SUMMARY
Cartilage is one of the most preferable grafts for tympanoplasty (TPL). The anatomical and audiological results and take rates of perichondrium attached cartilage island graft in tympanoplasty (PACIT) are presented herein. One hundred ninety four ears of 191 patients (108 male, 83 female) were evaluated retrospectively in terms of the type of surgery, graft take rate and hearing results. Type I, II, and III TPL were performed in 127 (65.46%), 45 (23.20%), and 22 (11.34%) ears, respectively. The overall mean preoperative pure tone average-air bone gaps (PTA-ABGs) for TPL types were 33.74 ± 9.60, 52.58 ± 9.07, and 56.58 ± 10.27 dB HL, respectively; postoperative mean values for TPL groups were 18.55 ± 9.25, 31.21 ± 4.36, and 44.84 ± 12.45 dB HL. Postoperative hearing results showed an improvement (≥ 10 dB) in 76.81% of ears with a mean gain of 20 dB HL (range 10-40 dB). However, 19.07% of ears showed no change (< 10, ≥ 0 dB) in hearing, and hearing worsened in 4.12% of ears (< 0 dB) postoperatively. Overall, graft take was 91.24% at least 13 months (mean 68.64) after surgery with a graft failure rate of 8.76%. Graft take was successful in TPL groups. Postoperative PTA-ABG results demonstrated significant improvement. The long-term eligibility of perichondrium attached cartilage island graft in TPL is emphasised with this study.
KEY WORDS: Chronic otitis media, Cartilage tympanoplasty, Cholesteatoma, Mastoidectomy, Graft take rate, Pure tone audiogram, Air bone gap, PACIT
RIASSUNTO
La cartilagine rappresenta una delle opzioni più interessanti per il confezionamento dell'innesto nella timpanoplastica (TPL). Col presente studio presentiamo i nostri risultati audiologici e il rate di attecchimento nei casi di TPL trattati con innesto di cartilagine con pericondrio (PACIT). Sono stati analizzati, in termini di tipo di chirurgia effettuata, attecchimento dell'innesto e risultati audiologici, 194 orecchi di 191 pazienti (108 maschi, 83 donne). Sono state effettuate 127 (65,46%) TPL tipo I, 45 (23,20%) tipo II e 22 (11,34%) tipo III. Il gap medio fra via aerea e via ossea all'audiometria tonale preoperatoria è stato rispettivamente 33,74 ± 9,60, 52,58 ± 9,07, e 56,58 ± 10,27 dB HL; i valori nel postoperatorio sono stai invece 18,55 ± 9,25, 31,21 ± 4,36, and 44,84 ± 12,45 dB HL. Nel postoperatorio di è registrato un miglioramento della soglia (≥ 10dB) nel 76,81% degli orecchi valutati, con un recupero medio di 20 dB HL (range 10-40 dB). Tuttavia il 19,07% degli orecchi valutati non ha mostrato un miglioramento della soglia uditiva, e il 4,12% ha manifestato un peggioramento della soglia. L'innesto ha attecchito correttamente nel 91,24% dei casi con follow-up di almeno 13 mesi con una media di 68,64 mesi, mentre si è registrato un fallimento nel 8,76% dei casi. In considerazione dei livelli postoperatori della soglia uditiva e dell'elevato rate di attecchimenti registrato, il presente studio ha evidenziato l'efficacia a lungo termine dell'innesto di cartilagine con pericondrio.
Introduction
Tympanoplasty (TPL) and tympano-mastoidectomy operations have been performed in the treatment of chronic otitis media (COM) since 1774 1. Temporalis fascia and perichondrium can be used as a graft material to repair tympanic membrane with high success rates, up to 95%. These materials may not be appropriate to use in cases with severe tubal dysfunction, total tympanic membrane perforation, fibro-adhesive processes and revision operations. In such situations, a cartilage graft is a good choice because of its stability, and there is no need for extra instruments during the operation 2. Cartilage grafts are also used in revision surgery, in which the tympanic membrane was previously reconstructed with fascia, and in recurrent cholesteatoma cases 3. Cartilage grafts may be used in different ways, such as perichondrium cartilage island, palisade or shield graft and cartilage reinforcement technique 4 5.
The aim of this study was to establish the long term results of type I-II-III cartilage TPL achieved with a cartilage island graft with its perichondrium attached to one side, defined as perichondrium attached cartilage island tympanoplasty (PACIT). Patients were evaluated for extent of disease, surgical procedures, take rates and hearing results. An overview of the literature on the cartilage TPL is also presented.
Materials and methods
The study was approved by the Ethics Committee of Bursa Sevket Yilmaz Training and Research Hospital. The study included 194 ears in 191 patients (83 females, 108 males) with a mean age of 42.64 years who underwent PACIT. The operations were classified as originally described by Wullstein in 1956 6. The patients who underwent type I, II and III TPL were included in the study. Operations which were performed along with partial or total ossicular replacement prosthesis were excluded from the study.
All operations were performed by two senior surgeons (FS, DA) between 2002 and 2012 at Department of Otolaryngology. In the cases of bilateral TPL, the second operation was performed with an interval of at least 6 months. Surgical records and patient charts were reviewed retrospectively.
Data on background variables (gender, age, side, TM perforation and middle ear pathology), surgical approach, complications and anatomical and functional outcome were collected from the patient charts. Each patient had a pure tone audiogram (PTA) at 0.5, 1, 2 and 4 KHz frequencies preoperatively and at least 6 weeks postoperatively. The failure of middle ear surgery was accepted when there was a re-perforation, lateralisation or retraction of the tympanic membrane, graft failure, sensorineural hearing loss, facial nerve injury and residual cholesteatoma. All patients included in the study were regularly monitored for at least one year following surgery.
All operations were performed under general anaesthesia. Four quadrants of the external ear canal and both sides of tragus were infiltrated using 1% lidocaine with epinephrine 1:100,000 before the operation. The surgery was performed in a post auricular or endaural approach. After the edges of the tympanic membrane perforation were denuded and tympanic membrane remnants with tympanosclerosis were removed, a tympanomeatal flap (vascular strip) was elevated from 12 to 6 o'clock. Then the middle ear was explored, the status of the ossicular chain was checked, and any pathology in this area was removed. If there was a fixation or defect on the ossicular chain, mobilisation and reconstruction of the chain was performed.
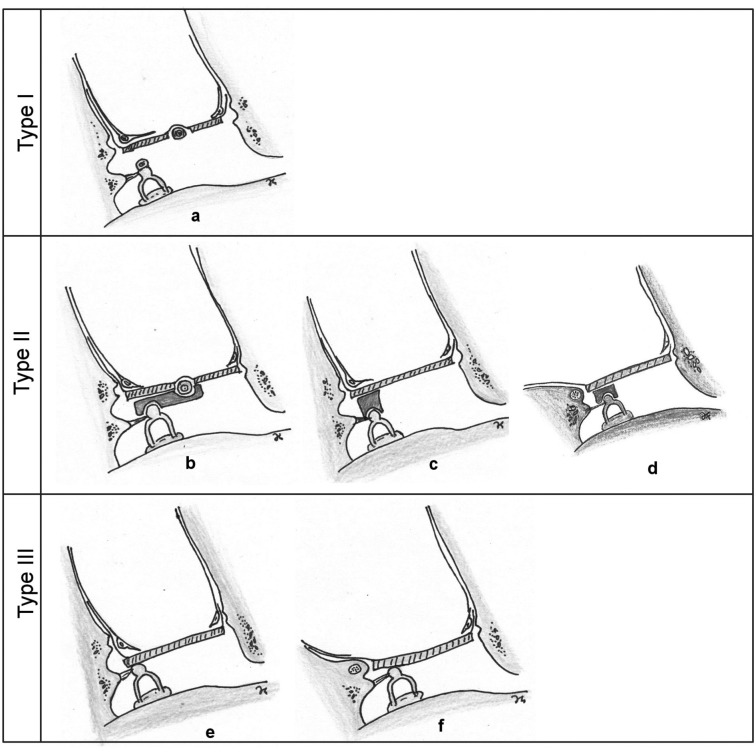
Continuity of the ossicular chain was restored with a strut (reshaped incus or cortical bone) in type II tympanoplasty (Fig. 1b,c,d). In the cases of type III tympanoplasty, the graft was placed directly on the capitulum of stapes as myringo-stapediopexy (Fig. 1e,f). Primary type II and III tympanoplasty operations were performed with intact canal wall (ICW) and canal wall down (CWD) procedures. We did not use partial or total ossicular replacement prosthesis in any of cases included in this study.
Fig. 1.
Schematic drawings of PACIT types. Type I (a), type II; partial ossicular reconstruction, cartilage graft plus interposition with reshaped incus or cortical bone on stapedial capitulum in intact canal wall and canal wall down tympanoplasty (b,c,d), type III; intact canal wall with myringostapediopexy (e) and canal wall down tympanoplasty with myringostapediopexy (f).
The cartilage graft with bilateral perichondrium was harvested from the tragus without thinning out. To prepare a perichondrium attached cartilage graft (PACG), the perichondrium on one side of cartilage was elevated and left attached to spread on the external ear canal and adhere to the tympanomeatal flap subsequently (Fig. 1a). Next, the cartilage was sized to the tympanic annulus and a V-shaped piece of cartilage was excised to accommodate the graft to the manubrium of malleus in type I TPL (Fig. 2).
Fig. 2.
The cartilage graft harvested from the tragus. The perichondrium on one side is elevated and left attached; a V-shaped wedge of cartilage is excised to accommodate the manubrium of the malleus for type I tympanoplasty.
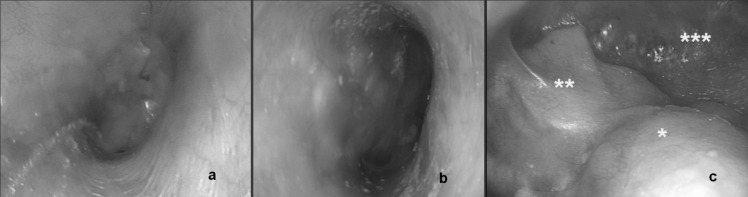
Fig. 3.
Postoperative appearance of cartilage graft in type I, II and III tympanoplasty. Type I in a right ear at postoperative 15th month (a); type II-intact canal wall in a right ear at postoperative 13th month (b); type III-canal wall down at 18th month postoperatively. Facial ridge (single asterisk), cartilage graft (double asterisk), mastoid cavity (three asterisks) (c).
The PACG was placed with the underlay technique. The attached perichondrium part of graft was spread on the posterior quadrant of external auditory canal or mastoid cavity. The middle ear was packed with gelfoam, and gelfoam pledgets impregnated with antibiotic ointment (Furacin®, Zentiva, Istanbul, Turkey) were placed lateral to the graft for stabilisation and to secure proper positioning of the tympanomeatal flap. Skin and subcutaneous incisions were closed in two layers. A rolled gauze pack impregnated with antibiotic ointment was placed in the external ear canal, and a mastoid dressing was applied for 3 days.
Skin sutures were removed 1 week after surgery. Absorbable gelatine sponges were partially suctioned from the external ear canal in CWD and ICW cases at 1 and 2 weeks after the surgery, respectively. Ear drops with steroid (Onadron®, IE Ulagay-Menarini Group, Istanbul, Turkey) and antibiotic (Siprogut®, Bilim Pharmaceuticals, Istanbul, Turkey) were prescribed for 2 weeks. The take of tympanic membrane was examined and audiometry was carried out at least 6 weeks after surgery. The patients were followed up postoperatively by serial audiometries at 1.5, 6, and 12 months and yearly thereafter.
Ears were evaluated for the closure of tympanic membrane (take rates) at least 6 weeks after the operation. Long term take rates with respect to tympanoplasty types were evaluated on the basis of last visit after surgery. Preoperative and postoperative pure tone average-air bone gaps (PTA-ABG) regarding to TPL types were compared with Student's t test. A p value less than 0.05 was considered significant.
The improvements in air conduction levels were also evaluated. Ears were rated with respect to the difference between preoperative and postoperative air conduction levels (dB) as improved (≥ 10 dB), no change (< 10, 0 ≥ dB) and worsened (< 0 dB).
Results
The study included 191 patients (194 ears) who underwent PACIT. Eighty-three (85 ears) (43.81%) were female and 108 (109 ears) (56.19%) were male. The age of patients ranged from 18 to 59, with a mean age of 42.64 ± 8.8 years. The mean follow-up time was 68.64 ± 8.0 months (range 13 to 110). Three patients (3 female, 1 male) had underwent bilateral TPL. Of the remaining 188 ears, 86 had right (45.87%) TPL and 102 had left (54.12%) TPL.
All patients required total tympanic membrane reconstruction for the following causes: 120 ears (61.85%) had central perforation, 33 (17.01%) ears had large -total/subtotal- perforation and 41 (21.14%) had perforation with cholesteatoma. The distribution of preoperative middle ear disease and tympanic membrane perforations is shown in Table I.
Table I.
Preoperative middle ear/TM status of operated ears.
| Middle ear and TM disease | ||||
|---|---|---|---|---|
| Type I (N = 127) n/% |
Type II (N = 45) n/% |
Type III (N = 22) n/% |
Total n/% |
|
| Central TM perforation | 120/61.85 | 0/0 | 0/0 | 120/61.85 |
| Large-total/subtotal-TM perforation | 07/03.61 | 26/13.40 | 0/0 | 33/17.01 |
| Cholesteatoma | 0/0 | 19/09.80 | 22/11.34 | 41/21.14 |
| Total | 127/65.46 | 45/23.20 | 22/11.34 | 194/100.00 |
n: number of ears, TM: tympanic membrane
Type I TPL without mastoidectomy was performed in 127 (65.46%) ears, type II tympanoplasty in 45 (23.20%) (ICW = 33, CWD = 13) and 22 (11.34%) ears underwent type III TPL (ICW = 5, CWD = 16). Of the 41 ears with cholesteatoma, 29 had CWD and 12 had ICW procedures. There were no complications such as haematoma, facial nerve injury, wound infection, fistula, or sensorineural hearing loss. During the follow-up period, recurrent cholesteatoma occurred in 2 patients (4.88%) at 11 and 18 months after primary ICW procedures. The diseases were treated successfully with CWD. Only the audiological results of primary operations were evaluated in the study. There were 3 cases of graft medialisation in the type II TPL group. No complications such as stenosis of the external auditory canal were reported after harvesting the tragal cartilage.
Patients were followed postoperatively by serial PTAABG at 1.5, 6 and 12 months and yearly thereafter. The follow-up periods that were more than 12 months in 194 ears were considered adequate to interpret the stability of postoperative graft take.
Overall, graft take was successful in 177 ears (91.24%) of all procedures at least 13 months after the surgery. Two (0.98%) grafts failed due to the recurrence of cholesteatoma. No new perforations occurred during follow-up period. Moreover, there was no lateralisation or medial retraction of the graft. Overall, failure rates according to the groups are shown in Table II.
Table II.
Overall failure and recurrence of cholesteatoma rates.
| Overall failure | ||||
|---|---|---|---|---|
| Type I (N = 127) n/% |
Type II (N = 45) n/% |
Type III (N = 22) n/% |
Total n/% |
|
| Overall graft failure | 10/05.15 | 4/02.06 | 3/01.55 | 17/08.76 |
| Medialisation | 0 | 3/01.55 | 0 | 3/01.55 |
| Recurrence of cholesteatoma п | 0 | 1/00.515 | 1/00.515 | 2/01.03 |
| Total graft failure for each group | 10/07.88 | 4/08.89 | 3/13.64 |
assessed in terms of cause of failure
n: number of ears
The overall mean pre-operative PTA-ABGs for type I, II and III TPL were 33.74 ± 9.60, 52.58 ± 9.07 and 56.58 ± 10.27 dB HL, respectively, whereas postoperative PTA-ABG values were 18.55 ± 9.25, 31.21 ± 4.36 and 44.84 ± 12.45 dB HL for the same groups. When preoperative and postoperative PTA-ABG were compared, there was a statistically significant improvement in PTA-ABG for all three TPL types (p < 0.05) (Table III).
Table III.
Overall pre- and post-operative Pure Tone Averages – Air Bone Gap (dB HL).
| Pure Tone Averages – Air Bone Gap (dB HL) | |||
|---|---|---|---|
| Type I (N = 127) PTA ± SD |
Type II (N = 45) PTA ± SD |
Type III (N = 22) PTA ± SD |
|
| Preoperative | 33.74 ± 9.60 | 52.58 ± 9.07 | 56.58 ± 10.27 |
| Postoperative | 18.55 ± 9.25 | 31.21 ± 4.36 | 44.84 ± 12.45 |
| p* | < 0.0001 | < 0.0001 | 0.0012 |
Student's t test used, p < 0.05
PTA: pure tone averages
Evaluation of the difference between pre- and post-operative air conduction levels revealed that the latter decreased in 8 (4.12%) ears; the early postoperative hearing results (at 1.5 and 3 months after surgery) remained stable in all patients. Postoperative hearing results in our study showed an improvement (≥ 10 dB) in 149 ears (76.81%) with a mean gain of 20 dB (range 10-40 dB). The difference between pre- and post-operative air conduction levels was unchanged (< 10, 0 ≥ dB) in 37 (19.07%) ears. The improvements in postoperative hearing levels regarding tympanoplasty types are summarized in Table IV.
Table IV.
Hearing improvement after the operations in tympanoplasty groups.
| Audiological change**(dB HL) | ||||
|---|---|---|---|---|
| Type I (N = 127) n/% |
Type II (N = 45) n/% |
Type III (N = 22) n/% |
Overall n/% |
|
| Improved (≥ 10 dB | 106/83.46 | 29/64.45 | 13/59.09 | 148/76.29 |
| No Change (< 10, 0 ≥ dB) | 21/16.54 | 10/22.22 | 04/18.18 | 35/18.04 |
| Worsened (< 0 dB) | 00/00.00 06/ | 06/13.33 | 05/22.73 | 11/05.67 |
| Total | 127/100.00 | 45/100.00 | 22/100.00 | 194/100.00 |
The difference = preoperative air conductive level – postoperative air conduction level (dB HL)
n: number of ears
Discussion
Tympanoplasty is performed to repair the tympanic membrane. With this surgical procedure there are two main targets. The first aim is to close the tympanic membrane and to have a closed middle ear, which will prevent the ear from subsequent infection and drainage. The second is to provide free movement of ossicles, which will result in better sound transmission and hearing. Skin, fascia lata, vein, temporalis fascia, perichondrium and dura mater have been used in the literature 7. Today, temporalis fascia is the most commonly employed material for tympanic membrane reconstruction 8.
The use of cartilage is proposed in middle ear surgery, since it offers a reliable technique in cases of advanced middle ear pathology and eustachian tube dysfunction 9. In 1963, Salen 10 and Jansen 11 first reported the use of cartilage composite grafts for tympanic membrane reconstruction. The interest for this material has risen in last decade. Clinical and experimental studies show that the cartilage is well tolerated in tympanoplastic surgery 12 13.
Despite the thickness of cartilage, various authors pointed out equal or better hearing results for the cartilage comparing to temporalis fascia in tympanoplasty 9 14. Shield cartilage TPL using sliced tragal cartilage-perichondrium composite graft in terms of functional and anatomic results has been studied. The perforation closure and air bone gap closure was reported to be successful 15. In a systematic review on 1,475 patients comparing cartilage and fascia graft in TPL, no statistically significant difference between cartilage and temporalis fascia regarding function and hearing outcome was reported. In addition, TPL using cartilage with or without perichondrium was reported to have better morphological outcomes than TPL using temporalis fascia 16.
Cartilage grafts may be used in different ways, such as perichondrium cartilage island graft, palisade or shield graft and cartilage reinforcement techniques 4 5. The use of cartilage as shield graft in tympanic membrane reconstruction is an easily applied technique, and is recommend by many authors 17. The reconstructed membrane will have resistance against the negative middle ear pressure, and long term integrity will be provided. Cartilage graft is mostly preferred in the posterosuperior retraction pockets of TM, since recurrent retractions are observed with the use of fascia graft over time 18.
The cartilage graft may be harvested from tragus or concha. We prefer the tragal cartilage, because of its flat surface, ideal thickness and sufficient size. It was used as cartilage island graft with the perichondrium attached to one side, since its thickness is less than 1 mm.17
Guneri et al. 3 reported a mean gain of 20 dB (64%) in a retrospective clinical study presenting their experience with cartilage grafts in ear surgery; postoperative hearing levels were improved in all type III tympanoplasties with ossicular reconstruction without mastoidectomies (100%), followed by CWD tympanomastoidectomy with ossicular reconstruction (66%), type I TPL (62%), and ICW tympanomastoidectomy with ossicular reconstruction (25%).
Cavaliere et al. 7 reported their personal experience with "tragal cartilage shield" graft in TPL with 306 adult patients. Graft take was achieved in 304 patients (99.35%) and there was no immediate post-operative complication. The overall preoperative PTA-ABG was 43.79 ± 7.07 dB, whereas it was 10.43 ± 5.25 dB at one year after the surgery. Conchal cartilage, shaped as a shield, was used to replace the entire tympanic membrane and reconstruct the ossicular chain in patients with an absent incus as type III cartilage "shield" TPL. It was reported as an effective technique for hearing improvement in selected patients with chronic otitis media 19.
Ozbek et al. 20 studied the long-term efficacy of cartilage palisades in TPL for atelectatic ears. The mean followup time was 44.5 months. The closure of tympanic membrane perforation was achieved in 91% of ears. Postoperative PTA-ABG was less than 20 dB in 71% of ears. The average preoperative and postoperative ABG values, including all types of tympanoplasty operations (type I, II and III), were 28.4 ± 5.8 and 16.9 ± 6.7 dB, respectively (p < 0.001). They concluded that palisade cartilage tympanoplasty was an effective technique for tympanic membrane closure and hearing improvement in atelectatic ears. They also indicated that the mastoidectomy did not affect anatomic or audiological outcomes.
The reported follow-up rates in the current literature are between 19.9 months and 12 years according to our search 3 7 20-22. Mean follow-up time was 68.64 months in the present study. It is a relatively long time period, compared with many studies in the literature.
Of the 41 ears with cholesteatoma, recurrent disease emerged in 2 patients after ICW procedures, which were managed successfully with CWD. The overall take rate was 91.24% for all patients; in type I, II, III TPL take rates were 92.12%, 91.11% and 86.36% respectively. No new reperforations occurred during follow-up period. The postoperative hearing results in our series showed an improvement in 76.29%, no change in 18.04% and a worsening in 5.67% of ears. Of the 11 ears whose hearing levels worsened postoperatively, 6 had primary CWD + Type II TPL and 5 had primary CWD + Type III TPL. Decreasing hearing levels may be due to the structural changes of middle ear during surgery.
Conclusions
Our study represents the results of PACG in type I, II and III primary TPL for treatment of COM with or without cholesteatoma. A limitation of study is the heterogeneity of the middle ear pathologies: we did not evaluate the effect of atelectasis, cholesteatoma and revision on the success rate of TPL. The inherent disadvantages of a retrospective study prevent formation of a true control group, and there may also be bias in selection of techniques. The overall graft take rate for PACIT was 91.24% at least 13 months after surgery. Postoperative PTA-ABG results demonstrated a significant improvement in our study for all types of TPL. The worsening hearing results were observed in the ears that underwent CWD due to cholesteatoma. This situation may depend on the structural changes of middle ear during surgery, rather than the type of graft used for tympanic membrane reconstruction. A cartilage island graft with the perichondrium attached to one side harvested from tragus may be useful in type I, II and III TPL due to high stability and good hearing results.
References
- 1.Wolferman A, Farrior JB. Classification of tympanoplasty. Arch Otolaryngol. 1971;94:380–380. doi: 10.1001/archotol.1971.00770070572020. [DOI] [PubMed] [Google Scholar]
- 2.Kerr AG, Byrene JET, Smyth GDL. Cartilage homografts in the middle ear: longterm histologic study. J Laryngol Otol. 1973;87:1193–1199. doi: 10.1017/s0022215100078166. [DOI] [PubMed] [Google Scholar]
- 3.Güneri EA, Ikiz AO, Erdag TK, et al. Cartilage tympanoplasty: Indications, techniques and results. J Otol-Head Neck Surg. 2009;38:362–368. [PubMed] [Google Scholar]
- 4.Dornhoffer J. Cartilage tympanoplasty: indications, techniques and outcomes in a 1,000-patient series. Laryngoscope. 2003;113:1844–1856. doi: 10.1097/00005537-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Neumann A, Schultz-Coulon HJ, Jahnke K. Type III tympanoplasty applying the palisade technique: a study of 61 cases. Otol Neurotol. 2003;24:33–37. doi: 10.1097/00129492-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Wullstein H. Theory and practice of tympanoplasty. Laryngoscope. 1956;66:1076–1093. doi: 10.1288/00005537-195608000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Cavaliere M, Mottola G, Rondinelli M, et al. Tragal cartilage in tympanoplasty: anatomic and functional results in 306 cases. Acta Otorhinolaryngol Ital. 2009;29:27–32. [PMC free article] [PubMed] [Google Scholar]
- 8.Sheehy JL, Anderson RG. Myringoplasty. A review of 472 cases. Ann Otol Rhinol Laryngol. 1980;89:331–334. doi: 10.1177/000348948008900407. [DOI] [PubMed] [Google Scholar]
- 9.Amedee RG, Mann WJ, Riechelmann H. Cartilage palisade tympanoplasty. Am J Otol. 1989;10:447–450. doi: 10.1097/00129492-198911000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Salen B. Myringoplasty using septum cartilage. Acta Otolaryngol. 1963;188:82–91. [PubMed] [Google Scholar]
- 11.Jansen C. Cartilage-tympanoplasty. Laryngoscope. 1963;73:1288–1302. doi: 10.1288/00005537-196310000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto E, Iwanaga M, Fukumoto M. Histologic study of homograft cartilage implanted in the middle ear. Otolaryngol Head Neck Surg. 1988;98:546–551. doi: 10.1177/019459988809800602. [DOI] [PubMed] [Google Scholar]
- 13.Hamed M, Samir M, El Bigermy M. Fate of cartilage material used in middle ear surgery light and electron microscopy study. Auris Nasus Larynx. 1999;26:257–262. doi: 10.1016/s0385-8146(99)00012-7. [DOI] [PubMed] [Google Scholar]
- 14.Heermann J. Autograft tragal and conchal palisade cartilage and perichondrium in tympanomastoid reconstruction. Ear Nose Throat J. 1992;71:344–349. [PubMed] [Google Scholar]
- 15.Khan MM, Parab SR. Primary cartilage tympanoplasty: our technique and results. Am J Otolaryngol. 2011;32:381–387. doi: 10.1016/j.amjoto.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Mohamad SH, Khan I, Hussain SS. Is cartilage tympanoplasty more effective than fascia tympanoplasty? A systematic review. Otol Neurotol. 2012;33:699–705. doi: 10.1097/MAO.0b013e318254fbc2. [DOI] [PubMed] [Google Scholar]
- 17.Gerber MJ, Mason JC, Lambert PR. Hearing results after primary cartilage tympanoplasty. Laryngoscope. 2000;110:1994–1999. doi: 10.1097/00005537-200012000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Couloigner V, Molony N, Viala P, et al. Cartilage tympanoplasty for posterosuperior retraction pockets of the pars tensa in children. Otol Neurotol. 2003;24:264–269. doi: 10.1097/00129492-200303000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Kyrodimos E, Sismanis A, Santos D. Type III cartilage "shield" tympanoplasty: an effective procedure for hearing improvement. Otolaryngol Head Neck Surg. 2007;136:982–985. doi: 10.1016/j.otohns.2006.12.025. [DOI] [PubMed] [Google Scholar]
- 20.Ozbek C, Ciftçi O, Ozdem C. Long-term anatomic and functional results of cartilage tympanoplasty in atelectatic ears. Eur Arch Otorhinolaryngol. 2010;267:507–513. doi: 10.1007/s00405-009-1084-7. [DOI] [PubMed] [Google Scholar]
- 21.Onal K, Arslanoglu S, Oncel S, et al. Perichondrium/cartilage island flap and temporalis muscle fascia in type I tympanoplasty. J Otolaryngol Head Neck Surg. 2011;40:295–299. [PubMed] [Google Scholar]
- 22.Velepic MM, Manestar D, Starcević R, et al. Full thickness cartilage palisade tympanoplasty with malleus interposition: a study of the long term results. Coll Antropol. 2014;38:283–287. [PubMed] [Google Scholar]