SUMMARY
The widespread use of dental implants and reconstructive procedures for their positioning has led to an increase in sinonasal complications of dental disease and treatment (SCDDT). Diagnosis requires accurate dental and rhinological evaluation, including computed tomography (CT). The aim of this study is to investigate a multidisciplinary approach for the treatment of SCDDT by combining endoscopic endonasal surgery (EES) and an intraoral approach on the basis of a preliminary classification system already proposed by other authors. Moreover, we analysed the percentage of odontogenic maxillary sinusitis extending to the anterior ethmoidal sinuses and bacteria involved in the pathogenesis of SCDDT. Between January 2012 and August 2015, in our series of 31 patients, 16/31 patients (51.6%) were treated with EES, 3/31 patients (9.7%) with an intraoral approach and 12/31 patients (38.7%) with a combined approach. All patients reported improvement in sinusitis symptoms confirmed by clinical examinations and CT scan. No significant complications were recorded and revision surgery was not required. Finally, the results of this preliminary study suggest that a multidisciplinary approach to SCDDT from diagnosis to therapy allows more precise diagnosis and comprehensive therapy to achieve a rapid recovery and minimise the risk of recurrence.
KEY WORDS: Odontogenic maxillary sinusitis, Chronic rhinosinusitis, FESS, Sinus floor elevation, Oral implant
RIASSUNTO
L'utilizzo diffuso degli impianti dentali e delle procedure ricostruttive per il loro posizionamento ha portato un aumento delle complicanze sinusali da patologia o trattamenti dentali (SCDDT). La diagnosi richiede una valutazione dentale e rinologica accurata, compresa la tomografia computerizzata (TC). Lo scopo di questo studio è stato quello di considerare un approccio multidisciplinare per il trattamento delle SCDDT, combinando la chirurgia endoscopica endonasale (EES) e l'approccio intraorale sulla base di un sistema di classificazione preliminare già proposto da altri autori. Inoltre, gli autori hanno analizzato la percentuale di sinusite mascellare a eziologica odontogena che si estende a interessare i seni etmoidali anteriori come anche i batteri coinvolti nella patogenesi delle SCDDT. Tra il gennaio 2012 e agosto 2015, nella nostra casistica di 31 pazienti, 16/31 pazienti (51,6%) sono stati trattati con approccio EES, 3/31 pazienti (9,7%) con approccio intraorale, e 12/31 pazienti (38,7%) con approccio combinato. Tutti i pazienti hanno riferito un miglioramento dei sintomi della rinosinusite, confermato attraverso i risultati degli esami clinici e della TC di controllo. Non è stata osservata nessuna complicanza significativa, né si è ricorsi a una revisione chirurgica. Infine, i risultati di questo studio preliminare suggeriscono che un approccio multidisciplinare delle SCDDT dalla diagnosi alla terapia permette una diagnosi più precisa e una terapia più esauriente, così da ottenere un rapido recupero, riducendo al minimo il rischio di recidiva.
Introduction
Sinonasal complications of dental disease and treatment (SCDDT) are a significant disorder of the paranasal sinuses 1-4 accounting for 10-12% of all cases of chronic maxillary sinusitis (CMS) 5-12. In recent publications, it has been reported that 30-40% of CMS cases are of a dental origin 12-14 and 8% of all EES are due to odontogenic aetiologies 14.
SCDDT occurs when the Schneiderian membrane is violated by conditions such as: a) oroantral fistulae (OAF) 8 9 15 16; b) chronic periapical odontogenic infections of the maxillary posterior teeth; c) odontogenic cystitis; d) iatrogenic factors including intraoral foreign bodies (dental fillings, tooth roots in traumatic extraction and parts of broken instruments); e) penetration of dental implants into the maxillary sinus; f) elevation of the sinus floor followed by dislocation of the grafting material and/or dental implant into the sinusal cavity 6 10 11-21; g) maxillary osteomyelitis or maxillary medication related osteonecrosis of the jaw (MRONJ) 15 22.
SCDDT deserves special consideration because it differs from other forms of rhinogenous sinusitis in terms of pathophysiology, microbiology, diagnosis and management 6 10 17. A close collaboration between ENT, oral and maxillofacial specialists is essential for accurate diagnosis and optimal treatment of both sinusitis and the odontogenic source.
Our study included 31 patients with SCDDT who underwent surgery between January 2012 and August 2015. Despite its limited nature, the aims of this preliminary study were: a) to apply a classification system proposed by Felisati et al. 1, partially modified by us (Table I), for surgical treatment of SCDDT combining endoscopic endonasal surgery (EES) and an intraoral approach where necessary; b) to analyse the percentage of odontogenic maxillary sinusitis extending to the anterior ethmoid sinuses and investigate the presence of anatomical variations from maxillofacial computed tomography (CT) scans; and c) to investigate the bacteria and fungi involved in the pathogenesis of SCDDT (Table II).
Table I.
Patient demographics. Preoperative symptoms, signs and radiological characteristics. The classification of Felisati et al. 12 has been used, modified by us for aetiologic factors and surgical treatment of SCOD (No. of patients = 31).
| ID | Name | Sex | Age | Preoperative symptoms and signs |
Radiological characteristics | Aetiologic factors and class |
Surgical Treatment |
|---|---|---|---|---|---|---|---|
| 1 | MG | M | 55 | FP + NO | MS + OMC | 3a (DCY) | Intraoral approach |
| 2 | CG | M | 69 | PR | MS + OMC + ES | 3b | EES |
| 3 | SG | F | 47 | FP | MS + OMC | ST | Intraoral approach |
| 4 | MA | M | 45 | FP + SC | MS + OMC + SD | 3b (DCY) | EES |
| 5 | SS | M | 70 | PR + BS + NO + PD | MS + OMC + ES + SD | 3b | EES |
| 6 | CR | M | 41 | FP + NO + SC | MS + OMC | 3a (DCY) | Intraoral approach |
| 7 | CL | F | 61 | BS + PD | MS + OMC + ES + FS | 2c | EES + implant removal |
| 8 | DF | F | 51 | PR + NO + PD | MS + OMC + PMT | 3b | EES |
| 9 | CC | M | 44 | FP + NO + SC | MS + MSS | 3b (DCY) | EES |
| 10 | BV | M | 50 | PR + BS + NO + PD | MS + OMC + ES + SD | 2c | EES + implant removal |
| 11 | BL | F | 45 | BS + NO + PD | MS + OMC + BE | 2c | EES + implant removal |
| 12 | BV | M | 60 | FP + SC | MS + CB | 2a | Combined: EES + implant removal + OAF repair |
| 13 | PM | F | 42 | FP + SC | MS + OMC + UP | 2a | Combined: EES + implant removal + OAF repair |
| 14 | CC | M | 73 | PR + BS + NO + PD | MS + OMC + ES | 2a | Combined: EES + implant removal + OAF repair |
| 15 | MR | F | 42 | PR + BS + NO + PD | MS + OMC + ES | 3b | EES |
| 16 | PM | F | 56 | FP + SC | MS + CB | 2a | Combined: EES + implant removal + OAF repair |
| 17 | VR | F | 35 | FP + SC | MS + OMC | 3a (DCY) | Combined: EES + Canine fossa approach with endoscopic aid |
| 18 | FL | M | 36 | PR+FP+BS+NO+PD+SC | MS + OMC + ES + FS | 3b | Combined: EES + tooths removal |
| 19 | CP | F | 39 | PR+FP+BS+NO+PD+SC | MS + OMC + ES | 1 | Combined: EES + infected material removal + OAF repair |
| 20 | GM | F | 36 | PR+BS+PD | MS+ES+CB+AEA | 3b | EES |
| 21 | FA | F | 37 | PR+BS+NO+PD | MS+OMC+ES+FS+AEA | 3b | EES |
| 22 | NS | M | 33 | PR+FP+BS+NO+PD+SC | MS + OMC + ES + MSS |
3b | EES |
| 23 | PR | F | 56 | PR + BS + NO + PD | MS + CB + BE + UP | 3b | EES |
| 24 | GR | F | 51 | PR + BS + NO + PD | MS + OMC + ES + CB | 1 | Combined: EES + infected material removal + OAF repair |
| 25 | AF | F | 72 | PR + FP | MS + OMC + PMT | 2a | Combined: EES + implant removal + OAF repair |
| 26 | PG | F | 59 | FP + SC | MS + OMC + SSS | 1 | EES + infected material removal |
| 27 | MM | F | 57 | PR + BS + NO + PD | MS + OMC + ES + FS | 1a | EES + infected material removal |
| 28 | OM | M | 74 | PR + BS + NO + PD | MS + OMC + ES | 2a | Combined: EES + implant removal + OAF repair |
| 29 | CLA | M | 30 | BS + NO + PD | MS + OMC | 1 | Combined: EES + infected material removal + OAF repair |
| 30 | PS | F | 51 | PR + BS + NO + PD | MS + OMC + ES+FS | 1a | EES+ infected material removal |
| 31 | OI | F | 75 | PR + FP + SC | MS+OMC+ES+FS+CB+MSS+SSS | 1 | Combined: EES + infected material removal + OAF repair |
Symptoms and signs: FP = facial pain; NO = nasal obstruction; PR = purulent rhinorrhea; SC = swollen cheek; BS = bad smell; PD = post-nasal drip. Radiological characteristics: MS = maxillary sinusitis; ES = ethmoidal sinusitis; FS = frontal sinusitis; OMC = obstruction of the ostiomeatal complex; SD = significant septum deviation; PMT = paradoxical middle turbinate; MSS = septated maxillary sinus; BE = hypertrophic ethmoidal bulla; CB= concha bullosa; SSS = silent sinus syndrome; PU = hypertrophic uncinate process; AEA = anterior ethmoidal artery. Etiologic factors and class: DCY = dentigerous cyst; ST = supernumerary tooth; 1 = sinusitis after maxillary sinus (MS) lift with oroantral fistulae (OAF) (+/– dislocation of grafting material in MS); 1a = sinusitis after MS lift without OAF (+/– dislocation of grafting material in MS); 2a = peri-implant osteitis with sinusitis; 2c = implant dislocation with sinusitis and without OAF; 3a = Bacterial or fungal sinusitis with OAF resulting from conventional dental treatment complications 3b = bacterial or fungal sinusitis resulting from conventional dental treatment complications. Surgical treatment: EES = endoscopic endonasal surgery; OAF = oroantral fistulae. Note: # 6, 10, 18, 21, 24, 26 and 27 are reported in Figs 1–7.
Table II.
Comparison between preoperative and intraoperative positive bacterial cultures and histological examination. Note: # 6, 18, 21, 24, 26 and 27 are reported in Figs 1-7.
| ID | Name | Preoperative bacterial culture |
Intraoperative bacterial culture | Histological examination |
|---|---|---|---|---|
| 1 | MG | Odontogenic cyst | ||
| 2 | CG | Fungal Hyphae | ||
| 3 | SG | Aspergillus | ||
| 5 | SS | Staphylococcus aureus (g+) | Sinonasal aspergillosis | |
| 6 | CR | Odontogenic cyst | ||
| 8 | DF | Streptococcus constellatus (g+) | Chronic rhinosinusitis | |
| 9 | CC | Mucocele | ||
| 14 | CC | Streptococcus intermedius (g+) | Chronic rhinosinusitis | |
| 18 | FL | Staphylococcus aureus (g+) | Streptococcus constellatus (g+) | Chronic rhinosinusitis |
| 21 | FA | Aspergillus | Fungal hyphae | |
| 23 | PR | Aspergillus | Aspergillus | |
| 24 | GR | Streptococcus parasanguinis (g+) | Heterologous bone | |
| 26 | PG | Strepto coccus intermedius (g+) |
Chronic rhinosinusitis | |
| 27 | MM | Staphylococcus epidermidis (g+) |
Streptococcus constellatus (g+) and Staphylococcus epidermidis (g+) |
Heterologous bone |
| 28 | OM | Staphylococcus aureus (g+) | Streptococcus intermedius (g+) | Chronic rhinosinusitis with nasal polyps |
| 29 | CLA | Osteoma | ||
| 30 | PS | Stenotrophomonas maltophilia (g-) |
Streptococcus anginousus (g+) | Chronic rhinosinusitis with nasal polyps |
| 31 | OI | Staphylococcus epidermidis (g+) | Chronic rhinosinusitis with nasal polyps + heterologous bone |
Fig. 2.
Patient 10. SCDDT resulting from implant dislocation (Class 2c). A) Coronal CT scan showing the implant inside the maxillary sinus, near the natural ostium but unable to be dragged in the ostiomeatal complex due to the small size of the natural ostium itself; B) Endoscopic endonasal surgery and implant removal.
Fig. 3.

Patient 18. SCDDT resulting from dental treatment complicated by bacterial sinusitis (Class 3b). A) Swelling on the left cheek and B) relevant purulent secretion in the middle meatal and olfactory cleft of the left side with a fetid purulent discharge, in a patient with C) dental caries and presence of dental pathology; D) Coronal CT scan showing complete obliteration of the left maxillary sinus and the anterior ethmoid cells as well as the obstruction of the frontal recess. Note the asymmetrical skull base; E) Nine-month postoperative coronal CT scan showing complete aeration of all paranasal sinuses; F) as well as the complete absence of swelling on the cheek. G, H) The postoperative endoscopic view 9 months after endoscopic endonasal surgery showing the appearance of the anterior ethmoidectomy, turbinoplasty of the middle turbinate and maxillary sinusotomy. I) Intraoral appearance of healing after teeth extraction.
Fig. 5.
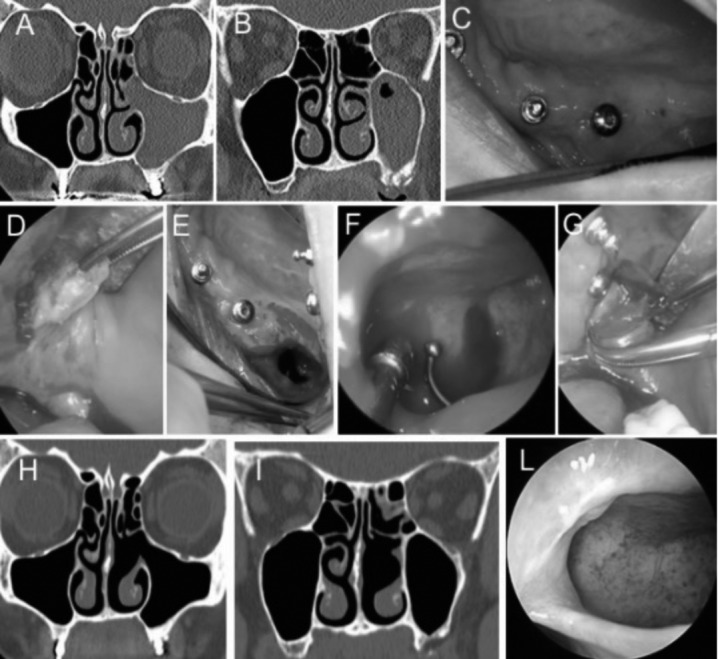
Patient 24. SCDDT resulting from maxillary sinus lift with OAF (Class 1). Preoperative coronal CT scans showing A) unilateral left maxillary sinusitis and obstruction of the ostiomeatal complex, and B) maxillary osteitis after bone graft in the posterior maxillary alveolar process; C) Preoperative intraoral view: no clinical evidence of infection; D) Intraoral approach with trapezoidal flap, and E) after bone graft removal and bone debridement; F) Intraoperative view showing a probe, inserted through the oroantral communication, visible from maxillary sinusotomy (45° endoscope); G) Buccal fat pad flap preparation, then Rehrmann buccal flap was used for pedicled buccal fat pad flap (PBFPF) covering; H, I) Control coronal CT scans, 6 months after surgery showing complete aeration of the maxillary and ethmoid sinuses on the left side as well as removal of the bone graft and its repair; L) Nasal endoscopy showing the maintenance of the maxillary sinusotomy and the absence of mucosal degeneration (45° endoscope).
Materials and methods
Between January 2012 and August 2015, 31 patients underwent surgery for SCDDT at the ENT Department in San Luigi Gonzaga Hospital, Turin, Italy (Table I). Eighteen patients were women (58.1%) and 13 were men (41.9%), aged from 30 to 75 years, with an average age of 51.3 (SD: 13.28), which is similar to that found by other authors 7 8 23. The male to female ratio was 1:1.4, similar to that reported in previous studies 7 10 12. Three patients underwent urgent surgery (# 18, 19, 22). The guidelines from the Helsinki Declaration were followed in this study, and informed consent was obtained from all patients.
All patients had a history of dental treatment and did not respond to medical therapy. Patients with a history of bilateral chronic rhinosinusitis, allergic rhinitis, or asthma, or OAF after tooth extraction without sinusitis, or those treated with only antibiotics after dental treatment were not included. We decided to limit fungal forms to only fungus balls by excluding invasive forms because these conditions are usually not of odontogenic origin. The interval from the dental procedure to first visit for symptoms was less 1 month in 3 patients (# 18,19,22) and 8-12 months for the remaining patients.
The suspected diagnosis of SCDDT was based on the presence of unilateral signs and symptoms of sinusitis, nasal endoscopy and oral examination. The definitive diagnosis was made by axial and coronal contiguous 1 mm CT scans, with post-processing sagittal CT scans 24 showing inflammation of the maxillary sinus, OAF, periapical lesions, dental roots, dental materials, implants, materials for sinus augmentation, or parts of broken instruments in the maxillary sinus. The diagnosis of anterior ethmoid sinusitis and/or the presence of anatomical variations was obtained from coronal CT scans. Recently, we have started using cone beam computed tomography (CBCT) to evaluate the dental cause of sinusitis, particularly in patients with peri-implant disease.
In the presence of peri-implant osteitis with sinusitis or other kinds of maxillary dentoalveolar infection associated with sinusitis or in presence of OAF, endoscopic endonasal surgery (EES) has been used along with an intraoral approach for the removal of infected bone or dental implants and the closure of oroantral communication. Therefore, by analysing the results of the literature, we have done is in accordance with what proposed by Felisati's classification.
Since August 2013, we implemented a standardised expert- team composed of ENT specialists and oral surgeons to resolve these pathologies with either EES alone, or a combination of EES and an intraoral approach.
Endoscopic endonasal surgery (EES)
With regards to these pathologies, EES not only has the objective of eliminating infection in the involved paranasal sinuses and removing infected grafting material from the maxillary sinus, but also removing any obstacle to correct sinus drainage and ventilation.
EES was performed under general anaesthesia with a local anaesthetic solution containing epinephrine to minimise bleeding. A rigid 0°, 4.0-mm endoscope (Karl Storz, Germany) was used to perform turbinoplasty of the middle turbinate, concha bullosa, or paradoxical middle turbinate. Then, an inferior uncinectomy was made and the natural ostium was identified. The ostium was enlarged in a postero-inferior direction to a size sufficient for clear visualisation of the maxillary sinus and for effective drainage after healing. SCDDT treatment generally requires a type II or III maxillary sinusotomy 25. Rigid 45° and 70°, 4.0-mm endoscopes (Karl Storz) were used for inspection and treatment of the inferior maxillary recess of the maxillary sinus and to allow the use of angled and curved instruments inside the sinus. In a type II sinusotomy, it is opened further posteriorly and inferiorly (< 2 cm diameter). In type III sinusotomy, the antrostomy is extended close to the level of the posterior wall of the maxillary antrum, anterior to the lacrimal sac, and inferior to the base of the inferior turbinate 25. In patients whose maxillary sinus infections were associated with ethmoidal cells, an anterior ethmoidectomy was performed with total removal of the uncinate process. Moreover, concomitant anatomical variations (significant septal deviation, concha bullosa, paradoxical middle turbinate, Haller's cell, hypertrophy of the uncinate process) were corrected to eliminate every possible obstacle to the recovery of sinus functionality, if present.
Intraoral surgery
The objective of the intraoral approach was to remove grafting material in the inferior portion and anterior recess of the maxillary sinus not reachable with endoscopy, remove necrotic bone, perform periapical endodontic surgery, and where necessary, close the oroantral communication by removing fistulae and performing a closure with local flaps.
When the EES had been completed, a full thickness buccal mucoperiosteal flap was prepared in the lateral-posterior maxilla according to the position of the OAF or infected implant allowing easy access to the alveolar process. In the case of maxillary osteitis or peri-implantitis, a meticulous revision of the alveolar process was performed using a diamond bur. In all cases, bone revision or implant removal led to an oroantral communication, and a local flap was used to close the communication with the maxillary sinus. Before suturing the flaps, an additional endoscopic control was performed and the maxillary sinus mucosa was washed with antibiotic solution (rifamycin). When the communication was very narrow (0.5-0.8 mm), a simple mucoperiosteal flap was used to close the communication and sutures were applied after careful flap mobilisation by periosteal incisions.
In the case of larger oroantral communication, a pedicled buccal fat pad flap (PBFPF) was used 22. The approach to the buccal fat pad was made by periosteal incision in the posterolateral region of the maxilla, and the fat pad was transferred onto the defect; after that, two or three holes were made in the lateral maxillary wall to secure the flap in the correct position without tension using a resorbable 3/0 suture. A trans-mucosal suture was then made to fix the flap on the palatal aspect. Finally, a mucosal flap was prepared to form a vestibular flap to cover the fat pad flap. A horizontal counter incision was made through the periosteum to release the mucosal flap and it was sutured over the PBFPF without tension. From the fifth postoperative day onward, physical therapy consisting of active mouthopening exercises is strongly recommended.
The hospitalisation period after surgery was 24 hours and nasal packaging was removed 48 h after surgery. All patients were instructed to: (i) follow antibiotic therapy (amoxicillin-clavulanic acid 2 g/day or levofloxacin 500 mg/day) before and after surgery, for 14 days total; (ii) administer saline nasal sprays and nasal wash with saline; (iii) apply nasal unguent for 60-90 days after surgery; (iv) optimise oral hygiene with chlorhexidine for 10-12 days until oral suture removal; (v) carry out physical therapy consisting of active mouth-opening exercises from the fifth postoperative day onward.
Results
The results of the study are shown in Tables I and II, and some clinical cases are presented in Figures 1-7.
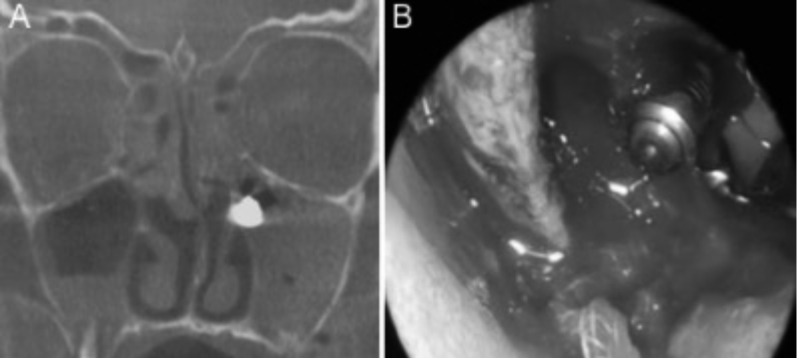
Fig. 1.
Patient 6. SCDDT resulting from odontogenic cyst (Class 3a). A) Coronal maxillofacial CT, and B) clinical examination showing a bulging of the upper gingiva caused by the cyst.
Fig. 7.
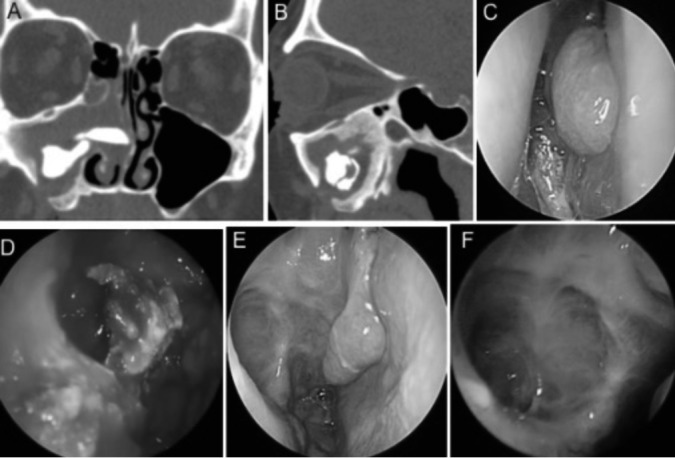
Patient 27. SCDDT as a result of elevation of the maxillary sinus floor with dislocation of grafting material (Class 1a). The patient was treated in 1990 for the elevation of the maxillary sinus floor. In 2007, three dental implants were added to the patient, which later were removed because of infection. The patient referred to us for a swollen cheek and unilateral purulent rhinorrhoea, without symptoms of OAF. She refused any oral procedures, and underwent EES. A, B) Coronal and sagittal CT scans showing filling material within the right maxillary sinus (MS), erosion of the inferior wall of the MS determined by the sinus floor lifting procedure and complete obliteration of both MS and the ostiomeatal complex; C) Purulent secretions in the middle meatal of the right nasal cavity; D) Removal of the grafting material used for sinus floor elevation and ethmoidectomy; E, F) Postoperative nasal endoscopy 5 months after surgery showing the restitutio ad integrum of the MS and the anterior ethmoid. Note the turbinoplasty of the middle turbinate.
Conventional dental treatment (class 3b) was the most common cause of SCDDT, found in nine patients (35.5%). Sinus floor elevation and grafting procedures with OAF (class 1) were present in five patients (16.1%), and without OAF (class 1a) in two patients (6.5%); peri-implant osteitis with sinusitis (class 2a) in six patients (19.4%); a odontogenic cyst (DCY) in five patients (16.2%) of which 3/5 with OAF (class 3a) while 2/5 without OAF (class 3b); implant dislocation with sinusitis and without OAF (class 2c) in three patients (9.7%); and a supernumerary tooth (ST) was present in one patient (3.1%).
Unilateral purulent rhinorrhoea was the most common presenting sign and symptom in 20 patients (64.5%), followed by nasal obstruction in 19 patients (61.3%), postnasal drip in 18 patients (58.1%), bad smell in 17 patients (54.9%), facial pain in 14 patients (45.2%) and swollen cheek in 12 patients (38.7%).
A paranasal sinus CT scan was carried out in all cases. In 16 of 31patients (51.6%), maxillary sinusitis was associated with anterior ethmoid sinusitis, in 4 of 31 patients (12.9%) maxillary sinusitis was associated with anterior ethmoid and frontal sinusitis, and in 16 of 31 patients (51.6%) concomitant anatomic variations were observed. Twenty-six of 31 patients (83.9%) presented obstruction of the ostiomeatal complex (OMC); in nine of 26 patients (35%), concomitant anatomic variations were observed. Saibene Am et al. 26 retrospectively evaluated 315 surgically treated SCDDT patients and in 18.7% have found bilateral involvement.
Sixteen of 31 patients (51.6%) were treated with EES; in 12 of 31 patients (38.7%), EES was combined with an intraoral approach, while the remaining 3 of 31 patients (9.7%) were only treated with an intraoral approach for removal of a large dentigerous cyst in two patients and a supernumerary tooth in the third patient. Anterior ethmoidectomy was performed in 16/31 (51.6%) patients whose maxillary sinus infection was associated with anterior ethmoidal cells. Cases affected by concomitant anatomical variations (16/31 patients) were treated to eliminate every possible obstacle to recovery of sinus functionality. Follow-up was performed with nasal endoscopy (rigid optic 0-45°, 3 mm) and scheduled at 1-3-5-8-12-16-24 weeks, and then after 1 year. No major intraoperative or immediate postoperative complications were observed in any patient, and no recurrences were observed during the follow-up period. A minor complication, nasal synechia, was seen in one case (# 14). Twenty-nine of 31 patients had CT scans about 4-5 months after surgery, which showed a significant improvement in line with clinical and radiological findings.
Preoperative bacterial culture, endoscopically obtained from the middle meatus with nasal swab, was performed on 20/31 patients with unilateral purulent rhinorrhoea. Bacteriological examination was positive in 8/20 patients (Table II), while it was negative on the remaining 12/20 patients.
Positive intraoperative cultures were obtained in eight patients, and new specific antibiotic therapies guided by antibiograms were prescribed. The predominant organisms identified using classic biochemical methods were Grampositive aerobes (Table II). No anaerobes were observed in our cases, while Saibene AM et al. reported the presence of anaerobes in 14% of cases 27.
Drago L et al. 28 recently described the identification of Dialister pneumosintes in a case of chronic maxillary sinusitis of odontogenic origin. D. pneumosintes is a known endodontic and periodontal pathogen found in necrotic pulp, subgingival plaque and deep periodontal pockets.
In agreement with other authors 23 29, the removed extramucosal material of fungal aspect was sent for histopathological analysis as well as a biopsy of the mucosal sinus wall (Table II). The biopsy of the mucosal sinus was done when a fungal infection was suspected in advance.
On the basis of histopathological results, the presence of extramucosal non-invasive fungal hyphae forms were found in five cases (# 2,3,5,21,23). In 3/5 cases, the causative agent was Aspergillus (Table II). Furthermore, other dental-related microbes caused by Actinomyces spp. can be found in histopathological examination 30. In no case was the biopsy of the mucosal sinus positive for fungal hyphae, but they were all non-invasive extramucosal fungal forms. Therefore, no local or general antifungal treatment was administered, as reported by other authors 27 31.
Discussion
The incidence of SCDDT is very low despite the high frequency of dental pathologies 8. In a meta-analysis by Arias-Irimia et al. 7, the most common cause of SCDDT was iatrogenic effects (55.97%) – extrusion of endodontic obturation materials in the maxillary sinus, amalgama remaining after apicoectomy, elevation of the sinus floor with poorly positioned dental implants or those which had migrated to the maxillary sinus with OAF – followed by periodontitis (40.38%) and dentigerous cysts (6.66%). In a retrospective study of 27 patients with SCDDT, Lee and Lee reported that implant related causes were the most common (37%), followed by dental extraction-related complications (29.6%) and dentigerous cysts (11.1%); radicular cyst, dental caries and a supernumerary tooth accounted for 7.4% of cases 8. In our study, the most common cause of SCDDT was conventional dental treatment in 29% of patients.
Classic symptoms of SCDDT can include unilateral purulent rhinorrhoea and nasal obstruction, bad smell and taste, hyposmia, headache, post-nasal drip and ipsilateral cheek pain 6 8 12. In a series of 21 patients with SCDDT, Longhini and Ferguson reported dental pain in only 29% of patients 13. In our study, 70.1% of patients complained of unilateral purulent rhinorrhoea as the main symptom.
The diagnostic work-up requires evaluation of symptoms, history of dental treatment, dental examination and nasal endoscopy. In addition, in the presence of unilateral purulent rhinorrhoea, we recommend preoperative and/ or intraoperative bacterial culture from the middle meatus under endoscopic guidance, so as to prescribe antibiotics guided by an antibiogram.
CT is the gold standard in the diagnosis of SCDDT due to its high resolution and ability to discern bone and soft tissue 17. It can show the relationship between the odontogenic origin and the maxillary sinus, foreign bodies within the maxillary sinus, opacification of the maxillary sinus and OMC, OAF, periapical lesions defined as a rounded lucency adjacent to the roots of a tooth, dental roots, dental materials, dental implants, material for sinus elevation, or parts of broken instruments in the maxillary sinus as well as the spread of inflammation into the other paranasal sinuses and anatomical variations 5 32 33. In the presence of suspected fungal balls on CT scans, magnetic resonance imaging (MRI) with gadolinium can also be useful (Fig. 4).
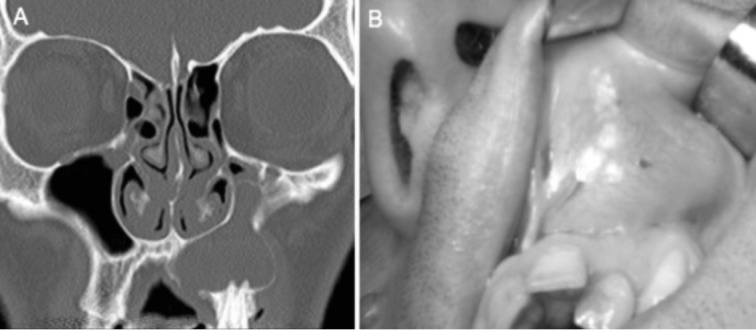
Fig. 4.
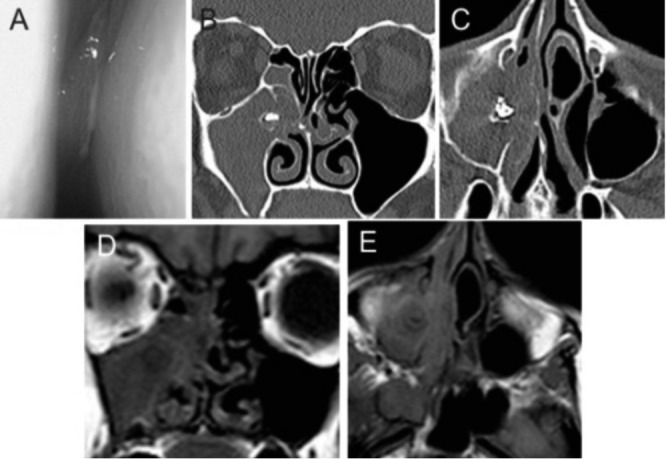
Patient 21. SCDDT resulting from dental treatment complicated by fungal ball sinusitis (Class 3b). A) Preoperative endoscopic view of purulent secretions in the right middle meatus; B, C) Coronal and axial maxillofacial CT scans showing radiodense material and erosion of bone in the right maxillary sinus indicative of aspergillosis with obstruction of the ostiomeatal complex; D, E) Coronal and axial T1 magnetic resonance image in the same patient showing iso- or hypointensity on T1-weighted images in the right maxillary sinus.
Previous studies have identified anterior ethmoid involvement during SCDDT without determining its prevalence 34 35. In our series, although limited, 16/31 patients (51.6%) also presented unilateral anterior ethmoid sinusitis, while 16/31 patients (51.6%) had anatomical variations so as to cause obstruction of the OMC.
However, Saibene AM et al. found in a retrospective study of 315 patients surgically treated for SCDDT that 18.7% of cases were affected by bilateral sinonasal involvement 26. Di Pasquale D et al. reported a case of bilateral odontogenic sinusitis after a bilateral maxillary sinus augmentation 36 similar to other authors 37.
Recently, cone beam computed tomography (CBCT) has been introduced in dental and maxillofacial imaging. It has several advantages over traditional CT including utilising approximately 10% of the radiation dose of conventional CT, higher resolution and is a chairside process 38. The technique is gaining popularity in the field of implant dentistry as there is frequently a need to assess the thickness of the floor of the maxillary sinus and to eliminate the presence of concurrent sinus disease before implantation.
However, at the moment, because of its high costs, CBCT, even if it allows examination of all paranasal sinuses and alveolar processes, is only complementary to traditional CT.
A combination of medical and surgical approaches is generally required for the treatment of SCOD. The Caldwell- Luc technique was the first to be described and used for SCDDT, while EES is a recent addition 9 21 39. Moreover, the Caldwell-Luc technique can induce sinusal sclerosis, atelectasis and hypoplasia of the maxillary sinus 40 as well as silent sinus syndrome (Fig. 6), infraorbital nerve damage, facial swelling, facial and teeth paraesthesia, OAF and recurrent sinusitis 40 41. In addition, the Caldwell-Luc operation is an absolute contraindication to performing sinus elevation 42.
Fig. 6.
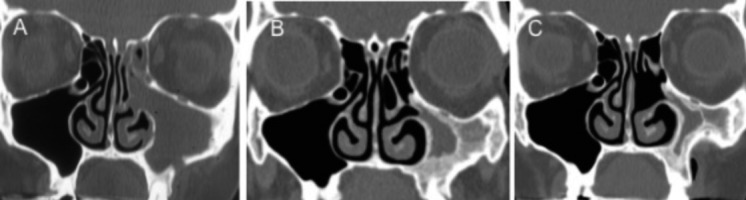
Patient 26. SCDDT resulting from possible complications in the Caldwell-Luc technique. A) Coronal CT scan after Caldwell-Luc technique and inferior meatotomy for left odontogenic sinusitis; B) Coronal CT scan 7 years after Caldwell-Luc technique showing atelectasis and sclerosis of the left maxillary sinus, hypoplasia and progressive enophthalmos in silent sinus syndrome.
Furthermore, the maxillary sinus has an effective mucociliary clearance to the natural ostium; this remains after EES through middle meatal antrostomy, but not after the Caldwell-Luc technique, because the artificial antrostomy is made in the inferior meatus 43. EES can be considered to be a relevant improvement for several reasons: (i) it is less invasive with low morbidity 34 40; (ii) it allows recovery of normal sinus function through spontaneous drainage from the natural ostium; (iii) it eliminates the need for total sinus mucosa removal, as originally proposed by Caldwell and Luc; (iv) it is possible to surgically manage the other paranasal cavities involved in the infection as well as that of widening the ostium and to treat anatomic variations that might contribute to normal ventilation of the OMC 44-46. Lopatin et al. 9 were the first to report 70 cases of SCDDT treated with EES, and since then, EES has been the surgical technique indicated in the treatment of this disease. In our series, 28/31 (90.3%) of patients were treated with EES or EES combined with oral surgery and none experienced any complications.
In accordance with the literature we wish to stress the importance of close collaboration between the implantologist, maxillofacial/oral and ENT specialists to treat complex cases of SCDDT, to distinguish osteitis or osteomyelitis of the alveolar process and to prevent recurrence and complications 47 48. In this regard, the surgical treatment for SCDDT as already reported in Felisati et al. classification 1 is represented in most cases by a multidisciplinary approach combining EES with an intraoral approach (Classes 1, 2, 3a). We have added subclass "1a" to include patients suffering from sinusitis after maxillary sinus lift without OAF, who request only EES.
In the combined approach, the intraoral approach, allows treatment of pathologies that are impossible to treat with EES only 1, such as: (i) removal of infected dental implants 49 with apical portions penetrating into the maxillary sinus or any other migrated material 50; (ii) foreign bodies or odontogenic cyst 51; (iii) removal of infected grafting material which can be more difficult to eliminate with endoscopy; (iv) maxillary osteitis or osteomyelitis; (v) periapical odontogenic infections of the teeth; (vi) dentigerous cysts; (vii) dental extraction-related complications; and (viii) the closure of OAF. In addition, OAF must be quickly closed as its persistence intensifies the possibility of inflammation of the sinus by infection from the oral cavity. Concerning the EES approach: (i) it is possible to surgically manage the paranasal cavities eventually involved in the infection, which are not reachable via an intraoral approach while preserving physiological sinonasal cavity function; (ii) it is possible to eliminate the anatomical variations that might contribute as co-factors to infection or obstruction of OMC; (iii) it is also possible to treat a foreign body, implant or grafting material dislocated into the sinusal cavity, fungus ball, or persistent maxillary sinus problems dependent on dental pathology under the control of rigid 4 mm, 45° and 70° angled endoscopes and a microdebrider with 40° curved blade, which are useful to treat the deepest regions of the maxillary sinus such as the alveolar recess. Furthermore, a one-step surgical procedure including simultaneously EES and a sinus floor elevation procedure through an intra-oral approach can be performed in selected cases. Thus, treatment of local contraindications to sinus augmentation can help prevent a second surgical procedure and a reduce the waiting period before final prosthetic rehabilitation 52-55.
Finally, a review of the current literature indicates that the results of treatment of SCDDT, where the most common causes are iatrogenic effects and periodontitis, have a high success rate in terms of healing (80-100%) with low complication rates (trigeminal neuralgia, orbital haematoma, visual disturbance, cerebrospinal fluid leak, nasal synechiae), recurrence (OAF, sinusitis) and revision surgery (< 10%) as well as a reduction in the time required for rehabilitation 9 18 21 34 39.
Conclusions
The possibility of SCDDT should always be considered when a patient has unilateral nasal symptoms that do not respond to medical treatment. Despite the limited number of cases treated on the basis of these preliminary satisfactory results, implantologist, maxillofacial/oral specialists and rhinological consultations are mandatory. The same is needed for an accurate diagnosis of infections of dental origin and associated sinusitis in SCDDT to resolve the odontogenic source and sinus infection in the shortest possible time without risking relapse.
The results of our study seem to be in accordance with the classification system proposed by Felisati, to which we referred. This could be useful in the standardisation of surgical treatment protocols, according to pathological conditions, to better harmonise cases reported by different authors. Nonetheless, we think that the number of the subgroups could be increased, especially for the pathological conditions included in Class 3.
Lastly, in our experience we can assert that EES must be associated with an intraoral approach whenever the maxillary alveolar process is affected by an infectious disease such as osteitis, osteomyelitis, peri-implant pathology, teeth periapical lesions, maxillary sinus lift complications, oroantral fistulae, or oroantral communication.
References
- 1.Felisati G, Chiapasco M, Lozza P, et al. Sinonasal complications resulting from dental treatment: outcome-oriented proposal of classification and surgical protocol. Am J Rhinol Allergy. 2013;27:101–106. doi: 10.2500/ajra.2013.27.3936. [DOI] [PubMed] [Google Scholar]
- 2.Saibene AM, Lozza P. Endoscopic sinus surgery and intraoral approaches in sinus oral pathology. J Craniofac Surg. 2015;26:322–323. doi: 10.1097/SCS.0000000000001223. [DOI] [PubMed] [Google Scholar]
- 3.Wang KL, Nichols BG, Poetker DM, et al. Odontogenic sinusitis: a case series studying diagnosis and management. Int Forum Allergy Rhinol. 2015;5:597–601. doi: 10.1002/alr.21504. [DOI] [PubMed] [Google Scholar]
- 4.Giovannetti F, Priore P, Raponi I, et al. Endoscopic sinus surgery in sinus-oral pathology. J Craniofac Surg. 2014;25:991–994. doi: 10.1097/SCS.0000000000000608. [DOI] [PubMed] [Google Scholar]
- 5.Mehra P, Jeong D. Maxillary sinusitis of odontogenic origin. Curr Allergy Asthma Rep. 2009;9:238–243. doi: 10.1007/s11882-009-0035-0. [DOI] [PubMed] [Google Scholar]
- 6.Brook I. Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg. 2006;135:349–355. doi: 10.1016/j.otohns.2005.10.059. [DOI] [PubMed] [Google Scholar]
- 7.Arias-Irimia O, Barona-Doraldo C, Santos-Marino JA, et al. Meta-analysis of the etiology of odontogenic maxillary sinusitis. Med Oral Patol Oral Cir Bucal. 2010;15:e70–e73. doi: 10.4317/medoral.15.e70. [DOI] [PubMed] [Google Scholar]
- 8.Lee KC, Lee SJ. Clinical features and treatments of odontogenic sinusitis. Yonsei Med J. 2010;51:932–937. doi: 10.3349/ymj.2010.51.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopatin AS, Sysolyatin SP, Sysolyatin PG, et al. Chronic maxillary sinusitis of dental origin: is external surgical approach mandatory? Laryngoscope. 2002;112:1056–1059. doi: 10.1097/00005537-200206000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Mehra P, Murad H. Maxillary sinus disease of odontogenic origin. Otolaryngol Clin North Am. 2004;37:347–364. doi: 10.1016/S0030-6665(03)00171-3. [DOI] [PubMed] [Google Scholar]
- 11.Kretzschmar DP, Kretzschmar JL. Rhinosinusitis: review from a dental perspective. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:128–135. doi: 10.1016/s1079-2104(03)00306-8. [DOI] [PubMed] [Google Scholar]
- 12.Patel NA, Ferguson BJ. Odontogenic sinusitis: an ancient but under-appreciated cause of maxillary sinusitis. Curr Opin Otolaryngol Head Neck Surg. 2012;20:24–28. doi: 10.1097/MOO.0b013e32834e62ed. [DOI] [PubMed] [Google Scholar]
- 13.Longhini AB, Ferguson BJ. Clinical aspects of odontogenic maxillary sinusitis: a case series. Int Forum Allergy Rhinol. 2011;1:409–415. doi: 10.1002/alr.20058. [DOI] [PubMed] [Google Scholar]
- 14.Hoskison E, Daniel M, Rowson JE, et al. Evidence of an increase in the incidence of odontogenic sinusitis over the last decade in the UK. J Laryngol Otol. 2012;126:43–46. doi: 10.1017/S0022215111002568. [DOI] [PubMed] [Google Scholar]
- 15.Racić A, Dotlić J, Janosević L. Oral surgery as risk factor of odontogenic maxillary sinusitis. Srp Arh Celok Lek. 2006;134:191–194. doi: 10.2298/sarh0606191r. [DOI] [PubMed] [Google Scholar]
- 16.Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 17.Simuntis R, Kubilius R, Vaitkus S. Odontogenic maxillary sinusitis: a review. Stomatologija. 2014;16:39–43. [PubMed] [Google Scholar]
- 18.Chiapasco M, Felisati G, Maccari A, et al. The management of complications following displacement of oral implants in the paranasal sinuses: a multicenter clinical report and proposed treatment protocols. Int J Oral Maxillofac Surg. 2009;38:1273–1278. doi: 10.1016/j.ijom.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Fusetti S, Emanuelli E, Ghirotto C, et al. Chronic oroantral fistula: combined endoscopic and intraoral approach under local anesthesia. Am J Otolaryngol. 2013;34:323–326. doi: 10.1016/j.amjoto.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 20.Tomomatsu N, Uzawa N, Aragaki K, et al. Aperture width of the osteomeatal complex as a predictor of successful treatment of odontogenic maxillary sinusitis. Int J Oral Maxillofac Surg. 2014;43:1386–1390. doi: 10.1016/j.ijom.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Costa F, Emanuelli E, Robiony M, et al. Endoscopic surgical treatment of chronic maxillary sinusitis of dental origin. J Oral Maxillofac Surg. 2007;65:223–228. doi: 10.1016/j.joms.2005.11.109. [DOI] [PubMed] [Google Scholar]
- 22.Berrone M, Florindi FU, Carbone V, et al. Medication-related osteonecrosis of the posterior maxilla: surgical treatment using a pedicled buccal fat pad flap: case reports. J Oral Maxillofac Surg. 2015;15:900–903. doi: 10.1016/j.joms.2015.06.165. [DOI] [PubMed] [Google Scholar]
- 23.Naghibzadeh B, Razmpa E, Alavi Sh, et al. Prevalence of fungal infection among Iranian patients with chronic sinusitis. Acta Otorhinolaryngol Ital. 2011;31:35–38. [PMC free article] [PubMed] [Google Scholar]
- 24.Manfrè L, Ferlito S, Conticello S, et al. A comparative study of the pterygopalatine fossa by computed tomography and magnetic resonance. Radiol Med. 1994;3:183–189. [PubMed] [Google Scholar]
- 25.Simmen D, Jones N. Indication for infundibulotomy and maxillary sinusotomy. In: Simmen D, Jones N, editors. Manual of endoscopic sinus and skull base surgery. Second Edition. Stuttgart, New York: Thieme; 2014. pp. 92–94. [Google Scholar]
- 26.Saibene AM, Pipolo GC, Lozza P, et al. Redefining boundaries in odontogenic sinusitis: a retrospective evaluation of extramaxillary involvement in 315 patients. Int Forum Allergy Rhinol. 2014;4:1020–1023. doi: 10.1002/alr.21400. [DOI] [PubMed] [Google Scholar]
- 27.Saibene AM, Vassena C, Pipolo C, et al. Odontogenic and rhinogenic chronic sinusitis: a modern microbiological comparison. Int Forum Allergy Rhinol. 2015 Sep 08; doi: 10.1002/alr.21629. [DOI] [PubMed] [Google Scholar]
- 28.Drago L, Vassena C, Saibene AM, et al. A case of coinfection in a chronic maxillary sinusitis of odontogenic origin: identification of Dialister pneumosintes. J Endod. 2013;39:1084–1087. doi: 10.1016/j.joen.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 29.Nicolai P, Mensi M, Marsili F, et al. Maxillary fungus ball: zinc-oxide endodontic materials as a risk factor. Acta Otorhinolaryngol Ital. 2015;35:93–96. [PMC free article] [PubMed] [Google Scholar]
- 30.Saibene AM, Pasquale D, Pipolo C, et al. Actinomycosis mimicking sinonasal malignant disease. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-200300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dufour X, Kauffmann-Lacroix C, Ferrie JC, et al. Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis. A retrospective analysis of 173 cases from a single medical center in France, 1989-2002. Med Mycol. 2006;44:61–67. doi: 10.1080/13693780500235728. [DOI] [PubMed] [Google Scholar]
- 32.Crovetto-Martinez C, Martin-Arregui FJ, Lopez-de-Maturana AZ, et al. Frequency of the odontogenic maxillary sinusitis extended to the anterior ethmoid sinus and response to surgical treatment. Med Oral Patol Oral Cir Buccal. 2014;1:409–413. doi: 10.4317/medoral.19629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Konen E, Faibel M, Kleinbaum Y, et al. The value of the occipitomental (Waters') view in diagnosis of sinusitis: a comparative study with computed tomography. Clin Radiol. 2000;55:856–860. doi: 10.1053/crad.2000.0550. [DOI] [PubMed] [Google Scholar]
- 34.Andric M, Saranovic V, Drazic R, et al. Functional endoscopic sinus surgery as an adjunctive treatment for closure of oroantral fistulae: a retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:510–516. doi: 10.1016/j.tripleo.2009.10.028. [DOI] [PubMed] [Google Scholar]
- 35.Stammberger H, Zinreich SJ, Koop W, et al. Surgical treatment of chronic recurrent sinusitis – the Caldwell-Luc versus a functional endoscopic technique. HNO. 1987;35:93–105. [PubMed] [Google Scholar]
- 36.Pasquale D, Saibene AM, Bebi V, et al. Calcifications afloat: bad omens in maxillary sinus augmentation. BMJ Case Rep. 2013 Dec 17; doi: 10.1136/bcr-2013-201581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Felisati G, Saibene AM, Lenzi R, et al. Late recovery from foreign body sinusitis after maxillary sinus floor augmentation. BMJ Case Rep. 2012 Dec 12; doi: 10.1136/bcr-2012-007434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nair UP, Nair MK. Maxillary sinusitis of odontogenic origin: cone-beam volumetric computerized tomography-aided diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e53–e57. doi: 10.1016/j.tripleo.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 39.Albu S, Baciut M. Failures in endoscopic surgery of the maxillary sinus. Otolaryngol Head Neck Surg. 2010;142:196–201. doi: 10.1016/j.otohns.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 40.Nemec SF, Peloschek P, Koelblinger C, et al. Sinonasal imaging after Caldwell-Luc surgery: MDCT findings of an abandoned procedure in times of functional endoscopic sinus surgery. Eur J Radiol. 2009;70:31–34. doi: 10.1016/j.ejrad.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 41.DeFreitas J, Lucent FE. The Caldwell-Luc procedure: institutional review of 670 cases: 1975-1985. Laryngoscope. 1988;98:1297–1300. doi: 10.1288/00005537-198812000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Bergh JP, Bruggenkate CM, Disch FJ, et al. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000;11:256–265. doi: 10.1034/j.1600-0501.2000.011003256.x. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy DW, Shaalan H. Reevaluation of maxillary sinus surgery: experimental study in rabbits. Ann Otol Rhinol Laryngol. 1989;98:901–906. doi: 10.1177/000348948909801112. [DOI] [PubMed] [Google Scholar]
- 44.Pignataro L, Mantovani M, Torretta S, et al. ENT assessment in the integrated management of candidate for maxillary sinus lift. Acta Otorhinolaryngol Ital. 2008;28:110–119. [PMC free article] [PubMed] [Google Scholar]
- 45.Testori T, Capelli M, Galli F, et al. Complications associated with maxillary sinus lift: diagnostic/therapeutic interdisciplinary consensus and clinical recommendations in reducing the incidence. Ital Oral Surg. 2011;10:139–140. [Google Scholar]
- 46.Fadda GL, Rosso S, Succo G, et al. Multiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. Acta Otorhinolaryngol Ital. 2012;32:244–251. [PMC free article] [PubMed] [Google Scholar]
- 47.Felisati G, Saibene AM, Pipolo C, et al. Implantology and otorhinolaryngology team-up to solve a complicated case. Implant Dent. 2014;23:617–621. doi: 10.1097/ID.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 48.Mantovani M. The ENT's role in sinus lift management doesn't need misleading messages. Acta Otorhinolaryngol Ital. 2012;32:404–404. [PMC free article] [PubMed] [Google Scholar]
- 49.Albu S. The 'double-barrel' approach to the removal of dental implants from the maxillary sinus. Int J Oral Maxillofac Surg. 2013;42:1529–1532. doi: 10.1016/j.ijom.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 50.Mantovani M, Pipolo C, Messina F, et al. Antral retriever and displaced dental implants in the maxillary sinus. J Craniofac Surg. 2011;22:2275–2277. doi: 10.1097/SCS.0b013e3182327125. [DOI] [PubMed] [Google Scholar]
- 51.Biglioli F, Goisis M. Access to the maxillary sinus using a bone flap on a mucosal pedicle: Preliminary report. J Craniomaxillofac Surg. 2002;30:255–259. doi: 10.1054/jcms.2002.0279. [DOI] [PubMed] [Google Scholar]
- 52.Felisati G, Borloni R, Chiapasco M, et al. Maxillary sinus elevation in conjunction with transnasal endoscopic treatment of rhino-sinusal pathoses: preliminary results on 10 consecutively treated patients. Acta Otorhinolaryngol Ital. 2010;30:289–293. [PMC free article] [PubMed] [Google Scholar]
- 53.Felisati G, Borloni R, Chiapasco M, et al. Reply to: "the ENT's role in sinus lift management doesn't need misleading messages". Acta Otorhinolaryngol Ital. 2013;33:47–48. [PMC free article] [PubMed] [Google Scholar]
- 54.Testori T, Drago L, Wallace SS, et al. Prevention and treatment of postoperative infections after sinus elevation surgery: clinical consensus and recommendations. Int J Dent. 2012;2012:365809–365809. doi: 10.1155/2012/365809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Colletti G, Felisati G, Biglioli F, et al. Maxillary reconstruction and placement of dental implants after treatment of a maxillary sinus fungus ball. Int J Oral Maxillofac Implants. 2010;25:1041–1044. [PubMed] [Google Scholar]


