SUMMARY
Arteriovenous malformation (AVM) of the head and neck is a rare and potentially life threatening entity due to massive haemorrhage. There are several indications for treatment, including age of the patient and location, extent and type of vascular malformation. Endovascular therapy can effectively cure most lesions with limited tissue involvement. Surgery can be used in selected cases in combination with embolization. Here we report the case of a young woman affected by a massive AVM on the left side of the mandible and submandibular region, and also review the literature on AVM with special attention to treatment strategies.
KEY WORDS: Arterio-venous malformation, Mandible, Submandibular region, Treatment
RIASSUNTO
Le malformazioni arterovenose (MAV) del distretto cervico-facciale sono patologie rare e potenzialmente letali a causa delle imponenti emorragie che possono determinare. Il trattamento dipende dall'età del paziente, dalla sede, dall'estensione e dalla tipologia della malformazione. La terapia endovascolare è efficace nella maggior parte dei casi che presentano un'estensione limitata. In casi selezionati, e sempre in associazione con l'embolizzazione, si può ricorrere alla chirurgia. Nel presente articolo riportiamo il caso di una giovane donna affetta da un'estesa MAV dell'emimandibola e della regione sottomandibolare sinistra. Viene inoltre effettuata una revisione della letteratura prodotta su questo argomento con particolare attenzione alla strategia di trattamento.
Introduction
According to Mulliken and Young, two types of vascular lesions can be recognized, which depend on the intrinsic properties of endovascular cells, namely haemangiomas and vascular malformations 1. Haemangiomas demonstrate endothelial hyperplasia and enlarge by cellular proliferation. Clinically, haemangiomas usually appear in early infancy, grow rapidly during the first months of life, then slowly involuting over 5 or 6 years 2 3.
Arteriovenous malformations (AVMs) in contrast to the abnormal proliferation of endothelial cells of a haemangioma, display progressive ectasia of abnormal vessels, lined by flat endothelium. AVMs occur as a result of errors in embryogenesis, are always present at birth, may manifest at any time during life and grow proportionately with the child 3 4. AVMs can be subdivided based on the rate of blood flow: "slow flow" (capillary, venous, lymphatic or mixed) and "fast flow" (arterial, arteriovenous, fistulae or shunt) subtypes 5. Vascular malformations are frequently seen in the skin, but rarely affect the visceral organs or bones; approximately 51% occur in the head and neck, with a malefemale ratio of 1 to 1.5. About 50% of all bone involvement occur in the skull and the maxillo-facial area 6 7.
Lesions of the mandible are rare and potentially lifethreatening entities that can present as innocuous episodes of gingival bleeding, slow-growing expansile masses, or severe haemorrhage. A biopsy or even a simple tooth extraction can cause a catastrophic bleeding that may even lead to death 8-12. However, the clinical course of malformations involving the mandible and the maxilla remains unclear and unpredictable. Treatment may be surgical or non-surgical. The latter includes intravascular embolization with coil and/or sclerosing solutions. Surgical resection is reserved for lesions that are extensive and/or refractory to endovascular therapy. Cure is defined as the complete eradication of disease or permanent resolution of symptoms with complete devascularization 8-16.
Herein, we report the case of a 23-year-old woman with an AVM of the mandible and submandibular region, and review the relevant literature, focusing on the best options for treatment.
Case report
In December 2009, a 23-year-old woman, after tooth extraction, presented at our ENT division with a massive haemorrhage from the left side of the mandible.
The bleeding was initially controlled by packing the mandible, and blood transfusions were required. The patient reported no malocclusion and no history of infection, and family history was also unremarkable. She was affected by insulin dependent diabetes mellitus. The only extraoral finding was a slight left facial swelling.
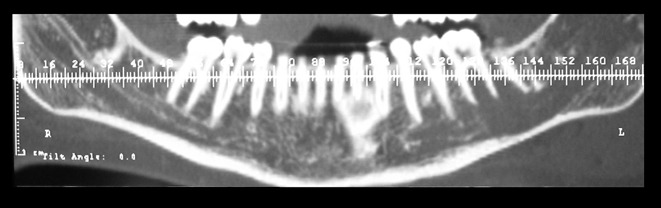
Retrospective analysis of the radiograms used for dental cure revealed the following. By panoramic radiograph, an extensive radiolucency in the left mandible involving the molar area (Fig. 1) was evident, while by dental scan, an abnormal enlargement of the left alveolar canal with integral cortical bone (Fig. 2) was present.
Fig. 1.
Extensive radiolucency in the left mandible by panoramic radiograph.
Fig. 2.
Abnormal enlargement of the left alveolar canal with integral cortical bone by dental scan.
In the subsequent, urgent surgical intervention, a temporary ligation of the external carotid artery was ineffectively attempted because of a large anastomotic blood supply. The haemorrhage was then controlled by filling the mandibular cavity with sheets of oxidized cellulose, taking advantage of the natural pathway created by the previous tooth extraction. A haemostatic suture of the alveolar mucosa was finally done.
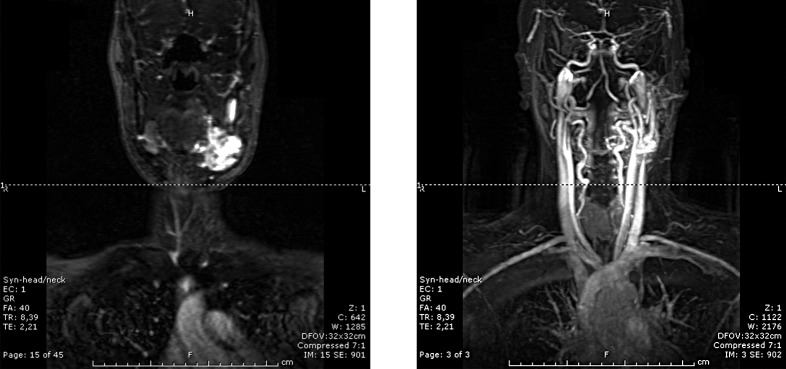
In the strong suspicion of a vascular malformation, the patient underwent head and neck magnetic resonance imaging (MRI) and magnetic resonance with angiography (MRA). The examination showed an extensive highly vascularized lesion involving the left side of the mandible and left submandibular region (Fig. 3).
Fig. 3.
MRI and MRA scans showing an extensive highly vascularized lesion involving the left side of the mandible and left submandibular region.
Ten days later, after the correction of severe diabetic decompensation, an angiography was performed. This study confirmed the diagnosis of arteriovenous malformation in the sites mentioned before, and associated with feeding vessels from the external carotid artery. Superselective coil embolization was performed of the facial artery, lingual artery and internal maxillary artery.
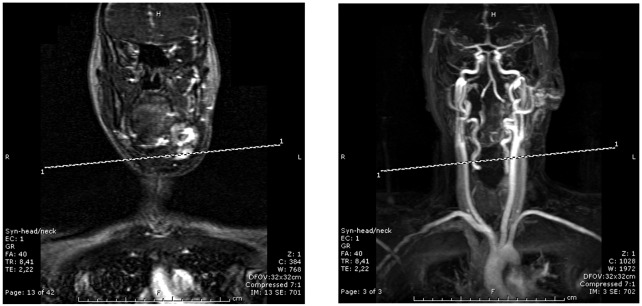
The day after, follow-up MRI and MRA revealed a subtotal closure of the AVM (Fig. 4).
Fig. 4.
Subtotal closure of the AVM on MRI and MRA performed the day after embolization.
Two days later, the patient underwent surgical intervention. Passing through the incision of the previous carotid ligation, we removed a large highly vascularized lesion occupying the left submandibular region and substituting the submandibular gland itself. From the empty alveolar ridge, the intraosseous component of the AVM was injected with sodium tetradecyl sulphate (3%). There was no damage to the mandibular branch of the facial nerve. There were no intraoperative complications, and the estimated blood loss was 500 ml. The postoperative period was uneventful, and the patient was discharged on the fifth postoperative day. The final histopatological diagnosis was arterio-venous malformation.
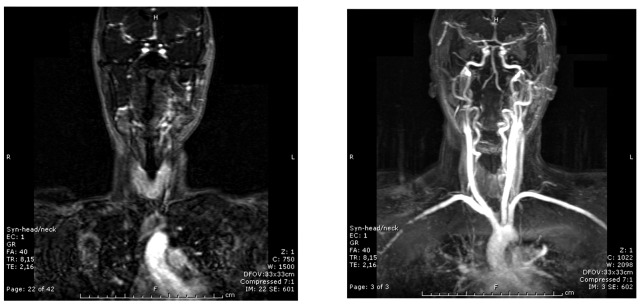
At the time of writing, after six months of follow-up, the patient has not experienced symptoms of trigeminal neuralgia. A minor bleeding episode was controlled with intraosseous injection of methylprednisolone acetate. Subsequently, no further episodes of bleeding were observed. Two months after the operation, post-surgical MRI and MRA showed an empty submandibular triangle and almost complete reabsorption of the AVM in the mandible (Fig. 5). Bone fractures and tissue necrosis or infection have not occurred.
Fig. 5.
Two months after intervention, post-surgical MRI and MRA showed an empty submandibular triangle and almost complete reabsorption of the AVM in the mandible.
Discussion
AVMs are extremely rare entities that can be life threatening if left untreated due to massive blood loss during tooth extraction or biopsy. Although rare, 50% of all intraosseous AVMs occur in the maxillo-facial region and are extremely infrequent in the mandible 17. Very few cases of extraosseous submandibular AVMs have been reported, with 6 cases cited in the literature (5 females and 1 male) 18-20. Our study confirms this trend. To our knowledge, this is the first documented case of a combined AVM involving both the mandible and the submandibular region. AVMs usually present with non-specific symptoms including bruit, dental loosening, swelling of soft tissues, change in skin and mucosal colour and dysesthesia of the lower lip or chin. Although CT, MRI and MRA may localize the arterio-venous shunt lesion, superselective arteriography remains an essential tool for diagnosis and planning of treatment 8-10 13 14. Management of AVMs is usually complex and requires a multidisciplinary team for successful outcome. Observation may be used as a temporary measure in special situations, such as extreme age, pregnancy or refusal of therapy. No spontaneous regressions have been documented. On the other hand, it has been reported that the volume of the lesion may gradually increase 9.
Arterial ligature was used in the past as a purely symptomatic treatment or before surgery. At present, it is well known that ligation of external carotid artery should not be performed, firstly as many anastomoses promote the rapid appearance of a collateral circulation, and secondly because future embolization would be impossible 9 10 13. In addition, in our experience, emergency ligation of the external carotid artery is insufficient to stop the haemorrhage because of a large and already developed network of anastomotic blood vessels.
At present, superselective angiographic embolization is considered first line treatment, alone or in combination with surgical approach to reduce intraoperative bleeding. Occlusion of the lesion is obtained using movable balloon, coils or liquid glue. Endovascular therapy as definitive treatment for the AVMs of the mandible has been reported to have a success rate of 70%. This avoids mutilating surgery and related sequelae, especially if AVMs occur before adolescence 8-10 13-16.
However, serious complications after embolization (e.g., occlusion of pulmonary or cerebral vessels) or recurrence of AVMs should be considered. In some cases, the procedure has to be carried out in several sessions such as previous history of arterial ligation or high flow characteristics of the lesion or microshunts, which are invisible during hyperselective catheterization and therefore inaccessible to treatment 9 11 13.
Therefore, intraosseous injection of sclerosing agents should be used to achieve further obliteration of the AVMs 16. In this case, we used sodium tetradecyl sulphate 3% which in our division is regularly employed to treat many different vascular lesions of the head and neck with a high cure rate and very low incidence of side effects.
Surgery is not the treatment of choice for AVMs of the mandible. Block resection of the affected area has been suggested, and temporary reconstruction with alloplastic bone plate or with the patient's own free, previously curetted mandibular segment has been reported. More definite bony reconstruction is recommended as soon as possible with a free fibular graft or iliac crest to avoid facial deformities and allow dental implantation 8-10 11 12 21.
In the past years, some authors have commented that radical surgical resection as in threating cancer 22 23. This has been tempered by acknowledgement that radical resection and reconstruction of an extensive benign vascular lesion of the maxillo-facial and mandibular area typically causes severe disfigurement with considerable morbidity. Furthermore, recurrences may occur even after radical resection, and relapses are reported to be even more difficult to treat 8.
On the other hand, surgical excision of AVMs involving soft tissues such as the submandibular space can be achieved without severe sequelae 18. No data on relapse have been reported for this very rare condition. According to the literature, we tailored treatment of the present case by performing superselective arterial embolization, leaving the intraosseous part of the AVM in situ and resecting only the part located in submandibular region. Surgery should always be performed after embolization, with a short interval between the procedures, based on the general recommendation that surgery should take place within 48 hours to 2 weeks to avoid revascularization of the lesion. In this period, we recommend MRI and MRA angiography studies to evaluate the effective devascularization of AVMs.
In conclusion, considering the present case and literature data, we can define the following general principles of treatment.
Arterial ligation should not be performed, even in emergency settings. Superselective arterial embolization is the treatment of choice and can be repeated in the case of relapse. Intraosseous injection of sclerosing agents can be used in the attempt to reduce the number of arterial embolizations. In AVMs of the mandible, surgery should be reserved only for cases that are refractory to endovascular therapy and/or for therapeutic complications that are not otherwise treatable (bone fractures and/or necrosis). In AVMs of the soft tissue, surgery could be used if there are no significant side effects. Lastly, the interval between embolization and surgery should be as short as possible, and MRI and MRA should be repeated before surgery.
References
- 1.Mulliken JB, Young AE. Vascular birthmarks: hemangiomas and malformations. WB Saunders; 1988. [Google Scholar]
- 2.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412–422. doi: 10.1097/00006534-198203000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Waner M, Suen JY. Management of congenital vascular lesions of the head and neck. Oncology. 1995;9:989–994. [PubMed] [Google Scholar]
- 4.Higuera S, Gorldey K, Metry DW, et al. Management of heamangiomas and pediatric vascular malformations. J Craniofac Surg. 2006;17:783–789. doi: 10.1097/00001665-200607000-00034. [DOI] [PubMed] [Google Scholar]
- 5.Hurwitz DJ, Kerber CW. Hemodinamic considerations in the treatment of arteriovenous malformations of the face and scalp. Plast Reconstr Surg. 1981;67:421–432. doi: 10.1097/00006534-198104000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Persky MS. Congenital vascular lesions of the head and neck. Laryngoscope. 1986;96:1002–1015. [PubMed] [Google Scholar]
- 7.Unni KK, Ivins JC, Beabout JW, et al. Hemangioma, hemangiopericytoma and hemangioendothelioma of bone. Cancer. 1971;27:1403–1414. doi: 10.1002/1097-0142(197106)27:6<1403::aid-cncr2820270621>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 8.Yoshiga K, Tanimoto K, Okui T, et al. High-flow arteriovenous malformation of the mandible: treatment and 7-year follow-up. Brit J Oral Maxillofac Surg. 2003;41:348–350. doi: 10.1016/s0266-4356(03)00132-3. [DOI] [PubMed] [Google Scholar]
- 9.Giauoi L, Princ G, Chiras J. Treatment of vascular malformations of the mandible: a description of 12 cases. Int J Oral Maxillofac Surg. 2003;32:132–136. doi: 10.1054/ijom.2002.0268. [DOI] [PubMed] [Google Scholar]
- 10.Sakkas N, Schramm A, Metzeger MC, et al. Arteriovenous malformation of the mandible: a life-threatening situation. Ann Hematol. 2007;86:409–413. doi: 10.1007/s00277-007-0261-2. [DOI] [PubMed] [Google Scholar]
- 11.Hohlweg-Majert B, Metzeger MC, Schramm A, et al. Complication of intraoral procedures in patients with vascular tumors. J Craniofac Surg. 2008;19:816–819. doi: 10.1097/SCS.0b013e31816aaba0. [DOI] [PubMed] [Google Scholar]
- 12.Shum JW, Clayman L. Resection and immediate reconstruction of a pediatric vascular malformations in the mandible: case report. Oral Surg Oral Med Oral Pathol Radiol Endod. 2010;109:517–524. doi: 10.1016/j.tripleo.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 13.Persky MS, Yoo HJ, Berenstein A. Management of vascular malformations of the mandible and maxilla. Laryngoscope. 2003;113:1885–1892. doi: 10.1097/00005537-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Benndorf G, Kim DM, Menneking H, et al. Endovascular management of a mandibular aeìrteriovenous malformation in a patient with severe hemophilia A. AJNR Am J Neuroradiol. 2004;25:614–617. [PMC free article] [PubMed] [Google Scholar]
- 15.Fan XD, Su LX, Zheng JW, et al. Ethanol embolization of arteriovenous malformation of the mandible. AJNR Am J Neuroradiol. 2009;30:1178–1183. doi: 10.3174/ajnr.A1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen W, Ye T, Xu L, et al. A multidisciplinary approach to treating maxillofacial arteriovenous malformations in children. Oral Surg Oral Med Oral Pathol Radiol Endod. 2009;108:41–47. doi: 10.1016/j.tripleo.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Mohammadi H, Said-al-Naief NA, Hetfez LB. Arteriovenous malformation of the mandible: report of a case with a note on the differential diagnosis. Oral Surg Oral Med Oral Pathol Radiol Endod. 1997;84:286–289. doi: 10.1016/s1079-2104(97)90344-9. [DOI] [PubMed] [Google Scholar]
- 18.Burns JC, Julian J, Alexander J. Arteriovenous malformation of the submandibular triangle. J Oral Maxillofac Surg. 1989;43:294–296. doi: 10.1016/0278-2391(85)90292-7. [DOI] [PubMed] [Google Scholar]
- 19.Fine MJ, Holliday RA, Roland JT. Clinically unsuspected venous malformation limited to the submandibular triangle: CT findings. AJNR Am J Neuroradiol. 1995;16:491–494. [PMC free article] [PubMed] [Google Scholar]
- 20.Stocks HM, Sacksman A, Thompson P, et al. First documented case of a submandibular arteriovenous malformation in a male patient. Am J Otolaryngol Head Neck Med Surg. 2007;28:275–276. doi: 10.1016/j.amjoto.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 21.Behnia H, Motamedi MHK. Treatment of central arteriovenous malformation of the mandible via resection and immediate replantation of the segment: a case report. J Oral Maxillofac Surg. 1997;55:79–84. doi: 10.1016/s0278-2391(97)90453-5. [DOI] [PubMed] [Google Scholar]
- 22.Azzolini A, Bertani A, Riberti C. Superselective embolization and immediate surgical treatment: our present approach to treatment of large vascular hemangiomas of the face. Ann Plast Urg. 1982;9:42–60. doi: 10.1097/00000637-198207000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Withers EH, Franklin JD, Lynch JB. Case report: resection of a massive arteriovenous malformation of the head and neck. Plast Reconstr Surg. 1979;63:566–569. doi: 10.1097/00006534-197904000-00028. [DOI] [PubMed] [Google Scholar]