P, Chaudhuri KR, Rojo-Abuin JM, et al. Assessing the non-motor symptoms of Parkinson's disease: MDS-UPDRS and NMS Scale. Eur. J. Neurol. 2015;22(1):37–43. doi: 10.1111/ene.12165. [DOI] [PubMed] [Google Scholar]
- 7.Weintraub D, Burn DJ. Parkinson's disease: the quintessential neuropsychiatric disorder. Mov. Disord. 2011;26(6):1022–1031. doi: 10.1002/mds.23664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alvarado-Bolanos A, Cervantes-Arriaga A, Rodriguez-Violante M, et al. Impact of neuropsychiatric symptoms on the quality of life of subjects with Parkinson's disease. J. Parkinsons Dis. 2015;5(3):541–548. doi: 10.3233/JPD-150597. [DOI] [PubMed] [Google Scholar]
- 9.Todorova A, Jenner P, Ray Chaudhuri K. Non-motor Parkinson's: integral to motor Parkinson's, yet often neglected. Pract. Neurol. 2014;14(5):310–322. doi: 10.1136/practneurol-2013-000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ravina B, Marder K, Fernandez HH, et al. Diagnostic criteria for psychosis in Parkinson's disease: report of an NINDS, NIMH work group. Mov. Disord. 2007;22(8):1061–1068. doi: 10.1002/mds.21382. [DOI] [PubMed] [Google Scholar]; •• Work of considerable interest to review the current clinical criteria for the diagnosis of psychosis in PD.
- 11.Alzahrani H, Venneri A. Cognitive and neuroanatomical correlates of neuropsychiatric symptoms in Parkinson's disease: a systematic review. J. Neurol. Sci. 2015;356(1–2):32–44. doi: 10.1016/j.jns.2015.06.037. [DOI] [PubMed] [Google Scholar]; • Interesting review to better understand the pathophysiology of psychotic symptoms, including hallucinations and delusions.
- 12.Lenka A, Arumugham SS, Christopher R, Pal PK. Genetic substrates of psychosis in patients with Parkinson's disease: a critical review. J. Neurol. Sci. 2016;364:33–41. doi: 10.1016/j.jns.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Oeda T, Umemura A, Mori Y, et al. Impact of glucocerebrosidase mutations on motor and nonmotor complications in Parkinson's disease. Neurobiol. Aging. 2015;36(12):3306–3313. doi: 10.1016/j.neurobiolaging.2015.08.027. [DOI] [PubMed] [Google Scholar]
- 14.Gama RL, De Bruin VM, De Bruin PF, et al. Risk factors for visual hallucinations in patients with Parkinson's disease. Neurol. Res. 2015;37(2):112–116. doi: 10.1179/1743132814Y.0000000418. [DOI] [PubMed] [Google Scholar]
- 15.Gibson G, Mottram PG, Burn DJ, et al. Frequency, prevalence, incidence and risk factors associated with visual hallucinations in a sample of patients with Parkinson's disease: a longitudinal 4-year study. Int. J. Geriatr. Psychiatry. 2013;28(6):626–631. doi: 10.1002/gps.3869. [DOI] [PubMed] [Google Scholar]
- 16.Llebaria G, Pagonabarraga J, Martinez-Corral M, et al. Neuropsychological correlates of mild to severe hallucinations in Parkinson's disease. Mov. Disord. 2010;25(16):2785–2791. doi: 10.1002/mds.23411. [DOI] [PubMed] [Google Scholar]
- 17.Lee AH, Weintraub D. Psychosis in Parkinson's disease without dementia: common and comorbid with other non-motor symptoms. Mov. Disord. 2012;27(7):858–863. doi: 10.1002/mds.25003. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• A review of clinical comorbidities associated with the development of psychosis in PD which helps characterize this population.
- 18.Fenelon G, Soulas T, Cleret De Langavant L, Trinkler I, Bachoud-Levi AC. Feeling of presence in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry. 2011;82(11):1219–1224. doi: 10.1136/jnnp.2010.234799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fenelon G, Soulas T, Zenasni F, Cleret De Langavant L. The changing face of Parkinson's disease-associated psychosis: a cross-sectional study based on the new NINDS-NIMH criteria. Mov. Disord. 2010;25(6):763–766. doi: 10.1002/mds.22839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pagonabarraga J, Martinez-Horta S, Fernandez De Bobadilla R, et al. Minor hallucinations occur in drug-naive Parkinson's disease patients, even from the premotor phase. Mov. Disord. 2016;31(1):45–52. doi: 10.1002/mds.26432. [DOI] [PubMed] [Google Scholar]
- 21.Muller AJ, Shine JM, Halliday GM, Lewis SJ. Visual hallucinations in Parkinson's disease: theoretical models. Mov. Disord. 2014;29(13):1591–1598. doi: 10.1002/mds.26004. [DOI] [PubMed] [Google Scholar]
- 22.Goetz CG, Stebbins GT, Ouyang B. Visual plus nonvisual hallucinations in Parkinson's disease: development and evolution over 10 years. Mov. Disord. 2011;26(12):2196–2200. doi: 10.1002/mds.23835. [DOI] [PubMed] [Google Scholar]; •• A very interesting publication describing the course of psychosis in PD.
- 23.Burghaus L, Eggers C, Timmermann L, Fink GR, Diederich NJ. Hallucinations in neurodegenerative diseases. CNS Neurosci. Ther. 2012;18(2):149–159. doi: 10.1111/j.1755-5949.2011.00247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Archibald NK, Clarke MP, Mosimann UP, Burn DJ. Visual symptoms in Parkinson's disease and Parkinson's disease dementia. Mov. Disord. 2011;26(13):2387–2395. doi: 10.1002/mds.23891. [DOI] [PubMed] [Google Scholar]
- 25.Pagonabarraga J, Llebaria G, Garcia-Sanchez C, Pascual-Sedano B, Gironell A, Kulisevsky J. A prospective study of delusional misidentification syndromes in Parkinson's disease with dementia. Mov. Disord. 2008;23(3):443–448. doi: 10.1002/mds.21864. [DOI] [PubMed] [Google Scholar]
- 26.Moro A, Munhoz RP, Moscovich M, Arruda WO, Teive HA. Delusional misidentification syndrome and other unusual delusions in advanced Parkinson's disease. Parkinsonism Relat. Disord. 2013;19(8):751–754. doi: 10.1016/j.parkreldis.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 27.Moroy A, Bellivier F, Fenelon G. Olfactory reference syndrome: an unusual delusion in a patient with Parkinson's disease. J. Neuropsychiatry Clin. Neurosci. 2012;24(3):E2. doi: 10.1176/appi.neuropsych.11070163. [DOI] [PubMed] [Google Scholar]
- 28.Forsaa EB, Larsen JP, Wentzel-Larsen T, et al. A 12-year population-based study of psychosis in Parkinson disease. Arch. Neurol. 2010;67(8):996–1001. doi: 10.1001/archneurol.2010.166. [DOI] [PubMed] [Google Scholar]
- 29.Kang GA, Bronstein JM. Psychosis in nursing home patients with Parkinson's disease. J. Am. Med. Dir. Assoc. 2004;5(3):167–173. doi: 10.1097/01.JAM.0000123028.10575.45. [DOI] [PubMed] [Google Scholar]
- 30.Forsaa EB, Larsen JP, Wentzel-Larsen T, Alves G. What predicts mortality in Parkinson disease?: a prospective population-based long-term study. Neurology. 2010;75(14):1270–1276. doi: 10.1212/WNL.0b013e3181f61311. [DOI] [PubMed] [Google Scholar]; • Important article for the clinician to learn factors that increase risk of mortality in PD.
- 31.Skorvanek M, Rosenberger J, Minar M, et al. Relationship between the non-motor items of the MDS-UPDRS and quality of life in patients with Parkinson's disease. J. Neurol. Sci. 2015;353(1–2):87–91. doi: 10.1016/j.jns.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 32.Connolly B, Fox SH. Treatment of cognitive, psychiatric, and affective disorders associated with Parkinson's disease. Neurotherapeutics. 2014;11(1):78–91. doi: 10.1007/s13311-013-0238-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keyser DL, Rodnitzky RL. Neuroleptic malignant syndrome in Parkinson's disease after withdrawal or alteration of dopaminergic therapy. Arch. Intern. Med. 1991;151(4):794–796. [PubMed] [Google Scholar]
- 34.Poewe W. Psychosis in Parkinson's disease. Mov. Disord. 2003;18(Suppl. 6):S80–S87. doi: 10.1002/mds.10567. [DOI] [PubMed] [Google Scholar]
- 35.Williams-Gray CH, Foltynie T, Lewis SJ, Barker RA. Cognitive deficits and psychosis in Parkinson's disease: a review of pathophysiology and therapeutic options. CNS drugs. 2006;20(6):477–505. doi: 10.2165/00023210-200620060-00004. [DOI] [PubMed] [Google Scholar]
- 36.Lenka A, Jhunjhunwala KR, Saini J, Pal PK. Structural and functional neuroimaging in patients with Parkinson's disease and visual hallucinations: a critical review. Parkinsonism Relat. Disord. 2015;21(7):683–691. doi: 10.1016/j.parkreldis.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 37.Goetz CG, Vaughan CL, Goldman JG, Stebbins GT. I finally see what you see: Parkinson's disease visual hallucinations captured with functional neuroimaging. Mov. Disord. 2014;29(1):115–117. doi: 10.1002/mds.25554. [DOI] [PubMed] [Google Scholar]
- 38.Ballanger B, Strafella AP, Van Eimeren T, et al. Serotonin 2A receptors and visual hallucinations in Parkinson disease. Arch. Neurol. 2010;67(4):416–421. doi: 10.1001/archneurol.2010.35. [DOI] [PubMed] [Google Scholar]
- 39.Wolters EC, Hurwitz TA, Mak E, et al. Clozapine in the treatment of parkinsonian patients with dopaminomimetic psychosis. Neurology. 1990;40(5):832–834. doi: 10.1212/wnl.40.5.832. [DOI] [PubMed] [Google Scholar]
- 40.Low-dose clozapine for the treatment of drug-induced psychosis in Parkinson's disease. The Parkinson Study Group. N. Engl. J. Med. 1999;340(10):757–763. doi: 10.1056/NEJM199903113401003. [DOI] [PubMed] [Google Scholar]
- 41.Factor SA, Friedman JH, Lannon MC, Oakes D, Bourgeois K Parkinson Study Group. Clozapine for the treatment of drug-induced psychosis in Parkinson's disease: results of the 12 week open label extension in the PSYCLOPS trial. Mov. Disord. 2001;16(1):135–139. doi: 10.1002/1531-8257(200101)16:1<135::aid-mds1006>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 42.Clozapine in drug-induced psychosis in Parkinson's disease. The French Clozapine Parkinson Study Group. Lancet. 1999;353(9169):2041–2042. [PubMed] [Google Scholar]
- 43.Pollak P, Tison F, Rascol O, et al. Clozapine in drug induced psychosis in Parkinson's disease: a randomised, placebo controlled study with open follow up. J. Neurol. Neurosurg. Psychiatry. 2004;75(5):689–695. doi: 10.1136/jnnp.2003.029868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ellis T, Cudkowicz ME, Sexton PM, Growdon JH. Clozapine and risperidone treatment of psychosis in Parkinson's disease. J. Neuropsychiatry Clin. Neurosci. 2000;12(3):364–369. doi: 10.1176/jnp.12.3.364. [DOI] [PubMed] [Google Scholar]
- 45.Goetz CG, Blasucci LM, Leurgans S, Pappert EJ. Olanzapine and clozapine: comparative effects on motor function in hallucinating PD patients. Neurology. 2000;55(6):789–794. doi: 10.1212/wnl.55.6.789. [DOI] [PubMed] [Google Scholar]
- 46.Morgante L, Epifanio A, Spina E, et al. Quetiapine versus clozapine: a preliminary report of comparative effects on dopaminergic psychosis in patients with Parkinson's disease. Neurol. Sci. 2002;23(Suppl. 2):S89–S90. doi: 10.1007/s100720200084. [DOI] [PubMed] [Google Scholar]
- 47.Morgante L, Epifanio A, Spina E, et al. Quetiapine and clozapine in parkinsonian patients with dopaminergic psychosis. Clin. Neuropharmacol. 2004;27(4):153–156. doi: 10.1097/01.wnf.0000136891.17006.ec. [DOI] [PubMed] [Google Scholar]
- 48.Merims D, Balas M, Peretz C, Shabtai H, Giladi N. Rater-blinded, prospective comparison: quetiapine versus clozapine for Parkinson's disease psychosis. Clin. Neuropharmacol. 2006;29(6):331–337. doi: 10.1097/01.WNF.0000236769.31279.19. [DOI] [PubMed] [Google Scholar]
- 49.Ondo WG, Tintner R, Voung KD, Lai D, Ringholz G. Double-blind, placebo-controlled, unforced titration parallel trial of quetiapine for dopaminergic-induced hallucinations in Parkinson's disease. Mov. Disord. 2005;20(8):958–963. doi: 10.1002/mds.20474. [DOI] [PubMed] [Google Scholar]
- 50.Rabey JM, Prokhorov T, Miniovitz A, Dobronevsky E, Klein C. Effect of quetiapine in psychotic Parkinson's disease patients: a double-blind labeled study of 3 months’ duration. Mov. Disord. 2007;22(3):313–318. doi: 10.1002/mds.21116. [DOI] [PubMed] [Google Scholar]
- 51.Kurlan R, Cummings J, Raman R, Thal L Alzheimer's Disease Cooperative Study Group. Quetiapine for agitation or psychosis in patients with dementia and parkinsonism. Neurology. 2007;68(17):1356–1363. doi: 10.1212/01.wnl.0000260060.60870.89. [DOI] [PubMed] [Google Scholar]
- 52.Shotbolt P, Samuel M, Fox C, David AS. A randomized controlled trial of quetiapine for psychosis in Parkinson's disease. Neuropsychiatr. Dis. Treat. 2009;5:327–332. doi: 10.2147/ndt.s5335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fernandez HH, Okun MS, Rodriguez RL, et al. Quetiapine improves visual hallucinations in Parkinson disease but not through normalization of sleep architecture: results from a double-blind clinical-polysomnography study. Int. J. Neurosci. 2009;119(12):2196–2205. doi: 10.3109/00207450903222758. [DOI] [PubMed] [Google Scholar]
- 54.Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson's disease. Mov. Disord. 2011;26(Suppl. 3):S42–S80. doi: 10.1002/mds.23884. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Current treatment recommendations for nonmotor symptoms in PD, including psychosis, from the Movement Disorders Society.
- 55.Hack N, Fayad SM, Monari EH, et al. An eight-year clinic experience with clozapine use in a Parkinson's disease clinic setting. PLoS ONE. 2014;9(3):e91545. doi: 10.1371/journal.pone.0091545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Friedman JH. Atypical antipsychotic drugs in the treatment of Parkinson's disease. J. Pharm. Pract. 2011;24(6):534–540. doi: 10.1177/0897190011426556. [DOI] [PubMed] [Google Scholar]
- 57.Fernandez HH, Trieschmann ME, Friedman JH. Aripiprazole for drug-induced psychosis in Parkinson disease: preliminary experience. Clin. Neuropharmacol. 2004;27(1):4–5. doi: 10.1097/00002826-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 58.Pintor L, Valldeoriola F, Bailles E, Marti MJ, Muniz A, Tolosa E. Ziprasidone versus clozapine in the treatment of psychotic symptoms in Parkinson disease: a randomized open clinical trial. Clin. Neuropharmacol. 2012;35(2):61–66. doi: 10.1097/WNF.0b013e31824d5115. [DOI] [PubMed] [Google Scholar]
- 59.Weintraub D, Chiang C, Kim HM, et al. Association of antipsychotic use with mortality risk in patients with Parkinson disease. JAMA Neurol. 2016;73(5):535–541. doi: 10.1001/jamaneurol.2016.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lenka A, Hegde S, Jhunjhunwala KR, Pal PK. Interactions of visual hallucinations, rapid eye movement sleep behavior disorder and cognitive impairment in Parkinson's disease: a review. Parkinsonism Relat. Disord. 2016;22:1–8. doi: 10.1016/j.parkreldis.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 61.Goetz CG, Fan W, Leurgans S, Bernard B, Stebbins GT. The malignant course of “benign hallucinations” in Parkinson disease. Arch. Neurol. 2006;63(5):713–716. doi: 10.1001/archneur.63.5.713. [DOI] [PubMed] [Google Scholar]
- 62.Goetz CG, Fan W, Leurgans S. Antipsychotic medication treatment for mild hallucinations in Parkinson's disease: positive impact on long-term worsening. Mov. Disord. 2008;23(11):1541–1545. doi: 10.1002/mds.22132. [DOI] [PubMed] [Google Scholar]
- 63.Lutz UC, Sirfy A, Wiatr G, et al. Clozapine serum concentrations in dopamimetic psychosis in Parkinson's disease and related disorders. Eur. J. Clin. Pharmacol. 2014;70(12):1471–1476. doi: 10.1007/s00228-014-1772-0. [DOI] [PubMed] [Google Scholar]
- 64.Honigfeld G, Arellano F, Sethi J, Bianchini A, Schein J. Reducing clozapine-related morbidity and mortality: 5 years of experience with the Clozaril National Registry. J. Clin. Psychiatry. 1998;59(Suppl. 3):3–7. [PubMed] [Google Scholar]
- 65.Aschenbrenner DS. Strengthened safety measures with Clozapine. Am. J. Nurs. 2016;116(1):22. [Google Scholar]
- 66.Meltzer HY, Mills R, Revell S, et al. Pimavanserin, a serotonin(2A) receptor inverse agonist, for the treatment of Parkinson's disease psychosis. Neuropsychopharmacology. 2010;35(4):881–892. doi: 10.1038/npp.2009.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson's disease psychosis: a randomised, placebo-controlled Phase 3 trial. Lancet. 2014;383(9916):533–540. doi: 10.1016/S0140-6736(13)62106-6. [DOI] [PubMed] [Google Scholar]; •• This is the study showing significant benefits of pimavanserin for the treatment of psychosis. Drug recently approved by the US FDA.
- 68.Yasue I, Matsunaga S, Kishi T, Kiyoshi F, Iwata N. Serotonin 2A receptor inverse agonist as a treatment for Parkinson's disease psychosis: a systematic review and meta-analysis of Serotonin 2A receptor negative modulators. J. Alzheimers Dis. 2016;50(3):733–740. doi: 10.3233/JAD-150818. [DOI] [PubMed] [Google Scholar]
- 69.Hubbard D, Hacksell U, McFarland K. Behavioral effects of clozapine, pimavanserin, and quetiapine in rodent models of Parkinson's disease and Parkinson's disease psychosis: evaluation of therapeutic ratios. Behav. Pharmacol. 2013;24(7):628–632. doi: 10.1097/FBP.0b013e3283656db6. [DOI] [PubMed] [Google Scholar]
- 70.Oh YS, Kim JS, Lee PH. Effect of Rivastigmine on behavioral and psychiatric symptoms of Parkinson's disease dementia. J. Mov. Disord. 2015;8(2):98–102. doi: 10.14802/jmd.15041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zahodne LB, Fernandez HH. Pathophysiology and treatment of psychosis in Parkinson's disease: a review. Drugs Aging. 2008;25(8):665–682. doi: 10.2165/00002512-200825080-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ueda S, Koyama K, Okubo Y. Marked improvement of psychotic symptoms after electroconvulsive therapy in Parkinson disease. J. ECT. 2010;26(2):111–115. doi: 10.1097/YCT.0b013e3181c18a3d. [DOI] [PubMed] [Google Scholar]
- 73.Usui C, Hatta K, Doi N, et al. Improvements in both psychosis and motor signs in Parkinson's disease, and changes in regional cerebral blood flow after electroconvulsive therapy. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2011;35(7):1704–1708. doi: 10.1016/j.pnpbp.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 74.Calderon-Fajardo H, Cervantes-Arriaga A, Llorens-Arenas R, Ramirez-Bermudez J, Ruiz-Chow A, Rodriguez-Violante M. Electroconvulsive therapy in Parkinson's disease. Arq. Neuropsiquiatr. 2015;73(10):856–860. doi: 10.1590/0004-282X20150131. [DOI] [PubMed] [Google Scholar]
- 75.Quelhas R. Psychiatric care in Parkinson's disease. J. Psychiatr. Pract. 2013;19(2):118–141. doi: 10.1097/01.pra.0000428558.94329.6d. [DOI] [PubMed] [Google Scholar]
- 76.Wand AP, Peisah C. Managing psychosis in Parkinson's disease without drugs. Neurodegener. Dis. Manag. 2015;5(4):271–274. doi: 10.2217/nmt.15.27. [DOI] [PubMed] [Google Scholar]
- 77.Rabovsky K, Trombini M, Allemann D, Stoppe G. Efficacy of bifocal diagnosis-independent group psychoeducation in severe psychiatric disorders: results from a randomized controlled trial. Eur. Arch. Psychiatry Clin. Neurosci. 2012;262(5):431–440. doi: 10.1007/s00406-012-0291-1. [DOI] [PubMed] [Google Scholar]