Abstract
Recent increases in state Medicaid payments to nursing homes have the potential to reduce disparities in nurse staffing between facilities with high and low concentrations of racial/ethnic minority residents. Analyses of nursing home and state policy survey data for the period 2001–11 suggest that registered nurse and licensed practical nurse staffing levels increased slightly during this period, regardless of racial/ethnic minority resident concentration. Adjusted disparities in registered nurse hours per resident day between nursing homes with high and low concentrations of racial/ethnic minority residents persisted, although they were reduced. Certified nursing assistant hours per patient day increased in nursing homes with low concentrations of racial/ethnic minorities but decreased in homes with high concentrations, creating a new disparity. Overall, increases in state Medicaid payment rates to nursing homes were associated with improvements in staffing and reduced staffing disparities across facilities, but the adoption of case-mix payments had the opposite effect. Further reforms in health care delivery and payment are needed to address persistent disparities in care between nursing homes serving higher proportions of minority residents and those serving lower proportions, and to prevent unintended exacerbations of such disparities.
Racial and ethnic disparities in the quality of nursing home care have been documented for multiple chronic conditions and nursing areas.[1–4] A large body of literature has also reported that widespread disparities exist across facilities essentially because racial/ethnic minority residents tend to be cared for in facilities with limited financial and clinical resources and high numbers of care deficiencies.[5–10] In a landmark study conducted more than a decade ago, Vincent Mor and coauthors[5] reported that across the United States 40 percent of black residents, but only 9 percent of whites, resided in these lower-tier facilities.
During the past several decades, substantial efforts have been made to address deficiencies in nursing home quality. Studies suggest that quality of care may have improved due to such efforts as improved state Medicaid payment rates[11–14] and national public reporting intended to foster market-driven quality improvements.[15]
As the nursing home industry makes efforts to improve quality in response to state and federal policy initiatives, it is important to recognize that potential improvements in nursing home quality may not automatically benefit all subgroups of patients or facilities equally.[8,9,16–18] Studies have reported that differences in quality and risk-adjusted outcomes between nursing homes with high concentrations of racial/ethnic minority residents and other nursing homes might persist despite evidence of industrywide improvements.
There is a broad consensus—supported by substantial evidence—that higher nurse staffing levels, especially higher registered nurse (RN) hours, improve resident outcomes directly.[16,19–22] Higher staffing levels are also likely to be associated with more individual attention to residents and, therefore, improved quality of life and experience of care.[23] Several population-based studies reported that RN staffing levels, for example, might have improved in the past two decades in nursing homes.[14,24,25]
It has also been shown that nursing facilities with high concentrations of racial/ethnic minority residents tend to have lower nurse staffing levels than other facilities.[5–7] However, it is not known if such disparities have changed in recent years, or if broadly targeted quality efforts, such as improved Medicaid payments, have affected the disparities.
State Medicaid programs cover the majority of nursing home services, paying for roughly 70 percent of total bed days or 50 percent of overall expenses.[11] Thus, Medicaid payment rates and methods are critical factors that determine the level of resources available to nursing homes and the level of care they deliver.[12–14]
Medicaid payment policies vary substantially across states and over time. Mor and coauthors[13] reported that states’ average nursing home payment rates ranged from $91 to $189 per day in 2004. The study also reported that from 1998 to 2004, the inflation-adjusted daily rate had increased from $109 to $131, and the number of states that used payments adjusted by case-mix had increased from twenty-six to thirty-five.
Beyond its potential positive impact on overall staffing rates and nursing home quality,[12–14] the recently increased Medicaid payment rate could help reduce across-facility disparities in staffing for at least two reasons. First, the increased rate is expected to improve the financial status of all facilities, but especially those with high concentrations of Medicaid residents—facilities that also serve disproportionately higher numbers of racial/ethnic minority residents. To the degree that these lower-tier facilities improved their financial performance more substantially as a result of the increased Medicaid payment rate, they could be able to better improve staffing levels and compositions than other facilities (and thus reduce disparities). Second, the fact that these lower-tier facilities originally had lower staffing levels could give them more room for improvements and greater incentives to improve when it becomes financially possible to do so, compared to other facilities.
Previous studies have reported that state adoption of case-mix nursing home reimbursement was associated with reduced nurse staffing and possibly worse resident outcomes.[12–14] In many states case-mix payment systems were primarily designed as a way to contain costs. The systems reimburse nursing homes according to the estimated average use of resources for homogeneous resident groups and do not reimburse nursing homes for costs incurred beyond such estimates. This creates incentives for efficient resource use in nursing homes.
However, as suggested by the literature,[12–14] it may also lead nursing homes to reduce necessary services and staffing levels to lower costs and increase profits. This unintended effect of case-mix payments may be more pronounced in nursing homes with high concentrations of racial/ethnic minority residents, many of which are more financially stressed and face more pressures to minimize costs of care, compared to nursing homes with low concentrations of such residents.
This study tracked the longitudinal trend in nurse staffing levels in nursing homes during the period 2001–11, focusing on disparities between nursing homes with high concentrations of racial/ethnic minority residents and those with low concentrations. Given the prominent role of Medicaid payments in determining nursing home care, we also examined the associations of the Medicaid payment rate and use of the case-mix reimbursement method with nurse staffing levels and disparities in staffing levels over time.
Study Data And Methods
Data And Sample
The primary data source was the 2000–11 Online Survey Certification and Reporting (OSCAR) System files. OSCAR is maintained and updated annually by the Centers for Medicare and Medicaid Services (CMS) for all nursing homes certified by Medicare, Medicaid, or both. OSCAR contains key facility-level information, including self-reported staffing levels, that allows for longitudinal tracking of facility performance. OSCAR data are generally believed to be reliable for research purposes.[26]
We linked the OSCAR files to the publicly available LTCfocus nursing home and state databases.[27]. The LTCfocus files were created by the Center for Gerontology and Healthcare Research at Brown University using multiple sources of data, including the Minimum Data Set, Medicare insurance files, OSCAR, and state policy surveys.
Our sample included data for all freestanding nursing homes in the United States. That is, we excluded the roughly 9 percent of facilities that are affiliated with hospitals because their staffing patterns and patient mix differ from those of freestanding facilities. We also excluded 7,666 facility-years (roughly 5 percent of the total sample) with potentially erroneous staffing data (described below). A small number of observations (roughly 3 percent) with missing information about nursing home concentrations of racial/ethnic minority residents were also excluded.
Our analytic sample consisted of 141,326 facility-years (12,000–13,500 facilities for each year), with nurse staffing measures for 2001–11 and other facility characteristics lagged by one year (2000–10). We included lagged independent variables to temper concerns about potential endogeneity.[13])
Dependent Variables
The dependent variables were hours per resident day for RNs, licensed practical nurses (LPNs), all licensed nurses (RNs and LPNs), certified nursing assistants (CNAs), and all nurses (RNs, LPNs and CNAs); and a measure of nurse skill mix, RN hours per resident day as a percentage of all nurse hours per resident day.[20] Following the procedures adopted by CMS and used in previous studies,[12,16] we cleaned up the staffing data by excluding facilities with zero or more than twenty-four hours of staffing and by excluding remaining facilities with staffing levels outside three standard deviations of the national mean.
Independent Variables
The key independent variable was the percentage of racial/ethnic minority residents (American Africans, Hispanics, Asians or Pacific Islanders, and American Indians or Alaskan Natives) in a nursing home on the first Thursday of April in each year during the period 2000–10. This variable was obtained from the LTCfocus files and was originally defined using the race and ethnicity information in the Minimum Data Set and Medicare enrollment databases.
Our preliminary analyses suggested nonlinear associations of facility racial/ethnic composition with staffing measures. We thus followed a previous national study[8] and categorized facilities into four groups to capture such nonlinear associations: facilities with low concentrations of minority residents (less than 5 percent), medium concentrations (5–14.9 percent), medium-high concentrations (15–34.9 percent), and high concentrations (35 percent or more). We examined alternative cutoff points for categorization in sensitivity analyses; the results remained similar and thus are not presented here.
For each year from 2000 to 2010 we obtained the following facility-level covariates from OSCAR, which had potential associations with nursing home operations and staffing inputs:[10,12,14,16,20] number of beds, affiliation with a chain (yes or no), ownership type (for-profit, nonprofit, or government owned), occupancy rate, percentage of Medicare residents, percentage of Medicaid residents, and location in a rural county (yes or no). We obtained data on the following additional covariates from the LTCfocus facility files, the percentage of female residents, average age of residents, and a facility-level case-mix index that was derived from the Resource Utilization Group (RUG) III classification[28] of all residents in the facility on the first Thursday of April in each year. The case-mix index was calculated by averaging the acuity scores of all residents, with a higher value indicating a higher average acuity.
We also defined a market competition measure using the Herfindahl–Hirschman Index calculated from nursing home beds available in the county each year. Finally, we defined variables for state Medicaid average daily rate and whether the state had implemented a case-mix payment system each year in the period 2000–09 from the LTCfocus state databases (2010 state policy data were not available). Payment rates were inflation-adjusted to 2009 dollars.
Statistical Analysis
In bivariate analyses separately performed for each year, we compared nurse staffing measures and nursing home and county covariates across facility minority concentration groups. Comparisons were made with analysis of variance tests for continuous variables and with chi-square tests for categorical variables.
In multivariable analyses of the longitudinal trend of disparities in nurse staffing during the period 2001–11, we estimated separate linear regressions that modeled each staffing measure as a function of dummies for minority concentration groups (the low concentration group was omitted to serve as the reference group), year dummies (2001 was omitted), their interactions, facility and county covariates, and state dummies. We used facility random effects to control for repeated observations of facilities over time.[29] We did not estimate models with fixed effects given our focus on across-site, instead of within-site, disparities.
In addition, the key independent variable for minority concentration groups was largely time-invariant, given that only about 10 percent of facilities moved from one group to another during the study period. Our definition of this variable allowed for both cross-sectional and secular variations of categorization.
To explore the potential role of Medicaid payment policies in the period 2000–09 in addressing disparities, we further estimated longitudinal random-effects linear regressions with the unit of analysis being the facility-year. In each regression, the staffing measure (for 2001–10) was modeled as a function of minority concentration groups, year dummies, their interactions, the Medicaid daily rate and its interactions with minority concentration groups, use of the case-mix payment method and its interactions with minority concentration groups, facility and county covariates, and state dummies.
Limitations
This study had several potential limitations. First, our analyses of relationships between staffing disparities among nursing homes with different minority concentrations and the Medicaid payment rate and case-mix reimbursement might have been confounded by unmeasured state policy factors (for example, the wage pass-through policies in many states that make additional funds available for direct-care staff members). However, this potential limitation was largely tempered by the statistical controls we used for state dummies and secular trends.
Second, our findings might have been confounded by unmeasured county-level covariates such as community socioeconomic factors. But recent studies[3,8] showed that further controlling for such factors had minimal impacts on estimated across-site disparities.
Finally, nurse staffing variables in the OSCAR files may be subject to self-reporting errors that biased our model’s estimates. However, there is no evidence that potential reporting errors would be more serious in facilities serving largely racial/ethnic minority residents than in other facilities. Thus, our major findings of across-facility disparities should not be biased in any material way.
Study Results
In 2010, 43 percent (12,128) of all freestanding nursing homes had low concentrations of racial/ethnic minority residents. The other three groups—facilities with medium, medium-high, and high concentrations—each accounted for 17–22 percent of freestanding facilities (see online Appendix Exhibit A1).[30] Average minority concentrations ranged from less than 2 percent in the low concentration group to 56 percent in the high concentration group. Key nursing home characteristics such as bed size, profit status, and overall resident sociodemographic status differed significantly across facility groups.
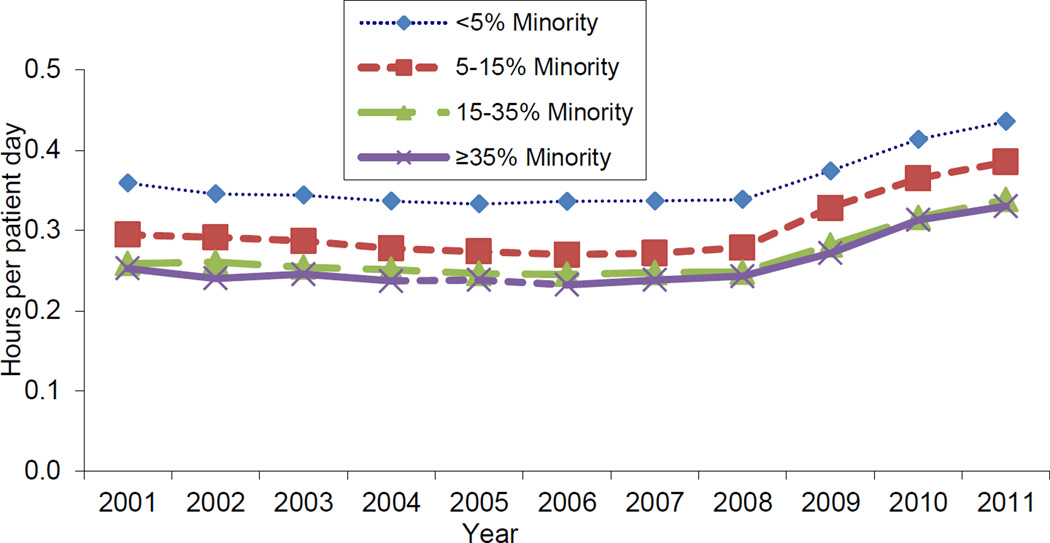
From 2001 to 2011 unadjusted RN staffing levels increased slightly for all facility groups. For example, the level for the low concentration group rose from 0.36 hours per resident day to 0.44 hours, and the level for the high concentration group rose from 0.25 hours per resident day to 0.33 hours—an increase of 0.08 hours, or 4.8 minutes, per resident day in both cases (Exhibit 1).
EXHIBIT 1.
Trends In Unadjusted Registered Nurse Staffing Hours Per Patient Day By Nursing Home Concentration Of Racial/Ethnic Minority Residents, 2001–11
Source/Notes: SOURCE Authors’ analysis of data for 2001–11 from the Online Survey Certification and Reporting (OSCAR) System files and the LTCfocus files (see Note 27 in text). NOTE Concentration groups of minority residents are: low, less than 5%; medium, 5–14.9%; medium-high, 15–34.9%; and high, 35% or more.
However, facilities with high concentrations showed persistently lower RN hours per resident day, and thus a lower skill mix, compared to facilities in the low concentration group (see Appendix Exhibit A5).[30]. Facilities with high concentrations also showed persistently higher LPN hours per resident day, compared to the low concentration group (Appendix Exhibit A2). Not surprisingly, then, the two groups persistently had similar licensed nurse hours (RN and LPN hours combined) (Appendix Exhibit A3).[30]
Multivariable analyses suggested that—after important facility and county covariates and state dummies were adjusted for—the lower RN staffing level found in facilities in the high concentration group, compared to the level in the low concentration group, persisted over time (the disparity was −0.015 in 2001 and −0.012 in 2011; Exhibit 2). However, group differences in LPN staffing and licensed nurse staffing tended to disappear and become insignificant over time.
Exhibit 2.
Nurse Staffing Hours Per Patient Day, By Nursing Home Concentration Of Racial/Ethnic Minority Residents And Year
| Concentration of minority residents |
Adjusted disparitya | Change in adjusted disparity, 2001 to 2011 |
||
|---|---|---|---|---|
| 2001 | 2006 | 2011 | ||
| Registered nurse hours | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium | −0.013*** | −0.010*** | 0.002 | 0.015*** |
| Medium-high | −0.021**** | −0.014*** | −0.006 | 0.016*** |
| High | −0.015*** | −0.009 | −0.012** | 0.003 |
| Licensed practical nurse hours | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium | −0.004 | 0.005 | −0.005 | −0.001 |
| Medium-high | −0.013** | 0.003 | −0.003 | 0.010 |
| High | −0.006 | −0.006 | 0.000 | 0.006 |
| All licensed nurse hours | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium | −0.017*** | −0.006 | −0.004 | 0.013 |
| Medium-high | −0.034**** | −0.012 | −0.010 | 0.025*** |
| High | −0.021*** | −0.017* | −0.013 | 0.008 |
| Certified nursing assistant hours | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium | −0.016 | 0.007 | −0.073**** | −0.057*** |
| Medium-high | 0.013 | 0.013 | −0.132**** | −0.145**** |
| High | 0.047** | 0.004 | −0.155**** | −0.202**** |
| All nurse hours | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium | −0.033** | 0.001 | −0.078**** | −0.045** |
| Medium-high | −0.022 | −0.001 | −0.144**** | −0.122**** |
| High | 0.021 | −0.018 | −0.174**** | −0.195**** |
| Registered nurse hours as a percentage of total nurse hours | ||||
| Low | Ref | Ref | Ref | Ref |
| Medium | −0.359*** | −0.318*** | 0.267** | 0.625**** |
| Medium-high | −0.720**** | −0.421*** | 0.314** | 1.034**** |
| High | −0.628**** | −0.216 | 0.293 | 0.921**** |
SOURCE Authors’ analysis of data for 2001–11 from the Online Survey Certification and Reporting (OSCAR) System files and the LTCfocus files (see Note 27 in text). NOTE Concentration groups of minority residents are: low, less than 5%; medium, 5–14.9%; medium-high, 15–34.9%; and high, 35% or more. All licensed nurses are registered nurses and licensed practical nurses. All nurses are all licensed nurses and certified nursing assistants. Multivariable random-effects linear regression estimated each staffing measure as a function of minority concentration groups, year dummies, and their interactions; bed size; chain affiliation; nonprofit ownership; government ownership; occupancy rate; percentage of Medicare residents; percentage of Medicaid residents; case-mix; percentage of female residents; average age of residents; market competition; rural location; and state dummies. For unadjusted staffing levels in an expanded version of this exhibit, see Appendix Exhibit A6 (see Note 30 in text).
p < 0.05
p < 0.01
p < 0.001
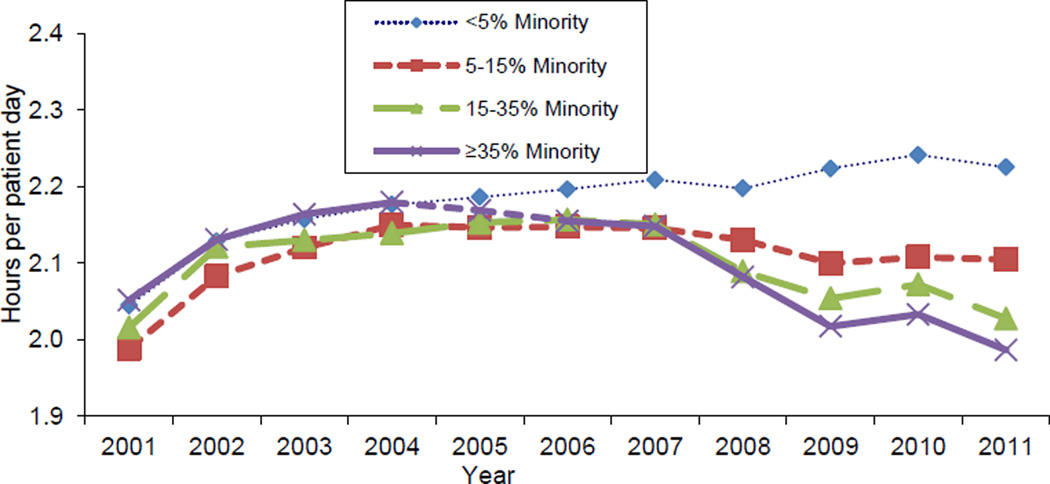
Unadjusted CNA staffing levels increased from 2.04 hours per resident day in 2001 to 2.23 hours per resident day in 2011 for the low concentration group (Exhibit 3). However, for the high concentration group, staffing levels increased slightly between 2001 and 2008 (from 2.05 hours per resident day to 2.08 hours) and then decreased to 1.99 hours per resident day in 2011. Consequently, although disparities in CNA staffing between the two groups were not apparent in 2001, they were in later years of the study period. Multivariable analyses revealed that in 2011, facilities in the high concentration group had an average adjusted CNA staffing level that was 0.155 hours per resident day lower than the level in facilities in the low concentration group (Exhibit 3). The trend in disparities between the low and high concentration groups in the all-nurse (RN, LPN, and CNA) staffing level was similar to that for the CNA staffing level.
EXHIBIT 3.
Trends In Unadjusted Certified Nursing Assistant Staffing Hours Per Patient Day By Nursing Home Concentration Of Racial/Ethnic Minority Residents, 2001–11
Source/Notes: SOURCE Authors’ analysis of data for 2001–11 from the Online Survey Certification and Reporting (OSCAR) System files and the LTCfocus files (see Note 27 in text). NOTE Concentration groups of minority residents are: low, less than 5%; medium, 5–14.9%; medium-high, 15–34.9%; and high, 35% or more.
Exhibit 4 summarizes results of multivariable analyses related to state Medicaid payment policies. We found that each $10 increase in the Medicaid daily rate was associated with higher hours per resident day for every group of nurses except for RNs alone. The increase was also associated with lower nurse skill mix—that is, a reduction in RN hours per patient day as a percentage of all nurse hours.
Exhibit 4.
Effect Of State Nursing Home Payment Policies On Nurse Staffing Hours Per Patient Day And Racial/Ethnic Disparitiesa
| Staffing hours per patient day | ||||||
|---|---|---|---|---|---|---|
| State policy | RN | LPN | All licensed nurse |
CNA | All nurse | RN hours as % of all nurse hours |
| Medicaid payment rate (in $10) | −0.001 | 0.006**** | 0.006*** | 0.006*** | 0.012**** | −0.065**** |
| Case-mix payment (yes or no) | −0.010** | 0.002 | −0.008 | 0.004 | −0.005 | −0.389*** |
| Payment rate (in $10) multiplied by concentration of minority residents | ||||||
| Low | Ref | Ref | Ref | Ref | Ref | Ref |
| Medium | −0.001 | 0.001 | −0.000 | 0.004** | 0.003 | −0.039** |
| Medium-high | 0.002** | 0.002** | 0.004*** | 0.006** | 0.009*** | 0.053** |
| High | 0.004**** | 0.000 | 0.004*** | −0.001 | 0.001 | 0.163**** |
| Case-mix payment multiplied by concentration of minority residents | ||||||
| Low | Ref | Ref- | Ref | Ref | Ref | Ref |
| Medium | −0.001 | 0.000 | −0.001 | 0.003 | 0.002 | −0.033 |
| Medium-high | −0.003 | −0.012** | −0.015** | −0.045*** | −0.061*** | 0.141 |
| High | −0.007 | −0.011 | −0.018** | −0.086**** | −0.106**** | 0.300 |
SOURCE Authors’ analysis of data for 2001–10 from the Online Survey Certification and Reporting (OSCAR) System files and the LTCfocus files (see Note 27 in text). NOTES “All licensed nurses” is registered nurses (RNs) and licensed practical nurses (LPNs). “All nurses” is RNs, LPNs, and certified nursing assistants (CNAs). Concentration groups of minority residents are: low, less than 5%; medium, 5–14.9%; medium-high, 15–34.9%; and high, 35% or more. Multivariable longitudinal (2001–10) random-effects linear regression estimated each staffing measure as a function of minority concentration groups, year dummies, and their interactions; each state policy variable and its interactions with minority concentration groups; bed size; chain affiliation; nonprofit ownership; government ownership; occupancy rate; percentage of Medicare residents; percentage of Medicaid residents; case-mix; percentage of female residents; average age of residents; market competition; rural location; and state dummies.
p < 0.05
p < 0.01
p < 0.001
Higher daily rates may also be associated with slightly reduced disparities in staffing, given the positive and significant estimates for some of the interactive terms of payment rate (Exhibit 4). In contrast, state use of the case-mix payment system was associated with reduced RN hours per resident day. It was also associated in some cases with increased disparities, given the negative and significant estimates for the interactive terms of case-mix payment (Exhibit 4).
Discussion
This national study revealed that during the period 2001–11, RN and LPN staffing increased in nursing homes with high concentrations of racial/ethnic minority residents) and in those with low concentrations (Exhibit 1 and Appendix Exhibit A2). However, facilities serving high concentrations of racial/ethnic minority residents showed persistently lower RN staffing levels over time than nursing homes with low concentrations of these residents, even after multivariable adjustment for facility, market, and state covariates. Meanwhile, CNA staffing levels increased gradually in nursing homes with low concentrations of racial/ethnic minority residents between 2001 and 2011 but decreased in nursing homes in the high concentration group in recent years, which resulted in disparities between the two groups.
Further analyses suggested that increases in the Medicaid nursing home daily rate were associated with both overall improved staffing levels and reduced across-site disparities. In contrast, state use of the case-mix payment system was associated with reduced RN hours and potentially increased disparities in staffing.
Across-Site Disparities In Nurse Staffing
The across-site disparities in RN and CNA staffing are of particular concern because both types of nurses play important roles in appropriate resident care and outcomes. The increased staffing hours for licensed nurses (RNs and LPNs) in all groups of facilities in the past decade are reassuring, and they may have contributed to nationally improved care in nursing homes. Broad improvement in licensed nurse staffing levels may be attributed to such factors as improved state Medicaid reimbursement,[12,14] increased federal and state regulations,[31] and market-oriented initiatives such as public reporting.[15] However, the persistently lower RN staffing level found in nursing homes serving high concentrations of racial/ethnic minority residents suggests that less skilled (and therefore less expensive) LPNs are more likely to be used instead of more skilled RNs in this group of nursing homes, compared to nursing homes with low concentrations of minority residents. Thus, although nursing homes with high concentrations of racial/ethnic minority residents and those with low concentrations may have similar staffing levels for all licensed nurses, the facilities in the high concentration group have a lower nurse skill mix than those in the low concentration group.
Previous studies have demonstrated that higher levels of RN staffing are associated with fewer deficiency citations and reduced severity of cited deficiencies,[19,21,24] as well as with improved resident outcomes such as reduced rates of pressure ulcers, urinary tract infections, and mortality.[19–21] Thus, the enduring disparities in RN staffing between nursing homes in the high concentration group and those in the low concentration group throughout the past decade may have contributed to the enduring disparities in resident outcomes reported previously.[8,9]
The finding of more pronounced across-site disparities in CNA hours since 2008 is also concerning. The reasons for reduced CNA staffing levels at nursing homes in the high concentration group—in spite of the increased CNA staffing levels at homes in the low concentration group—are unknown. Many facilities in the high concentration group rely heavily on payments from Medicaid (which uses a much lower daily rate than private payers do) and are financially strained.[10] Thus, it is possible that the recent recession may have negatively affected the financial performance of nursing homes with high concentrations of racial/ethnic minority residents in particular, leading to CNA staffing reductions in those facilities.
The majority of CNAs are front-line caregivers who assist residents in the activities of daily living (such as dressing and using the toilet) and in ambulation and provide other direct care. Evidence suggests that higher CNA staffing levels are associated with a lower number of cited deficiencies in a nursing home and lower severity of those deficiencies,[24] with improvements in a broad set of clinical outcomes such as pressure ulcers, physical restraint use, and pain management,[19,21,25] and with higher satisfaction with care.[9,23] Given this body of evidence, our finding that CNA staffing levels have fallen in nursing homes with high concentrations of racial/ethnic minority residents since 2008 raises concerns about the potential of impaired care in these facilities, which would disproportionately affect the well-being of those residents.
Potential Impact Of Medicaid Payment Policies
The nursing home industry may have responded to regulatory and market-based quality initiatives and improved the quality of care in recent decades. Nonetheless, the persistent differences in resources and organizational structures between nursing homes in the high concentration group and those in the low concentration group may perpetuate or even increase disparities in quality.[5,8,9,18] Our findings of the enduring disparities in RN staffing levels and the increased disparities in CNA staffing levels between the two groups in recent years seem to support this concern.
One limitation of the extant literature is that it has not determined the potential positive or negative impacts of major quality drivers (for example, Medicaid policies and public reporting) on existing racial/ethnic disparities. Our study addressed this knowledge gap by further exploring the associations between state Medicaid payment policies and nurse staffing. We focused on Medicaid payments, given both the predominant role of Medicaid in financing nursing homes and the readily available data from state policy surveys.
Our findings of improved staffing levels (except for RNs) associated with higher payment rates are consistent with previous findings.[12–14] Meanwhile, the additional increases in staffing hours associated with higher daily rates among facilities in the high concentration group provide empirical evidence that increased Medicaid generosity may benefit these facilities more than those in the low concentration group. That would further help reduce disparities in staffing levels.
The estimated association of state case-mix payment with reduced RN staffing hours in our study is also consistent with findings of previous studies.[12–14] Our findings that case-mix payment was associated with further reductions in both licensed and unlicensed nurse staffing in nursing homes with high concentrations of racial/ethnic minority residents suggest an additional “disparity-increasing” effect of case-mix payment.
Concerns exist that case-mix payment methods may inadvertently lead nursing homes to stint on necessary resident care—for example, by reducing staffing inputs. The negative impact on across-site disparities that we found seems to further suggest that this unintended effect is more evident in nursing homes in the high concentration group, since they are more reliant on (and thus more affected by) Medicaid payment policies, and that their relatively poorer financial status makes them more likely to respond inappropriately to state efforts to contain costs (such as case-mix payments), compared to nursing homes in the low concentration group.
Policy Implications
Our findings have important policy implications. In particular, although the national increase in licensed nurse staffing hours in the past decade are encouraging, the persistent disparities in RN hours between nursing homes in the high concentration group and those in the low concentration group and the reduction in CNA hours in recent years at nursing homes in the high concentration group suggest that future quality initiatives should focus more attention than previously on the disparity issues beyond overall quality deficits inherent to the industry.
State policies may have conflicting impacts on persistent disparities. For example, we found that increasing the payment rate may help improve staffing levels for all groups of nursing homes and reduce across-facility disparities, while implementing case-mix payment may have the opposite effects.
Given the current efforts to rebalance long-term care toward home- and community-based services and the budget shortfalls in many states, it seems unlikely that states will dramatically increase their overall Medicaid payment rates to nursing homes to address staffing deficits and disparities. However, more generous reimbursement targeted to facilities whose residents are predominantly covered by Medicaid and members of racial/ethnic minority groups may be a feasible and effective way to improve overall staffing levels and reduce disparities.
Meanwhile, states that reimburse nursing homes with rates adjusted for case-mix should be aware of the possible negative impacts of that approach on nurse staffing levels (particularly for nursing homes with high concentrations of racial/ethnic minority residents). Those states should make efforts to improve their existing payment systems—for example, by refining their case-mix adjustment methodologies—to minimize such unintended effects.
Finally, current federal and state health care reforms such as Medicare’s bundled-payment programs and the establishment of accountable care organizations are resulting in the development of preferred networks of high-performing providers of postacute and long-term care. These networks may draw resources away from nonpreferred providers, such as nursing facilities with the lowest staffing levels.[32] This could exacerbate across-site disparities in nursing home care. Future studies are necessary to track such possible unintended effects of ongoing health care delivery and payment reforms.
Conclusion
This study found persistently lower RN staffing hours during 2001–11, and lower CNA staffing hours in recent years, for nursing homes with high concentrations of racial/ethnic minority residents, compared to those with low concentrations of such residents. Increasing Medicaid nursing home payment rates was associated with improved staffing levels and reduced staffing disparities across the two groups of facilities, but the use of case-mix payment was associated with worse staffing levels and disparities. Efforts are needed to better address across-facility disparities in nursing home care.
Supplementary Material
Acknowledgments
This study was funded by the National Institute on Minority Health and Health Disparities (NIMHD; Grant No. R01MD007662). The views expressed in this article are those of the authors and do not necessarily represent the views of the NIMHD of the National Institutes of Health.
Contributor Information
Yue Li, Email: yue_li@urmc.rochester.edu, The Department of Public Health Sciences at the University of Rochester, in New York.
Charlene Harrington, Nursing at the University of California, San Francisco.
Dana B. Mukamel, The Department of Medicine of the University of California, Irvine.
Xi Cen, The Department of Public Health Sciences at the University of Rochester.
Xueya Cai, The Department of Biostatistics and Computational Biology at the University of Rochester.
Helena Temkin-Greener, The Department of Public Health Sciences at the University of Rochester.
Notes
- 1.Christian JB, Lapane KL, Toppa RS. Racial disparities in receipt of secondary stroke prevention agents among US nursing home residents. Stroke. 2003;34(11):2693–2397. doi: 10.1161/01.STR.0000096993.90248.27. [DOI] [PubMed] [Google Scholar]
- 2.Li Y, Mukamel DB. Racial disparities in receipt of influenza and pneumococcus vaccinations among US nursing-home residents. Am J Public Health. 2010;(100 Suppl 1):S256–S262. doi: 10.2105/AJPH.2009.173468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y, Glance LG, Yin J, Mukamel DB. Racial disparities in rehospitalization among Medicare patients in skilled nursing facilities. Am J Public Health. 2011;101(5):875–882. doi: 10.2105/AJPH.2010.300055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y, Cai X. Racial and ethnic disparities in social engagement among US nursing home residents. Med Care. 2014;52(4):314–321. doi: 10.1097/MLR.0000000000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fennell ML, Feng Z, Clark MA, Mor V. Elderly Hispanics more likely to reside in poor-quality nursing homes. Health Aff (Millwood) 2010;29(1):65–73. doi: 10.1377/hlthaff.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation disparities in quality across U.S nursing homes. Health Aff (Millwood) 2007;26(5):1448–1458. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- 8.Li Y, Yin J, Cai X, Temkin-Greener J, Mukamel DB. Association of race and sites of care with pressure ulcers in high-risk nursing home residents. JAMA. 2011;306(2):179–186. doi: 10.1001/jama.2011.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y, Ye Z, Glance LG, Temkin-Greener H. Trends in family ratings of experience with care and racial disparities among Maryland nursing homes. Med Care. 2014;52(7):641–648. doi: 10.1097/MLR.0000000000000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chisholm L, Weech-Maldonado R, Laberge A, Lin FC, Hyer K. Nursing home quality and financial performance: does the racial composition of residents matter? Health Serv Res. 2013;48(6 Pt 1):2060–2080. doi: 10.1111/1475-6773.12079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng T, Harrington C, Musumeci M, Reaves EL. Medicaid home and community-based services programs: 2010 data update. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2014. Mar, [Google Scholar]
- 12.Harrington C, Swan JH, Carrillo H. Nurse staffing levels and Medicaid reimbursement rates in nursing facilities. Health Serv Res. 2007;42(3 Pt 1):1105–1129. doi: 10.1111/j.1475-6773.2006.00641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mor V, Gruneir A, Feng Z, Grabowski DC, Intrator O, Zinn J. The effect of state policies on nursing home resident outcomes. J Am Geriatr Soc. 2011;59(1):3–9. doi: 10.1111/j.1532-5415.2010.03230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feng Z, Grabowski DC, Intrator O, Zinn J, Mor V. Medicaid payment rates, case-mix reimbursement, and nursing home staffing—1996–2004. Med Care. 2008;46(1):33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- 15.Mukamel DB, Weimer DL, Spector WD, Ladd H, Zinn JS. Publication of quality report cards and trends in reported quality measures in nursing homes. Health Serv Res. 2008;43(4):1244–1262. doi: 10.1111/j.1475-6773.2007.00829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Serv Res. 2012;47(1 Pt 1):106–128. doi: 10.1111/j.1475-6773.2011.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrington C, Stockton J, Hoopers S. The effects of regulation and litigation on a large for-profit nursing home chain. J Health Polit Policy Law. 2014;39(4):781–809. doi: 10.1215/03616878-2743039. [DOI] [PubMed] [Google Scholar]
- 18.Konetzka RT, Werner RM. Disparities in long-term care: building equity into market-based reforms. Med Care Res Rev. 2009;66(5):491–521. doi: 10.1177/1077558709331813. [DOI] [PubMed] [Google Scholar]
- 19.Harrington C, Kovner C, Mezey M, Kayser-Jones J, Burger S, Mohler M, et al. Experts recommend minimum nurse staffing standards for nursing facilities in the United States. Gerontologist. 2000;40(1):5–16. doi: 10.1093/geront/40.1.5. [DOI] [PubMed] [Google Scholar]
- 20.Konetzka RT, Stearns SC, Park J. The staffing-outcomes relationship in nursing homes. Health Serv Res. 2008;43(3):1025–1042. doi: 10.1111/j.1475-6773.2007.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abt Associates Inc. Appropriateness of minimum nurse staffing ratios in nursing homes: report to Congress: phase II final: volume 1 [Internet] Cambridge (MA): Abt Associates Inc; 2001. Dec 24, [cited 2015 Oct 1]. Available from: http://theconsumervoice.org/uploads/files/issues/CMS-Staffing-Study-Phase-II.pdf. [Google Scholar]
- 22.Harrington C, Choiniere J, Goldmann M, Jacobsen FF, Lloyd L, McGregor M, et al. Nursing home staffing standards and staffing levels in six countries. J Nurs Scholarsh. 2014;44(1):88–98. doi: 10.1111/j.1547-5069.2011.01430.x. [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Cai X, Ye Z, Glance LG, Harrington C, Mukamel DB. Satisfaction with Massachusetts nursing home care was generally high during 2005–09, with some variability across facilities. Health Aff (Millwood) 2013;32(8):1416–1425. doi: 10.1377/hlthaff.2012.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim H, Kovner C, Harrington C, Greene W, Mezey M. A panel data analysis of the relationships of nursing home staffing levels and standards to regulatory deficiencies. J Gerontol B Psychol Sci Soc Sci. 2009;64(2):269–278. doi: 10.1093/geronb/gbn019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castle NG, Anderson RA. Caregiver staffing in nursing homes and their influence on quality of care: using dynamic panel estimation methods. Med Care. 2011;49(6):545–552. doi: 10.1097/MLR.0b013e31820fbca9. [DOI] [PubMed] [Google Scholar]
- 26.Zhang NJ, Paek SC, Wan TT. Reliability estimates of clinical measures between Minimum Data Set and Online Survey Certification and Reporting data of US nursing homes. Med Care. 2009;47(4):492–495. doi: 10.1097/mlr.0b013e31818c014b. [DOI] [PubMed] [Google Scholar]
- 27.LTCfocus [home page on the Internet] Providence (RI): Brown University School of Public Health. [cited 2015 Oct 1]. Available from: http://ltcfocus.org/
- 28.Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III) Med Care. 1994;32(7):668–685. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for mixed models [Internet] 2nd. Cary (NC: SAS Institute Inc; 2006. [cited 2015 Oct 1]. Available from: http://ebooks.cawok.pro/SAS.Publishing.SAS.for.Mixed.Models.2nd.Edition.Mar.2006.pdf. [Google Scholar]
- 30.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 31.Mukamel DB, Weimer DL, Harrington C, Spector WD, Ladd H, Li Y. The effect of state regulatory stringency on nursing home quality. Health Serv Res. 2012;47(5):1791–1813. doi: 10.1111/j.1475-6773.2012.01459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mechanic R. Post-acute care—the next frontier for controlling Medicare spending. N Engl J Med. 2014;370(8):692–694. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.