Abstract
IgG4-related disease (IgG4-RD) is a fibroinflammatory condition that can affect practically every organ. Although it was first identified in pancreas and salivary glands, major organs like liver, biliary tree, kidney, thyroid glands and lungs are commonly involved, sometimes resulting in organ failure. We describe a case of an 41-year-old man presented with back pain after a rotator cuff injury. A Computed Tomography (CT) revealed incidentally a right lower lobe paravertebral lesion extending across the T5 and T6 vertebral levels and invading into the adjacent pleural surface. The laboratory findings and the CT guided biopsy were inconclusive. Morphological and immunohistochemical findings after a lung biopsy by video-assisted thoracic surgery (VATS) were suggestive to IgG4-related lung disease (IgG4-RLD), which was confirmed with high serum levels of IgG4. This represents the first case of a IgG4-RLD lesion located in the mediastinum and extending to the adjacent pleural surface and vertebrae and should be included in the differential diagnosis of posterior mediastinal masses.
Keywords: IgG4 lung disease, Vertebral invasion, Lung surgery
1. Introduction
Immunoglobulin G4-related disease (also called IgG4-related systemic disease, IgG4-related sclerotic disease, IgG4-positive multiorgan lymphoproliferative syndrome, IgG4-related autoimmune disease, systemic IgG4 plasmatic syndrome, IgG4-associated multifocal systemic fibrosis) was first mentioned as a systemic disease in 2003 by Kamisawa et al. [1], [2], [3]. However, two years later Zen and al firstly reported inflammatory pseudotumors of the lung with high levels of IgG4 [4]. IgG4-RD is usually presented in middle age males as an enlargement or swelling of one or more organs, a fact that raises concern for malignancy [5], [6]. The IgG4-RD's lesion can manifest as pseudotumor and is characterized by dense lymphoplasmacytic inflammation infiltrating within the organs parenchyma, fibrosis, phlebitis and increased levels of IgG4-positive plasma cells [7], [8], [9]. The disease can be present in one or more organs simultaneously or metachronously [9]. The fact that IgG4 lung disease can be asymptomatic (only with abnormal findings on imaging) or can manifest with non-specific clinical symptoms like cough, dyspnea, fever, chest pain and hemoptysis can delay the diagnosis [10], [11]. Herein, we report a case of IgG4-RLD lesion in the mediastinum extending to the adjacent pleural surface and vertebrae which was successfully treated with steroids and rituximab.
2. Illustrative case presentation
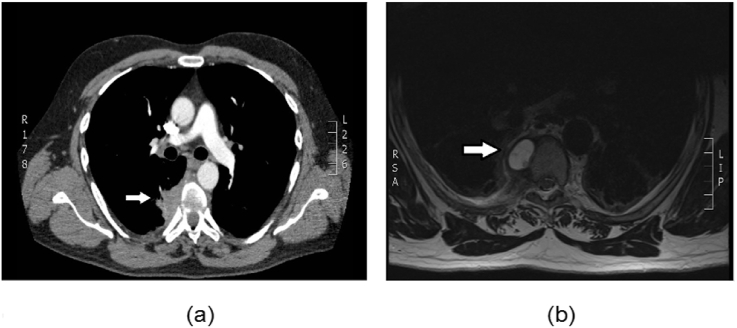
A 41-year-old man working as a chauffeur was presented to his GP with subsequent back pain after rotator cuff injury. Physical examination was unremarkable. In terms of medical history there was no exposure to tuberculosis, he had a 20 pack year history of smoking and there was no relevant surgical history. Although his chest X-ray was normal, the back pain insisted. A MRI of the chest was performed revealing a right paravertebral mass (Fig. 1b). In order to better define the lesion and exclude any other organ involvement, a computed tomography (CT) of thorax and abdomen (with contrast) was performed. The CT confirmed a 3 cm right lower lobe paravertebral soft tissue density mass lesion, invading into the adjacent pleural surface (Fig. 1a). Lymphadenopathy of station 2R and station 4R was noted. An extension across the T5 and T6 vertebral levels with frank destruction of the right T6 costovertebral joint and some enlargement of the right neural foramina were also found. Lungs, pleural spaces, mediastinum, thoracic esophagus and abdomen structures were of normal appearance. In order to specify the histopathology of the lesion, a CT guided biopsy was performed but it was not diagnostic. After multidisciplinary meeting and after written consent was obtained from the patient a right 3 ports VATS biopsy of the mediastinal mass was performed. The postoperative course was unremarkable and the patient was discharged in stable condition on the 3rd postoperative day. With regard to the treatment plan, the patient received initially 60mg of enteric-coated corticosteroids (Prednisolone) that have been gradually tapered after 4 weeks due to patient's steroid-related psychosis. These were replaced with rituximab at a 1 g IV dose every 15 days for a total of two doses. The PET/CT scan performed 3 months later showed that the paravertebral lesion was resolved, with only minimal activity. The visualized part of the musculoskeletal system including the spine showed physiological distribution of fluorodeoxyglucose (FDG). There were no FDG avid lymphadenopathy or other organ involvement.
Fig. 1.
(a) CT scan with contrast revealed a 3 cm right lower lobe paravertebral lesion extending across the T5 and T6 vertebral levels and invading into the adjacent pleural surface (arrow) (b) MRI revealing a right paravertebral mass (arrow).
3. Histology report
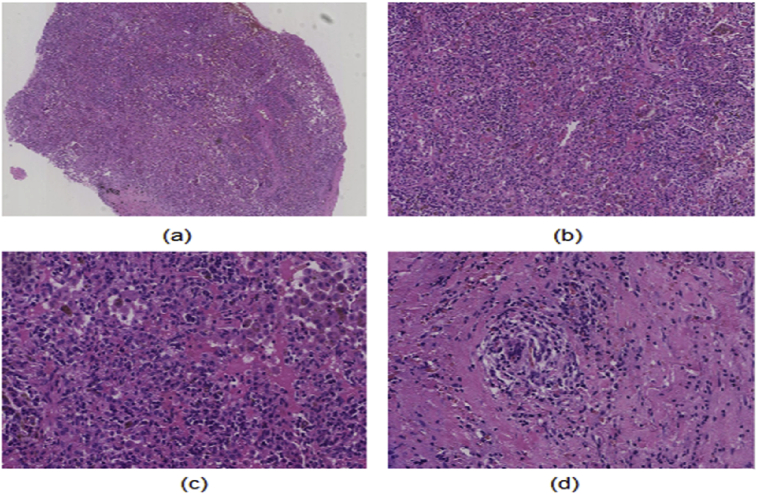
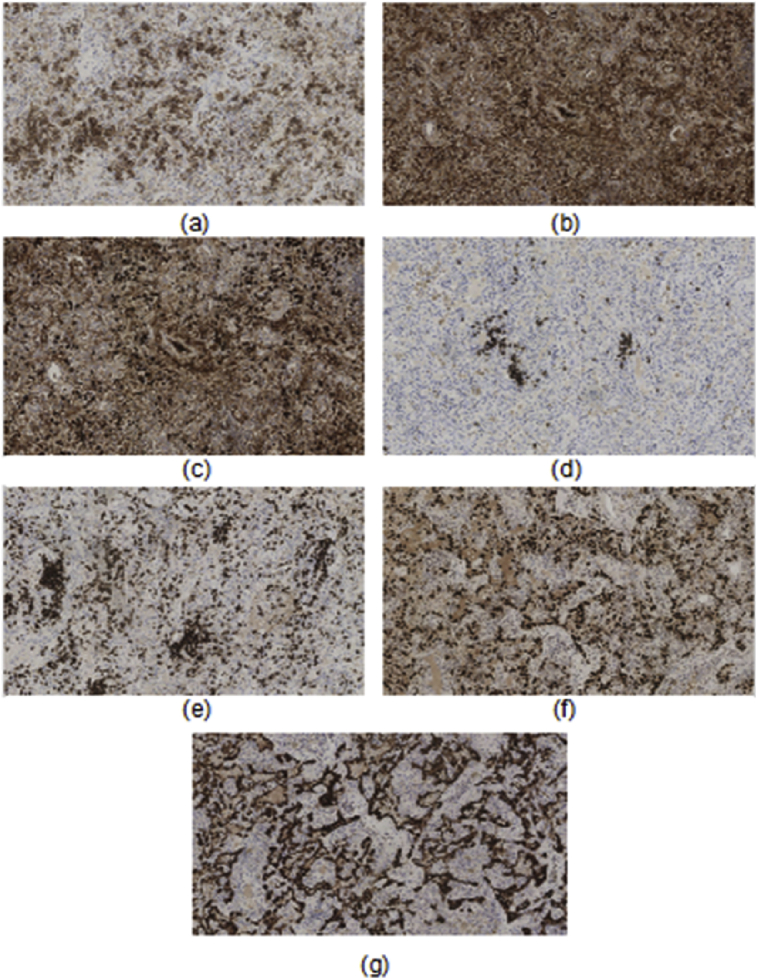
Subsequent histological examination of the specimen was performed. The macroscopic description of the lesion was characterized by multiple fragments of firm dark brown and cream colored nodular tissue measuring 15 × 15 × 3 mm aggregate. It was firmly adhered to the lung and was highly vascularized. With reference to the microscopic description, sections of lung parenchyma and adjacent fibrous tissue showed a dense lymphoplasmacytic infiltration predominantly located in the lung parenchyma (Fig. 2a, b, c). The fibrotic areas adjacent to the lung parenchyma showed a similar but less pronounced lymphoplasmacytic inflammatory infiltration. Within the lung parenchyma there were foci suggested but not diagnostic for obliterative phlebitis (Fig. 2d). The alveolar spaces showed occasional pneumocyte metaplasia with no cytological atypia. Immunohistochemistry performed showed (Fig. 3) that the inflammatory infiltration was predominantly composed of CD138 (Fig. 3a) positive plasma cells along with moderate amount of CD3 positive T-lymphocytes and scattered CD20 positive B-lymphocytes (Fig. 3d). Most plasma cells were noted to express IgG (Fig. 3b) and a large proportion of these plasma cells are also noted to co-express IgG4 (Fig. 3c). The IgG4 positive plasma cells, in areas were noted to amount up to more than 150 cells per high power field and amount up to more than 40% of the total plasma cells present. CK7 and TTF-1 highlight the pulmonary parenchymal architecture which was in areas distorted due to marked inflammatory component (Fig. 3f and g). Serum IgG4 levels were also elevated (3,95 g/l) with overall IgG within range of normality. A diagnosis of IgG4-related lung disease was made considering the lymphoplasmacytic inflammatory infiltrate of the lesion, the laboratory findings and the radiological image.
Fig. 2.
IgG4-related lung disease photomicrographs (a) Heavily inflamed lung parenchyma (Hematoxylin-eosin stain, original magnification,×25) (b,c) Dense lymphoplasmacytic inflammatory infiltrate within the lung parenchyma (Hematoxylin-eosin stain, original magnification in b, ×100; and in c,×200) (d) Focus of obliterative phlebitis (Hematoxylin-eosin stain, original magnification, ×200).
Fig. 3.
Immunohistochemistry shows that the inflammatory infiltration is predominantly composed of (a) CD138 positive plasma cells along with moderate amount of (b) CD3 positive T-lymphocytes and scattered (c) CD20 positive B-lymphocytes. Most plasma cells were noted to express (d) IgG and a large proportion of these plasma cells are also noted to co-express (e) IgG4. (f) CK7 and (g) TTF-1 highlight the pulmonary parenchymal architecture which was in areas distorted due to marked inflammatory component.
4. Discussion
The spectrum of pathologic entities which can appear in the mediastinum is wide and includes neoplastic and non-neoplastic lesions. Most of the non-neoplastic lesions do not extend across the adjacent anatomical structures. [12], [13], [14]. Although there have been reported IgG4-RD lesions of the mediastinum extending to the adjacent pleural surface, the present case indicates that such a lesion can invade to the adjacent vertebrae [21]. IgG4-related disease (IgG4-RD) is an uncommon fibroinflammatory condition that can affect practically every organ, simultaneously or metachronously [9]. IgG4-RD is usually presented in middle age males as an enlargement or swelling of one or more organs, a fact that raises concern for malignancy [5], [6], [11]. It was first mentioned as a systemic disease in 2003 by Kamisawa et al. [1], [2], [3]. However, the first who reported inflammatory pseudotumors of the lung with high levels of IgG4 were Zen and al [4]. Intrathoracic IgG4-RD lesions usually coexist with autoimmune pancreatitis and retroperitoneal fibrosis [10], [15], [22]. In most cases (75%) it is presenting as an asymptomatic lesion which is found incidentally by abnormal findings on imaging [16], [17]. In some patients can manifest with non-specific clinical symptoms like cough, dyspnea, fever, chest pain and hemoptysis a fact that can delay the diagnosis [10], [11]. Depending on the radiologic findings, IgG4-related lung lesions can be divided into four groups: solid nodular, round-shaped GGO, alveolar interstitial, and bronchovascular [10]. The IgG4-RD's lesion is characterized by dense lymphoplasmacytic inflammation infiltrating within the organ's parenchyma, fibrosis, phlebitis and increased levels of IgG4-positive plasma cells [7], [8], [9]. Moreover, in most cases it is reported an elevation of serum IgG4 concentration (more than 135 mg/dl). Recently there have been diagnostic criteria established for IgG4-RD which include: (a) swelling or masses in one or multiple organs; (b) serum IgG4 concentrations > 135 mg/dl; and (c) histopathologic examination showing infiltration and fibrosis by lymphocytes and plasmatocytes or infiltration of IgG4 + plasma cells ratio of IgG4 + /IgG + cells > 40% and >10 IgG4 plasma cells/high power fields (HPF) [18]. However, diagnostic criteria should be established for each organ that can be affected. With reference to the treatment, glucocorticoids appear to be effective in most of the patients [10]. Treatment with rituximab can be an effective alternative choice [19], [20].
In conclusion, this case report demonstrated the existence of a posterior mediastinal IgG4-RD lesion extending to the adjacent pleural surface and vertebrae. To the best of our knowledge there has not been reported a similar case. The pathogenesis and the relation with malignancy of this disease are to be further investigated.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- 1.Umehara H. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod. Rheumatol. Jpn. Rheum. Assoc. Feb. 2012;22(1):1–14. doi: 10.1007/s10165-011-0508-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamisawa Terumi, Egawa Naoto, Nakajima Hitoshi. Autoimmune pancreatitis is a systematic autoimmune disease. Am. J. Gastroenterol. Dec 2003;98.12:2811–2812. doi: 10.1111/j.1572-0241.2003.08758.x. [DOI] [PubMed] [Google Scholar]
- 3.Kamisawa T., Funata N., Hayashi Y., Eishi Y., Koike M., Tsuruta K., Okamoto A., Egawa N., Nakajima H. A new clinicopathological entity of IgG4-related autoimmune disease. J. Gastroenterol. Jan. 2003;38(10):982–984. doi: 10.1007/s00535-003-1175-y. [DOI] [PubMed] [Google Scholar]
- 4.Zen Y., Kitagawa S., Minato H., Kurumaya H., Katayanagi K., Masuda S., Niwa H., Fujimura M., Nakanuma Y. IgG4-positive plasma cells in inflammatory pseudotumor (plasma cell granuloma) of the lung. Hum. Pathol. Jul. 2005;36(7):710–717. doi: 10.1016/j.humpath.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 5.Khosroshahi A., Stone J.H. A clinical overview of IgG4-related systemic disease. Curr. Opin. Rheumatol. 2011;23(1):57–66. doi: 10.1097/BOR.0b013e3283418057. [DOI] [PubMed] [Google Scholar]
- 6.Zen Y., Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am. J. Surg. Pathol. Dec. 2010;34(12):1812–1819. doi: 10.1097/PAS.0b013e3181f7266b. [DOI] [PubMed] [Google Scholar]
- 7.Chen G., Cheuk W., Chan J.K. IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. Zhonghua bing li xue za zhi Chin. J. Pathol. Dec. 2010;39(12):851–868. [PubMed] [Google Scholar]
- 8.Masaki Y. Proposal for a new clinical entity, IgG4-positive multiorgan lymphoproliferative syndrome: analysis of 64 cases of IgG4-related disorders. Ann. Rheum. Dis. Aug. 2009;68(8):1310–1315. doi: 10.1136/ard.2008.089169. [DOI] [PubMed] [Google Scholar]
- 9.Guma M., Firestein G.S. IgG4-related diseases. Best Pract. Res. Clin. Rheum. 2012;26:425–438. doi: 10.1016/j.berh.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Zen Y., Inoue D., kitao A., Onodera M., Abo H., Miyayama S., Gabata T., Matsui O. IgG4-related lung and pleural disease: a clinicopathologic study of 21 cases. Am. J. Surg. Pathol. 2009;33:1886–1893. doi: 10.1097/PAS.0b013e3181bd535b. [DOI] [PubMed] [Google Scholar]
- 11.Inoue D., Zen Y., Abo H. Immunoglobulin G4-related lung disease: CT findings with pathologic correlations. Radiology. 2009;251:260–270. doi: 10.1148/radiol.2511080965. [DOI] [PubMed] [Google Scholar]
- 12.Juanpere S., Cañete N., Ortuño P., Martínez S., Sanchez G., Bernado L. A diagnostic approach to the mediastinal masses. Insights Imaging. 2013;4(1):29–52. doi: 10.1007/s13244-012-0201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis R.D., Oldham H.N., Sabiston D.C. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann. Thorac. Surg. 1987;44:229–237. doi: 10.1016/s0003-4975(10)62059-0. [DOI] [PubMed] [Google Scholar]
- 14.Macchiarini P., Ostertag H. Uncommon primary mediastinal tumours. Lancet Oncol. 2004;5:107–118. doi: 10.1016/S1470-2045(04)01385-3. [DOI] [PubMed] [Google Scholar]
- 15.Shigemitsu H., Koss M.N. IgG4-related interstitial lung disease: a new and evolving concept. Curr. Opin. Pulm. Med. 2009;15:513–516. doi: 10.1097/MCP.0b013e32832ea509. [DOI] [PubMed] [Google Scholar]
- 16.Umeda M., Fujikawa K., Origuchi T., Tsukada T., Kondo A., Tomari S., Inoue Y., Soda H., Nakamura H., Matsui S., Kawakami A. A case of IgG4-related pulmonary disease with rapid improvement. Mod. Rheumatol. Jpn. Rheum. Assoc. Nov. 2012;22(6):919–923. doi: 10.1007/s10165-012-0600-6. [DOI] [PubMed] [Google Scholar]
- 17.Lighaam L., Aalberse R., Rispens T. IgG4-Related fibrotic diseases from an immunological perspective: regulators out of control? Int. J. Rheumatol. 2012;2012:789164. doi: 10.1155/2012/789164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Umehara H. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod. Rheumatol. Jpn. Rheum. Assoc. Feb. 2012;22(1):21–30. doi: 10.1007/s10165-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 19.Khosroshahi A., Bloch D.B., Deshpande V., Stone J.H. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum. Jun. 2010;62(6):1755–1762. doi: 10.1002/art.27435. [DOI] [PubMed] [Google Scholar]
- 20.Khosroshahi A., Carruthers M.N., Deshpande V., Unizony S., Bloch D.B., Stone J.H. Rituximab for the treatment of IgG4-related disease: lessons from 10 consecutive patients. Medicine. Jan. 2012;91(1):57–66. doi: 10.1097/MD.0b013e3182431ef6. [DOI] [PubMed] [Google Scholar]
- 21.Fei Y., Shi J., Lin W., Chen Y., Feng R., Wu Q., Gao X., Xu W., Zhang W., Zhang X., Zhao Y., Zeng X., Zhang F. Intrathoracic involvements of immunoglobulin G4-related sclerosing disease. Medicine. Dec. 2015;94(50):e2150. doi: 10.1097/MD.0000000000002150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palazzo E., Palazzo C., Palazzo M. IgG4-related disease. Joint, bone, spine. Rev. Du. Rhum. 2013;81(1):27–31. doi: 10.1016/j.jbspin.2013.06.001. [DOI] [PubMed] [Google Scholar]