Abstract
Objectives
Outpatient treatment of acute venous thromboembolism (VTE) requires the selection of patients with a low risk of bleeding during the first few weeks of anticoagulation. The accuracy of four systems, originally derived for predicting bleeding in VTE treated with vitamin K antagonists (VKAs), was assessed in VTE patients treated with rivaroxaban.
Methods
All patients treated with rivaroxaban in the multinational EINSTEIN deep vein thrombosis (DVT) and pulmonary embolism (PE) trials were included. Major bleeding was defined as ≥2 g/dL drop in hemoglobin or ≥2‐unit blood transfusion, bleeding in critical area, or bleeding contributing to death. The authors examined the incidence of major bleeding in patients with low‐risk assignment by the systems of Ruiz‐Gimenez et al. (score = 0 to 1), Beyth et al. (score = 0), Kuijer et al. (score = 0), and Landefeld and Goldman. (score = 0). For clinical relevance, the definition of low risk for all scores except Kuijer includes all patients < 65 years with no prior bleeding history and no comorbid conditions (current cancer, renal insufficiency, diabetes mellitus, anemia, prior stroke, or myocardial infarction).
Results
A total of 4,130 patients (1,731 with DVT only, 2,399 with PE with or without DVT) were treated with rivaroxaban for a mean (±SD) duration of 207.6 (±95.9) days. Major bleeding occurred in 1.0% (40 of 4,130; 95% confidence interval [CI] = 0.7% to 1.3%) overall. Rates of major bleeding for low‐risk patients during the entire treatment period were similar: Ruiz‐Gimenez et al., 12 of 2,622 (0.5%; 95% CI = 0.2% to 0.8%); Beyth et al., nine of 2,249 (0.4%; 95% CI = 0.2% to 0.8%); Kuijer et al., four of 1,186 (0.3%; 95% CI = 0.1% to 0.9%); and Landefeld and Goldman, 11 of 2,407 (0.5%; 95% CI = 0.2% to 0.8%). At 30 days, major bleed rates for low‐risk patients were as follows: Ruiz‐Gimenez et al., five of 2,622 (0.2%; 95% CI = 0.1% to 0.4%); Beyth et al., five of 2,249 (0.2%; 95% CI = 0.1% to 0.5%); Kuijer et al., three of 1,186 (0.3%; 95% CI = 0.1% to 0.7%); and Landefeld and Goldman, seven of 2,407 (0.3%; 95% CI = 0.1% to 0.6%). No low‐risk patient had a fatal bleed.
Conclusions
Four scoring systems that use criteria obtained in routine clinical practice, derived to predict low bleeding risk with VKA treatment for VTE, identified patients with less than a 1% risk of major bleeding during full‐course treatment with rivaroxaban.
Three systematic reviews in patients with pulmonary embolism (PE) have suggested a very low rate of recurrent venous thromboembolism (VTE) associated with home treatment in patients identified as low risk by validated prognostic scores (e.g., Pulmonary Embolism Severity Index, Hestia criteria).1, 2, 3 However, there is uncertainty about the risk of major bleeding during the initial treatment as the third systematic review observed a high relative risk of major bleeding, albeit statistically nonsignificant (relative risk = 4.91, 95% confidence interval [CI] = 0.24 to 101.57; p = 0.30).3
The transformation of the payment structure for health care in the United States toward a fixed‐sum model (e.g., accountable care organization) provides an economic incentive to treat as many VTE patients as safely possible at home. The commercial introduction of direct oral anticoagulants for treatment of VTE has facilitated the ability to treat patients with acute symptomatic deep vein thrombosis (DVT) and PE in the outpatient setting (clinic, emergency department, office or urgent care) without hospitalization.4 However, reluctance for outpatient treatment could be based on the uncertainty about the risk of major bleeding for acute patients treated with direct oral anticoagulants. Accordingly, validated clinical criteria are needed to help clinicians select patients with DVT and PE who are not only at a low risk for recurrent VTE, but also at a low risk of major bleeding.
At least four scoring systems (Landefeld and Goldman,5 Beyth et al.,6 Kuijer et al.,7 and Ruiz‐Gimenez et al.8) have been derived and initially validated to predict risk of major bleeding after starting vitamin K antagonist (VKA) treatment for VTE.5, 6, 7, 8 All of these tools share common predictors, including age, comorbid conditions and, with exception of Kuijer et al., prior bleeding history. Details of the individual scoring systems are provided in Table 1. To our knowledge, no bleeding score has been tested in patients treated with direct oral anticoagulants.
Table 1.
Predictor Variables for Major Bleeding and Their Frequency in the Entire Cohort
| Variable | Points | N (+)a | N (–)b | Missing Values |
|---|---|---|---|---|
| Ruiz‐Gimenez et al.8 (score = 0–1 low risk) | ||||
| Age > 75 yr | 1 | 1,283 (15.5) | 6,998 (84.5) | 0 |
| Active cancer at baseline | 1 | 462 (5.6) | 7,819 (94.4) | 0 |
| Clinically overt PE | 1 | 4,809 (58.1) | 3,472 (41.9) | 0 |
| Recent major bleeding | 2 | 0 | 8,281 (100%) | 0 |
| Creatinine level > 1.2 mg/dL | 1.5 | 915 (11.1) | 7,278 (87.9) | 88 (1.1) |
| Anemia (hemoglobin < 12 g/dL for women and < 13 g/dL for men) | 1.5 | 1,791 (21.6) | 6,408 (77.4) | 82 (1.0) |
| Beyth et al.6 (score = 0 low risk) | ||||
| Age ≥ 65 yr | 1 | 3,085 (37.3) | 5,196 (62.8) | 0 |
| History of stroke | 1 | 222 (2.7) | 8,059 (97.3) | 0 |
| History of gastrointestinal bleeding | 1 | 73 (0.9) | 8,208 (99.1) | 0 |
| Serious comorbid condition (one or more of the following) | 1 | |||
| Renal insufficiency (serum creatinine > 1.5 mg/dL) | 1 | 194 (2.3) | 7,999 (96.6) | 88 (1.1) |
| Recent myocardial infarction | 1 | 0 | 8,081 (100%) | 0 |
| Severe anemia (hemoglobin < 10 g/dL) | 1 | 280 (3.4) | 7,919 (95.6) | 82 (1.0) |
| Diabetes mellitus at baseline | 1 | 840 (10.1) | 7,441 (89.9) | 0 |
| Kuijer et al.7 (score = 0 low risk) | ||||
| Age ≥ 60 yr | 1.6 | 3,969 (48.0) | 4,312 (52.1) | 0 |
| Sex (female) | 1.3 | 3,765 (45.5) | 4,516 (54.5) | 0 |
| Malignancy | 2.2 | 462 (5.6) | 7,819 (94.4) | 0 |
| Landefeld and Goldman5 (score = 0 low risk) | ||||
| Age ≥ 65 yr | 1 | 3,085 (37.3) | 5,196 (62.8) | 0 |
| History of stroke (one of the following) | 1 or 2 | |||
| History of stroke (either current or past) | 1 | 223 (2.7) | 8,465 (97.3) | 0 |
| History of stroke (both current and past) | 2 | 1 (0.01) | 8,280 (99.9) | 0 |
| History of gastrointestinal bleeding | 1 | 73 (0.9) | 8,208 (99.1) | 0 |
| Serious comorbid condition (one or more of the following) | 1 | |||
| Renal insufficiency (serum creatinine > 1.5 mg/dL) | 1 | 194 (2.3) | 7,999 (96.6) | 88 (1.1) |
| Recent myocardial infarction | 1 | 0 | 8,281 (100%) | 0 |
| Severe anemia (hemoglobin < 10 g/dL) | 1 | 280 (3.4) | 7,919 (95.6) | 82 (1.0) |
| Atrial fibrillation | 1 | 190 (2.3) | 8,091 (97.7) | 0 |
Number with the feature.
Number lacking the feature (% of 8,281).
Taking advantage of data from the EINSTEIN DVT and EINSTEIN PE clinical trials, we sought to measure the incidence of major bleeding for patients treated with rivaroxaban who had a low risk for major bleeding according to these scores.9, 10, 11 In addition, we present these incidences for patients who did not have low bleeding risk scores and for patients who were treated with enoxaparin/VKAs.
Methods
Study Design
This was a secondary analysis of data pooled from EINSTEIN DVT and EINSTEIN PE, which were multinational, phase III randomized, open‐label trials. Both trials (NCT numbers 00439777 and 00440193) were sponsored by Bayer Healthcare and Ortho‐McNeil.9, 10, 11 Protocols were approved by institutional review boards, and patients provided written informed consent.
Study Setting and Population
Patients were potentially eligible if they had objectively confirmed symptomatic DVT and/or PE. Patients were excluded for the following reasons: 1) received a therapeutic dose of low‐molecular‐weight heparin, fondaparinux, or unfractionated heparin for more than 48 hours; 2) received more than a single dose of a VKA; 3) the qualifying VTE having been treated with thrombectomy, a vena cava filter, or fibrinolytic therapy; 4) any contraindication listed in the local labeling of enoxaparin, warfarin, or acenocoumarol; 5) an estimated creatinine clearance < 30 mL/min; 6) clinically significant liver disease (e.g., acute hepatitis, chronic active hepatitis, or cirrhosis); 7) systolic blood pressure greater than 180 mm Hg or diastolic blood pressure greater than 110 mm Hg; 8) childbearing potential without proper contraceptive measures, pregnancy, or breast‐feeding; 9) concomitant use of strong cytochrome P‐450 3A4 inhibitors (e.g., human immunodeficiency virus protease inhibitors or systemic ketoconazole) or inducers (e.g., rifampicin, carbamazepine, or phenytoin); and 10) life expectancy of less than 3 months.
Study Protocol
Patients assigned to rivaroxaban were given 15 mg orally twice daily for the first 3 weeks, followed by 20 mg once daily for the intended treatment duration of 3, 6, or 12 months, as determined locally. Patients who were assigned to standard therapy received subcutaneous enoxaparin, 1.0 mg/kg body weight twice daily, and either warfarin or acenocoumarol, started within 48 hours after randomization. Enoxaparin was discontinued when the international normalized ratio (INR) was 2.0 or more for two consecutive days and the patient had received at least 5 days of enoxaparin treatment. The dose of the VKA was adjusted to maintain an INR of 2.0 to 3.0. The INR was determined at least once per month.
Surveillance for Bleeding
In both studies, patients were followed for the intended treatment duration and seen at fixed intervals that were identical for the rivaroxaban and comparison groups, at which time a checklist that included specific questions about bleeding, including its location, severity, and treatment, was completed. Patients were instructed to report to the study center immediately if any bleeding occurred. Bleeding was defined as major if it was clinically overt and associated with a decrease in hemoglobin level of ≥2.0 g/dl; if bleeding led to the transfusion of ≥2 units of red cells; or if bleeding was intracranial or retroperitoneal, occurred in another critical site, or contributed to death.12 Clinically relevant nonmajor bleeding was defined as overt bleeding that did not meet the criteria for major bleeding but was associated with medical intervention, unscheduled contact with a physician, interruption or discontinuation of study drug, or discomfort or impairment of activities of daily life.
Data Analysis
Data for the four bleeding scores were collected directly from data sourced from case report forms for each patient as recorded in the locked database. The hematocrit, graded as abnormal when lower than 30%, as required by the Landefeld and the Beyth risk scores, was not collected in the EINSTEIN studies and operationalized as a hemoglobin below 10 g/dL. Any missing data were assumed to fall in the normal or negative range for the purpose of computing each score. Data were extracted using scripts written in SAS (version 9.2). Success was defined as an upper limit of the 95% exact CI of the incidence of major bleeding below 1.0%. Bleeding rates were calculated both for the entire treatment period and for the first 30 days.
Results
In the pooled sample, a total of 8,281 patients with valid informed consent were randomized at 314 sites in 38 countries.11 Figure 1 shows the flow of patients, of whom 4,130 received treatment with rivaroxaban and 4,116 enoxaparin/VKA, for mean (±SD) durations of 207.6 (±95.9) and 203.8 (±97.4) days, respectively. Table 1 shows the distribution of the components of the four scoring systems, including the numbers of missing data. No patients had recent bleeding as this was an exclusion to enrollment. Table 2 shows the demographic features and past medical history of patients with DVT only (EINSTEIN DVT) or PE with or without DVT (EINSTEIN PE) and the pooled sample. The proportions of patients with older age, recent surgery, active cancer, and immobility were not different between the treatment groups and between the EINSTEIN DVT and EINSTEIN PE studies.
Figure 1.
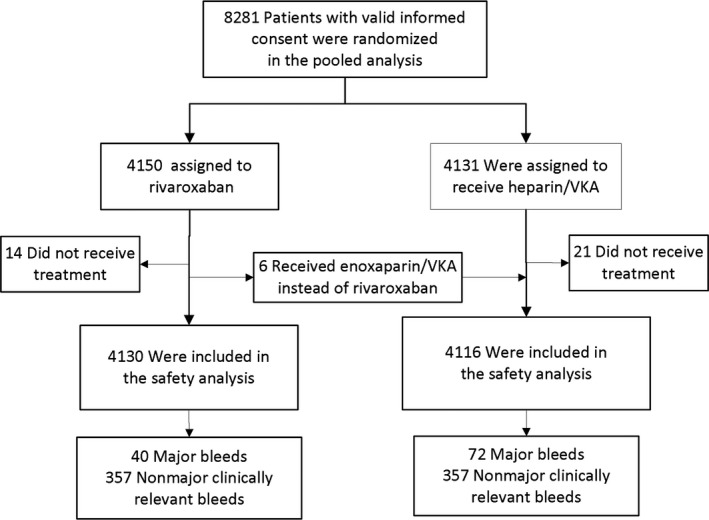
Flow diagram showing numbers of patients enrolled and their bleeding‐related outcomes in each treatment arm. VKA = vitamin K antagonist.
Table 2.
Demographic and Clinical Characteristics
| Characteristic | EINSTEIN DVT | EINSTEIN PE | EINSTEIN Pooled | |||
|---|---|---|---|---|---|---|
| Rivaroxaban | Heparin/ VKA | Rivaroxaban | Heparin/ VKA | Rivaroxaban | Heparin/ VKA | |
| (N = 1,731) | (N = 1,718) | (N = 2,419) | (N = 2,413) | (N = 4,150) | (N = 4,131) | |
| Male sex | 993 (57.4) | 967 (56.3) | 1309 (54.1) | 1247 (51.7) | 2302 (55.5) | 2214 (53.6) |
| Age (yr) | 55.8 ± 16.4 | 56.4 ± 16.3 | 57.9 ± 17.3 | 57.5 ± 17.2 | 57.0 ± 17.0 | 57.0 ± 16.8 |
| Race (white) | 1,327 (76.7) | 1,319 (76.8) | 1,585 (65.5) | 1,587 (65.8) | 2,912 (70.2) | 2,906 (70.3) |
| Recent surgery or trauma | 338 (19.5) | 335 (19.5) | 415 (17.2) | 398 (16.5) | 753 (18.1) | 733 (17.7) |
| Previous VTE | 336 (19.4) | 330 (19.2) | 455 (18.8) | 489 (20.3) | 791 (19.1) | 819 (19.8) |
| Active cancer | 118 (6.8) | 89 (5.2) | 114 (4.7) | 109 (4.5) | 232 (5.6) | 198 (4.8) |
| Immobilization | 265 (15.3) | 260 (15.1) | 384 (15.9) | 380 (15.7) | 649 (15.6) | 640 (15.5) |
| Known thrombophilic condition | 107 (6.2) | 116 (6.8) | 138 (5.7) | 121 (5.0) | 245 (5.9) | 237 (5.7) |
| Unprovoked VTE | 1,055 (60.9) | 1,083 (63.0) | 1,566 (64.7) | 1,551 (64.3) | 2,621 (63.1) | 2,634 (63.8) |
| Duration of treatment (days)a | 193.6 ± 89.3 | 187.5 ± 92.5 | 216.3 ± 98.7 | 214.3 ± 98.9 | 207.6 ± 95.9 | 203.8 ± 97.4 |
Data are shown as n (%) or mean ± SD.
Duration of actual study treatment after randomization until end of treatment (safety population).
DVT = deep venous thrombosis; PE = pulmonary embolism; VKA = vitamin K antagonist; VTE = venous thromboembolism.
Overall, major bleeding occurred in 40 of 4,130 (1.0%, 95% CI = 0.7% to 1.3%) patients treated with rivaroxaban during the entire study period and occurred at a mean (±SD) of 69 (±72.5) days (median 43 days, interquartile range = 7.5–117.5 days) of treatment. Of the patients treated with rivaroxaban, 2,622 (63.6%), 2,249 (54.5%), 1,186 (28.7%), and 2,407 (58.3%) qualified for the low‐risk categories according to the scoring systems of Ruiz‐Gimenez et al., Beyth et al., Kuijer et al., and Landefeld and Goldman, respectively. The incidences of major bleeding for the entire treatment period in these patients were as follows: Ruiz‐Gimenez et al., 12 of 2,622 (0.5%, 95% CI = 0.2% to 0.8%); Beyth et al., nine of 2,249 (0.4%, 95% CI = 0.2% to 0.8%); Kuijer et al., four of 1,186 (0.3%, 95% CI = 0.1% to 0.9%); and Landefeld and Goldman, 11 of 2,407 (0.5%, 95% CI = 0.2% to 0.8%). Incidences of major bleeding during the entire treatment period in other risk categories and in the enoxaparin/VKA group are given in Table 3.
Table 3.
Rate of Major Bleeding According to Score, Observation Period, and Treatment
| System | Score Points | Rivaroxaban | H/VKA | ||||
|---|---|---|---|---|---|---|---|
| Subjects per Score Category, n (%) (N = 4,130) | Number During Days 1–30 (%; 95% CI) | Number During Entire Study Period (%; 95% CI) | Subjects per Score Category, n (%) (N = 4,116) | Number During Days 1–30 (%; 95% CI) | Number During Entire Study Period (%; 95% CI) | ||
| Ruiz‐Gimenez et al.8 | Low (0–1) | 2,622 (63.6) | 5 (0.2; 0.1–0.4) | 12 (0.5; 0.2–0.7) | 2,638 (64.1) | 9 (0.3; 0.2–0.7) | 25 (0.9; 0.5–1.3) |
| Moderate (1.5–2) | 569 (13.8) | 5 (0.9; 0.3–2.0) | 8 (1.4; 0.4–2.4) | 617 (15.0) | 10 (1.6; 0.8–2.9) | 15 (2.4; 1.2–3.6) | |
| High (>2) | 939 (22.7) | 7 (0.7; 0.3–1.5) | 20 (2.1; 1.2–3.1) | 861 (20.9) | 17 (2.0; 1.2–3.1) | 32 (3.7; 2.4–5.0) | |
| Beyth et al.6 | Low (0) | 2,249 (54.5) | 5 (0.2; 0.1–0.5) | 9 (0.4; 0.2–0.8) | 2,274 (55.2) | 7 (0.3; 0.1–0.6) | 18 (0.8; 0.5–1.2) |
| Moderate (1–2) | 1,850 (44.8) | 12 (0.6; 0.3–1.1) | 31 (1.7; 1.1–2.3) | 1,816 (44.1) | 27 (1.5; 1.0–2.1) | 52 (2.9; 2.1–3.6) | |
| High (>2) | 31 (0.8) | 0 | 0 | 26 (0.6) | 2 (7.7; 0.9–23.5) | 2 (7.7; 0.9–23.5) | |
| Kuijer et al.7 | Low (0) | 1,186 (28.7) | 3 (0.3; 0.1–0.7) | 4 (0.3; 0.1–0.9) | 1,157 (28.1) | 4 (0.3; 0.1–0.9) | 8 (0.7; 0.3–1.3) |
| Moderate (1–3) | 2,726 (66.0) | 12 (0.4; 0.2–0.8) | 33 (1.2; 0.8–1.7) | 2,778 (67.5) | 25 (0.9; 0.6–1.3) | 56 (2.0; 1.5–2.6) | |
| High (≥3) | 218 (5.3) | 2 (0.9; 0.1–3.2) | 3 (1.4; 0.3–3.9) | 181 (4.4) | 7 (3.9; 1.5–7.5) | 8 (4.4; 1.8–8.2) | |
| Landefeld and Goldman5 | Low (0) | 2,407 (58.3) | 7 (0.3; 0.1–0.6) | 11 (0.5; 0.2–0.8) | 2,412 (58.6) | 7 (0.3; 0.1–0.6) | 18 (0.7; 0.4–1.2) |
| Moderate (1–2) | 1,694 (41.0) | 10 (0.6; 0.3–1.1) | 29 (1.7; 1.1–2.4) | 1,679 (40.8) | 27 (1.6; 1.0–2.3) | 51 (3.0; 2.2–3.9) | |
| High (>2) | 29 (0.7) | 0 | 0 | 25 (0.6) | 2 (8.0; 0.9–24.3) | 3 (12.0; 2.3–28.2) | |
H/VKA = heparin/vitamin K antagonist.
None of the low‐risk rivaroxaban‐treated patients by any system had a fatal bleed. Incidences of major bleeding in low‐risk patients at 30 days were as follows: Ruiz‐Gimenez et al., five of 2,622 (0.2, 95% CI = 0.1% to 0.4%); Beyth et al., five of 2,249 (0.2, 95% CI = 0.1% to 0.5%); Kuijer et al., three of 1,186 (0.3, 95% CI = 0.1% to 0.7%); and Landefeld and Goldman, seven of 2,407 (0.3, 95% CI = 0.1% to 0.6%). Incidences of major bleeding in the first 30 days in other risk categories and in the enoxaparin/VKA group are given in Table 3. Only one low‐risk enoxaparin/VKA‐treated patient had fatal bleeding.
The rates of clinically relevant nonmajor bleeding for the different risk categories according to time at risk (entire study period, first 30 days) are shown in Table 4. In general, patterns were similar to the results observed for major bleeding and the risks of clinically relevant nonmajor bleeding were lowest in those patients qualifying for “low risk,” according to the scoring system.
Table 4.
Rate of Clinically Relevant Nonmajor Bleeding According to Score, Observation Period, and Treatment
| System | Score Points | Rivaroxaban | H/VKA | ||||
|---|---|---|---|---|---|---|---|
| Subjects per Score Category, n/N (%) (N = 4,130) | Number During Days 1–30 (%; 95% CI) | Number During Entire Study Period (%; 95% CI) | Subjects per Score Category, n/N (%) (N = 4,116) | Number During Days 1–30 (%; 95% CI) | Number During Entire Study Period (%; 95% CI) | ||
| Ruiz‐Gimenez et al.8 | Low (0–1) | 2,622 (63.6) | 88 (3.4; 2.7–4.1) | 180 (6.9; 5.9–7.8) | 2,638 (64.1) | 88 (3.3; 2.7–4.0) | 207 (7.8; 6.8–8.9) |
| Moderate (1.5–2) | 569 (13.8) | 31 (5.5; 3.5–7.3) | 56 (9.8; 7.4–12.3) | 617 (15.0) | 28 (4.5; 2.9–6.2) | 57 (9.2; 6.9–11.5) | |
| High (>2) | 939 (22.7) | 67 (7.1; 5.4–8.7) | 121 (12.9; 10.7–15.0) | 861 (20.9) | 40 (4.7; 3.2–6.1) | 93 (10.8; 8.7–12.9) | |
| Beyth et al.6 | Low (0) | 2,249 (54.5) | 79 (3.5; 2.7–4.2) | 159 (7.1; 5.6–7.7) | 2,274 (55.2) | 63 (2.8; 2.1–3.4) | 169 (7.4; 5.9–8.0) |
| Moderate (1–2) | 1,850 (44.8) | 105 (5.7; 4.4–6.5) | 194 (10.5; 8.3–10.8) | 1,816 (44.1) | 91 (5.0; 3.9–5.8) | 185 (10.2; 8.0–10.6) | |
| High (>2) | 31 (0.8) | 2 (6.5; 0.7–20.2) | 4 (12.9; 3.2–26.7) | 26 (0.6) | 2 (7.7; 0.9–23.5) | 3 (11.5; 2.2–27.4) | |
| Kuijer et al.7 | Low (0) | 1,186 (28.7) | 31 (2.6; 1.7–3.6) | 65 (5.5; 4.0–6.6) | 1,157 (28.1) | 27 (2.3; 1.5–3.3) | 68 (5.9; 4.3–7.0) |
| Moderate (1–3) | 2,726 (66.0) | 140 (5.1; 4.1–5.7) | 267 (9.8; 7.9–10.0) | 2,778 (67.5) | 119 (4.3; 3.4–4.9) | 268 (9.6; 7.8–9.9) | |
| High (≥3) | 218 (5.3) | 15 (6.9; 3.6–10.4) | 25 (11.5; 6.8–14.8) | 181 (4.4) | 10 (5.5; 2.5–9.4) | 21 (11.6; 6.6–15.5) | |
| Landefeld and Goldman8 | Low (0) | 2,407 (58.3) | 90 (3.7; 2.9–4.4) | 175 (7.3; 5.8–7.8) | 2,412 (58.6) | 70 (2.9; 2.2–3.5) | 180 (7.5; 6.0–8.0) |
| Moderate (1–2) | 1,694 (41.0) | 93 (5.5; 4.2–6.3) | 177 (10.4; 8.2–10.9) | 1,679 (40.8) | 82 (4.9; 3.7–5.7) | 173 (10.3; 8.1–10.8) | |
| High (>2) | 29 (0.7) | 3 (10.3; 2.0–25.0) | 5 (17.2; 5.0–31.1) | 25 (0.6) | 4 (16.0; 3.9–31.7) | 4 (16.0; 3.9–31.7) | |
Discussion
Patients with VTE who were treated with rivaroxaban, and who were at low risk for major bleeding based on scores developed for bleeding during VKA treatment, had no fatal bleeding and a low incidence of major bleeding, with the upper limit of the 95% CI excluding an incidence of higher than 1%. This result was observed for both the initial 30‐day and the entire treatment period and was consistent among all four evaluated bleeding risk scoring systems. The scoring system according to Ruiz‐Giminez et al. classified the highest number of patients as low risk and had the lowest incidence of major bleeding during the initial 30 days of treatment.
From a clinician's stance, the important message of this analysis is that VTE patients under age 65 years with normal renal function, no anemia or history of overt bleeding, and no history of cancer or stroke, have a low 30‐day risk to develop major bleeding when treated with rivaroxaban. The criteria for all scores can be obtained at the bedside and from routinely performed laboratory studies (complete blood count and renal function studies). Interestingly, the incidences of major bleeding in all low‐risk categories of the four scoring systems were consistently lower in rivaroxaban recipients compared to those receiving standard anticoagulation with enoxaparin, followed by VKA. In this latter group, the upper limit of the 95% CI of major bleeding in the low‐risk categories of the four scores did not exclude an incidence of major bleeding of more than 1%, despite the relative large number of patients in these categories.
In current practice, physicians admit most patients with acute PE diagnosed in the outpatient or emergency care setting.13 However, it should be realized that many patients who have acute symptomatic DVT, including those who are currently treated on an outpatient basis, may also have concomitant asymptomatic PE.14 Indeed, there are risk scores to identify PE patients at low risk of recurrence who might be treated at home. In an unselected cohort of 291 patients with PE, seven (2.4%) deteriorated during the first 5 days primarily due to bleeding on heparin‐VKA.15 The current analysis suggests that the application of a simple bleeding risk score could reduce this proportion substantially. Strengths of our analyses include the prospective data collection, monitoring for source verification, completeness of follow‐up, and the independent assessment of outcomes.
Limitations
Limitations include the fact that this analysis, despite prospective data collection, was defined retrospectively and patients were not managed based on their bleeding risk scores. In addition, baseline data were missing in a fraction of patients for hemoglobin and creatinine, and we assumed that these values in those patients were normal. This constitutes a conservative bias. Moreover, some items of the bleeding risk score were not specifically asked for but were part of the elicited general medical history and were assumed to be present or absent based on this information only, which could have added noise. Finally, we analyzed major bleeding during the first 30 days of treatment and the entire treatment period, while physicians for their decision making might be most interested in major bleeding that occurs very early during treatment. It should be noted that all four scoring systems only require standard clinical data available from the patient or medical records.
Potential limitations to adoption include the fact that these data represent the result of patients who consented to participate in a randomized trial and were then monitored closely as part of the study protocol. It is possible that the EINSTEIN sample has fewer comorbidities and higher compliance rate than would occur in a real‐world setting. For example, the Ruiz‐Gimenez score was ≤1 in 64% (95% CI = 63% to 65%) of all patients in the present study, which appears to be significantly higher than the 44% (95% CI = 43% to 46%) who were low risk in the RIETE registry.8 Additionally, the present data do not assess risk of bleeding in later years of treatment.
Conclusions
All four scoring systems derived to predict low bleeding risk with vitamin K antagonist treatment excluded a higher than 1% risk of major bleeding in the low‐risk category within the entire treatment period with rivaroxaban. The Ruiz‐Gimenez et al. score ≤ 1 occurred in the largest fraction of patients and had the lowest rate of major bleeding at 30 days. This score could be used to supplement other criteria to select venous thromboembolism patients at low risk for complications for outpatient treatment with rivaroxaban
Academic Emergency Medicine 2016;23:144–150 © 2016 by the Society for Academic Emergency Medicine26765080
Disclosures: Jeffrey A. Kline—consultant, Janssen and Stago Diagnostica; grant support, Ikaria and NIH (R); David Jimenez—consultant, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Daiichi Sankyo, Leo Pharma, Pfizer, Sanofi, and Rovi. (A); D. Mark Courtney—Grant support, Stago Diagnostica; Juliana Ianus—employee, Division of Biostatistics, Medical Affairs (Cardiovascular and Metabolism), and Janssen Research and Development, LLC; Lynn Cao—employee, programming, Janssen Research and Development, LLC; Anthonie W.A. Lensing—employee, Bayer Healthcare; Martin H. Prins—consultant, Bayer, Sanofi Aventis, Boehringer Ingelheim, GlaxoSmithKline, Daiichi Sankyo, LEOPharma, ThromboGenics and Pfizer; Philip S. Wells—consultant, Bayer, Bristol Myers Squibb, and Daiichi Sankyo. Drs. Kline and Courtney, both editors at this journal, had no role in the peer‐review process or publication decision for this paper.
References
- 1. Vinson DR, Zehtabchi S, Yealy DM. Can selected patients with newly diagnosed pulmonary embolism be safely treated without hospitalization? A systematic review. Ann Emerg Med 2012;60:651–62. [DOI] [PubMed] [Google Scholar]
- 2. Piran S, Le GG, Wells PS, et al. Outpatient treatment of symptomatic pulmonary embolism: a systematic review and meta‐analysis. Thromb Res 2013;132:515–9. [DOI] [PubMed] [Google Scholar]
- 3. Yoo HH, Queluz TH, El Dib R. Outpatient versus inpatient treatment for acute pulmonary embolism. Cochrane Database Syst Rev 2014;11:CD010019. [DOI] [PubMed] [Google Scholar]
- 4. Beam DM, Kahler ZP, Kline JA. Immediate discharge and home treatment of low risk venous thromboembolism diagnosed in two U.S. emergency departments with rivaroxaban: a one‐ year preplanned analysis. Acad Emerg Med 2015;22:788–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Landefeld CS, Goldman L. Major bleeding in outpatients treated with warfarin: incidence and prediction by factors known at the start of outpatient therapy. Am J Med 1989;87:144–52. [DOI] [PubMed] [Google Scholar]
- 6. Beyth RJ, Quinn LM, Landefeld CS. Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin. Am J Med 1998;105:91–9. [DOI] [PubMed] [Google Scholar]
- 7. Kuijer PM, Hutten BA, Prins MH, Buller HR. Prediction of the risk of bleeding during anticoagulant treatment for venous thromboembolism. Arch Intern Med 1999;159:457–60. [DOI] [PubMed] [Google Scholar]
- 8. Ruiz‐Gimenez N, Suarez C, Gonzalez R, et al. Predictive variables for major bleeding events in patients presenting with documented acute venous thromboembolism. Findings from the RIETE Registry. Thromb Haemost 2008;100:26–31. [DOI] [PubMed] [Google Scholar]
- 9. Bauersachs R, Berkowitz SD, Brenner B, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 2010;363:2499–510. [DOI] [PubMed] [Google Scholar]
- 10. Buller HR, Prins MH, Lensin AW, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 2012;366:1287–97. [DOI] [PubMed] [Google Scholar]
- 11. Prins MH, Lensing AW, Bauersachs R, et al. Oral rivaroxaban versus standard therapy for the treatment of symptomatic venous thromboembolism: a pooled analysis of the EINSTEIN‐DVT and PE randomized studies. Thromb J 2013;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. J Thromb Haemost 2005;3:692–4. [DOI] [PubMed] [Google Scholar]
- 13. ˜Vinson DR, Drenten CE, Huang J, et al. Impact of relative contraindications to home management in emergency department patients with low‐risk pulmonary embolism. Ann Am Thorac Soc 2015;12:666–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tzoran I, Saharov G, Brenner B, et al. Silent pulmonary embolism in patients with proximal deep vein thrombosis in the lower limbs. J Thromb Haemost 2012;10:564–71. [DOI] [PubMed] [Google Scholar]
- 15. Kabrhel C, Okechukwu I, Hariharan P, et al. Factors associated with clinical deterioration shortly after PE. Thorax 2014;69:835–42. [DOI] [PubMed] [Google Scholar]


