Abstract
Background
There is no single approach that provides adequate exposure for treatment of all types of acetabular fractures. We describe our experience with an easier, relatively less invasive pubic symphysis approach (PSA) for the treatment of acetabular fractures.
Material/Methods
Between March 2011 and March 2012, fifteen patients with acetabular fracture underwent surgery using the PSA technique. Fracture reduction and treatment outcomes were assessed by clinical and radiological examination. Operation time, intraoperative blood loss and postoperative complications were documented.
Results
Mean operative time was 222±78 minutes. Average blood loss was 993±361 mL. Anatomical reduction was achieved in all patients. Minimum follow-up period was 31 months. Postoperative hypoesthesia in the area of innervation of the lateral femoral cutaneous nerve was reported in one patient, with spontaneous recovery at one month after surgery. No complications were reported during the follow-up period. At the most recent follow up, clinical outcomes were graded as “excellent” in six patients, “good” in eight patients and “fair” in one patient based on the modified Merle d’Aubigné-Postel score.
Conclusions
PSA appears to be a timesaving and safe approach for treatment of acetabular fractures that affords good visual access and allows for excellent fracture reduction. Our preliminary results revealed a much lower incidence of complications than traditional approaches, suggesting PSA is an alternative for treatment of acetabular fractures.
MeSH Keywords: Acetabulum; Bone Plates; Fracture Fixation; Fractures, Bone
Background
The Judet and Letournel classification provides a framework for the systematic, step wise approach to treatment of acetabular fractures [1,2]. However, there is no single approach that provides adequate exposure for treatment of all types of acetabular fractures [2,3]. The choice of surgical approach is based on variables like fracture pattern, direction of displacement, skin condition at the surgical incision site, and time elapsed since injury [2,4–7].
The ilioinguinal approach has been the preferred approach due to the pitfalls associated with the other approaches [8–10]. It has also been developed as an approach to the inner aspect of the innominate bone [11]. However, this approach is time consuming and involves a complex sequence of steps to obtain access through the four windows, and is associated with complications such as thrombosis, lymphedema, hernia, and lateral femoral cutaneous nerve injury [8,9,12].
In the 1990s, Cole and Hirvensalo separately reported on a modified Stoppa approach which conferred additional benefits in comparison to the ilioinguinal approach [8,13]. Yet this approach is associated with the risk of some complications [6,8,9,13].
In recent years, several modifications of these two approaches have been devised, each having its own set of strengths and limitations [4,8,9,13–18].
In this paper, we present our successful experience with a novel pubis symphysis approach (PSA) for treatment of acetabular fractures. The advantages accruing from this approach include minimal tissue damage and a relatively quick exposure of the entire pelvic brim and the quadrilateral surface. Our results indicate that PSA as a potential alternative (but not replacement) to the classical anterior approaches for exposure of the acetabulum.
Material and Methods
Between March 2011 and March 2012, fifteen patients with displaced acetabular fractures were surgically treated using PSA developed by one of the authors (Dr. ZQA). The choice of surgical approach was based of the fracture site, its pattern, and associated displacement. Injuries involving the anterior column that met indications for use of an anterior approach were treated using PSA. The study protocol was approved by the Ethics Committee of the local University.
The study population was comprised of thirteen male and two female patients with an average age of 37 years (range, 18–53 years). Seven patients had sustained fractures on the left side while the remaining eight patients had right-sided fractures. In eight patients, the injury mechanism involved a fall from height, while seven patients sustained injuries in motor vehicle accidents. According to the Judet and Letournel classification system [1,2] there were four fractures of both columns, three T shaped fractures, three transverse fractures, three anterior and posterior hemi-transverse fractures, and two anterior column fractures. Eleven patients had sustained multiple injuries. These included, chest injuries (n=2), spine injuries (n=3), pelvic fractures (n=2) and limb fractures (n=7). Additional complications included pulmonary embolism (n=1), and deep vein thrombosis (DVT) (n=1). The patients included both primary and secondary referrals to our Level I university trauma center. The time span between injury and surgical intervention averaged 10 days (range, 3–31 days) (Table 1).
Table 1.
Patient characteristics.
| No. | Gender | Age | Side | Injury | Classification | Additional injuries | Time to surgery (day) |
|---|---|---|---|---|---|---|---|
| 1 | Male | 52 | Left | MVA | Anterior + posterior hemi transverse | Pelvic fracture, upper limb fracture | 3 |
| 2 | Female | 18 | Left | MVA | T shaped | Pelvic fracture, limb fractures, pulmonary embolism | 9 |
| 3 | Male | 53 | Right | MVA | Transverse | Chest injury | 18 |
| 4 | Male | 47 | Left | Fall | Both column | Upper limb fractures, urethral injury | 15 |
| 5 | Male | 18 | Right | MVA | Anterior column | Intestinal rupture, spine injury | 20 |
| 6 | Male | 50 | Right | Fall | T shaped | Spine injury, upper limb fracture | 6 |
| 7 | Male | 32 | Right | Fall | Both columns | None | 6 |
| 8 | Male | 26 | Right | MVA | Transverse | Central dislocation, lower limb fracture, spine injury | 31 |
| 9 | Male | 42 | Left | Fall | Anterior column | None | 3 |
| 10 | Male | 18 | Right | Fall | Anterior + posterior hemi transverse | Pelvic fracture, intraperitoneal hemorrhage | 5 |
| 11 | Male | 51 | Left | MVA | T shaped | Lower limb fractures | 6 |
| 12 | Female | 25 | Right | MVA | Both columns | Deep vein thrombosis | 9 |
| 13 | Male | 44 | Left | Fall | Anterior + posterior hemitransverse | Chest injury, pelvic fracture, upper limb fracture | 10 |
| 14 | Male | 32 | Left | Fall | Transverse | None | 4 |
| 15 | Male | 45 | Right | Fall | Both column | None | 7 |
MVA – motor vehicle accident.
Operative technique
All surgical procedures were carried out under general anesthesia with adequate muscle relaxation. The patients were placed in the supine position on a radiolucent operative table with a 30-degree elevation of the injured side (Figure 1). A floppy lateral position was used for cases in which a simultaneous posterior exposure was considered a possibility. The lower abdomen, pelvic region, entire hindquarter, and lower extremity of the affected side were prepped and draped, leaving the ipsilateral lower extremity free. The genitalia were separated from the operative field with the help of drapes fixed by suturing. Sticky sheaths were used on the border of drapes and the operation field.
Figure 1.

The patient was placed supine with approximately 30° elevation of the injured side. The incision was made at the symphysis pubis level. The lateral incision was made along the iliac crest.
In patients with involvement of posterior acetabular elements a Kocher-Langenbeck (K-L) approach was first used. In these patients, the posterior wall was temporarily fixed by K-wires, while the posterior column was fixed by a 4-hole plate with one screw at both ends. A total of seven patients were treated with PSA alone, while the remaining eight patients required PSA in combination with the K-L approach.
PSA procedure
A 10 cm long transverse incision was made at the level of pubis symphysis extending from the pubic tubercle of the contralateral side to that on the injured side (Figures 1, 2). The incision was carried down through skin and subcutaneous tissue. The spermatic chord or round ligament was retracted laterally carefully. The anterior rectus abdominis sheath was incised at the anteroinferior surface of pubis symphysis (Figure 3); with a sharp dissection, the rectus was elevated subperiosteally to expose pubis symphysis and pubic tubercles on both sides and the retropubic space of Retzius. The reflected ligament was stripped sharply, while the pectineus muscle along with periosteum were stripped bluntly for enabling exposure of both superior rami (Figure 4). At this juncture, a bump was placed under the ipsilateral knee, and the hip joint was flexed and adducted to allow relaxation of the iliopsoas muscle and femoral vessels. Blunt dissection was then carried out along the pelvic brim with periosteal elevator exposing the anterior part of the quadrilateral surface and iliopectineal eminence. Adequate precautions were taken to protect the obturator neurovascular bundle during this procedure. Dissection and separation of these structures is not required in the PSA.
Figure 2.

A 10 cm long transverse incision was made at the level of pubis symphysis
Figure 3.

The anterior rectus abdominis sheath was incised at the surface of pubis symphysis, infero-medial to the inguinalis superficialis. The incision did not involve the inguinal canal.
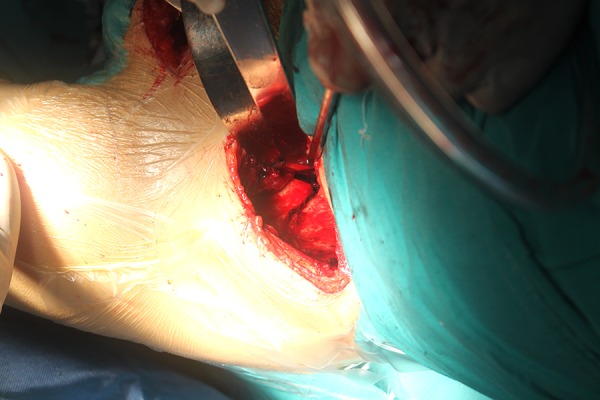
Figure 4.

Through the incision, stripping started from the pubis symphysis towards iliopectineal eminence, under the interspace between vascular anastomoses and pubic rami.
A lateral window similar to the one in the ilioinguinal approach was used for fractures with extremely high anterior acetabular column component, or those which required manipulation of the posterior column. The incision extended approximately 10 cm starting from the anterior superior iliac spine and proceeding posteriorly along the iliac crest (Figure 1). The insertion of external oblique muscle was sharply released. The origin of the iliacus muscle was dissected and elevated subperiosteally to expose the posterior parts of both the pelvic brim and quadrilateral surface and anterior part of the sacroiliac joint. With the hip joint in flexion, the pectineal ligament could be elevated bluntly along the pelvic brim and acetabular roof using a narrow periosteal elevator. A submuscular tunnel was created by working through both incisions.
Reduction of the iliac wing was attained through the lateral window. Two Steinmann pins were inserted into the anterior superior iliac spine which worked as manipulating handles. With manual traction of the ipsilateral limb performed by an assistant, the fractures were reduced and temporarily fixed by K-wires. Fractures near the pelvic brim were fixed with K-wires or a six-hole reconstruction plate.
Fractures of the quadrilateral surface and pubic ramus were reduced through PSA (Figure 5). A narrow abdominal retractor was used to protect and retract the femoral neuromuscular bundle anterolaterally. Flexion and internal rotation of the hip joint greatly assisted in relaxing the retracted structures. Shortening deformity of pubic ramus was corrected and maintained with a point reduction forceps clipped onto it. Then lateral traction of ipsilateral femoral head was applied. The two aforementioned Steinmann pins were rotated medially and distally to reduce the iliac segment, which usually controls an extended part of the acetabular roof. The combination of a point reduction forceps inserted through lateral window with a periosteal elevator inserted through PSA was used to attain reduction of the quadrilateral surface. The posterior inward-turned bony plate and anterior part of the quadrilateral surface were stabilized, and temporarily fixed by K-wires (Figure 6). Evaluation of the temporary reduction was done with fluoroscopy using AP pelvis, iliac oblique, and obturator oblique views. After obtaining anatomic reduction, the posterior column was fixed first. A pre-shaped 3.5 mm (12–14-hole) reconstruction plate was introduced through the submuscular tunnel as described earlier, and slid along the pelvic brim. At this stage, the anterior and posterior ends of the plate were situated lateral to the pubis symphysis and sacroiliac joint, respectively. The plate was fixed with at least three screws at each end (Figure 7).
Figure 5.

Reduction of quadrilateral surface and pubic ramus through the pubic symphysis approach (PSA).
Figure 6.
Reduction of the posterior inward-turned bony plate of quadrilateral surface.
Figure 7.

Reconstruction plate introduced through the submuscular tunnel and slid along the pelvic brim.
The quadrilateral fragment near the greater sciatic notch can be fixed by placing a four-hole reconstruction plate vertically. For the ones near the obturator canal, fixation can be achieved by inserting screws through the plate along the pelvic brim. Screws must be inserted with great care. They are required to be directed down and inward to control their points of exit either along or through the quadrilateral surface. Cases of sole fracture of the quadrilateral surface can be exposed and fixed through the PSA alone. A short plate can be placed in an intrapelvic fashion with the plate placed along the posterior surface of the superior ramus and onto the upper portion of the quadrilateral plate and posterior column (Figure 8).
Figure 8.

A short plate can be placed in an intrapelvic position along the posterior surface of the superior ramus and onto the upper portion of the quadrilateral plate and posterior column.
After achieving osteosynthesis, stability was verified by moving the hip joint in all directions. Occurrence of a discernible grating sensation is usually an indication of protrusion of the screw into the acetabulum. Finally, after wound irrigation, a suction drain was placed in the retropubic space of Retzius and a second drain was placed on the internal iliac fossa if the lateral window is used. A rectus abdominis sheath was stitched subperiosteally with an interrupted figure-of-eight suture.
Postoperative prophylactic antibiotics were administered for three days. Drains were removed when there was less than 15 mL of drainage in a 24-hour period. Once pain relief was obtained, patients were asked to actively flex and extend the hip joint in bed. Stitches were removed two weeks after the operation. A range of non-weight-bearing movements were advised for the first six weeks. Computed tomography (CT) scanning was done in all patients at the completion of the twelfth postoperative week. Partial weight-bearing walking was allowed after fracture healing was confirmed. Complete weight bearing was allowed after the eighteenth postoperative week. Patients were followed up every six weeks in the first six months, and then once every two months until one year. Subsequent follow-up was done once every six months.
Results
The mean duration of operation was 222±78 minutes (120–390 minutes); average blood loss was 993±361 mL (500–1,500 mL). For the patients in which PSA was used alone, the average duration of operation was 159±29 minutes (120–180 minutes) and the average blood loss was 1,057±378 mL (500–1,500 mL). The mean postoperative hospital stay was 15.8 days (7–31 days) (Table 2). No complication occurred intraoperatively and postoperatively during hospitalization. The quality of reduction was assessed by intraoperative and postoperative radiographs of AP pelvis and Judet views. All patients obtained anatomical reduction according to Matta’s Criteria [10].
Table 2.
Results.
| No. | Approach | OR-Time (min) | Blood loss (mL) | Stay (days) | Modified Merle d’Aubigné/Postel score |
|---|---|---|---|---|---|
| 1 | Combined | 220 | 1100 | 7 | 16 |
| 2 | Combined | 390 | 700 | 29 | 14 |
| 3 | Combined | 220 | 1500 | 26 | 17 |
| 4 | PSA | 180 | 1500 | 19 | 17 |
| 5 | PSA | 180 | 700 | 10 | 17 |
| 6 | PSA | 150 | 1000 | 8 | 18 |
| 7 | PSA | 120 | 1200 | 10 | 18 |
| 8 | PSA | 180 | 1500 | 31 | 18 |
| 9 | PSA | 120 | 500 | 7 | 18 |
| 10 | Combined | 330 | 1400 | 8 | 18 |
| 11 | Combined | 285 | 900 | 13 | 17 |
| 12 | Combined | 300 | 500 | 16 | 17 |
| 13 | PSA | 180 | 1000 | 17 | 16 |
| 14 | Combined | 270 | 700 | 10 | 18 |
| 15 | Combined | 210 | 700 | 26 | 15 |
Combined – PSA+K-L approach.
All patients were followed up clinically and radiographically for an average period of 39 months (31–43 months). All incisions healed well, without either deep or superficial infection. No reduction loss was detected. Fracture union was confirmed in all patients by CT scan twelve weeks after their operation. The clinical outcome was measured using the Merle d’Aubigné-Postel rating system modified by Matta [10]. The mean score at the time of last follow-up was 16.9 (range 14–18). The scores indicated excellent outcome in six patients, good in eight patients, and fair in one patient. One patient developed postoperative hypoesthesia in the innervation area of lateral femoral cutaneous nerve, which recovered spontaneously within one month. The insertion of rectus healed without failure in all patients and no hernia was detected. No chronic infection or thromboembolic phenomenon was detected. Up to the last follow-up, no avascular necrosis of femoral head, heterotopic ossification, or osteoarthrosis was observed (Figure 9) [19,20].
Figure 9.
Preoperative iliac oblique view (A) and obturator oblique view (B) radiographs show an anterior column fracture in an 18-year-old male following a motor vehicle accident; anatomical reduction was achieved through PSA (C); Follow-up radiographs at 18 months after surgery (D); Function (E) and wound (F) recovery.
Discussion
Among the various approaches for surgical management of acetabular fractures, no single surgical approach will provide adequate exposure for treating all fractures [3]. The optimal approach in a particular case depends upon the individual characteristics of the case. Therefore, precise preoperative mapping of the fracture is considered essential for achieving successful outcomes [2].
Most acetabular fractures can be treated with either an anterior or posterior approach or both [4,6,21]. Over the years, the classical anterior approaches like the ilioinguinal approach and the modified Stoppa approach have evolved into widely used approaches, not only to the anterior column but also to almost the entire inner aspect of the innominate bone [6,10,12,21,22]. Some modifications or new approaches were designed to expand the utility of the classical approaches [18].
Postoperative orthopedic wound infection is, to an extent, attributable to surgical trauma and disruption of vascular supply [3,21]. The PSA has a distinct advantage of being relatively less invasive and not requiring detachment of the entire anterior abdominal wall. This confers considerable advantage in minimizing instances of infection. The blood loss in PSA is comparable to that of other approaches [16]. It is acknowledged that the blood loss is more dependent on patient factors such as the severity of the acetabular fracture, associated injuries, coagulability, and bone bleeding [6,8,16,23], and it does not affect the outcome score [6]. In a hip fracture, the blood loss could exceed one liter. In such cases, a less invasive incision is preferred [23]. Moreover, prolonged traumatic surgical dissection is known to increase the incidence of heterotopic ossification [8]. This can be avoided by using a single midline intrapelvic approach. Indomethacin has been widely used as a prophylactic therapy against heterotopic ossification. However, it was not administered in our series and there was no heterotopic ossification (according to the Brooker system) in our patients at the last follow-up [19]. Using indomethacin is associated with an increased risk of gastrointestinal bleeding. Patients with acetabular fractures usually have multiple existing injuries thereby increasing the potential hazards of using indomethacin [8]. The PSA is therefore a valuable alternative for such patients. Moreover, with less soft tissue damage, patients have less pain, which allows functional rehabilitation to begin more rapidly [24].
It is acknowledged that anatomic reduction is essential to assure a good long-term outcome of acetabular fractures [21]. Matta has shown that long-term outcomes tend to strongly correlate with initial reduction as judged by plain radiography [11]. The PSA can expose the entire pelvic brim from the pubis symphysis to the anterior aspect of sacroiliac joint. Compared to the classical ilioinguinal approach, this offers the surgeon better visibility of all anterior elements and the quadrilateral plate, and enables fixation and medial buttressing of the quadrilateral plate with a reconstruction plate directly and medially to the hip joint. In this study, anatomical reduction was achieved in all fifteen patients and there was no secondary displacement. The outcomes were excellent in six patients, good in eight patients, and fair in one patient. This approach also allows direct visualization and access to the vascular anastomoses as the surgeon is positioned on the opposite side. In our experience, a ligation or mobilization of the vessel is generally not necessary. With careful manipulation, the reconstruction plate can be inserted through the sufficient interspace between it and pubic rami (Figure 4). This particular assertion is in agreement with the findings reported by Khoury [6].
Dissection and manipulation of the femoral vessel structures is implicated in the pathogenesis of DVT and lymphatic congestion. These can also put the vascular at a risk of iatrogenic laceration [8–10,12]. The PSA keeps these structures in their fasciae and are therefore manipulated as a group. Theoretically, this should minimize the risk of injury and thrombosis. In our study, no such intraoperative or postoperative complications were encountered in any of our patients. Another the advantage of the single midline approach is that it provides access to the entire pelvic ring so that fractures of both sides can be approached through a single incision. Moreover, the procedure can be extended into a complete ilioinguinal approach if needed.
However, this approach does not enable the manipulation and anatomical reduction of the iliac wing, which is an essential step for anatomical restoration of the anterior wall [3,6]. In such cases, a lateral window is needed. This can be encountered in as many as 60–93% of the cases [4,6,8,9,13,14,16]. Yet another advantage of PSA is that the lateral incision does not extend beyond the anterior superior iliac spine, and consequently reduces the risk of injuries to the lateral femoral cutaneous nerve. In our study, one patient developed hypoesthesia in the innervation area of the lateral femoral cutaneous nerve. We suspect that it was a result of iatrogenic stretch with the retractor.
The PSA also has several advantages over the Stoppa approach. First, it is a relatively easy anatomical dissection involving fewer anatomical layers than Stoppa (Figure 10). The duration of surgical exposure is another factor related to infection [3,25]. We think this easy and time-saving approach can play a role in preventing infection by shortening this procedure time.
Figure 10.

Sagittal plane shows that PSA involves fewer anatomical layers and does not involve rectus or peritoneum.
Second, although in the Stoppa approach we do not open the inguinal canal completely, it does interrupt the integrity of the inguinalis superficialis, and splits of the rectus abdominis. In addition, hernia is still a complication associated with this approach [6,8,13,22]. Sagi et al. also reported a case of postoperative atrophy of rectus abdominis associated with the Stoppa approach [13]. The PSA does not involve dissection around the inguinal canal or the belly of rectus abdominis muscle (Figures 3, 10). Therefore, this approach does not increase the risk of postoperative hernia. In this series, none of the patients developed postoperative hernia.
Third, the Stoppa approach carries the risk of peritoneal perforation [8,9], while in the PSA the incision is located at the level of pubic symphysis (Figure 10), and does not involve dissection of the rectus abdominis muscle. Manipulations are limited in the pelvic cavity away from the peritoneum. Moreover, the abdominal organs are retracted away and protected by abdominal retractors.
Finally, the lower location of the PSA allows its use in patients in whom the Stoppa approach is contraindicated, for example, preexisting suprapubic catheter (Figure 1) or previous lower abdomen surgical procedures (Figure 9). Furthermore, the skin incision in PSA is inferior to the ‘bikini line’, the approach is cosmetic to patients, especially young female patients.
Matta suggested bringing the medial portion of the ilioinguinal approach slightly proximal so as to reduce chances of infection of the retropubic space of Retzius. The obturator nerve injury was also reported as a complication of the Stoppa approach. However, since the beginning of this study until present, PSA has been used in 290 patients and neither of these complications has been detected.
Our study has its own limitations, although the outcomes in our preliminary study are comparable to outcomes reported from earlier studies. Our findings need further confirmation from additional studies involving a larger series of patients to ascertain the favorable outcomes (like lower complications) demonstrated in our study compared to the classical approach.
Conclusions
PSA is a convenient, technically easy approach that provides good visualization for reduction and fixation of acetabular fractures with a low incidence of complications. The PSA provides a definite value addition to supplement other commonly used approaches. Fractures that met indications for use of an anterior intrapelvic approach, like the ilioinguinal and modified Stoppa approach, can be controlled and reduced by PSA, especially when the skin condition of the surgical field does not allowed the classical anterior approach. PSA is not intended to replace classical approaches in all cases, but rather to provide a helpful easy alternative to the more demanding original exposure.
Footnotes
Source of support: Departmental sources
Conflict of interest
There is no conflict of interest in relation to this article.
References
- 1.Judet R, Judet J, Letournel E. Fractures of the acetabulum: Classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–46. [PubMed] [Google Scholar]
- 2.Letournel E. Acetabulum fractures: Classification and management. Clin Orthop Relat Res. 1980;(151):81–106. [PubMed] [Google Scholar]
- 3.Goulet JA, Bray TJ. Complex acetabular fractures. Clin Orthop Relat Res. 1989;(240):9–20. [PubMed] [Google Scholar]
- 4.Andersen RC, O’Toole RV, Nascone JW, et al. Modified stoppa approach for acetabular fractures with anterior and posterior column displacement: Quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010;24:271–78. doi: 10.1097/BOT.0b013e3181b2b4ca. [DOI] [PubMed] [Google Scholar]
- 5.Durkee NJ, Jacobson J, Jamadar D, et al. Classification of common acetabular fractures: radiographic and CT appearances. Am J Roentgenol. 2006;187:915–25. doi: 10.2214/AJR.05.1269. [DOI] [PubMed] [Google Scholar]
- 6.Khoury A, Weill Y, Mosheiff R. The Stoppa approach for acetabular fracture. Oper Orthop Traumatol. 2012;24:439–48. doi: 10.1007/s00064-011-0093-z. [DOI] [PubMed] [Google Scholar]
- 7.Halvorson JJ, Lamothe J, Martin CR, et al. Combined acetabulum and pelvic ring injuries. J Am Acad Orthop Surg. 2014;22:304–14. doi: 10.5435/JAAOS-22-05-304. [DOI] [PubMed] [Google Scholar]
- 8.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;(305):112–23. [PubMed] [Google Scholar]
- 9.Ponsen KJ, Joosse P, Schigt A, et al. Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: Technical aspects and operative results. J Trauma. 2006;61:662–67. doi: 10.1097/01.ta.0000219693.95873.24. [DOI] [PubMed] [Google Scholar]
- 10.Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach. A 10-year perspective. Clin Orthop Relat Res. 1994;(305):10–19. [PubMed] [Google Scholar]
- 11.Matta JM. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–45. [PubMed] [Google Scholar]
- 12.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;(292):62–76. [PubMed] [Google Scholar]
- 13.Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–70. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 14.Jakob M, Droeser R, Zobrist R, et al. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006;60:1364–70. doi: 10.1097/01.ta.0000208139.97474.f7. [DOI] [PubMed] [Google Scholar]
- 15.Kloen P, Siebenrock KA, Ganz R. Modification of the ilioinguinal approach. J Orthop Trauma. 2002;16:586–93. doi: 10.1097/00005131-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Ruchholtz S, Buecking B, Delschen A, et al. The two-incision, minimally invasive approach in the treatment of acetabular fractures. J Orthop Trauma. 2013;27:248–55. doi: 10.1097/BOT.0b013e3182690ccd. [DOI] [PubMed] [Google Scholar]
- 17.Seyyed Hosseinzadeh HR, Eajazi A, Hassas Yeganeh M, et al. Modified ilioinguinal approach to the acetabulum and pelvis from beneath the inguinal ligament: A subinguinal approach. Hip Int. 2010;20:150–55. doi: 10.1177/112070001002000204. [DOI] [PubMed] [Google Scholar]
- 18.Wolf H, Wieland T, Pajenda G, et al. Minimally invasive ilioinguinal approach to the acetabulum. Injury. 2007;38:1170–76. doi: 10.1016/j.injury.2006.06.116. [DOI] [PubMed] [Google Scholar]
- 19.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–32. [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helfet DL, Schmeling GJ. Management of complex acetabular fractures through single nonextensile exposures. Clin Orthop Relat Res. 1994;(305):58–68. [PubMed] [Google Scholar]
- 22.Isaacson MJ, Taylor BC, French BG, Poka A. Treatment of acetabulum fractures through the modified Stoppa approach: Strategies and outcomes. Clin Orthop Relat Res. 2014;472:3345–52. doi: 10.1007/s11999-014-3460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imbelloni LE, Lima U, Pedrosa FK. Successful anesthesia and hip surgery in a 107-year-old patient. Am J Case Rep. 2014;15:308–11. doi: 10.12659/AJCR.889961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zobrist R, Messmer P, Levin LS, Regazzoni P. Endoscopic-assisted, minimally invasive anterior pelvic ring stabilization: A new technique and case report. J Orthop Trauma. 2002;16:515–19. doi: 10.1097/00005131-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Li Q, Liu P, Wang G, et al. Risk factors of surgical site infection after acetabular fracture surgery. Surg Infect (Larchmt) 2015;16:577–82. doi: 10.1089/sur.2014.134. [DOI] [PubMed] [Google Scholar]



