Abstract
Background:
The optimal treatment for acute Achilles tendon ruptures is still an ongoing debate. Acute ultrasonography (US) investigation to measure the diastasis between the tendon ends has previously been used to classify acute Achilles tendon ruptures; however, no study has used US to predict reruptures and functional outcomes.
Purpose:
To investigate whether acute US can be used to predict the risk of reruptures and outcomes after treatment of an acute Achilles tendon rupture.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
Forty-five patients (37 men, 8 women) with a mean age of 39 ± 9.2 years (range, 23-59 years) from a cohort of 97 patients participating in a randomized controlled study comparing surgical and nonsurgical treatment were included. US was performed within 72 hours from the index injury. Diastasis between the tendon ends was documented. Reruptures were documented, and the patients’ functional outcomes were measured 12 months after injury.
Results:
Patients with a diastasis of >10 mm treated nonsurgically had a higher degree of rerupture. In the nonsurgically treated group, 3 of 4 patients with a diastasis of >10 mm suffered from rerupture (P < .001). Moreover, in the nonsurgical group, there was significantly worse outcomes in patients with a diastasis of >5 mm in terms of patient-reported outcomes using the Achilles tendon Total Rupture Score (ATRS) (P = .004) and heel-rise height at 12 months (P = .048) compared with the group with a lesser degree of tendon separation.
Conclusion:
US may be a useful tool to predict the risk of rerupture and greater degree of functional deficit. It may be an important measure in a clinical treatment algorithm for deciding whether a patient will benefit from surgical intervention after an acute Achilles tendon rupture.
Keywords: ultrasonography, Achilles tendon rupture, rerupture, diastasis
There is a seemingly never-ending debate on which treatment should be recommended for patients with an acute Achilles tendon rupture.7 Results from several randomized controlled trials (RCTs) and meta-analyses have shown a higher rerupture rate in patients treated nonsurgically compared with a greater risk of wound infection after surgery.2,7 The results after nonsurgical treatment have markedly improved since the introduction of a functional brace and early weightbearing.12 Focus has recently shifted toward providing individualized recommendations.15 However, further research is needed to determine which factors can predict success with either treatment.4,15
The greater incidence of rerupture in nonsurgical patients may be due to nonhealing, which in turn could be a result of a large initial gap between the tendon ends. Thermann and Zwipp18 proposed that an initial diastasis of more than 5 mm would adversely affect the functional outcome. Ultrasonography (US) in 25° of plantar flexion was suggested to be able to identify those patients who were suitable for nonsurgical treatment.
US has been used as an image modality for the diagnosis and evaluation of injuries for over 20 years.5 However, acute Achilles tendon rupture is mainly a clinical diagnosis, where the history of an audible snap and sudden pain combined with a palpable gap and a positive Thompson test is sufficient to establish the diagnosis.10 In patients with a typical history of trauma, a complete rupture can be assumed since partial ruptures are uncommon.10 US is not recommended as a means to establish diagnosis since there is risk that the patient is not treated correctly if the physician relies too heavily on US alone.11
On the other hand, Kotnis et al8 used dynamic US as a selective criterion for determining whether patients should receive surgical or nonsurgical treatment. According to these researchers, a gap less than 5 mm was proposed as a limit for to whom nonsurgical treatment could be recommended. However, to the best of our knowledge, no prospective comparative research has been performed using acute US to predict reruptures and correlate with subjective and functional outcome. There is no study that has evaluated whether there is a difference in complications, symptoms, and function in patients with different sized diastases.
The aim of this study was to assess whether acute US could be used to predict rerupture and outcomes. The hypothesis was that in patients with an initial large diastasis between the tendon ends treated nonsurgically, there would be a greater risk of rerupture as well as inferior functional and patient-reported outcomes 12 months after treatment.
Methods
Participants
The first 45 patients from a cohort of 97 patients from an RCT comparing surgical and nonsurgical treatment were included in this study.12 We were not able to perform US on the remaining 52 patients due to new organization within the hospital, which occurred during the RCT. Demographics are reported in Table 1. The diagnosis was established by medical history and clinical examination (palpable gap, positive Thompson test). Inclusion criteria were any patient with a complete closed unilateral midsubstance acute Achilles tendon rupture with treatment initiated within 72 hours from injury. The randomization was performed by computer-generated sealed envelopes, and the process was administered by a study coordinator with surgeon involvement. Exclusion criteria were diabetes mellitus, previous Achilles tendon rupture, other lower leg injuries, immunosuppressive therapy, and neurovascular disease. None of the included patients had a medical history of either fluoroquinolone use or corticosteroid injection in the area.
TABLE 1.
Patient Demographics (N = 45)a
| Age, y, mean (range) | 37 (23-59) |
| Sex, male/female, % (n) | 82 (37) / 18 (8) |
| Weight, kg, mean (range) (n) | 83 (62-109) (42) |
| Male | 87 (68-109) (35) |
| Female | 67 (62-70) (7) |
| Height, cm, mean (range) (n) | 179 (161-193) (42) |
| Male | 181 (166-193) (35) |
| Female | 167 (161-173) (7) |
| Surgery, yes/no, % (n) | 47 (21) / 53 (24) |
The 45 participants in this study underwent US (within 72 hours) prior to initiating treatment, where the diastasis was measured and classified. US was not used for decision making (randomization) in terms of treatment selection.
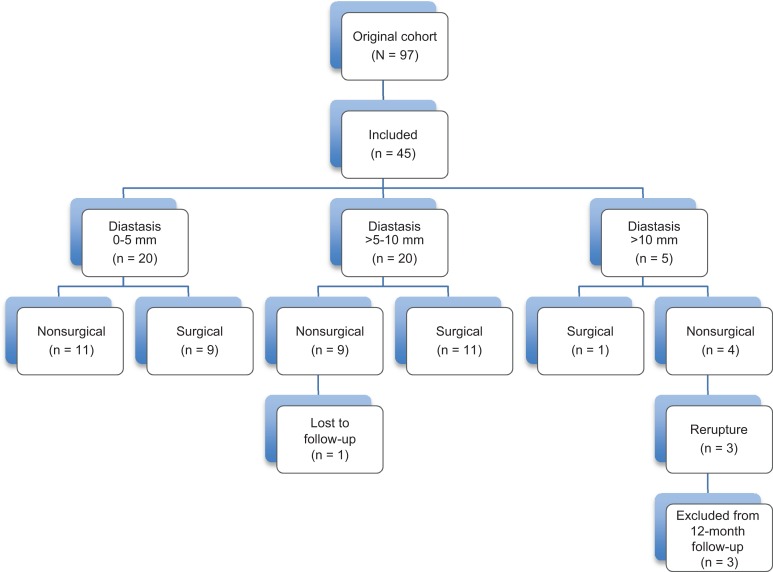
All patients received identical rehabilitation supervised by experienced physical therapists. Patient-reported outcomes together with functional outcome measures were evaluated at 12 months. A flow diagram of the study process is shown in Figure 1. All identified reruptures underwent surgical treatment and were excluded from subsequent follow-up.
Figure 1.
Flow diagram of the study.
Treatment Procedure
The surgical technique was performed under local, spinal, or general anesthesia with the patient in the prone position. An open Achilles tendon repair was done with a 5- to 8-cm medial skin and paratenon incision. The tendon ends were sutured with an end-to-end modified Kessler suture technique. Postoperatively, a below-the-knee cast with the foot in a 30° equinus position was used for 10 to 14 days. Nonsurgical treatment was initiated immediately after diagnosis with a below-the-knee cast with the foot in a 30° equinus position for 10 to 14 days.
After 10 to 14 days, an adjustable brace (DonJoy ROM Walker; DJO Nordic) was used for both groups for a further 6 weeks. The brace was limited to −30° of dorsiflexion with unlimited plantar flexion for the first 2 weeks, −10° for the next 2 weeks, and +10° for the last 2 weeks.
Weightbearing was allowed as much as tolerated after 6 weeks. A physical therapist did all brace adjustments. Excluding surgery, identical treatment and rehabilitation protocols were used.12
All patients followed a standardized rehabilitation protocol and visited a physical therapist 2 to 3 times per week.12 The rehabilitation period lasted 6 months or longer. The rehabilitation protocol is presented in detail in the original RCT.12
Ultrasonography Assessment
All patients were evaluated using US within 72 hours of injury. US was performed by 1 of 2 experienced radiologists using a Siemens Sonoline Antares system (Siemens Healthcare Global) provided with a variable frequency (VF) of 13.5 mHz multifrequency linear array transducer, using an 11.4-mHz default setting and scanning parameters aimed for superficial musculoskeletal scanning. Scanning of the Achilles tendon was performed in both longitudinal and axial planes assisted by dynamic scanning during passive ankle motion to facilitate identification of the tears. Moreover, extended-field-of-view scanning (SieClear, compound scanning) was done to illustrate the tendon gap (Figure 2), while all measurements were performed using real-time scanning. No stand-off pads were used, and scanning was performed with the ankle in both neutral and approximately 30° of passive plantar flexion. Frank anechoic tendon defects or tendon discontinuities of the fibrillary echo texture were direct criterion of tendon tears. The gap between the 2 tendon ends was measured in approximately 30° of plantar flexion at the center of the tendon gap and graded as 0 to 5 mm, >5 to 10 mm, and >10 mm. These groups were used to evaluate whether there was a difference in rerupture occurrence between groups. Measurements were performed by identifying the tendon ends on the central part of the tendon on a sagittal scan. Imaging was performed using optimal settings including the highest resolution possible, with measurements performed on zoomed images, and the mean of 3 separate measurements was used as the result value of the gap. Only the tendon fibers were scanned, and no attention was given to the paratenon. All patients scanned had sustained complete Achilles tendon ruptures; no partial tears were included in the investigation.
Figure 2.
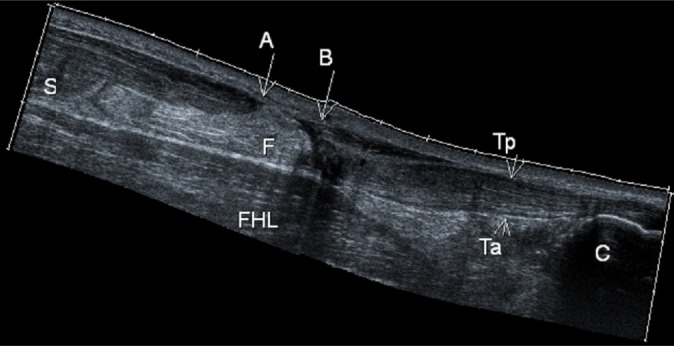
Ultrasonography: longitudinal compounds scan of a tendon tear with the ankle in neutral position. A-B, gap of tendon rupture; C, calcaneus; F, fat tissue; FHL, flexor hallucis longus muscle; S, soleus muscle; Ta, anterior tendon surface; Tp, posterior tendon surface.
Functional Testing
The MuscleLab system (Ergotest Technology) was used for the functional evaluation. The MuscleLab system has been used in several studies to evaluate outcome after Achilles tendon rupture.12,14,16 The functional testing consisted of 2 jump tests and 1 endurance test performed as described by Silbernagel et al.17 In the present study, the heel-rise test, countermovement jump (CMJ), and hopping were evaluated 12 months after the index injury. The results of the functional tests are presented as limb symmetry index (LSI) values, with the numbers given as a percentage compared with the contralateral uninjured side.
For the heel-rise endurance test, the patients were asked to perform as many single-leg standing heel-rises as possible and as high as possible while standing on a box with an incline of 10°. A metronome was used to assist the patient with keeping the pace of performing 30 reps/min. The number of heel rises as well as the height of each heel rise and the total amount of work (body weight × total distance in joules) were used for analysis. The maximal heel-rise height was also documented. The CMJ test involves the participants making a vertical jump after having bent their knee to a desired flexion. Three jumps on each side were performed, and the mean was used for analysis. The maximum jumping height (in cm) was used. Hopping is a rhythmical jump similar to skipping rope. This was performed 1 leg at a time; 25 jumps were recorded. The hopping height (in cm) as well as the hopping quotient (flight time/contact time) were used for data analysis.
Patient-Reported Outcomes
The Achilles tendon Total Rupture Score (ATRS), a reliable and validated patient-reported outcome, was used to evaluate patient symptoms at the 12-month follow-up.13 This questionnaire consists of 10 questions concerning symptoms and functional ability after an Achilles tendon rupture. The maximum score is 100, indicating no symptoms and full recovery. The minimal detectable change has been shown to be 6.8 points.3
Statistical Analysis
All data were analyzed using SPSS Statistics for Windows version 22.0 (IBM Corp). Descriptive data are reported as mean, standard deviation, and range. The level of significance was set at P < .05. The LSI was calculated to compare the 2 treatment groups. The LSI was defined as the ratio between the involved limb score and the uninvolved limb score, expressed as a percentage: LSI = (Involved limb/Uninvolved limb) × 100.
The 3 groups (0-5 mm, >5-10 mm, and >10 mm) were used to compare the occurrence of reruptures. When comparing reruptures, a Pearson chi-square analysis between the 3 groups was performed. Positive predictive value was calculated as patients in the group with a rerupture divided by all the patients in the group.
At the 12-month follow-up, the >10-mm group only consisted of 2 patients since 3 of the 5 had suffered from a rerupture and were not included in the 12-month follow-up. Therefore, it was decided to merge the remaining 2 patients from the >10-mm group into 2 groups (≤5 mm, >5 mm) for the 12-month follow up. The Mann-Whitney U test was performed to compare the 2 groups at the 12-month follow-up. Moreover, 1 patient was unable to attend the 12-month follow-up due to systemic illness and was therefore excluded.
All patients gave their written consent to participate. Ethical approval was granted from the regional ethical review board in Sweden.
Results
The US results measuring the diastases between the tendon ends are reported in Table 2. The diastasis measurement showed that the ≤5-mm group consisted of 20 (44%) patients and the >5-mm group had 25 (56%) patients.
TABLE 2.
Patients in Each Study Group
| No. of Patients | |||
|---|---|---|---|
| Treatment | ≤5 mm Diastasis | >5-10 mm Diastasis | >10 mm Diastasis |
| Nonsurgical | 11 | 9 | 4 |
| Surgical | 9 | 11 | 1 |
| Total | 20 | 20 | 5 |
Reruptures
There were 3 total reruptures in the study population (6.7%), all of which were initially treated nonsurgically and had a gap >10 mm. Three of the 4 patients with a gap >10 mm sustained a rerupture. This gives a positive predictive value of 75% of sustaining a rerupture when having a tendon gap greater than 10 mm treated nonsurgically. Using the chi-square test, there was a significant difference (P < .001) found between the 3 groups.
Patient-Reported Outcomes
There were no significant differences (P = .17) in ATRS in the entire group between the ≤5 mm and >5 mm diastases at the 12-month follow-up, as seen in Table 3. When analyzing the treatment groups separately, a significant difference (P = .004) in ATRS was found between ≤5 mm and >5 mm groups for the nonsurgical treatment; the >5 mm group had a greater degree of symptoms (Table 4). There were no significant differences between groups for surgically treated patients.
TABLE 3.
Patients Stratified by Diastasis Group at 1-Year Follow-upa
| Parameter | ≤5 mm Diastasis | >5 mm Diastasis | P Valueb |
|---|---|---|---|
| ATRS, No. of patients | 20 | 21 | .17 |
| Mean ± SD | 92.2 ± 12.0 | 84.7 ± 20.8 | |
| Heel-rise height, No. of patients | 20 | 20 | .62 |
| Mean ± SD | 81.2 ± 12.2 | 79.4 ± 10.8 | |
| Heel-rise work, No. of patients | 20 | 19 | .61 |
| Mean ± SD | 73.7 ± 19.2 | 70.1 ± 17.9 | |
| CMJ, No. of patients | 20 | 21 | .91 |
| Mean ± SD | 90.4 ± 11.9 | 89.9 ± 15.6 | |
| Hopping, No. of patients | 20 | 21 | .94 |
| Mean ± SD | 100 ± 19.6 | 99 ± 39.8 |
aLimb symmetry index values are used for functional tests. ATRS, Achilles tendon Total Rupture Score; CMJ, countermovement jump.
bAn independent-samples Mann-Whitney U test was used for the comparison between diastasis groups.
TABLE 4.
Results of the 12-Month Postinjury Evaluations by Treatment Groupa
| Surgically Treated | Nonsurgically Treated | |||||
|---|---|---|---|---|---|---|
| Parameter | ≤5 mm Diastasis | >5 mm Diastasis | P Valueb | ≤5 mm Diastasis | >5 mm Diastasis | P Valueb |
| ATRS, No. of patients | 9 | 12 | .585 | 11 | 9 | .004 |
| Mean ± SD | 89.4 ± 16.7 | 92.4 ± 7.1 | 94.4 ± 6.1 | 74.3 ± 28.2 | ||
| Heel-rise height, No. of patients | 9 | 11 | .49 | 11 | 9 | .048 |
| Mean ± SD | 79.9 ± 15.6 | 84.0 ± 10.5 | 82. ± 9.4 | 73.7 ± 8.5 | ||
| Heel-rise work, No. of patients | 9 | 11 | .636 | 11 | 8 | .08 |
| Mean ± SD | 75.6 ± 23.3 | 79.6 ± 13.6 | 72.1 ± 16.1 | 58.2 ± 16.1 | ||
| CMJ, No. of patients | 9 | 12 | .486 | 11 | 9 | .258 |
| Mean ± SD | 89.8 ± 16.0 | 94.4 ± 13.4 | 90.1 ± 7.7 | 84.0 ± 17.8 | ||
| Hopping, No. of patients | 9 | 12 | .711 | 11 | 9 | .749 |
| Mean ± SD | 100.5 ± 20.7 | 103.8 ± 18.6 | 100.7 ± 19.6 | 94.6 ± 58.6 | ||
aAll patients stratified by diastasis group at 1-year follow-up. Limb symmetry index values are used for functional tests. Boldfaced P values indicate statistically significant difference between diastasis groups (P < .05). ATRS, Achilles tendon Total Rupture Score; CMJ, countermovement jump.
bAn independent-samples Mann-Whitney U test was used for the comparison between diastasis groups.
Functional Outcome
No significant differences were observed for the entire group in terms of heel-rise test, hopping, and CMJ, regardless the size of the gap, at the 12-month follow-up (Table 3). However, when the surgically and nonsurgically treated groups were compared separately, a significant difference was found between the ≤5-mm and the >5-mm groups for the nonsurgical group regarding heel-rise height (P = .048). No differences were found for any other tests irrespective of treatment or ≤5-mm and >5-mm index gap (Table 4).
Comparing nonsurgical and surgical patients with an index gap of >5 mm, there was a significant difference for heel-rise height and heel-rise work between the groups in favor of surgical treatment (Table 5). However, no significant difference was observed for ATRS or jump tests.
TABLE 5.
Results of the 12-Month Postinjury Evaluations for Patients With a Diastasis >5 mm by Treatment Groupa
| Parameter | Surgically Treated | Nonsurgically Treated | P Valueb |
|---|---|---|---|
| ATRS, No. of patients | 12 | 9 | .069 |
| Mean ± SD | 92.4 ± 7.1 | 74.3 ± 28.2 | |
| Heel-rise height, No. of patients | 11 | 9 | .037 |
| Mean ± SD | 84.0 ± 10.5 | 73.7 ± 8.5 | |
| Heel-rise work, No. of patients | 11 | 8 | .01 |
| Mean ± SD | 79.6 ± 13.6 | 58.2 ± 16.1 | |
| CMJ, No. of patients | 12 | 9 | .394 |
| Mean ± SD | 94.4 ± 13.4 | 84.0 ± 17.8 | |
| Hopping, No. of patients | 12 | 9 | .227 |
| Mean ± SD | 103.8 ± 18.6 | 94.6 ± 58.6 |
aAll subjects stratified by diastasis group at 12-month follow-up. Limb symmetry index values are used for functional tests. Boldfaced P values indicate statistically significant difference between treatment groups (P < .05). ATRS, Achilles tendon Total Rupture Score; CMJ, countermovement jump.
bAn independent-samples Mann-Whitney U test was used for the comparison between diastasis groups.
Discussion
One of the most important findings in this study was that all the identified reruptures were in the >5-mm group (>10-mm subgroup) and treated nonsurgically. The total number of patients in the subgroup was 4, 3 of which sustained a rerupture. This gives a positive predictive value of 75% to sustain a rerupture when having an initial gap >10 mm and being treated nonsurgically. Moreover, in the nonsurgically treated group, patients with an initial gap >5 mm had a significantly greater (P = .004) degree of symptoms (ATRS) and significantly lower (P = .048) heel-rise height.
This study supports the use of acute US to measure tendon diastasis as part of a clinical treatment algorithm to determine whether a patient with an acute Achilles tendon rupture will benefit from surgical treatment. It has been shown that surgical treatment is related to an increased risk of infection and sural nerve damage whereas nonsurgical treatment may lead to an increased risk of rerupture.7 A rerupture is one of the most serious complications; it is therefore of great interest to identify risk factors to avoid rerupture. The aim of the current research was to find measures that can help with the decision of whether surgical treatment is of benefit for an individual patient to minimize the risk of rerupture despite the increased risk of other complications. In the present study, there was a correlation between a large initial diastasis and the risk of rerupture in nonsurgically treated patients. However, our sample was too small to determine whether surgical treatment of those with a gap >10 mm will prevent rerupture. Our findings further suggest that a diastasis of more than 5 mm between the tendon ends indicates a need for surgical treatment to improve clinical outcomes. This conclusion is similar to the findings of Kotnis et al.8
Previous work by Thermann et al19 and Kotnis et al8 has suggested that a more than 5-mm diastasis may be considered to confirm nonapposition of the tendon ends and hence be a recommended cutoff point to offer surgical management. If the tendon ends are not in proper contact during the first 2 weeks, this might lead to difficulties in terms of tendon healing, with either an increased risk of rerupture or poor outcome related to tendon lengthening. Voleti et al20 have shown that if there is insufficient tendon contact in the early phase, a healing problem can be expected. However, tendon healing is similar to bone healing, with new tendinous tissue forming a callus to bridge the gap between the tendon ends. To be able to restore the continuum, the ends need proximity as strength and other mechanical properties continuously improve during the healing phase.9 Even though nonsurgical treatment works well in most patients, in those with too large of a diastasis, there might be insufficient approximation of the tendon ends even if the injured leg is placed in the equinus position. In the present study, we found that the patients with a >10-mm diastasis had a greater degree of rerupture, indicating that the 5-mm diastasis might not be the definite cutoff point for predicting rerupture. On the other hand, those with a >5-mm diastasis and treated nonsurgically had a greater degree of symptoms and worse function. Hence, the results support using the size of the diastasis as a measurement for determining the need for surgical treatment, but further research is needed to confirm whether 5 mm is the optimal cutoff point.
US has previously been used early after injury.1 However, in this study, the purpose was to describe the frequency of various types of ruptures based on the location and contact types (contact and structure of interposition between the tendon ends). However, US is not recommended to be used as a diagnostic tool due to occurrence of false negatives, and patient history and clinical examination are sufficient for diagnosis.10 In this study the diagnosis of acute Achilles tendon rupture was made by the orthopaedic surgeon during the clinical examination prior to performing the US examination.
Magnetic resonance imaging (MRI) has also been shown to be a useful tool in assessing the diastasis between tendon ends.6 However, greater costs and not so easy accessibility restrict its use. With future development within the field of radiology and with more readily available MRI scans, it seems that MRI may have an increasing role in the future of assessing rupture patterns.
ATRS is a commonly used patient-reported outcome when evaluating outcomes after an acute Achilles tendon rupture. In our study, the nonsurgical group with a diastasis of >5 mm scored 20 points lower than patients with a diastasis of ≤5 mm (P = .004). However, this difference was not observed in the surgical group. The nonsurgical group with a diastasis of ≤5 mm also had similar results to surgically treated patients. Previous RCTs comparing surgical and nonsurgical treatment have not been able to demonstrate significant differences in ATRS after 12 months.12,16
This study also showed that patients with a larger diastasis treated nonsurgically had a significantly lower heel-rise height compared with those with a diastasis of ≤5 mm (P = .048). Heel-rise work showed a trend in favor of surgically treated patients (P = .08). The differences between nonsurgically and surgically treated patients were smaller and nonsignificant in terms of jump tests (CMJ, P = .258; hopping, P = .749). Furthermore, when comparing surgical and nonsurgical management for patients with a diastasis >5 mm, there was a significant difference in heel-rise height (P = .037) and heel-rise work (P = .01). This could indicate that nonoperative treatment of a large diastasis creates a worse outcome with regard to heel-rise function.
To our knowledge, there is no previous study that has been able to correlate findings between US and functional and patient-reported outcomes in a prospective study. The treatment protocols for both groups were identical except for the surgical or nonsurgical treatment. Since these patients were all part of an RCT with very strict inclusion and rehabilitation criteria and where both groups followed identical rehabilitation protocols, we consider this to be a strength of the present study.
A limitation of the present study is the limited number of patients. US imaging was planned for the entire RCT study, but due to hospital reorganization, we were only able to perform the US assessment on the first 45 patients, which makes it difficult to draw strong conclusions regarding rerupture. Another limitation of the study is that 2 experienced radiologists performed the US examinations; however, there is a possibility for varied assessment between the investigators; interrater reliability is missing in the present study.
Finally, there is a need for further larger studies to clarify the benefit of using US as a tool to select treatment for patients suffering from an acute Achilles tendon rupture.
Conclusion
Acute US measurement of the diastasis between the ruptured tendon ends may give the treating physician an indication of the risk of having a rerupture and poor outcome, hence providing guidance in the decision between surgical and nonsurgical management. Nonsurgical management of Achilles ruptures with a gap >10 mm had a significantly higher rate of rerupture than nonoperative treatment with a gap <10 mm. Nonsurgical management of ruptures with a gap >5 mm led to inferior outcomes for heel-rise height and heel-rise work compared with surgical treatment.
Acknowledgment
The authors thank Stefan Sewall for his help in performing the ultrasound investigations.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Amlang MH, Zwipp H, Friedrich A, Peaden A, Bunk A, Rammelt S. Ultrasonographic classification of Achilles tendon ruptures as a rationale for individual treatment selection. ISRN Orthop. 2011;2011:869703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bhandari M, Guyatt GH, Siddiqui F, et al. Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res. 2002;400:190–200. [DOI] [PubMed] [Google Scholar]
- 3. Carmont MR, Silbernagel KG, Mathy A, Mulji Y, Karlsson J, Maffulli N. Reliability of Achilles tendon resting angle and calf circumference measurement techniques. Foot Ankle Surg. 2013;19:245–249. [DOI] [PubMed] [Google Scholar]
- 4. Ganestam A, Kallemose T, Troelsen A, Barfod KW. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients [published online February 20, 2015]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3544-5. [DOI] [PubMed] [Google Scholar]
- 5. Gibbon WW, Cooper JR, Radcliffe GS. Sonographic incidence of tendon microtears in athletes with chronic Achilles tendinosis. Br J Sports Med. 1999;33:129–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Keene JS, Lash EG, Fisher DR, De Smet AA. Magnetic resonance imaging of Achilles tendon ruptures. Am J Sports Med. 1989;17:333–337. [DOI] [PubMed] [Google Scholar]
- 7. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute Achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87:2202–2210. [DOI] [PubMed] [Google Scholar]
- 8. Kotnis R, David S, Handley R, Willett K, Ostlere S. Dynamic ultrasound as a selection tool for reducing Achilles tendon reruptures. Am J Sports Med. 2006;34:1395–1400. [DOI] [PubMed] [Google Scholar]
- 9. Lin TW, Cardenas L, Soslowsky LJ. Biomechanics of tendon injury and repair. J Biomech. 2004;37:865–877. [DOI] [PubMed] [Google Scholar]
- 10. Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998;26:266–270. [DOI] [PubMed] [Google Scholar]
- 11. Maffulli N. Current concepts in the management of subcutaneous tears of the Achilles tendon. Bull Hosp Jt Dis. 1998;57:152–158. [PubMed] [Google Scholar]
- 12. Nilsson-Helander K, Silbernagel KG, Thomee R, et al. Acute Achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186–2193. [DOI] [PubMed] [Google Scholar]
- 13. Nilsson-Helander K, Thomeé R, Silbernagel KG, et al. The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med. 2007;35:421–426. [DOI] [PubMed] [Google Scholar]
- 14. Olsson N, Nilsson-Helander K, Karlsson J, et al. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2011;19:1385–1393. [DOI] [PubMed] [Google Scholar]
- 15. Olsson N, Petzold M, Brorsson A, Karlsson J, Eriksson BI, Silbernagel KG. Predictors of clinical outcome after acute Achilles tendon ruptures. Am J Sports Med. 2014;42:1448–1455. [DOI] [PubMed] [Google Scholar]
- 16. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41:2867–2876. [DOI] [PubMed] [Google Scholar]
- 17. Silbernagel KG, Gustavsson A, Thomeé R, Karlsson J. Evaluation of lower leg function in patients with Achilles tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2006;14:1207–1217. [DOI] [PubMed] [Google Scholar]
- 18. Thermann H, Zwipp H. Achilles tendon rupture [in German]. Orthopade. 1989;18:321–333. [PubMed] [Google Scholar]
- 19. Thermann H, Zwipp H, Tscherne H. Functional treatment concept of acute rupture of the Achilles tendon. 2 years results of a prospective randomized study [in German]. Unfallchirurg. 1995;98:21–32. [PubMed] [Google Scholar]
- 20. Voleti PB, Buckley MR, Soslowsky LJ. Tendon healing: repair and regeneration. Annu Rev Biomed Eng. 2012;14:47–71. [DOI] [PubMed] [Google Scholar]