Abstract
Endoscopic submucosal dissection (ESD) enables en bloc curative resection of early gastric cancers (EGCs) with a negligible risk of lymph node metastasis (LNM). Although ESD for EGCs with absolute and expanded indications is safe, the results differ between EGCs with specialized and common histologies. EGC with papillary adenocarcinoma is a differentiated-type adenocarcinoma. At present, it is treated with ESD according to the same criteria as other differentiated-type adenocarcinomas. The LNM rate under the current indication criteria is high, and over half of the patients who undergo ESD as a primary treatment for EGC with papillary adenocarcinoma achieve an out-of-ESD result. Gastric carcinoma with lymphoid stroma in EGC has a low LNM rate and a favorable outcome, despite deep submucosal invasion. Patients with this gastric cancer subtype may be good candidates for ESD, even with deep submucosal invasion. Large-scale prospective multi-center studies with longer follow-up periods are needed to set proper ESD criteria for these tumors. Clinicians should be aware of these disease entities and ESD should be more carefully considered for EGCs with papillary adenocarcinoma and gastric carcinoma with lymphoid stroma.
Keywords: Stomach, Neoplasms, Endoscopic resection, Histology, Lymph node metastasis
INTRODUCTION
Recent advances in endoscopic resection techniques, such as endoscopic submucosal dissection (ESD), allow for en bloc curative resection of early gastric cancers (EGCs) with a minimal risk of lymph node metastasis (LNM), regardless of tumor size or presence of submucosal fibrosis. ESD has several merits over gastrectomy: it leads to a more accurate histopathological diagnosis, it is a minimally invasive procedure, and it demonstrates a high rate of curative resection and a low rate of local recurrence. Thus, ESD has been accepted as a standard and safe treatment modality for EGCs in Eastern Asia including Korea and Japan [1-4]. The indications for ESD of EGCs have been gradually expanding [1,4]. ESD for EGCs with absolute and expanded indications is accepted as a safe treatment strategy, according to recent long-term follow-up studies on ESD for EGCs in Eastern Asia [2,4,5]. However, the results for ESD of EGCs with specialized histologies are somewhat different from those of EGCs with common histologies. Furthermore, there have been few reports on the safety and outcomes of ESD for EGCs with specialized histologies. Here, I summarize the outcomes of ESD for EGCs with two rare specialized histologies on the basis of my experience.
PAPILLARY ADENOCARCINOMA
Papillary adenocarcinoma (PAC) is a rare histologic entity among gastric adenocarcinomas. It demonstrates well-differentiated structures and its histopathologic characteristics are epithelial projections which are scaffolded by a central fibrovascular core [6]. Until now, the biological behavior and prognostic significance of PAC are unclear due to the rare incidence of PAC. At present, PAC is classified into intestinal-type adenocarcinoma using the Lauren classification [7], and as a differentiated-type adenocarcinoma using the Japanese classification of gastric carcinoma [8]. However, it is reported that PAC has higher rates of liver metastasis and LNM, and a lower 5-year overall survival rate than non-papillary gastric adenocarcinomas, such as tubular adenocarcinoma [6,9].
Considering that PAC has a more aggressive nature compared with other gastric adenocarcinomas, an inevitable question occurs whether it could be treated under the same ESD indication criteria as tubular adenocarcinomas. It is unlikely that the same ESD indication criteria can be rationally applied to gastric adenocarcinomas with and without considerable PAC components [10-12].
According to data from my hospital (Pusan National University Hospital, Busan, Korea) [13], 49 patients underwent surgery for EGC with PAC between January 2005 and May 2013. The LNM rate was 7.1% (1/14) in mucosal cancers, which was higher than that in differentiated-type mucosal cancers (0.4%), but similar to that in undifferentiated-type mucosal cancers (4.2% to 7.3%) [14]. When the current ESD indication criteria were applied to these 49 patients, 17 patients met the ESD indication criteria, as follows: six patients in the absolute indication criteria (mucosal cancer ≤20 mm in size without ulcerative findings) and 11 patients in the expanded indication criteria (four patients, mucosal cancer >20 mm in size without ulcerative findings; two patients, mucosal cancer ≤30 mm in size with ulcerative findings; and five patients, minute [<500 um from the muscularis mucosa] submucosal cancer ≤30 mm in size). Among the 17 patients with EGC who met the ESD indication criteria, two patients (11.8%) had LNM (Table 1) [13].
Table 1.
Lymph Node Metastasis in Early Gastric Cancers with Papillary Adenocarcinoma after Application to the Current Endoscopic Submucosal Dissection Indication Criteria
| Mucosal cancer, % |
Submucosal cancer, % |
||||||
|---|---|---|---|---|---|---|---|
| Ulcer (-) |
Ulcer (+) |
sm1 |
sm2 |
||||
| ≤20 mm (n=6) | >20 mm (n=4) | ≤30 mm (n=2) | >30 mm (n=2) | ≤30 mm (n=5) | >30 mm (n=3) | Any size (n=27) | |
| Lymph node metastasis | 0 | 25 | 0 | 0 | 20 | 0 | 26 |
Adapted from Lee et al. [13]
During the same period, 24 patients having EGC with PAC underwent ESD as a primary treatment at the same hospital. In the pre-ESD diagnostic work-up, 10 patients met the absolute ESD indication criteria and 14 patients met the expanded ESD indication criteria. In the final post-ESD histopathologic examination, 13 patients (54%) achieved an out-of-ESD result, nine had lymphovascular invasion or deep submucosal invasion, three had mucosal cancer >30 mm in size with ulcerative findings, and one had minute submucosal cancer >30 mm in size [13]. Of these patients, nine (37.5%) underwent additional gastrectomy with lymph node dissection for non-curative resection. The frequency of additional gastrectomy in patients with PAC is higher compared to the previously reported frequency of additional surgery after ESD (2.1% to 14.6%) [15,16]. Therefore, considering the higher frequency of LNM and additional surgery associated with this technique, ESD should be more carefully performed for EGCs with PAC, even in cases with suspected ESD indications after the pre-ESD work-up, compared with other differentiated-type adenocarcinomas.
GASTRIC CARCINOMA WITH LYMPHOID STROMA
Gastric carcinoma with lymphoid stroma (GCLS) is a rare histological variant of gastric cancer, according to the 2010 World Health Organization classification system, and it accounts for 1% to 4% of all gastric carcinomas [17]. Typically, the characteristic histopathologic features of GCLS include poorly developed tubular structures and prominent lymphoid infiltrates in non-desmoplastic stroma. However, there are no standardized diagnostic criteria and the histolopathological diagnosis for GCLS is obscure.
GCLS has distinct clinicopathologic characteristics and it is generally accepted that patients with GCLS have a favorable prognosis with a low LNM rate [18]. It has been reported that an increase in the number of tumor-infiltrating lymphocytes, which are reflective of the host’s immune response to tumor cells, is significantly associated with reduced metastasis and improved survival [19]. However, GCLS has histopathologically poorly developed tubular structures, and, therefore, it tends to be regarded as undifferentiated-type adenocarcinoma in the ESD indication criteria.
According to the data from my hospital, out of 59 patients with EGC with GCLS who underwent surgery between January 2007 and December 2014, two patients (3.4%) demonstrated LNM. The LNM rates are 0.0% (0/9) in mucosal cancers with GCLS and 4.0% (2/50) in submucosal cancers with GCLS, respectively. In particular, the LNM rate in submucosal cancers with GCLS (4.0%) was significantly lower than that in submucosal cancers with differentiated-type and undifferentiated-type adenocarcinoma (19.4%, 140/722) (Fig. 1).
Fig. 1.
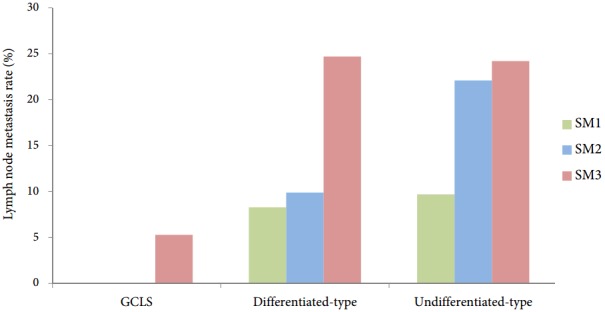
Lymph node metastasis rate according to tumor histology and depth of invasion in submucosal cancers. GCLS, gastric carcinoma with lymphoid stroma.
EGC with GCLS is a specific type of gastric cancer that has a favorable outcome, and is associated with a very low LNM rate despite deep submucosal invasion. Therefore, patients with EGC with GCLS, including those with deep submucosal invasion, may be good candidates for ESD as like well-differentiated neuroendocrine tumor. However, further investigation is needed to establish new recommendation criteria for ESD for EGCs with GCLS.
CONCLUSIONS
The current ESD indications for EGCs are based on the differentiation degree of the tumor. The data on ESD for EGCs with specialized histologies were scant until now. Although EGC with PAC is one of differentiated-type adenocarcinomas and so treated according to the same ESD indication criteria as for other differentiated-type adenocarcinomas, the LNM rate under the current ESD indication criteria was higher compared with other differentiated-type cancers. Furthermore, more than half of the patients undergoing ESD for EGC with PAC ultimately came to achieve out-of-ESD indication. On the other hand, EGC with GCLS is a specific type of gastric cancer with a favorable outcome. This outcome is associated with a very low LNM rate in patients having EGC with GCLS, even in patients with deep submucosal invasion. This suggests that patients with EGC with GCLS, even those with deep submucosal invasion, may be potential candidates for ESD. Although large-scale prospective multi-center studies with longer follow-up periods will be required to determine the optimal ESD criteria for these tumors, clinicians should be aware of these rare disease entities. ESD should be more carefully considered for EGCs with PAC and GCLS.
Footnotes
Conflicts of Interest: The author has no financial conflicts of interest.
REFERENCES
- 1.Abe N, Gotoda T, Hirasawa T, et al. Multicenter study of the long-term outcomes of endoscopic submucosal dissection for early gastric cancer in patients 80 years of age or older. Gastric Cancer. 2012;15:70–75. doi: 10.1007/s10120-011-0067-8. [DOI] [PubMed] [Google Scholar]
- 2.Choi MK, Kim GH, Park DY, et al. Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a single-center experience. Surg Endosc. 2013;27:4250–4258. doi: 10.1007/s00464-013-3030-4. [DOI] [PubMed] [Google Scholar]
- 3.Abe S, Oda I, Suzuki H, et al. Short- and long-term outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Endoscopy. 2013;45:703–707. doi: 10.1055/s-0033-1344396. [DOI] [PubMed] [Google Scholar]
- 4.Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009;69:1228–1235. doi: 10.1016/j.gie.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 5.Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 6.Hu B, El Hajj N, Sittler S, Lammert N, Barnes R, Meloni-Ehrig A. Gastric cancer: classification, histology and application of molecular pathology. J Gastrointest Oncol. 2012;3:251–261. doi: 10.3978/j.issn.2078-6891.2012.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 8.Japanese Gastric Cancer Association Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 9.Yasuda K, Adachi Y, Shiraishi N, Maeo S, Kitano S. Papillary adenocarcinoma of the stomach. Gastric Cancer. 2000;3:33–38. doi: 10.1007/pl00011687. [DOI] [PubMed] [Google Scholar]
- 10.Takizawa K, Ono H, Kakushima N, et al. Risk of lymph node metastases from intramucosal gastric cancer in relation to histological types: how to manage the mixed histological type for endoscopic submucosal dissection. Gastric Cancer. 2013;16:531–536. doi: 10.1007/s10120-012-0220-z. [DOI] [PubMed] [Google Scholar]
- 11.Hanaoka N, Tanabe S, Mikami T, Okayasu I, Saigenji K. Mixed-histologic-type submucosal invasive gastric cancer as a risk factor for lymph node metastasis: feasibility of endoscopic submucosal dissection. Endoscopy. 2009;41:427–432. doi: 10.1055/s-0029-1214495. [DOI] [PubMed] [Google Scholar]
- 12.Okada K, Fujisaki J, Yoshida T, et al. Long-term outcomes of endoscopic submucosal dissection for undifferentiated-type early gastric cancer. Endoscopy. 2012;44:122–127. doi: 10.1055/s-0031-1291486. [DOI] [PubMed] [Google Scholar]
- 13.Lee HJ, Kim GH, Park DY, et al. Is endoscopic submucosal dissection safe for papillary adenocarcinoma of the stomach? World J Gastroenterol. 2015;21:3944–3952. doi: 10.3748/wjg.v21.i13.3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akagi T, Shiraishi N, Kitano S. Lymph node metastasis of gastric cancer. Cancers (Basel) 2011;3:2141–2159. doi: 10.3390/cancers3022141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noh H, Park JJ, Yun JW, et al. Clinicopathologic characteristics of patients who underwent curative additional gastrectomy after endoscopic submucosal dissection for early gastric cancer or adenoma. Korean J Gastroenterol. 2012;59:289–295. doi: 10.4166/kjg.2012.59.4.289. [DOI] [PubMed] [Google Scholar]
- 16.Jung H, Bae JM, Choi MG, Noh JH, Sohn TS, Kim S. Surgical outcome after incomplete endoscopic submucosal dissection of gastric cancer. Br J Surg. 2011;98:73–78. doi: 10.1002/bjs.7274. [DOI] [PubMed] [Google Scholar]
- 17.Lauwers GY, Carneiro F, Graham DY, et al. Gastric carcinoma. In: Bosman FT, Carneiro F, Hruban RH, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research against Cancer; 2010. pp. 48–58. [Google Scholar]
- 18.Lee JH, Kim SH, Han SH, An JS, Lee ES, Kim YS. Clinicopathological and molecular characteristics of Epstein-Barr virus-associated gastric carcinoma: a meta-analysis. J Gastroenterol Hepatol. 2009;24:354–365. doi: 10.1111/j.1440-1746.2009.05775.x. [DOI] [PubMed] [Google Scholar]
- 19.Lee HE, Chae SW, Lee YJ, et al. Prognostic implications of type and density of tumour-infiltrating lymphocytes in gastric cancer. Br J Cancer. 2008;99:1704–1711. doi: 10.1038/sj.bjc.6604738. [DOI] [PMC free article] [PubMed] [Google Scholar]


