SUMMARY
The treatment of Bell's palsy (BP), based on steroids and/or antiviral drugs, may still leave a certain percentage of affected subjects with disfiguring sequelae due to incomplete recovery. The different procedures of physical rehabilitation have not been demonstrated to play a favourable role in this disorder. The aim of the present study was to compare functional outcomes in severe cases of Bell's palsy when treated by steroids alone or by steroids accompanied by Kabat physical rehabilitation. This prospective study included 94 subjects who showed sudden facial nerve (FN) palsy with House-Brackmann grade IV or V and who were divided into two groups on the basis of the therapeutic approach: one group (a) was treated by steroids, and the other (b) received steroids in combination with physical rehabilitation. Medical treatment consisted in administration of steroids at a dosage of 60 mg per day for 15 days; physical rehabilitative treatment consisted in proprioceptive neuromuscular facilitation according to Kabat, and was administered to one of the two groups of subjects. Recovery rate, degree of recovery and time for recovery were compared between the two groups using the Mann-Whitney and univariate logistic regression statistical tests (Ward test). Kabat patients (group b) had about 20 times the odds of improving by three HB grades or more (OR = 17.73, 95% CI = 5.72 to 54.98, p < 0.001) than patients who did not receive physical treatment (group a). The mean speed of recovery in group b was the half of that recorded for group a (non-Kabat subjects). No difference was observed in the incidence of synkineses between the two groups. Steroid treatment appears to provide better and faster recovery in severe cases (HB IV and V) of BP when complemented with Kabat physical rehabilitation.
KEY WORDS: Bell's palsy, Physical rehabilitation, Kabat, House-Brackmann grading system, Steroid treatment
RIASSUNTO
La terapia della paralisi di Bell, incentrata su farmaci steroidei e/o antivirali, può ancora far esitare nei soggetti affetti sequele disfiguranti per un recupero incompleto. Le diverse procedure riabilitative non si sono dimostrate al giorno d'oggi in grado di giocare un ruolo favorevole in questo senso. Scopo di questo lavoro è stato quello di mettere a confronto i risultati funzionali di pazienti affetti da forme severe di paralisi di Bell, quando trattati con solo cortisone con quelli nei quali al cortisone è stata affiancata una terapia riabilitativa secondo Kabat. Lo studio prospettico ha incluso 94 soggetti con paralisi di Bell di grado IV e V secondo House-Brackmann (HB) a loro volta suddivisi in due gruppi: (a) trattato con terapia steroidea; (b) trattato con terapia steroidea e riabilitazione Kabat. Il trattamento medico è consistito di 60 mg di prednisolone al giorno per 15 giorni; la terapia riabilitativa è consistita nel trattamento di facilitazione neuromuscolare propiocettiva secondo Kabat. Percentuale, grado e tempi di recupero sono stati comparati utilizzando l'analisi statistica Mann-Whitney e il test di regressione logistica multivariata (Ward test). I pazienti Kabat (gruppo b) hanno avuto 20 volte di più la possibilità di migliorare di 3 o più gradi HB (OR = 17,73, 95% IC = 5,72 a 54,98, p < 0,001) rispetto a quelli di gruppo a. La velocità media di recupero nel gruppo b è risultata la metà di quella registrata nel gruppo a. Nessuna differenza è stata invece riscontrata sull'incidenza di sincinesie. Si può dunque concludere che la terapia steroidea permette un migliore e più rapido recupero dei casi severi di paralisi di Bell, quando associata a terapia riabilitativa Kabat.
Introduction
Bell's palsy (BP) is an acute, sudden unilateral peripheral paralysis of the facial nerve (FN) that accounts for almost 75% of all acute facial palsies (FP). The annual incidence varies between 11 and 40 cases per 100,000 subjects 1 2 or even higher, as indicated by a recent survey 3.
The aetiology of BP is still unknown, but reactivation of a latent Herpes simplex virus would seem to play a major role 4. Inflammation and entrapment of the nerve in the narrow bony labyrinthine segment of the Fallopian canal have specifically been proposed as possible mechanisms for inducing nerve sufferance 4 5.
The therapeutic options are not universally accepted in terms of priority. Medical treatment is based on administration of corticosteroids, and several studies have shown that they may be able to reduce the time of recovery and occurrence of sequelae 6 7, while no evidence has been gathered on the adjunctive role of antiviral drugs 7.
Surgical decompression of the FN has also been proposed in the past, with the rationale to release the edematous nerve from its bony canal, but its efficacy has been recently debated 8 and, in recent years, the number of these procedures has drastically reduced.
Several procedures of FN rehabilitation have also been applied in combination with medical treatment, mostly in the post-surgical FP setting, although a recent Cochrane review was unable to identify any significant benefit or harm by any type of rehabilitative procedure 9. When analysing physical rehabilitative procedures, the recent scientific contributions have examined the application of manual therapies 10-12, electrical stimulation 13, exercises and, ago-puncture 14 15 and laser 16. Barbara et al. compared clinical outcomes and ENoG values of patients affected by BP and rehabilitated with the Kabat method 17, showing that the better and faster recovery of an early rehabilitative protocol was independent of the nerve condition as assessed by ENoG findings 18.
The purpose of the present study was to shed light on the favourable role played by Kabat physical rehabilitation in the outcomes of subjects affected by severe BP. Clinical outcomes were compared between two different protocols: pharmacological treatment associated with physical rehabilitation and pharmacological treatment alone.
Materials and methods
A series of consecutive subjects admitted to the Emergency Department (ED) of a tertiary University Hospital with diagnosis of BP during the years 2005-2012 were considered. In all, FN palsy was graded according to the House- Brackmann (HB) system 19. From a total of 390 patients, only those staged HB IV or higher were taken into consideration. Pregnant women and individuals with involvement of other cranial nerves were also excluded from the study. Ninety-six patients, hence composing the study group, were enrolled: HB IV (66 subjects) and HB V (28 subjects).
Randomisation of these patients was performed by the personnel working at the ED that, on the basis of individual judgment on the FN severity, sent 66 BP patients home and 28 to our FN Center for consultation. In this way, two separate groups were identified:
study group a, formed by 66 patients, aged 16-90 years (mean = 57.1), 30 females and 36 males, 58 with HB IV and 8 with HB V. All these subjects were sent home by the ED with medical steroid protocol treatment, eye drops for eye protection and paracetamol in case of pain;
study group b, formed by 28 patients, aged 32- 74 years (mean = 55.7), 13 males, 15 females, 10 with HB IV and 18 with HB V. All these patients were sent for consultations to our FN Centre by ED staff. At our Centre, standard facial movements (brow lift, gentle eye closure, forced eye closure, snarling, smiling and lip pucking) were documented in each patient by video-recording with a mobile phone, and reviewed by a senior ENT to assign the appropriate HB grade. The Kabat physical rehabilitation was started within 7 days from BP onset, and was associated for two weeks with medical treatment, consisting of daily prednisolone (2 mg/kg), for 10 days and tapered off within 2 weeks.
Group b subjects were evaluated at our Centre twice a week, during the rehabilitation sessions and at the end of the cycle, defined with the maximum improvement of FN function that remained stable for a least 1 month of follow-up. Once a week from FP onset, group b patients were re-evaluated, so as to define the progression or eventual recovery in days via direct clinical observation.
At day 7 from FP onset, group a subjects received a telephone contact and were classified according to the capability of eye closure, so as to distinguish grade III or better from grade IV or worse. Next, they were asked to self-assess and report in a diary, from that day on, facial features such as:
symmetry of the face at rest: if the right and left sides of the face appeared similar at rest (without any movement);
facial motion through different facial movements (brow lift, gentle eye closure, forced eye closure, snarling, smiling and lip picking).
Kabat rehabilitation consists in the facilitation of the voluntary response of an impaired muscle through the global pattern of an entire muscular section that undergoes resistance. This method appears to be extremely rational for facial muscles, since most of the face muscular fibers run diagonally, with easy irradiation to the upper facial region due to the cross-FN innervations. Three regional fulcra were taken into consideration: upper, intermediate and lower fulcrum. The first (forehead and eyes) is connected via a vertical axis to the intermediate one (nose), while the lower mimic-chewing-articulatory fulcrum lies along the horizontal axis. Hence, action on the upper fulcrum also involves the other two fulcra. The manipulation of these three fulcra is carried out by utilising both contralateral contractions and basic propioceptive stimulation, including stretching, maximal resistance, manual contact and verbal input. In the upper fulcrum, the activation of the frontal, corrugators and orbicularis muscles is carried out by their upwards or downwards traction, which is always in a vertical plane depending on the specific function that needs to be activated. In the intermediate fulcrum, activation of the common elevator muscle of the ala nasi and the upper lip is also carried out using traction movements, in this case contrary to the normal direction, following a vertical line. For the lower fulcrum, the maneuvers are carried out on the risorium and orbicularis oris muscles in a horizontal plane, and on the mental muscle in a vertical plane.
For statistical purposes, the time of recovery has been expressed in days. The time of recovery and the final HB degree of palsy were compared between groups.
Statistical analysis
The dataset was cleaned before analysis with respect to inconsistent and missing values, duplicates, outliers, digit preference and normality of continuous variables. The non-parametric Mann-Whitney-Wilcoxon (MWW) U test was used to verify the null hypothesis that the two study groups are the same against an alternative hypothesis, namely that one group would tend to have better recovery values than the other. Univariate logistic regression (Ward test) was used to compare all rehabilitated (group b) and non-rehabilitated (group a) patients for the final grade of improvement, degree of improvement (1-grade, 2 grades, 3 grades and 4-grades) and timing of recovery. The effect of treatment was evaluated by three different approaches, adjusted for age and gender: i) multiple linear regression to model the paired change of HB grade between before and after treatment (at the end of follow-up); ii) multiple logistic regression to model the chances of having a paired decrease in disease status by three HB grades or more, before and after treatment (at the end of follow-up); iii) multiple Cox proportional hazards regression for time of improvement (speed of recovery), with follow-up time in days (information about patient status was retrieved daily). Statistical assumptions underlying the tests were systematically checked.
Results
Grade IV at baseline was recorded in 87.9% of group a and in 35.7% of group b. Grade V at baseline was present in 12.1% of group a and 64.3% of group b. Group b subjects with grade V at baseline underwent Kabat treatment and showed better improvement after treatment with a faster recovery time in comparison with group a (64.6 days in respect to 117.1 days in group a). Moreover, at the end of follow-up, in group b there was no case of one-grade improvement, while an improvement by four grades was found in 25.0% of subjects; in group a, one-grade improvement was observed in 16.7% of patients, and none showed a four-grade improvement (Table I).
Table I.
Sample description by categories of treatment strategy.
| Non-Kabat (n = 66) |
Kabat (n = 28) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean or proportion |
SD | Min | Max | Mean or proportion |
SD | Min | Max | p* |
| Age | 56.8 | 17.9 | 16 | 90 | 55.8 | 12.7 | 32 | 74 | 0.778 |
| Male | 54.5% | 57.1% | 0.817 | ||||||
| HB V at onset | 12.1% | 64.3% | < 0.001 | ||||||
| Synkineses after treatment | 12.1% | 7.1% | 0.479 | ||||||
| Time to first improvement (days) | 117.1 | 90.3 | 34 | 365 | 64.6 | 50.7 | 12 | 194 | |
| Grade improvement † at the end of follow-up | 2.0 | 0.6 | 1 | 3 | 3.0 | 0.7 | 2 | 4 | <0.001 |
| 1-grade improvement | 16.7 | 0.0 | |||||||
| 2-grades improvement | 69.7 | 28.6 | |||||||
| 3-grades improvement | 13.6 | 46.4 | |||||||
| 4-grades improvement | 0.0 | 25.0 | |||||||
P values were computed using univariate logistic regression (Wald test) with Kabat as outcome.
Negative values indicate improvement, i.e. decrease in grade.
Improvement means decrease in grade after treatment.
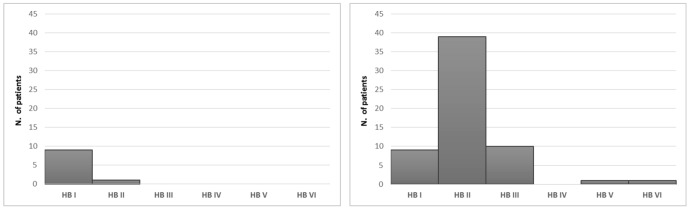
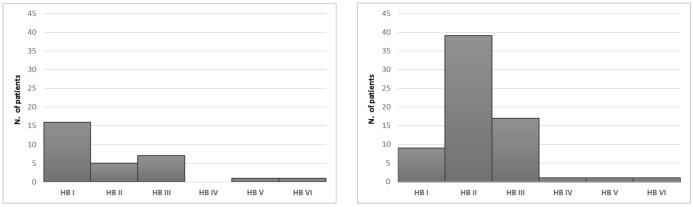
When comparing (MWW) the rehabilitated (group b) versus non-rehabilitated (group a) groups, independently of the initial FP grade, significant differences were found (p = 0.009546) and shown in Figure 1. With respect to the entire study group, a greater significance between the two modalities of treatment was identified when taking into account individually grade IV (p = 0.0001349) and grade V subjects (p = 0.009025) (Fig. 2 and 3).
Fig. 1.
Comparison between rehabilitated and non-rehabilitated groups (Mann-Whitney (U-test), HB IV and V together, independently of the severity of facial palsy at onset. A significant difference in the outcome was found between groups (p = 0.009546).
Fig. 2.
Comparison between rehabilitated and non-rehabilitated groups (Mann-Whitney (U-test) in HB IV subjects, independently of the severity of facial palsy at onset. A significant difference in the outcome was found between groups (p = 0.0001349).
Fig. 3.
Comparison between rehabilitated and non-rehabilitated groups (Mann-Whitney (U-test), in HB V subjects, independently of the severity of facial palsy at onset. A significant difference in the outcome was found between groups (p = 0.009025).
The multiple linear regression model for the change in HB grade after treatment is reported in Table II. With respect to group a, in the rehabilitated group (b) the HB grade decreased by one further point (coefficient = -0.99%, 95% CI = -1.27/1.71, p < 0.001), in HB IV (coefficient = 0.86, 95% CI = -1.23/0.49, p < 0.001) and in HB V ((coefficient = -1.10, 95% CI = -1.82/0.38, p < 0.005).
Table II.
Multiple linear regression model for the change in disease grade after treatment.
| Study group (n = 94) |
Grade IV at onset (n = 68) |
Grade V at onset (n = 26) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Change difference* |
95% CI | p | Change difference* |
95% CI | p | Change difference* |
95% CI | p |
| Kabat | -0.99 | -1.27, -0.71 | < 0.001 | -0.86 | -1.23, -0.49 | < 0.001 | -1.10 | -1.82, -0.38 | 0.005 |
| 10-years increase in age | 0.05 | -0.03, 0.13 | 0.206 | 57.1% | 0.01, 0.17 | 0.029 | -0.06 | -0.29, 0.16 | 0.56 |
| Male | -0.02 | 0.888 | 64.3% | -0.32, 0.21 | 0.698 | 0.08 | -0.58, 0.74 | 0.80 | |
Negative values indicate improvement, i.e. decrease in grade * All patients who had an improvement by three grades or more were treated with Kabat.
Group b patients showed about 20 times the odds of improving by three HB grades or more (OR = 17.73, 95% CI = 5.72 to 54.98, p < 0.001) than group a (Table III). Group b HB IV patients had 65 times the odds of a three-grade improvement than those in group a (non rehabilitated), while a three-grade improvement was only observed in HB V patients in group b. The mean speed of recovery in group b was half of that recorded in group a (HR = 2.19, 95% CI = 1.37 to 3.51, p = 0.001). Group b HB IV patients had seven times shorter times of recovery than similar grades of group a (HR = 7.92, 95% CI = 3.68 to 17.04, p < 0.001). Group b HB V patients showed nearly half shorter time of recovery than the same grade in group a (HR = 1.80, 95% CI = 0.65 to 5.01, p = 0.26) (Table IV). The incidence of synkineses after treatment was 7.1% in group b and 12.1% in group a, no statistical difference (p = 0.479).
Table III.
Multiple logistic regression model for the chances of having a decrease by three grades or more after treatment.
| Study group (n = 94) |
Grade IV at onset (n = 68) |
Grade V at onset (n = 26) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p |
| Kabat | 17.73 | 5.72, 54.98 | < 0.001 | 64.25 | 0.65, 660.41 | < 0.001 | N/A* | ||
| 10-years increase in age | 0.76 | 0.54, 1.08 | 0.122 | 0.65 | 0.42, 1.01 | 53 | 1.37 | 0.55, 3.38 | 0.500 |
| Male | 0.64 | 0.21, 1.93 | 0.443 | 0.48 | 0.11, 2.03 | 319 | 0.62 | 0.09, 4.31 | 0.631 |
All patients who had an improvement by three grades or more were treated with Kabat.
Table IV.
Multiple Cox proportional hazards model for time to first improvement (speed of recovery).
| Study group (n = 94) |
Grade IV at onset (n = 68) (n = 68) |
Grade V at onset (n = 26) (n = 26) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p |
| Kabat | 2.19 | 1.37, 3.51 | 1 | 7.92 | 3.68, 17.04 | < 0.001 | 1.80 | 0.65, 5.01 | 0.260 |
| 10-years increase in age | 0.85 | 0.74, 0.97 | 0.013 | 0.81 | 0.69, 0.94 | 6 | 0.93 | 0.67, 1.28 | 0.642 |
| Male | 1.61 | 1.06, 2.47 | 0.027 | 1.44 | 0.86, 2.40 | 0.167 | 1.49 | 0.65, 3.40 | 0.346 |
Discussion
Evaluation of the actual efficacy of the different treatments of BP is generally biased by several factors, such as the high likelihood of complete spontaneous recovery, the initial time of treatment and steroid administration that is generally given in all cases. Although steroid treatment is considered the gold standard of medical therapy, the observation that a not insignificant number of BP subjects may retain some important sequelae has promoted the adoption of additional forms of treatment and several types of rehabilitative procedures have also been taken into consideration. Each rehabilitative procedure would theoretically work with specific targets and is tailored to the patient's need and time from FP onset. For instance, the exercises based on gross movements determine a massive and spread contraction of the muscular components of the face, but a high likelihood of synkineses may develop even in the presence of improvement in facial stiffness 11. Laser and biofeedback techniques are usually performed only when signs of recovery of face movements are observed 16 18. Moreover, neuromuscular retraining therapy, which focuses on motor control of facial movements triggered by different feedback stimulation and which is particularly indicated to prevent or treat synkineses, is not advised before three months of paresis 19. Likewise, mime therapy, which consists of massage, relaxation, inhibition of synkinesis, and co-ordination and emotional expression exercises, has been proposed only at a late stage of paresis, with no reports on its potential role when applied at an early stage 20.
After having positively experienced the role of physical Kabat rehabilitation in the jatrogenic or post-surgical forms of FP, when applied at an early stage 21, it seemed reasonable to perform a study in order to assess whether this type of protocol, which involves an early approach to the affected patient, could also work in BP patients presenting with a HB grade IV or worse. In fact, to our knowledge, studies comparing the effect of physical treatment to that of exclusive steroid treatment in BP are scanty. In the present study, the composition of the study groups was not achieved by randomisation, but by the individual attitude of the ED staff to either send patients home or to our attention for consultation, although the former protocol mostly included less severe cases. In both instances, all patients received steroid treatment, while the Kabat rehabilitation was only performed on subjects that were sent and followed directly at our Clinic and that formed study group b.
In the present study, only the most severe cases, i.e. HB IV and V subjects, were taken into account for the final evaluation. Through this methodology, it was possible to have comparable patients in the study groups, as well as in HB IV or V subjects separately, for assessment of the primary outcomes of the study, i.e. recovery time, final HB grade and probability to achieve a 3-grade HB improvement.
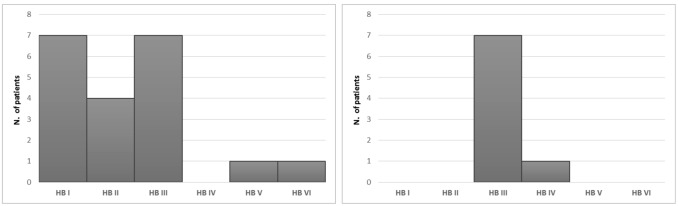
Although group a (steroids only) patients were numerically greater than those of group b, this latter included only the most severe HB grades and therefore all were addressed to rehabilitative treatment. The use of such physical rehabilitation led to a faster recovery time in group b, nearly half of that recorded in group a subjects, while for HB IV subjects it was reduced by seven times less than in group a. After physical rehabilitation, the degree of improvement (grade reduction at the HB) at the time of definitive clinical outcome was significant in comparison to the final condition of patients treated only with steroids, since patients treated simultaneously with pharmacological and rehabilitative therapy recovered in a significant number to normality (HB I), while in most of the patients who received only steroids, the maximum recovery was HB II.
When considering HB IV only, the significance value of difference between rehabilitated and non-rehabilitated cases was ten times less than that observed in the entire group (HB IV and V); the same finding was observed in HB V, with less significance than HB IV, due to a marked intersection of values at the HB III level. This is why in the most severe subjects (HBV), there was a prevalence of recovery to HB III in non-rehabilitated cases and to HBI in rehabilitated subjects.
Moreover, group b patients recovered by three grades two times more frequently than those in group a, and in group b the degree decreased, i.e. improved, by one further point, in total and single grades, compared to group a. In group b, moreover, a 20 fold higher probability of improvement by three HB grades was seen, and the most severe cases had similar improvement only when rehabilitated.
Most of the severe (HB V), non-rehabilitated patients reached as maximum result of HB III, while similar cases when undergoing Kabat rehabilitation could even obtain a normal facial function (HB I).
Conclusions
It is possible to conclude that, when Kabat rehabilitation is associated with standard steroid treatment in the case of severe BP, affected subjects may be likely to have a faster and better recovery than those in whom only medical treatment is applied. It would therefore be worthwhile to always include this type of physical rehabilitation in patients with BP, especially in the most severe cases which may carry the risk of disfiguring facial sequelae.
References
- 1.De Diego-Sastre JI, Prim-Espada MP. Fernàndez- Garcìa F. The epidemiology of Bell's palsy. Rev Neurol. 205;41:287–290. [PubMed] [Google Scholar]
- 2.Finsterer J. Management of peripheral facial nerve palsy. Eur Arch Otorhinolaryngol. 2008;265:743–752. doi: 10.1007/s00405-008-0646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monini S, Lazzarino AI, Iacolucci C, et al. Epidemiology of Bell's palsy in an Italian Health District: incidence and case-control study. Acta Otolaryngol It. 2010;30:198–206. [PMC free article] [PubMed] [Google Scholar]
- 4.Murakami S, Mizobuchi M, Nakashiro Y, et al. Bell's palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med. 1996;124:27–33. doi: 10.7326/0003-4819-124-1_part_1-199601010-00005. [DOI] [PubMed] [Google Scholar]
- 5.McCormick DP. Herpes-simplex virus as a cause of Bell's palsy. Lancet. 1997;1:937–939. doi: 10.1016/s0140-6736(72)91499-7. [DOI] [PubMed] [Google Scholar]
- 6.Engström M, Berg T, Stjernguist-Desatnik A, et al. Prednisolone and valaciclovir in Bell's palsy: a randomised, doubleblind, placebo-controlled, multicentre trial. Lancet Neurol. 1998;7:993–1000. doi: 10.1016/S1474-4422(08)70221-7. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan FM, Swan IRC, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell's palsy. New Eng J Med. 2007;357:1598–1607. doi: 10.1056/NEJMoa072006. [DOI] [PubMed] [Google Scholar]
- 8.McAllister K, Walker D, Donnan PT, et al. Surgical interventions for the early management of Bell's palsy. Cochrane Database Syst Rev. 2011;2:CD007468–CD007468. doi: 10.1002/14651858.CD007468.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Mosforth J, Taverner D. Physiotherapy for Bell's palsy. Br Med J. 1958;2:675–677. doi: 10.1136/bmj.2.5097.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flores PF, Medina RZ, Haro LG. Idiopathic peripheral facial paralysis treatment: physic therapy versus prednisone. [Tratamiento de la parálisis facial periférica idiopática: terapia física versus prednisona]. Revista médica del Instituto Mexicano del Seguro Social. 1998;36:217–221. [Google Scholar]
- 11.Manikandan N. Effect of facial neuromuscular re-education on facial symmetry in patients with Bell's palsy: a randomized controlled trial. Clin Rehabilitation. 2007;21:338–343. doi: 10.1177/0269215507070790. [DOI] [PubMed] [Google Scholar]
- 12.Alakram P, Puckree T. Effects of electrical stimulation on House-Brackmann scores in early Bell's palsy. Physiotherapy Theory Pract. 2010;26:160–166. doi: 10.3109/09593980902886339. [DOI] [PubMed] [Google Scholar]
- 13.Wang XH, Zhang LM, Han M, et al. Treatment of Bell's palsy with combination of traditional Chinese medicine and western medicine. Hua Xi Kou Qiang Yi Xue Za Zhi. 2004;22:211–213. [PubMed] [Google Scholar]
- 14.Zhou ZL, Zuo C, Cheng SL, et al. Application of grading evaluation on facial nerve function of Bell's palsy treated with electroacupuncture. Zhongguo Zhen Jiu. 2013;33:692–696. [PubMed] [Google Scholar]
- 15.Alayat MS, Elsodany AM, El Fiky AA. Efficacy of high and low level laser therapy in the treatment of Bell's palsy: a randomized double blind placebo-controlled trial. Lasers Med Sci. 2014;29:335–342. doi: 10.1007/s10103-013-1352-z. [DOI] [PubMed] [Google Scholar]
- 16.Kabat H, Knott M. Proprioceptive facilitation therapy for paralysis. Physiotherapy. 1954;40:171–176. [PubMed] [Google Scholar]
- 17.Barbara M, Antonini G, Vestri A, et al. Role of Kabat physical rehabilitation in Bell's palsy: a randomized trial. Acta Otolaryngol. 2010;130:167–172. doi: 10.3109/00016480902882469. [DOI] [PubMed] [Google Scholar]
- 18.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–147. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 19.Diels HJ, Combs D. Neuromuscular retraining for facial paralysis. Otolaryngol Clin North Am. 1997;30:727–743. [PubMed] [Google Scholar]
- 20.Barbara M, Monini S, Buffoni A, et al. Early rehabilitation of facial nerve deficit after acoustic neuroma surgery. Acta Otolaryngol. 2003;123:932–935. doi: 10.1080/00016480310000629. [DOI] [PubMed] [Google Scholar]
- 21.Beurskens CH, Heymans PG. Mime therapy improves facial symmetry in people with long-term facial nerve paresis: A randomized controlled trial. Aus J Physioth. 2006;52:177–183. doi: 10.1016/s0004-9514(06)70026-5. [DOI] [PubMed] [Google Scholar]