Abstract
Objectives: Racial/ethnic disparities in nursing homes (NHs) are associated with lower quality of care, and state Medicaid payment policies may influence NH quality. However, no studies analyzing disparities in NH quality of life (QoL) exist. Therefore, this study aims to estimate associations at the NH level between average number of QoL deficiencies and concentrations of racial/ethnic minority residents, and to identify effects of state Medicaid payment policies on racial/ethnic disparities. Method: Multivariable Poisson regression with NH random effects was used to determine the association between NH minority concentration in 2000 to 2010 and average number of QoL deficiencies in 2001 to 2011 at the NH level, and the effect of state NH payment policies on QoL deficiencies and racial/ethnic disparities in QoL deficiencies across NH minority concentrations. Results: Racial/ethnic disparities in QoL between high and low minority concentration NHs decrease over time, but are not eliminated. Case mix payment was associated with an increased disparity between high and low minority concentration NHs in QoL deficiencies. Discussion: NH managers and policy makers should consider initiatives targeting minority residents or low-performing NHs with higher minority concentrations for improvement to reduce disparities and address QoL deficiencies.
Keywords: nursing homes, racial/ethnic disparities, quality of life, deficiency citations, Medicaid payment
Introduction
Racial/ethnic disparities in nursing home (NH) quality have long been a concern for NH residents and policy makers, and exist in both clinical and interpersonal aspects of NH care. For example, Black NH residents have higher risk-adjusted rates of pressure ulcers (Li, Yin, Cai, Temkin-Greener, & Mukamel, 2011) and lower rates of annual influenza vaccination (Cai, Feng, Fennell, & Mor, 2011), compared with White residents. Racial/ethnic minority residents are also less socially engaged than non-Hispanic White residents (Li & Cai, 2014). Although minority access to NH care has increased in recent years, this is likely due to wealthier, non-Hispanic White elderly taking advantage of preferable assisted living and community-based options (Feng, Fennell, Tyler, Clark, & Mor, 2011; Kane & Kane, 2001; Reinhard, 2010), and may indicate inequities in minority access to these care alternatives (Feng et al., 2011).
Historically, NHs have been highly segregated, and this trend has persisted in recent years. NHs serving high proportions of minority residents tend to provide lower quality of care, often having a higher average number of deficiencies, as well as lower levels of direct care staffing and lower ratios of registered nurse (RN) staffing (Fennell, Feng, Clark, & Mor, 2010; Smith, Feng, Fennell, Zinn, & Mor, 2007, 2008). NHs that serve higher proportions of minorities usually also serve higher proportions of Medicaid residents and, because of this, face clinical and financial resource constraints; these NHs are less financially viable, due in part to an inability to cross-subsidize from private payers or Medicare, and are more likely to have their participation in Medicaid and Medicare programs terminated (Mor, Zinn, Angelelli, Teno, & Miller, 2004).
Subsequently, racial/ethnic disparities in NH quality of care are largely driven by site of care disparities, differences in where minority residents receive care, as opposed to disparities in care provided to minority and non-Hispanic White residents cared for in the same NHs. Site of care disparities influence not only clinical quality but also quality of life (QoL) of the residents. For example, in a study of resident and family member satisfaction, Li and colleagues found that site of care disparities existed over years in overall NH ratings, recommendation rate, and ratings on individual domains of resident life and care, with minority-serving NHs having lower satisfaction scores (Li, Ye, Glance, & Temkin-Greener, 2014).
Moreover, overall NH quality and QoL performance may have changed in recent years due to changes in federal and state policies (Harrington & Carrillo, 1999; Zhang & Grabowski, 2004). In the late 1980s, Congress passed the Nursing Home Reform Act, which was meant to improve NH care by increasing government regulation, and established federal requirements for NH certification. Following its enactment, studies found some quality improvements, including decreases in rates of pressure ulcers, physical restraint use, and urinary catheterization (Zhang & Grabowski, 2004), but average number of deficiencies at the NH level generally remained high (Harrington & Carrillo, 1999). Changes in Medicaid reimbursement rates may also influence NH quality and are associated with some improvements in resident outcomes, such as performance in activities of daily living, physical restraint use, and pressure ulcers (Grabowski, Angelelli, & Mor, 2004; Mor et al., 2011), but with mixed effects on nurse staffing (Feng, Grabowski, Intrator, Zinn, & Mor, 2008; Harrington, Swan, & Carrillo, 2007). An additional payment strategy, case mix reimbursement, attempts to “level the playing field,” reimbursing NHs with sicker, more costly residents at a higher rate (Feng, Grabowski, Intrator, & Mor, 2006). However, case mix reimbursement has been found to have mixed effects on NH quality, measured by staffing intensity and staffing mix (Harrington et al., 2007), and likelihood of meeting recommended nurse staffing levels (Feng et al., 2008). Although no associations with resident outcomes were found (Mor et al., 2011), case mix reimbursement is associated with increased resident acuity in NHs, suggesting that access to NH care for higher acuity Medicaid recipients may improve under case mix adjustment (Feng et al., 2006). Overall, federal and state policies and quality improvement initiatives may have mixed effects on NH quality of care and, therefore, on racial/ethnic disparities in NH quality.
Although racial/ethnic disparities in NH quality and resident outcomes have been widely documented, no national studies analyzing racial/ethnic disparities in resident QoL exist. Prior studies have reported on racial/ethnic disparities in NH residents’ QoL (Li et al., 2014), but have not identified national trends in racial/ethnic disparities in NH QoL. Recent studies have also analyzed racial/ethnic disparities in NH care deficiencies nationally (Li, Harrington, Temkin-Greener, et al., 2015), but did not consider racial/ethnic disparities in QoL. In addition, to our knowledge, only one study has examined the impact of state Medicaid payment policies on racial/ethnic disparities in NH care deficiencies (Li, Harrington, Temkin-Greener, et al., 2015). However, this study did not analyze the effects of these policies on NH QoL deficiencies, which measure overall resident experience in NHs, including patient autonomy, NH environment, and programming efforts (Harrington, Woolhandler, Mullan, Carrillo, & Himmelstein, 2002; Harrington, Zimmerman, Karon, Robinson, & Beutel, 2000).
Therefore, this study aims to address this knowledge gap by (a) examining longitudinal trends in racial/ethnic disparities in NHs’ QoL performance, measured by number of QoL deficiencies NHs received during 2001 to 2011, and (b) identifying effects of state Medicaid payment policies, namely, Medicaid payment rate and case mix adjustment, on these disparities.
Method
Data and Sample
Data were gathered from Online Survey, Certification, and Reporting (OSCAR) files and linked to Long Term Care Focus (LTCFocus) NH and state files for 2000 to 2011. OSCAR, maintained by the Centers for Medicare and Medicaid Services, is an inclusive source of NH level data, including structural and organizational characteristics and quality information. OSCAR is widely used for tracking NH quality of care and policy analyses (Harrington & Carrillo, 1999; Li & Cai, 2014; Li et al., 2011; Mor et al., 2004). LTCFocus files are publicly available as part of the Shaping Long-Term Care in America Project at the Center for Gerontology and Healthcare Research at Brown University (funded in part by the National Institute on Aging; http://ltcfocus.org), and combine multiple data sources, including the Minimum Data Set, OSCAR, state policy data, and the Area Resource File (LTCFocus, 2015).
The study sample includes approximately 14,000 free-standing NHs in the United States from 2000 to 2011. Hospital-based NHs were excluded from analyses because they serve only short-term residents, and are likely different from other NHs serving both short- and long-term residents in their care patterns, staffing levels, and case mix. After excluding hospital-based NHs, information on minority resident concentration was available for roughly 97% of NHs. The analytical sample included 147,435 facility-years and their deficiencies for 2001 to 2011. Other NH characteristics included in the analyses were lagged by 1 year (for an analytical period from 2000 to 2010) to eliminate potential endogeneity problems (Mor et al., 2011).
QoL Deficiency Citations
The dependent variable in the analyses was average number of QoL deficiencies at the NH level in each year between 2001 and 2011, which was obtained from OSCAR files of corresponding years. All Medicare and/or Medicaid-certified NHs undergo on-site inspections every 9 to 15 months where surveyors assess compliance with standards of care, including QoL. On the survey, there are 19 tags in the QoL deficiency group, concerned with overall resident experience in NHs, including patient autonomy (e.g., patients’ rights, physical restraint use, and practices regarding admission, transfer, and discharge), NH environment (such as facility décor, maintenance, and upkeep), and programming efforts (including social services, activities, and entertainment; Harrington et al., 2002; Harrington et al., 2000).
Independent Variables
The primary independent variable was NH concentration of racial/ethnic minority residents during 2000-2010 (lagged by 1 year). Preliminary analyses of associations between NH minority concentration and deficiency measures suggested non-linear associations; therefore, NHs were categorized as having a low concentration (<5%), medium concentration (5%-15%), medium-high concentration (15%-35%), and high concentration (≥35%) of racial/ethnic minority residents. These categories are consistent with those used in prior national analyses (Li, Harrington, Mukamel, et al., 2015; Li, Harrington, Temkin-Greener, et al., 2015; Li et al., 2011). In addition, sensitivity analyses conducted using alternate cutoff points yielded similar results, so they were not presented here. Percentage of racial/ethnic minority residents was obtained from LTCFocus files of corresponding years.
Analyses controlled for NH covariates from OSCAR for 2000 to 2010 that were commonly found to be associated with NH quality and QoL in the literature, including number of beds, chain affiliation (yes/no), profit status, occupancy rate, percentages of Medicare and Medicaid residents, and staffing per resident per day for certified nurse aides (CNAs), licensed practical nurses (LPNs), and RNs (Degenholtz, Kane, Kane, Bershadsky, & Kling, 2006; Degenholtz, Rosen, Castle, Mittal, & Liu, 2008; Harrington et al., 2002; Harrington et al., 2000; Hyer et al., 2011; Kane et al., 2004; Shippee, Henning-Smith, Kane, & Lewis, 2013; Shippee, Hong, Henning-Smith, & Kane, 2014). Analyses additionally controlled for NH covariates obtained from the LTCFocus files, including percent of female residents, average age of residents, and a case mix index calculated as the average of the acuity scores of all residents in an NH (higher score indicating higher average acuity). Analyses also controlled for market competition, which was derived using the Herfindahl–Hirschmann Index (HHI) and defined as the sum of squared shares of beds of all NHs in each county; market competition was then calculated as 1 − HHI, ranging from 0 (monopoly) to 1 (perfect competition). State Medicaid average per diem payment rate (a continuous variable) and whether the state implemented case mix adjustment (yes/no) in each year were also included in subsequent analyses.
Analyses
We performed bivariate analyses comparing NH and market covariates across percent minority concentration categories. For statistical inferences, we used analyses of variance for continuous variables to examine differences in means, and chi-square tests for categorical variables to examine differences in proportions.
Longitudinal multivariable Poisson regression with NH random effects was used to determine the association between NH racial/ethnic minority concentration in 2000 to 2010 and average number of QoL deficiencies in 2001 to 2011 at the NH level; we defined three dummy variables for NHs with medium, medium-high, and high minority concentrations, respectively, omitting low minority concentration NHs in the regression. Analysis controlled for year dummies, interactions between minority concentration groups and year dummies, NH and county characteristics described above, and state dummies. We calculated an adjusted disparity as Def × (IRR – 1), where Def is the mean number of QoL deficiencies for NHs with low concentrations of minority residents in the year, and IRR is the adjusted incidence rate ratio of each other concentration group estimated from the random-effects Poisson regression. Change in adjusted disparity was calculated as adjusted disparity of 2011 minus adjusted disparity of 2001.
In subsequent analysis, longitudinal multivariable Poisson regression with NH random effects was used to determine the effect of state NH payment policies on QoL deficiencies (main effects) and racial/ethnic disparities (effects of interactions) across NH minority concentration groups in QoL deficiencies. Analysis controlled for the NH, county, and state covariates described above, and additionally controlled for Medicaid payment rate and its interactions with minority concentration groups, and case mix payment and its interactions with minority concentration groups. We calculated the effect on deficiencies as Def × (IRR – 1), where Def is the mean number of QoL deficiencies of all NHs in the sample (for main effects) or NHs with low concentrations of minority residents (for interactive effects), and IRR is the adjusted IRR from the multivariable Poisson regression.
We chose random-effects (rather than fixed effects) Poisson regression models because our analyses were concerned with racial/ethnic disparities across NHs, as opposed to disparities within NHs, and because racial/ethnic minority concentration groups at the NH level were essentially time invariant during the study period.
Results
Descriptive statistics of free-standing NHs by concentration of racial/ethnic minority residents are provided in Table 1. Average concentration of racial/ethnic minority residents ranges from 1.4% in low concentration NHs to 55.7% in high concentration NHs, with variation increasing from low to high concentration NHs. NHs with high minority concentrations are larger and more likely to be for profit than those with low minority concentrations. High minority concentration NHs also have lower RN hours per resident day, compared with low minority concentration NHs. NHs with high minority concentrations also serve a smaller percentage of Medicare residents and a larger percentage of Medicaid residents than facilities with low minority concentrations.
Table 1.
Characteristics of Free-Standing NHs by Concentration of Racial/Ethnic Minority Residents, 2000 to 2010.
| Concentration of racial/ethnic minority residents in NHs |
||||
|---|---|---|---|---|
| Low (<5%) | Medium (5%-15%) | Medium-high (15%-35%) | High (≥35%) | |
| Number of observations (facility-years), number (%) | 67,530 (45.80%) | 32,450 (22.01%) | 25,506 (17.30%) | 21,949 (14.89%) |
| Concentration of minority residents, M ± SD, % | 1.36% ± 1.54% | 9.15% ± 2.87% | 23.43% ± 5.73% | 55.65% ± 15.71% |
| Number of beds, M ± SD | 97.99 ± 52.77 | 117.15 ± 63.72 | 123.63 ± 59.95 | 134.98 ± 74.25 |
| Chain affiliated, % | 53.81% | 59.52% | 61.67% | 58.76% |
| Profit status, % | ||||
| For-profit | 61.28% | 78.04% | 83.83% | 85.01% |
| Non-for-profit | 33.25% | 18.43% | 13.34% | 12.43% |
| Government | 5.48% | 3.53% | 2.84% | 2.56% |
| Occupancy rate, M ± SD, % | 86.22% ± 13.10% | 84.65% ± 13.80% | 84.26% ± 13.85% | 85.48% ± 12.35% |
| Nurse staffing (hours per resident day), M ± SD | ||||
| RN | 0.36 ± 0.27 | 0.30 ± 0.24 | 0.27 ± 0.27 | 0.26 ± 0.27 |
| LPN | 0.72 ± 0.40 | 0.78 ± 0.35 | 0.80 ± 0.32 | 0.81 ± 0.34 |
| Certified nursing assistant | 2.22 ± 0.85 | 2.14 ± 0.80 | 2.12 ± 0.77 | 2.12 ± 0.79 |
| Percentage of Medicare residents, M ± SD | 11.94% ± 10.77% | 13.15% ± 10.84% | 12.20% ± 10.06% | 10.64% ± 8.70% |
| Percentage of Medicaid residents, M ± SD | 56.81% ± 20.94% | 63.94% ± 18.57% | 70.14% ± 16.48% | 77.43% ± 14.88% |
| Case mix index, M ± SD | 0.79 ± 0.07 | 0.80 ± 0.08 | 0.79 ± 0.09 | 0.80 ± 0.10 |
| Percentage of female residents, M ± SD, % | 75.36% ± 9.11% | 72.88% ± 10.67% | 68.98% ± 11.90% | 62.15% ± 12.62% |
| Average age of residents, M ± SD | 83.70 ± 4.04 | 80.75 ± 5.89 | 78.13 ± 7.32 | 75.02 ± 8.37 |
| Market competition | 0.77 ± 0.23 | 0.82 ± 0.21 | 0.83 ± 0.22 | 0.85 ± 0.23 |
Note. p < .001 for comparisons of all characteristics across NH groups, based on analyses of variance for continuous variables and chi-square tests for categorical variables. NH = nursing home; RN = registered nurse; LPN = licensed practical nurse.
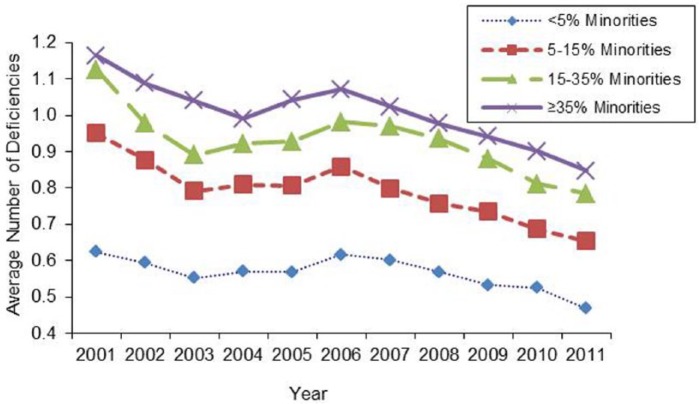
Figure 1 shows the longitudinal trend in QoL deficiencies by NH concentration of racial/ethnic minority residents. Although average number of QoL deficiencies across NH minority concentration groups is small, quality improvements can be observed. The difference between high minority concentration NHs and low minority concentration NHs is approximately 0.55 deficiencies in 2001; the difference between high minority concentration and low minority concentration NHs decreases to approximately 0.4 deficiencies by 2011, demonstrating a narrowing in the racial/ethnic disparity between high minority concentration and low minority concentration NHs, although this disparity still persists.
Figure 1.
Trend of quality of life deficiencies by nursing home concentration of racial/ethnic minority residents, 2001 to 2011.
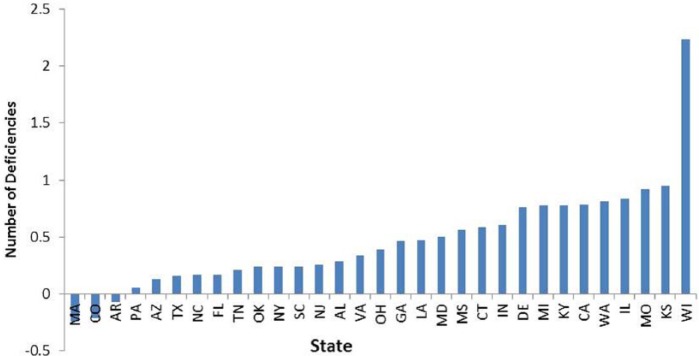
Unadjusted site-of-care disparities between NHs with high and low minority concentrations in average number of QoL deficiencies in 2011 and by state are shown in Figure 2. Site-of-care disparity is measured as the average number of QoL deficiencies in NHs with high minority concentrations minus the average number of QoL deficiencies with low minority concentrations in a given state. There is substantial variation in site-of-care disparities across states: site-of-care disparities in QoL deficiencies range from a high of about 2.2 deficiencies in Wisconsin, to a low of approximately 0 deficiencies in Arkansas and Pennsylvania.
Figure 2.
Site-of-care disparities between NHs with high concentrations of racial/ethnic minority residents (≥35%) and NHs with low minority concentrations (<5%) in average number of quality of life deficiencies, in 2011 and by state.
Note. States are not included here if, in 2011, they had less than five NHs in the group of low minority concentrations (Hawaii and New Mexico) or less than five NHs in the group of high minority concentrations (Alaska; Washington, D.C.; Iowa; Idaho; Maine; Minnesota; Montana; North Dakota; Nebraska; New Hampshire; Nevada; Oregon; Rhode Island; South Dakota; Utah; Vermont; West Virginia; and Wyoming). NH = nursing home.
Table 2 shows results of multivariable analyses of QoL deficiencies by concentration of racial/ethnic minority residents and year. The adjusted disparity between medium-high and low concentration NHs is 0.17 (p < .001) in 2001 and 0.05 (p < .01) in 2011, and the adjusted disparity decreases by 0.12 (p < .01) deficiencies over time. The adjusted disparity between high and low concentration NHs is 0.15 (p < .001) in 2001 and 0.03 (p > .05) in 2011, and the adjusted disparity also decreases by 0.12 (p < .01) deficiencies over time.
Table 2.
QoL Deficiencies by NH Concentration of Racial/Ethnic Minority Residents and Year.
| NH concentration of minority residents | 2001 |
2006 |
2011 |
Change in adj. disparitya | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadj. number | Unadj. disparity | Adj. disparityb | Unadj. number | Unadj. disparity | Adj. disparityb | Unadj. number | Unadj. disparity | Adj. disparityb | ||
| Low (<5%) | 0.62 | — | — | 0.62 | — | — | 0.47 | — | — | — |
| Medium (5%-15%) | 0.95 | 0.33 | 0.10*** | 0.86 | 0.24 | 0.05** | 0.65 | 0.18 | 0.04* | −0.06 |
| Medium-high (15%-35%) | 1.13 | 0.51 | 0.17*** | 0.98 | 0.36 | 0.06** | 0.79 | 0.32 | 0.05** | −0.12** |
| High (≥35%) | 1.16 | 0.52 | 0.15*** | 1.07 | 0.45 | 0.07** | 0.85 | 0.38 | 0.03 | −0.12** |
Note. Adj. = adjusted; Unadj. = unadjusted; IRR = incidence rate ratio; QoL = quality of life; NH = nursing home; RN = registered nurse; LPN = licensed practical nurse; CNA = certified nurse aide.
Adjusted disparity of 2011 – Adjusted disparity of 2001.
Calculated as Def × (IRR – 1), where Def is the mean number of QoL deficiencies for NHs with low concentrations of minority residents in the year, and IRR is the adjusted IRR of each other concentration group estimated from a multivariable random-effects Poisson regression that modeled deficiency number as a function of minority concentration groups, year dummies, their interactions, bed size, chain affiliation, non-profit ownership, government ownership, occupancy rate, staffing levels for RNs, LPNs, and CNAs, percentage of Medicare residents, percentage of Medicaid residents, case mix, percentage of female residents, average age of residents, market competition, and state dummies.
p < .05. **p < .01. ***p < .001.
Effects of state NH payment policies on QoL deficiencies and racial/ethnic disparities are shown in Table 3. Analyses found that higher Medicaid per diem payment rate (by every US$10) was associated with small, but statistically significant (p < .001), increases in number of QoL deficiencies. In contrast, case mix payment was associated with a 0.11 reduction in number of QoL deficiencies (p < .001), compared with non-case mix payment method. When looking at interactive effects, there is basically no difference in deficiencies between higher and low concentration NHs by payment rate. However, case mix payment may be associated with increased disparity between NHs with high and low racial/ethnic minority concentrations, as the number of deficiencies increased by 0.05 (p = .007).
Table 3.
Effect of State NH Payment Policies on QoL Deficiencies (Main Effects) and Racial/Ethnic Disparities (Effects of Interactions).a
| Medicaid payment or NH concentration of minorities | Adjusted IRRa | Effect on deficiencies or disparities |
|
|---|---|---|---|
| Effectb | p | ||
| Payment rate (in US$10) | 1.022 | 0.02 | .000 |
| Case mix payment | 0.848 | −0.11 | .000 |
| Payment rate (in US$10) × | |||
| Low (<5%) | — | — | — |
| Medium (5%-15%) | 0.992 | −0.01 | .047 |
| Medium-high (15%-35%) | 0.998 | −0.00 | .645 |
| High (≥35%) | 0.992 | −0.01 | .114 |
| Case mix payment × | |||
| Low (<5%) | — | — | — |
| Medium (5%-15%) | 0.995 | −0.00 | .834 |
| Medium-high (15%-35%) | 1.064 | 0.04 | .022 |
| High (≥35%) | 1.084 | 0.05 | .007 |
Note. IRR = incidence rate ratio; RN = registered nurse; LPA = licensed practical nurse; CNA = certified nurse aide; QoL = quality of life; NH = nursing home.
Multivariable longitudinal (2000-2010) random-effects Poisson regression modeled deficiency number as a function of minority concentration groups, year dummies, their interactions, Medicaid payment rate and its interactions with minority groups, case mix payment method and its interactions with minority groups, bed size, chain affiliation, non-profit ownership, government ownership, occupancy rate, staffing levels for RNs, LPNs, and CNAs, percentage of Medicare residents, percentage of Medicaid residents, case mix, percentage of female residents, average age of residents, market competition, and state dummies.
Calculated as Def × (IRR – 1), where Def is the mean number of QoL deficiencies of all NHs in the sample (for main effects) or NHs with low concentrations of minority residents (for interactive effects), and IRR is the adjusted IRR.
Discussion
Results demonstrate racial/ethnic disparities in NH QoL deficiencies nationally, which may have substantial implications for minority residents’ health and well-being. Similar to previous studies (Fennell et al., 2010; Mor et al., 2004; Smith et al., 2007, 2008), our analyses found that NHs with higher concentrations of racial/ethnic minority residents have structural characteristics that are likely to be associated with lower quality, including fewer RN hours per resident day and for-profit ownership, than NHs with the lowest concentration of racial/ethnic minority residents. Compared with non–minority-serving NHs, Medicaid pays for a larger proportion of residents in minority-serving NHs, and Medicare pays for a smaller proportion of residents. Improvements in overall quality were observed, as the average number of QoL deficiencies decreased across free-standing NHs, regardless of racial/ethnic minority concentration.
This study further shows that site-of-care disparities in QoL decreased over time, but persist in both crude and adjusted analyses, and there is substantial variation in site-of-care disparities across states. In addition, state NH payment policies intended to improve quality, such as case mix adjusted payments, may actually increase disparities between NHs with high and low minority concentrations.
Although NH quality has long been the focus of quality improvement initiatives and policies, residents’ QoL has gained less attention. Commonly examined NH quality measures, such as pressure ulcer rate and staffing intensity and mix, may not provide a complete representation of residents’ welfare and QoL. However, non-clinical aspects of NH performance, such as NH environment, programming, and resident autonomy, may be more indicative of experience with NH care from the perspective of residents and families (Campbell, Li, & Li, 2015). To our knowledge, no previous studies have examined racial/ethnic disparities in NH QoL, measuring QoL as the average number of QoL deficiencies. This study contributes to the nascent body of literature on racial/ethnic disparities in NH QoL, demonstrating site-of-care disparities in NHs both across and within states using recent longitudinal, national-level data.
Our longitudinal analysis demonstrated improvements in overall quality, measured by average number of QoL deficiencies, regardless of racial/ethnic minority concentration. Nevertheless, site-of-care disparities decreased but were not obviated after controlling for NH covariates and market competition, suggesting an area for improvement. Study findings indicate, however, that site-of-care disparities are a complex issue, and eliminating these disparities may require a multifaceted approach. For example, the difference in proportions of Medicaid and Medicare residents between minority-serving and majority-serving NHs suggests that minority-serving NHs may have greater financial resource constraints than non–minority-serving NHs. Also, variation across states suggests that additional state-level factors may contribute to site-of-care disparities.
In addition to examining NH and market factors, this study also considers the effects of state Medicaid payment policies, namely Medicaid payment rate and whether payment was case mix adjusted in each year. Medicaid payment rate is a key indicator of NH financial resource availability, and previous studies have found that Medicaid payment rate may be associated with higher staffing intensity and mix and improved resident outcomes (Feng et al., 2008; Grabowski et al., 2004; Harrington et al., 2007; Mor et al., 2011). Case mix reimbursement may have mixed effects on NH quality (Feng et al., 2008; Harrington et al., 2007); even so, it may improve access for higher acuity residents with Medicaid (Feng et al., 2006). Our results showed that Medicaid per diem payment rate was only minimally associated with QoL deficiencies, and that case mix adjustment was associated with improvements in QoL deficiencies. We further found that state case mix adjusted payment was associated with an increase in the disparity between high and low minority concentration NHs. These findings related to QoL deficiencies, together with findings of previous studies on clinical quality of care indicators, suggest the possibilities that although higher state NH payment rate may help improve NH quality of clinical and personal care (e.g., improved pressure ulcer rate and other clinical outcomes), higher payment rate may not help improve residents’ QoL in NHs. In addition, state Medicaid payment based on case mix adjustment may help reduce the number of QoL deficiencies for all NHs, but may also have an unintended effect that increases disparities in QoL deficiencies between majority-serving and minority-serving NHs.
Our results have substantial implications for current and future state NH policies. The proportions of Medicaid and Medicare residents in minority-serving NHs may limit financial resources in these facilities; subsequently, this may hinder minority-serving NHs’ ability to implement QoL improvement strategies or, under policies penalizing low-performing facilities, may further disadvantage patient populations in these NHs. However, increasing Medicaid payment rate on its own may not help improve residents’ QoL, and additional policies focusing on QoL may be necessary to augment NH QoL performance. Also, across-state variation in site-of-care disparities suggests that equity of NH care may be a more severe issue in some states, and state-level policies should be tailored to address disparities and to achieve better equity. Other NH payment policies not included in analyses, such as pay-for-performance programs, may also encourage further quality improvements, and more research is needed to identify effects these programs may have on site-of-care disparities. Future quality improvement strategies may need to target specific racial/ethnic minority groups, rather than implement interventions across all racial/ethnic groups, to encourage equitable QoL across NHs.
This study has several limitations. First, QoL was measured as the average number of QoL deficiencies in each year at the NH level, obtained from OSCAR data. Although the QoL section of the NH inspection covers multiple domains of resident life and care (Harrington et al., 2002; Harrington et al., 2000), examining QoL measured by resident and/or family reports may yield more direct measures from residents’ and families’ perspectives. Prior studies have examined resident and family reports in individual states (Campbell et al., 2015; Li et al., 2013), and have found racial/ethnic disparities in QoL (Li et al., 2014). Future studies could analyze multi-state trends in racial/ethnic disparities in QoL using data collected from NH residents or family members to better inform state policies. Second, our analyses focused on effects of state Medicaid NH payment policies due to their relevance to care delivery demonstrated in existing literature. Although the state dummies in multivariable analyses may help control for the effects of other unmeasured state factors, we acknowledge that these unmeasured state-level factors may confound results. Finally, this study uses the OSCAR and other administrative data, the limits of which are widely recognized. Reporting errors, particularly with respect to QoL deficiencies, may influence our results; however, it is unlikely that the key findings of this study would be invalidated.
In conclusion, our longitudinal analyses show improvements in NH QoL, measured by average number of QoL deficiencies. Site-of-care disparities improve over time, but do not disappear in multivariable analyses controlling for NH and market covariates. NH managers and state policy makers should be concerned by these disparities, and may consider quality initiatives targeting racial/ethnic minorities and/or low-performing facilities with higher percentages of racial/ethnic minority residents for improvement to achieve equity of QoL among NH residents.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Minority Health and Health Disparities of the National Institute of Health through Grant R01 MD007662.
References
- Cai S., Feng Z., Fennell M. L., Mor V. (2011). Despite small improvement, black nursing home residents remain less likely than whites to receive flu vaccine. Health Affairs (Millwood), 30, 1939-1946. doi: 10.1377/hlthaff.2011.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell L. J., Li Q., Li Y. (2015). Does nursing home ownership change affect family ratings on experience with care? Journal of Aging & Social Policy, 27, 314-330. doi: 10.1080/08959420.2015.1053739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenholtz H. B., Kane R. A., Kane R. L., Bershadsky B., Kling K. C. (2006). Predicting nursing facility residents’ quality of life using external indicators. Health Services Research, 41, 335-356. doi: 10.1111/j.1475-6773.2005.00494.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenholtz H. B., Rosen J., Castle N., Mittal V., Liu D. (2008). The association between changes in health status and nursing home resident quality of life. The Gerontologist, 48, 584-592. [DOI] [PubMed] [Google Scholar]
- Feng Z., Fennell M. L., Tyler D. A., Clark M., Mor V. (2011). The Care Span: Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Affairs (Millwood), 30, 1358-1365. doi: 10.1377/hlthaff.2011.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z., Grabowski D. C., Intrator O., Mor V. (2006). The effect of state medicaid case-mix payment on nursing home resident acuity. Health Services Research, 41 (4, Pt. 1), 1317-1336. doi: 10.1111/j.1475-6773.2006.00545.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z., Grabowski D. C., Intrator O., Zinn J., Mor V. (2008). Medicaid payment rates, case-mix reimbursement, and nursing home staffing—1996-2004. Medical Care, 46, 33-40. doi: 10.1097/MLR.0b013e3181484197 [DOI] [PubMed] [Google Scholar]
- Fennell M. L., Feng Z., Clark M. A., Mor V. (2010). Elderly Hispanics more likely to reside in poor-quality nursing homes. Health Affairs (Millwood), 29, 65-73. doi: 10.1377/hlthaff.2009.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski D. C., Angelelli J. J., Mor V. (2004). Medicaid payment and risk-adjusted nursing home quality measures. Health Affairs (Millwood), 23, 243-252. doi: 10.1377/hlthaff.23.5.243 [DOI] [PubMed] [Google Scholar]
- Harrington C., Carrillo H. (1999). The regulation and enforcement of federal nursing home standards, 1991-1997. Medical Care Research and Review, 56, 471-494. [DOI] [PubMed] [Google Scholar]
- Harrington C., Swan J. H., Carrillo H. (2007). Nurse staffing levels and Medicaid reimbursement rates in nursing facilities. Health Services Research, 42(3, Pt. 1), 1105-1129. doi: 10.1111/j.1475-6773.2006.00641.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington C., Woolhandler S., Mullan J., Carrillo H., Himmelstein D. U. (2002). Does investor-ownership of nursing homes compromise the quality of care? International Journal of Health Services, 32, 315-325. [DOI] [PubMed] [Google Scholar]
- Harrington C., Zimmerman D., Karon S. L., Robinson J., Beutel P. (2000). Nursing home staffing and its relationship to deficiencies. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 55, S278-S287. [DOI] [PubMed] [Google Scholar]
- Hyer K., Thomas K. S., Branch L. G., Harman J. S., Johnson C. E., Weech-Maldonado R. (2011). The influence of nurse staffing levels on quality of care in nursing homes. The Gerontologist, 51, 610-616. doi: 10.1093/geront/gnr050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane R. L., Bershadsky B., Kane R. A., Degenholtz H. H., Liu J. J., Giles K., Kling K. C. (2004). Using resident reports of quality of life to distinguish among nursing homes. The Gerontologist, 44, 624-632. [DOI] [PubMed] [Google Scholar]
- Kane R. L., Kane R. A. (2001). What older people want from long-term care, and how they can get it. Health Affairs (Millwood), 20, 114-127. [DOI] [PubMed] [Google Scholar]
- Li Y., Cai X. (2014). Racial and ethnic disparities in social engagement among US nursing home residents. Medical Care, 52, 314-321. doi: 10.1097/mlr.0000000000000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Cai X., Ye Z., Glance L. G., Harrington C., Mukamel D. B. (2013). Satisfaction with Massachusetts nursing home care was generally high during 2005-09, with some variability across facilities. Health Affairs (Millwood), 32, 1416-1425. doi: 10.1377/hlthaff.2012.1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Harrington C., Mukamel D. B., Cen X., Cai X., Temkin-Greener H. (2015). Nurse staffing hours at nursing homes with high concentrations of minority residents, 2001–11. Health Affairs, 34, 2129-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Harrington C., Temkin-Greener H., You K., Cai X., Cen X., Mukamel D. B. (2015). Deficiencies in care at nursing homes and racial/ethnic disparities across homes fell, 2006-11. Health Affairs (Millwood), 34, 1139-1146. doi: 10.1377/hlthaff.2015.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Ye Z., Glance L. G., Temkin-Greener H. (2014). Trends in family ratings of experience with care and racial disparities among Maryland nursing homes. Medical Care, 52, 641-648. doi: 10.1097/mlr.0000000000000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Yin J., Cai X., Temkin-Greener J., Mukamel D. B. (2011). Association of race and sites of care with pressure ulcers in high-risk nursing home residents. Journal of the American Medical Association, 306, 179-186. doi: 10.1001/jama.2011.942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LTCfocus. (2015). Retrieved from http://ltcfocus.org/1/about-us
- Mor V., Gruneir A., Feng Z., Grabowski D. C., Intrator O., Zinn J. (2011). The effect of state policies on nursing home resident outcomes. Journal of the American Geriatrics Society, 59, 3-9. doi: 10.1111/j.1532-5415.2010.03230.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V., Zinn J., Angelelli J., Teno J. M., Miller S. C. (2004). Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. The Milbank Quarterly, 82, 227-256. doi: 10.1111/j.0887-378X.2004.00309.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhard S. C. (2010). Diversion, transition programs target nursing homes’ status quo. Health Affairs (Millwood), 29, 44-48. doi: 10.1377/hlthaff.2009.0877 [DOI] [PubMed] [Google Scholar]
- Shippee T. P., Henning-Smith C., Kane R. L., Lewis T. (2013). Resident- and facility-level predictors of quality of life in long-term care. The Gerontologist, 55, 643-655. doi: 10.1093/geront/gnt148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee T. P., Hong H., Henning-Smith C., Kane R. L. (2015). Longitudinal changes in nursing home resident–reported quality of life: The role of facility characteristics. Research on Aging, 37, 555-580. doi: 10.1177/016402751454597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D. B., Feng Z., Fennell M. L., Zinn J. S., Mor V. (2007). Separate and unequal: Racial segregation and disparities in quality across U.S. nursing homes. Health Affairs (Millwood), 26, 1448-1458. doi: 10.1377/hlthaff.26.5.1448 [DOI] [PubMed] [Google Scholar]
- Smith D. B., Feng Z., Fennell M. L., Zinn J. S., Mor V. (2008). Racial disparities in access to long-term care: The illusive pursuit of equity. Journal of Health Politics, Policy and Law, 33, 861-881. doi: 10.1215/03616878-2008-022 [DOI] [PubMed] [Google Scholar]
- Zhang X., Grabowski D. C. (2004). Nursing home staffing and quality under the nursing home reform act. The Gerontologist, 44, 13-23. [DOI] [PubMed] [Google Scholar]