Abstract
Interrupted aortic arch is a rare congenital abnormality with a high infancy mortality rate. The principal finding is loss of luminal continuity between the ascending and descending portions of the aorta. Because of the high mortality rate in infancy, interrupted aortic arch is very rare among adults. In this report, we describe the case of a 76-year-old woman with asymptomatic interrupted aortic arch, severe tricuspid regurgitation, and bicuspid aortic valve. To our knowledge, she is the oldest patient ever reported with this possibly unique combination of pathologic conditions. In addition to reporting her case, we review the relevant medical literature.
Keywords: Adult; aorta, thoracic/abnormalities; aortic valve/abnormalities; arteriovenous malformations/diagnosis/surgery; heart defects, congenital; tricuspid valve/pathology; vascular malformations/physiopathology
Interrupted aortic arch (IAA) is a rare congenital abnormality (incidence rate, 3 per million live births per annum). Loss of luminal continuity between the ascending and descending portions of the aorta is the main pathologic condition.1 Some cardiac malformations—including patent ductus arteriosus, ventricular septal defect, bicuspid aortic valve (BAV), left ventricular (LV) outflow tract obstruction, and aortopulmonary window—have customarily been associated with IAA.2 On the basis of the site of the lesion, 3 types of disease have been reported. In type A, arch interruption occurs distal to the origin of the left subclavian artery (this is also known as interruption at the aortic isthmus). In type B, the lesion is distal to the origin of the left common carotid artery; and in type C, the interruption is between the common carotid arteries.3 Because of the high mortality rate—75% by 10 days and 90% at 12 months of life (without surgical correction in infancy)—IAA is very rare among adults.2,3 In this report, we describe the case of a 76-year-old woman with asymptomatic IAA, severe tricuspid regurgitation (TR), and BAV, a perhaps unique combination of pathologic conditions that no one, to our knowledge, has reported before.
Case Report
In August 2014, a 76-year-old woman was referred to our department for dyspnea on exertion (New York Heart Association functional class II), which had begun one month before referral. No other relevant information was found in her medical history. Upon physical examination, her peripheral pulses were palpable symmetrically, over the carotid arteries and in the upper limbs. We heard a machine-like murmur over the right scapula and a soft systolic murmur over the left sternal border space. Lower-limb pulses were not palpable. Chest radiographs revealed no pathologic abnormalities. An electrocardiogram showed sinus rhythm and right bundle branch block.
Transthoracic echocardiography revealed a normal LV ejection fraction (0.55), severe right ventricular dysfunction, BAV, mild aortic valve regurgitation, and severe tricuspid valve regurgitation (pulmonary artery pressure, 40 mmHg). Coronary angiography was performed via a right radial artery approach. The left anterior descending artery and the right coronary artery had significant stenoses. Aortography showed enlargement of the ascending aorta, BAV, normal aortic arch dimensions, and occlusion of the aorta immediately distal to the origin of the left subclavian artery (Fig. 1). Computed tomographic (CT) angiographic findings were compatible with a diagnosis of IAA (Fig. 2). After evaluation by our cardiovascular surgery service, open-heart surgical correction was recommended.
Fig. 1.

Aortogram shows a bicuspid aortic valve and no contrast medium passing through the descending aorta after aortic root injection.
Fig. 2.
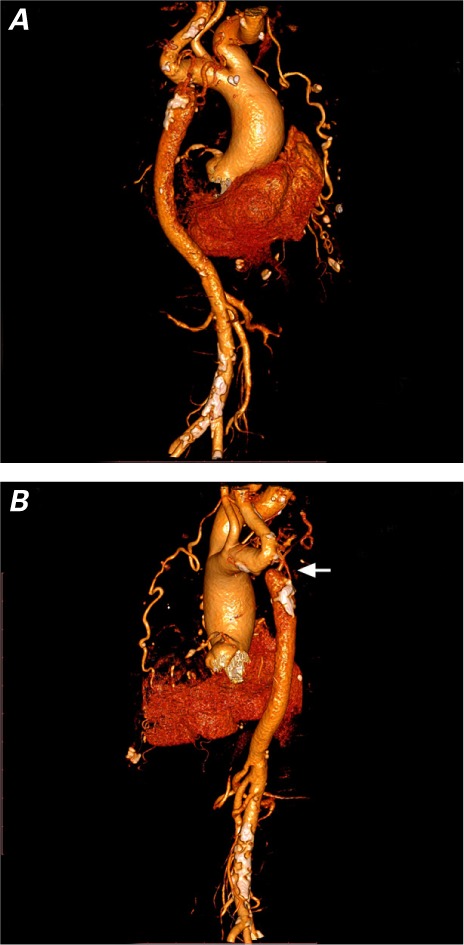
Computed tomographic angiograms (3-dimensional reconstruction) of the aorta show A) collateral circulation between the aortic arch and the descending aorta and B), in left posterior view, occlusion of the aorta (arrow) immediately distal to the left subclavian artery.
The patient underwent coronary artery surgery, bypass grafting of the ascending-to-descending aorta, and tricuspid valve repair. Postoperatively, she underwent a prolonged period of ventilator-dependent respiratory failure—complicated by a cerebrovascular accident that was manifested by left-sided hemiparesis and impaired speech and that was later confirmed by a spiral CT scan of the brain. She was later discharged to a rehabilitation facility. At the time of release from the hospital after one month, her ability to speak was unimpeded, she was able to do her work alone, and the forces exerted by her left hand and left foot were 4/5. Repeat transthoracic echocardiography, 2 months later, revealed a LV ejection fraction of about 0.55, BAV, mild aortic valve regurgitation, and mild-to-moderate TR (pulmonary artery pressure, 40 mmHg). The patient eventually died of postoperative sequelae (sepsis and tracheal stenosis).
Discussion
Severe congestive heart failure is the major presentation of IAA in infants. If the condition is left untreated, 90% of the affected infants die in the first year of life.4,5 The presence of collateral circulation is the only means of survival (Fig. 2A). The initial defect, one supposes, is coarctation of the aorta, which progresses to complete obstruction of the lumen (especially when the interruption is at the aortic isthmus).6 In adults, the clinical presentation of IAA varies from absence of symptoms to headache, malaise, hypertension, claudication, differential blood pressure between the arms and legs, limb swelling, and congestive heart failure. Examination of the upper and lower peripheral pulses plays a pivotal role in the diagnosis of IAA and coarctation of the aorta in young adults whose chief complaint is hypertension. Although echocardiography has some limitations in evaluating the aortic arch and the descending aorta, it is the technique of choice for detecting concomitant cardiac abnormalities. In addition, CT and magnetic resonance imaging are useful as combined diagnostic imaging methods for IAA.7
Our patient was diagnosed with IAA type A, severe TR, and BAV at 76 years of age, which makes her the oldest reported patient with IAA at the time of this writing. Despite the abundance of combined cardiac anomalies, to our knowledge and after a thorough search of the literature, we could not find any report of tricuspid valve involvement with IAA.
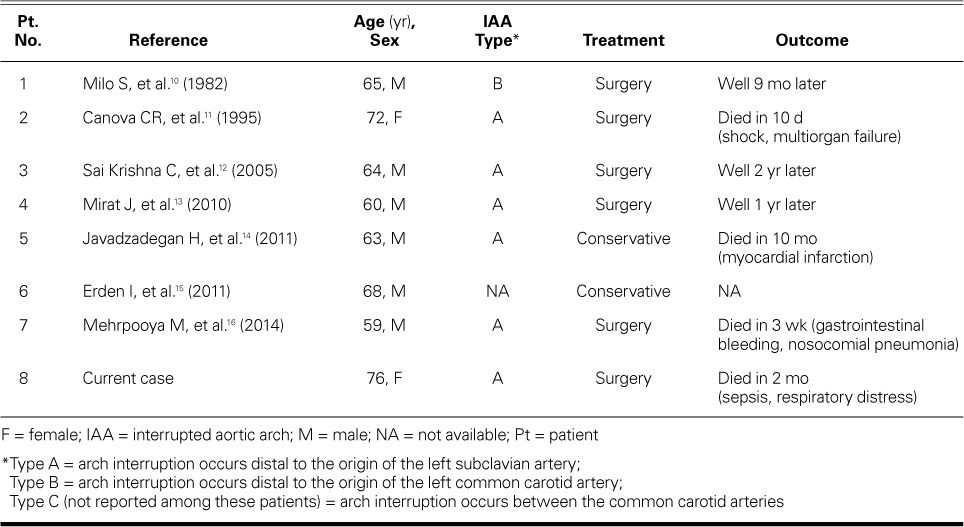
According to the literature, the preferred treatment for IAA is surgical correction.2 Surgical repair can be performed by extra-anatomic bypass, interposition of a tube graft, or end-to-end anastomosis, depending upon the anatomy and the location of the aortic interruption. The most frequently described surgical approach in adults is extra-anatomic, in preparation for a single-stage repair.8,9 A thorough search of the published literature showed few IAA patients over 60 years of age (Table I10–16). In one report, a 59-year-old man with severe aortic valve stenosis and IAA underwent surgical correction. After 3 weeks, he died of gastrointestinal bleeding and nosocomial pneumonia.16 In another report, a 72-year-old woman developed pericardial tamponade after a successful repair, and died of shock and multiorgan failure.11 A 63-year-old patient with IAA was a candidate for cardiothoracic surgery but refused it and was treated conservatively. After 10 months of monitoring, he died at home of myocardial infarction.14 A 60-year-old man with IAA underwent surgical correction. At the 1-year follow-up, he had no complication.13 Our patient underwent coronary artery and ascending-to-descending aorta bypass grafting, along with sealed Dacron surgery and tricuspid valve repair. After the surgery, she had a cerebrovascular accident and finally died of tracheal stenosis and sepsis. Because of the small number of cases, the higher incidence of surgical sequelae in older patients, and the widely varied results of both surgical and conservative treatments, it is difficult to decide on the best approach. Nevertheless, we suggest that conservative management might be beneficial in asymptomatic older adults.
TABLE I.
Reports of IAA in Patients ≥59 Years Old
Footnotes
From: Tehran Heart Center (Drs. Baradaran, Forouzannia, Kassaian, Sardari, and Tajdini) and School of Medicine (Dr. Hosseini), Tehran University of Medical Sciences, Tehran 1411713138, Iran
Dr. Hosseini is now at Massachusetts General Hospital, Boston, Massachusetts.
References
- 1.Bugan B, Iyisoy A, Celik M, Kucuk U, Boz U, Celik T. Isolated type A interrupted aortic arch in an asymptomatic 19-year-old man. Tex Heart Inst J. 2011;38(5):559–61. [PMC free article] [PubMed] [Google Scholar]
- 2.Ponte M, Dias A, Dias Ferreira N, Fonseca C, Mota JC, Gama V. Interrupted aortic arch: a misdiagnosed cause of hypertension. Rev Port Cardiol. 2014;33(6):389.e1–5. doi: 10.1016/j.repc.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Hokenek F, Sever K, Ugurlucan M, Sakliyan M, Kinoglu B. Interrupted aortic arch in adulthood. Thorac Cardiovasc Surg. 2008;56(3):140–2. doi: 10.1055/s-2007-965644. [DOI] [PubMed] [Google Scholar]
- 4.Messner G, Reul GJ, Flamm SD, Gregoric ID, Opfermann UT. Interrupted aortic arch in an adult: single-stage extra-anatomic repair. Tex Heart Inst J. 2002;29(2):118–21. [PMC free article] [PubMed] [Google Scholar]
- 5.Collins-Nakai RL, Dick M, Parisi-Buckley L, Fyler DC, Castaneda AR. Interrupted aortic arch in infancy. J Pediatr. 1976;88(6):959–62. doi: 10.1016/s0022-3476(76)81049-9. [DOI] [PubMed] [Google Scholar]
- 6.Lobato RF, Saliba LA, Ferreiro CR, Bacal F. Interrupted aortic arch with cardiac heart failure in young adult. Arq Bras Cardiol. 2008;91(1):e4–6. doi: 10.1590/s0066-782x2008001300012. [DOI] [PubMed] [Google Scholar]
- 7.Reardon MJ, Hallman GL, Cooley DA. Interrupted aortic arch: brief review and summary of an eighteen-year experience. Tex Heart Inst J. 1984;11(3):250–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Ozdogru I, Gunebakmaz O, Kaya MG, Dogan A. A case of aortic coarctation mimicking interrupted aorta [in Turkish] Turk Kardiyol Dern Ars. 2009;37(2):141–4. [PubMed] [Google Scholar]
- 9.Akdemir R, Ozhan H, Erbilen E, Yazici M, Gunduz H, Uyan C. Isolated interrupted aortic arch: a case report and review of the literature. Int J Cardiovasc Imaging. 2004;20(5):389–92. doi: 10.1023/b:caim.0000041940.14780.1c. [DOI] [PubMed] [Google Scholar]
- 10.Milo S, Massini C, Goor DA. Isolated atresia of the aortic arch in a 65-year-old man. Surgical treatment and review of published reports. Br Heart J. 1982;47(3):294–7. doi: 10.1136/hrt.47.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canova CR, Carrel T, Dubach P, Turina M, Reinhart WH. Interrupted aortic arch: fortuitous diagnosis in a 72-year-old female patient with severe aortic insufficiency [in German] Schweiz Med Wochenschr. 1995;125(1–2):26–30. [PubMed] [Google Scholar]
- 12.Sai Krishna C, Bhan A, Sharma S, Kiran U, Venugopal P. Interruption of aortic arch in adults: surgical experience with extra-anatomic bypass. Tex Heart Inst J. 2005;32(2):147–50. [PMC free article] [PubMed] [Google Scholar]
- 13.Mirat J, Galic E, Coric V, Rajsman G, Vrbanic L, Razov Radas M et al. Secondary hypertension due to isolated interrupted aortic arch in a 60-year-old person--one-year follow up. Coll Antropol. 2010;34(Suppl 1):307–9. [PubMed] [Google Scholar]
- 14.Javadzadegan H, Porhomayon J, Sadighi A, Yavarikia M, Nader N. Isolated interrupted aortic arch: unexpected diagnosis in a 63-year-old male. Case Rep Crit Care. 2011;2011:989621. doi: 10.1155/2011/989621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erden I, Kayapinar O, Erden EC, Yalcin S. Silent interrupted aortic arch in an elderly patient. Cardiol J. 2011;18(6):695–7. doi: 10.5603/cj.2011.0036. [DOI] [PubMed] [Google Scholar]
- 16.Mehrpooya M, Eskandari R, Salehi M, Shajirat Z, Golabchi A, Satarzadeh R, Zand-Parsa AF. Undiagnosed interrupted aortic arch in a 59-year-old male patient with severe aortic valve stenosis: a case report and literature review. ARYA Atheroscler. 2014;10(4):230–2. [PMC free article] [PubMed] [Google Scholar]


