Abstract
This review reports the current situation with respect to therapeutic options (lifestyle and drugs) reducing the concentrations of atherogenic low-density lipoprotein cholesterol (LDL-C) and lipoprotein(a) (Lp[a]). Three lipoprotein apheresis (LA) principles have been realized: precipitation, filtration, and adsorption. Available LA methods are herein described in detail – major components, pumps, extracorporeal volume, treated volume, and anticoagulation. General features of all LA methods as well as pleotropic effects are elaborated. Indications for LA therapy are quoted: homozygous familial hypercholesterolemia (HCH), severe HCH, and isolated elevation of Lp(a) and progress of atherosclerotic disease. A major focus is on the evidence of the effect of LA on cardiovascular outcome data, and the most important publications are cited in this context. The best studies have been performed in patients with elevated Lp(a) in whom cardiovascular events were reduced by more than 80%. Major adverse effects and contraindications are listed. The impact of an LA therapy on patient quality of life and the requirements they have to fulfill are also highlighted. Finally, the future role of LA in treating high-risk patients with high LDL-C and/or high Lp(a) is discussed. It is probable that the significance of LA for treating patients with elevated LDL-C will decrease (with the exception of homozygous familial HCH) due to the application of PCSK9 inhibitors. The antisense oligonucleotide against apolipoprotein(a) could replace LA in patients with high Lp(a), provided positive outcome data are generated.
Keywords: LDL cholesterol, lipoprotein(a), lipid-lowering therapy, lipoprotein apheresis, cardiovascular outcome
Video abstract
Introduction to current management strategies for patients with severe hypercholesterolemia and elevated lipoprotein(a)
Severe hypercholesterolemia (HCH) and elevation of lipoprotein(a) (Lp[a]) are serious risk factors inducing the development of atherosclerotic lesions leading to cardiovascular events such as myocardial infarction or stroke.1,2 Both metabolic abnormalities are primarily genetically based, which is reflected in their occurrence in close relatives (parents, children).
Lifestyle changes are always necessary. It must be admitted, however, that the effect of an optimal diet on low-density lipoprotein cholesterol (LDL-C) levels in severe HCH is rather limited (a 5% reduction is realistic with almost no reduction in patients with homozygous familiar HCH), and no effect of diet on Lp(a) concentrations has been observed. Physical activity does not exert an action on either parameter. Nonsmoking is of great relevance – the combination of the discussed metabolic disturbances and cigarette smoking is highly atherogenic.
In patients who have already developed atherosclerotic lesions (either documented by imaging techniques or having suffered from cardiovascular events), drug therapy is required.1 In HCH patients, the drugs of first choice are statins. Usually, one starts with a low dose and – when this is tolerated, but the effect is not sufficient – the physician then prescribes a higher dose (Figure 1A). Statins differ with respect to their effectiveness: atorvastatin and rosuvastatin are more potent. According to European Guidelines, an LDL-C target should be aimed for. In patients with proven atherosclerosis, LDL-C should be lowered to <1.8 mmol/L. If this target cannot be reached, either ezetimibe or a bile-acid sequestrant (or both) should be added to the statin. For high-risk patients whose LDL-C levels remain very far from the target despite the proposed drug treatment (or in patients with an intolerance to statins or the other suggested drugs),3 a new option is available: PCSK9 inhibitors.4 These can also be combined with a statin and help, in many patients, to lower LDL-C very effectively. The antisense oligonucleotide mipomersen represents an alternative therapeutic approach but is associated with a rather high rate of adverse effects and is only approved for use in the USA (not in Europe). In patients with homozygous familial HCH, the MTP inhibitor, lomitapide can be administered – usually in addition to a lipoprotein apheresis (LA) treatment. In these patients, PCSK9 inhibitors either show a limited effect on LDL-C levels or no effect (depending on the residual function of the LDL receptors).
Figure 1.
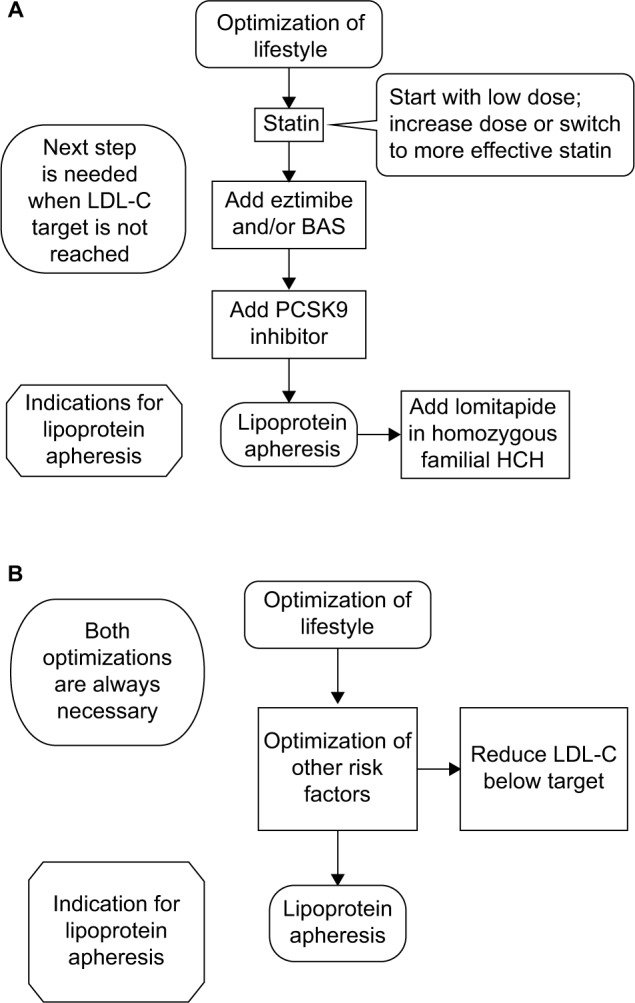
Therapeutic steps in treating patients with (A) high LDL-C or (B) high Lp(a).
Abbreviations: BAS, bile-acid sequestrant; HCH, hypercholesterolemia; Lp(a), lipoprotein(a); LDL-C, low-density lipoprotein cholesterol.
The next step is undertaken after at least a 3-month period in which the efficiency of the ongoing drug therapy is determined. PCSK9 inhibitors are prescribed only after 1 year of application of other lipid-lowering drugs (when the latter are tolerated).
The situation with respect to Lp(a) is quite different (Figure 1B). Statins do not affect Lp(a) concentrations (some studies have even shown an increase); other lipid-lowering drugs are also ineffective. The general policy for treating patients with high Lp(a) is to optimize other risk factors such as LDL-C (as already mentioned), diabetes, hypertension, and lifestyle.
PCSK9 inhibitors reduce Lp(a) levels up to 30%; however, in patients with very high Lp(a) concentrations, this effect is much less or even absent. An elevation of Lp(a) represents no indication for the administration of PCSK9 inhibitors, but these drugs could be used in patients with a parallel elevation of LDL-C. Mipomersen reduces Lp(a) as well.
In several large placebo-controlled studies, statins have been shown to effectively reduce the morbidity and mortality of cardiovascular diseases, reducing new events by 30%–40%. However, there remain patients who develop new events despite taking a statin. One possible reason for this could be that in many patients LDL-C target levels have not been reached. It is quite well accepted that the incidence of new events will be lower when LDL-C levels are lower. Ezetimibe added to a statin led to a further reduction in new events.5 No data with respect to the occurrence of cardiovascular events have been published for bile-acid sequestrants. For PCSK9 inhibitors, preliminary results point to their effectiveness in this respect, but the first controlled long-term study performed in more than 20,000 patients will only conclude in 2016.
At present, no effective drug therapy is available for Lp(a) – nicotinic acid was withdrawn from the market in Europe after two studies showed no positive effect on cardiovascular events and a rather high rate of adverse events (AEs).6 In one study, a new antisense oligonucleotide against apolipoprotein(a) has been shown to decrease Lp(a) very effectively.7
Review of clinical utility, recommendations, patient selection, and implementation of LA
The position of LA within the therapeutic regimen of lipid disorders is always at the end (Figure 1). Only high-risk patients are considered candidates for this extracorporeal treatment. LA does not play a major role in primary prevention, with the exception of homozygous familial HCH (when patients are at an extremely high risk to develop atherosclerosis).
In 1967, de Gennes et al8 performed plasmapheresis (discontinuous flow) to treat patients with homozygous familial HCH. In the 1970s and 1980s, several more specific LA methods were developed, first in Japan and then in Germany. The major aim of all available LA methods is to eliminate atherogenic LDL and Lp(a) particles from the blood, but other lipoproteins such as very LDL and high-density lipoprotein (HDL) are also being removed.
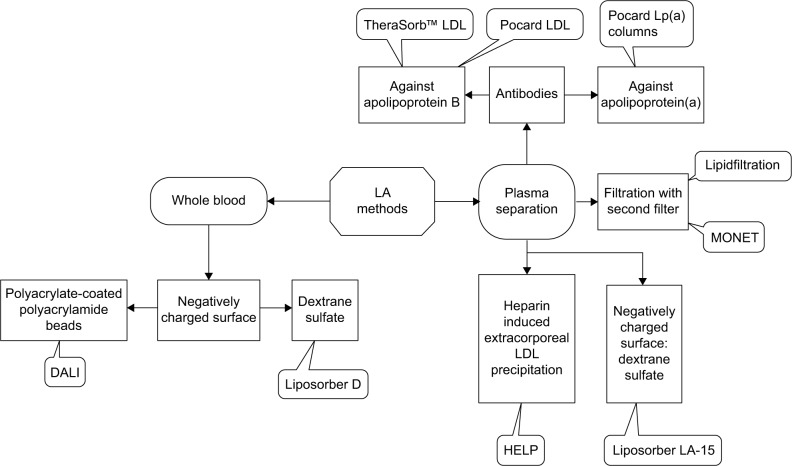
Some LA methods eliminate the lipoproteins from plasma – the first step is the separation of plasma either by filtration or by centrifugation. Other methods use whole blood (Figure 2).
Figure 2.
Principles of available LA methods.
Abbreviations: HELP, heparin-induced extracorporeal LDL precipitation; LA, lipoprotein apheresis; LDL, low-density lipoprotein; Lp(a), lipoprotein(a); DALI, direct adsorption of lipoproteins; MONET, membrane filtration optimized novel extracorporeal treatment.
After plasma separation, there are different techniques that can be used to remove atherogenic lipoproteins (names of the LA systems given; Figure 2 and Table 1):
Second filter that retains the lipoproteins (and also other proteins): Lipidfiltration and membrane filtration optimized novel extracorporeal treatment (MONET).
Addition of a large amount of heparin and an acetate buffer – at pH 5.12, lipoproteins are precipitated (and also fibrinogen); the excess of heparin is then removed by a heparin adsorber, and the pH is normalized by a bicarbonate dialysis: heparin-induced extracorporeal LDL precipitation (HELP).
Antibodies against apolipoprotein B (apoB) that are bound to sepharose; each patient has his/her own two columns that are at first loaded with plasma (the plasma is guided to the second column, while the first column is regenerated; both columns are loaded and regenerated alternatively); the regeneration starts: a glycine buffer separates the antigen from the antibodies, the antigen is washed out by a fluid, and the pH is normalized using a phosphate buffer: TheraSorb™ LDL; here the plasma separation is performed by centrifugation. This system allows single-needle handling. The Pocard LDL columns use the same principle.
Dextran sulfate bound to cellulose with a negatively charged surface binding apoB containing lipoproteins: Liposorber LA-15.
Table 1.
Overview of LA methods
| Volumes | Details | Precipitation | Adsorption | Filtration | |||||
|---|---|---|---|---|---|---|---|---|---|
| LA method | HELP | TheraSorb™ LDL | Pocard columns | DALI | Liposorber D | Liposorber LA-15 | Lipidfiltration | MONET | |
| Manufacturer | B Brauna | Miltenyib | Pocardc | Freseniusd | Kanekae | Kanekae | Diamedf | Freseniusd | |
| Machine | Plasmat Futura | Life 18/Life 21 | no | Art Universal | DX 21/MA-03 | MA-03 | Octo Nova | Art Universal | |
| Components | Plasma filter, precipitation filter, heparin adsorber, ultrafiltration filter | Disk separator; two columns with sepharose coated with antibodies | 1 or 2 columns with sepharose coated with antibodies, specific for Lp(a) or LDL | One or two columns with beads (500, 750, 1,000 [2×500], 1,250 [500+750]) | One or two columns (DL 75 or DL 100 [2×500]) | Plasma filter, two adsorber columns | Plasma filter, lipoprotein filter | Plasma filter, lipoprotein filter | |
| Pumps | Blood, ultrafiltration, plasma/buffer, dialysate | 18 pumpsg | Blood, plasma, regeneration solutions | Blood, citrate | Blood, citrate | Blood, plasma, regeneration fluid | Blood, plasma, citrate, retinate | Blood, plasma, citrate, flushing fluid | |
| Treated volume | Whole blood | Approximately 9,000 mL | Approximately 8,000 mL | ||||||
| Plasma | Up to 4,000 mL | Approximately 4,500 mL | Lipopak 400 Lp(a): about 6,000 ml LDL: up to 4,500 ml |
1.5 to 1.8 times the individual plasma volume | Approximately 4,000 mL | Approximately 4,000 mL | |||
| Extra-corporeal volumeh | Blood | 188 mL | 80 mL | Depending on the plasma separator | DALI 500: 330 mL; DALI 750: 430 mL; DALI 1,000: 580 mL; DALI 1,250: 680 mL | DL-75: 494 mL; DL-100: 696 mL | 130/160/185 mLi | 215 mL | 164 mL |
| Plasma | 400 mL | 310 mL | With AdaSorb Lipopak 200: 240 ml Lipopak 400: 350 ml |
221/261/291 mLi | 360 mL | 662 mL | |||
| Anticoagulationj | Heparin | Heparin, citratek | Heparin, citrate | Heparin (some patients), citrate | Heparin, citrate | Heparin | Heparin, citrate | Heparin, citrate | |
Notes:
B Braun Avitum AG, Melsungen, Germany.
Miltenyi Biotec GmbH, Bergisch-Gladbach, Germany.
Pocard Ltd., Moscow, Russia.
Fresenius Medical Care GmbH, Bad Homburg, Germany.
Kaneka Corporation, Japan.
DIAMED Medizintechnik GmbH, Cologne, Germany.
Functions of pumps: 2× NaCl to adsorbers/PBS-Azide to adsorbers; 2× PBS to adsorbers; 2× Gly-HCl to adsorbers; 2× plasma to adsorbers; 2× plasma from adsorber to blood cell concentrate; 2× fluid from adsorber to waste; plasma from disk separator to blood cell concentrate (adsorber bypass) and treated plasma of the adsorber to be loaded in the adsorber exchange step; whole blood from blood return line to patient; anticoagulant from bag to blood withdrawal line; whole blood from blood withdrawal line to separator; 2× for single needle use.
According to information obtained from the manufacturers.
Depending on the used plasma separator (OP-02/OP-05/OP-08).
Given to the patients.
TheraSorb™ LDL anticoagulation can be realized without heparin. Adapted from Clin Lipidol. 2013;8(6):693–705 with permission of Future Medicine Ltd.46
Abbreviations: HELP, heparin-induced extracorporeal LDL precipitation; DALI, direct adsorption of lipoproteins; LA, lipoprotein apheresis; LDL, low-density lipoprotein; MONET, membrane filtration optimized novel extracorporeal treatment; PBS, phosphate buffer solution.
There are two whole blood LA methods on the market (names of the systems given):
Polyacrylate-coated polyacrylamide beads with a negatively charged surface binding apoB containing lipoproteins: direct adsorption of lipoproteins (DALI).
Dextran sulfate bound to cellulose with a negatively charged surface binding apoB containing lipoproteins: Liposorber D.
The following issues apply to all LA methods:
Blood is usually obtained by venous puncture and returned via a vein at the contralateral arm. When the venous situation in a given patient is very poor, an arteriovenous fistula has to be established.
Part of the blood is extracorporeal during the session.
Duration of an LA session is between 1.5 and 4 hours depending on the method used, the treated volume, and the blood flow. Usually, the blood flow during the session is between 80 and 120 mL/min.
Anticoagulation is always needed, either with heparin or with citrate (or both; Table 1).
Plasma or blood volume to be treated during a session has to be individualized (taking into account venous access, tolerability, duration of session, and reduction rate of LDL-C and of Lp[a]). Volumes in Table 1 are those mostly reached at the Dresden Center for extracorporeal therapy (for Liposorber LA-15 and the Pocard columns data have been provided by the companies).
All offered systems are one-way systems. Only the columns of TheraSorb™ LDL and the Pocard LDL columns can be used several times for a given patient.
Blood cells are returned to the patient undamaged. For complete return, the systems are rinsed with saline at the end of the session. Thus, a certain part of the acute reduction in LDL-C and Lp(a) is due to dilution of the plasma – this effect can be checked for by simultaneous measurement of the hematocrit and a corresponding correction; in the daily routine, this is not done because the dilution effect is very small.
Following the acute reduction in LDL-C and Lp(a) after an LA session, both parameters increase in the following days. Thus, the usual recommendation is to treat patients weekly.
Additionally available methods are as follows: 1) Pocard Lp(a) columns – plasma separation by centrifugation and polyclonal monospecific antibodies against human Lp(a) bound to sepharose (POCARD Ltd., Moscow, Russia);9 and 2) Lipocollect 200/300 – cell separator and polyanionic porous silica particles (medicollect eK, Rimbach, Germany).10
All LA methods acutely reduce LDL-C and Lp(a) by more than 60%. The only exception is the Russian Lp(a) columns, which decrease only Lp(a) concentrations.
In addition to its effect on lipoproteins, LA also exerts so-called pleotropic effects.11–18 The following are most relevant:
A decrease in fibrinogen and other coagulatory and fibrinolytic markers; improvement in the rheological properties of the blood.
A decrease in C-reactive protein and other inflammatory markers.
A decrease in oxidized LDL particles.
A reduction in the expression of the proatherosclerotic oxLDL receptor LOX-1 and adhesion molecule VCAM-1 and an increase in the expression of vasoprotective and nitric oxide generating endothelial nitric oxide synthase in human endothelial cells in response to serum of hypercholesterolemic patients.
A reduction in the activity of oxidized phospholipids and lipoprotein-associated phospholipase A2, which are bound to Lp(a).
A decrease in serum PCSK9 levels.
An improvement of coronary blood flow.
An improvement of retinal blood flow.
These and other effects may have a positive effect on the development of atherosclerotic lesions, blood flow in organs, and vasoreactivity. The significance of these experimental findings for the clinical outcome of the apheresis patients remains to be determined. No long-term study has been performed to compare the outcome data for different LA methods, which clearly differ with respect to their pleotropic actions.
In Germany, the Gemeinsamer Bundesausschuss (Federal Joint Committee) decides on the acceptance of new therapeutic approaches.
Homozygous familial HCH
Homozygous familial HCH has also been accepted as an indication in other countries. The extracorporeal therapy should be started in childhood, at the age of approximately 5 years. Survival of these patients can be guaranteed (Table 2).
Table 2.
Accepted indications for LA in Germany
| 1. | Homozygous familial HCH. |
| 2. | Severe HCH, if the maximal documented diet and drug therapy for more than 1 year failed to lower low-density lipoprotein cholesterol (LDL-C) sufficiently. |
| 3. | Elevation of lipoprotein(a) (Lp[a]) levels ≥600 mg/L (≥120 nmol/L), normal LDL-C, and (clinically or by an imaging technique) documented progressive cardiovascular disease. |
In 2014 in Germany, 120 patients with this disorder were treated using LA.19
Severe HCH, if the maximal documented diet and drug therapy for more than 1 year failed to lower LDL-C sufficiently
The definition of “severe HCH” is not clear. Thus, usually, internationally accepted target levels for LDL-C are used (Introduction). It has been stressed that a maximal drug therapy, when tolerated, be performed for at least 1 year. For this indication, only patients who suffered from at least one severe atherosclerotic event, eg, myocardial infarction, are eligible. The general risk situation has to be taken into account: many patients have other risk factors such as hypertension, diabetes, and a family history of early cardiovascular events in first-degree relatives (Table 2).
The Federal Joint Committee decided that the minimal acute reduction in LDL-C by an LA session should amount to more than 60%.
Elevation of Lp(a) levels ≥600 mg/L (≥120 nmol/L), normal LDL-C, and (clinically or by an imaging technique) documented progressive cardiovascular disease
Here, the Federal Joint Committee defined a limit for Lp(a) to be ≥600 mg/L. A German group of LA specialists translated this limit into another dimension as ≥120 nmol/L. The latter result was obtained with newer measurement methods. Unfortunately, it is not possible to convert data obtained in one unit into the other one. However, in my experience, when both measurement systems in a group of patients were used in parallel, all patients with high Lp(a) values remained in this group with both methods. It has to be taken into consideration that the atherosclerotic risk associated with Lp(a) starts at levels exceeding 300 mg/L. No minimal acute reduction rate for Lp(a) has been officially established (Table 2).
The other precondition is that a progress of atherosclerosis has to have been documented either clinically (eg, several stenting procedures) or by an imaging technique (eg, new plaques at the carotids). But with regard to a 28-year-old male who suffered from a severe myocardial infarction and had extremely high Lp(a) levels, we decided not to wait for a second (possibly deadly) myocardial infarction and started LA therapy.
The HEART-UK criteria for the use of LA includes patients with progressive coronary artery disease, HCH, and Lp(a)>60 mg/dL in whom LDL-C remains elevated despite drug therapy.20 Several patients with elevated LDL-C concentrations simultaneously show elevated triglyceride (TG) concentrations. LA also effectively lowers TG, but hypertriglyceridemia is not officially recognized as an indication for LA. Taking into account the high frequency of mixed hyperlipidemia, we suggest calculating non-HDL-C to demonstrate the effectiveness of an LA session in these patients.21 Non-HDL-C is an internationally accepted indicator for atherosclerotic risk.
In patients with chylomicronemia syndrome, the common LA methods are not effective due to problems with the flow in the machine. This is the only remaining indication to perform a plasma exchange when the patient develops an acute pancreatitis. In these patients, one or two sessions are sufficient.
In some countries, patients with lipid disorders are still chronically being treated with plasma exchange. Because of the expressed loss of proteins and the high rate of adverse effects, this procedure is no longer recommended.
In Germany, all applications for LA treatment must be submitted to a specialized committee that works at the Associations of Statutory Health Care Physicians. The approval by this committee is based on accompanying lipidologic and cardiologic/angiologic evaluations and is required for reimbursement of LA by the health insurance companies. The Federal Joint Committee decided that only nephrologists can apply for permission to perform LA therapy. Physicians who think that their patients may benefit from LA treatment should send them to either a lipidologic center (where lipidologists give an advice for the best treatment for the patient) or directly to the nephrologist who has obtained permission.
In the past years, the number of LA centers, physicians, and patients has increased steadily in Germany (Table 3). Based on my own experience, the number of patients with high Lp(a) is especially growing because of a higher awareness of this atherogenic risk factor and the lack of therapeutic alternatives.
Table 3.
LA centers, physicians, and patients in Germany in 2013–2015
An LA registry had been started in Germany in 2011.22,23 As far as the author knows, LA is also performed in the USA, Canada, Great Britain, France, Italy, Russia, Czechia, Spain, and Japan. In other countries (such as the Netherlands, Sweden, or Denmark), only single patients are being treated.
Since 1992, the National Health Insurance Program (NHIP) in Japan has approved LA therapy (ten treatments over 3 months) for nonsurgical candidate patients with peripheral arterial disease (Fontaine classification>II) who have an LDL-C above 3.6 mmol/L.24 Also since 1992, the NHIP in Japan has approved LA therapy, specifically the Liposorber LA-15 System (12 treatments over a 12-week period), for nephritic syndrome patients with a total cholesterol >6.5 mmol/L who have been resistant to conventional therapy.25 In 2013, the US Food and Drug Administration (FDA) approved LA therapy for the new-onset focal segmental glomerulosclerosis in pre- or post-renal transplant pediatric patients who have been resistant to standard treatment options and who have a glomerular filtration rate >60 mL/min/1.73 m2.11
LA has been used to treat patients with a variety of other diseases: cerebrovascular disease, post-cardiac transplant, acute coronary syndrome, diabetic ischemic foot, ocular microcirculatory disturbances, preeclampsia, sudden idiopathic hearing loss, and age-related macular degeneration, although none of these disorders has been officially accepted as an indication for LA. The main mechanism explaining the effects of LA in these situations is probably its influence on lipids and on rheological properties of the blood.
Efficacy studies including any relevant case studies and ongoing studies
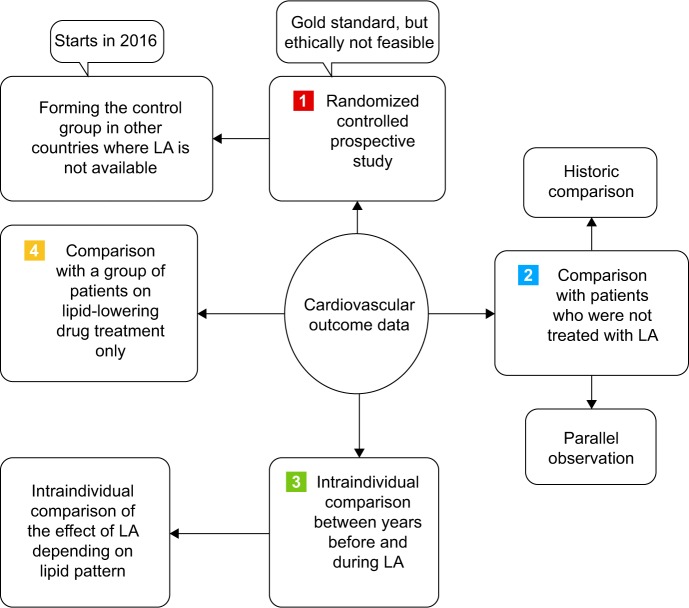
Randomized controlled prospective study
To date, no randomized controlled study has been performed to demonstrate the effects of LA on cardiovascular outcome date. When the Federal Joint Committee in Germany decided in 2008 to recognize an elevated Lp(a) level as an indication for LA, it requested that such a study should be started. A protocol has been written, but it was not approved by the ethical committee. In the meantime, the Federal Joint Committee has accepted this decision.
In order to solve this problem, an international prospective multicenter study in patients with high Lp(a) will start still in 2016 in which LA patients will be treated in Germany and carefully selected control patients will be picked up in countries where LA is not available (NCT02791802 on clinicaltrials.gov). A randomized study was done in patients with acute hearing loss.26 Patients who were treated with one HELP session had a benefit with respect to clinical parameters when compared with those who underwent a standard therapy (Figure 3).
Figure 3.
Principles of generating cardiovascular outcome data for LA treatment.
Abbreviation: LA, lipoprotein apheresis.
Comparison with patients who were not treated with LA
The life expectancy of patients with homozygous familial HCH is very short – usually <20 years. This could be significantly prolonged after LA was started in these patients. As described by Thompson et al,27 patients who started LA after 1994 were still alive 20 years later in contrast to those patients who started LA earlier. Life expectancy could also be prolonged by LA in patients after heart transplant when compared with patients who were not extracorporeally treated (Figure 3).28
A regular HELP therapy had been performed for 2 years.29 The angiographies from 33 patients obtained before and after 2 years were evaluated blindly. The authors concluded that regular treatment with HELP was able to stabilize progressive atherosclerotic disease and induce almost twice as much regression as the progression of atherosclerotic lesions. Usually one can assume that atherosclerotic lesions progress without an intervention.
Intraindividual comparison between years before and during LA
Several studies have compared the incidence of cardiovascular events before the start of LA treatment with that during the LA treatment. In the past years, the results of three multicenter studies with representative numbers of patients (>300) with highly elevated Lp(a) and normal LDL-C values have been published.30–32 LA therapy resulted in a >80% reduction in major adverse cardiovascular events. The Pro(a) Life study was performed prospectively (from the start of LA treatment).32 There have also been case reports from different LA centers showing the efficacy of LA with respect to outcome data (Figure 3).21,33,34
We were the first to compare the reduction in cardiovascular events by LA depending on the absence or presence of elevated Lp(a) levels.35 In HCH patients with normal Lp(a), the reduction in the incidence of new cardiovascular events induced by LA therapy was reduced by 54% when comparing the 2 years before LA start with 2 years during LA. In contrast, in patients with elevated Lp(a) (either with normal or with elevated LDL-C), this reduction amounted to 83%. This difference has been confirmed by a Bavarian group.34
Comparison with a group of patients on lipid-lowering drug treatment only
One nonrandomized trial examined the safety and efficacy of adding LA to standard lipid-modifying therapy (LMT) for patients (n=130) with heterozygous familial HCH and cardiovascular disease. Treatment was observed over a 6-year period and compared to patients with heterozygous familial HCH and cardiovascular disease on standard LMT.36,37 The primary end points (nonfatal myocardial infarction, coronary angioplasty, coronary artery bypass, and death from coronary heart disease) achieved a 72% relative risk reduction and a number needed to treat of four with LA therapy compared with standard LMT (Figure 3).
In the randomized LDL-Apheresis Atherosclerosis Regression Study (LAARS), 42 males with HCH and severe coronary atherosclerosis were treated with either biweekly LA plus medication (40 mg simvastatin) or medication alone for 2 years.38 Only in the LA group did more minor lesions disappear in comparison to the medication group. During bicycle exercise tests, the time to 0.1 mV ST-segment depression increased significantly by 39%, while the maximum level of ST depression decreased significantly by 0.07 mV in the LA group versus no changes in the medication group. One critical point of this study is that patients underwent a biweekly LA interval, which is clearly not optimal and explains for the minor differences between the two groups.
In another trial involving an apheresis device that only removes Lp(a) (Pocard Lp[a] columns; POCARD Ltd., Moscow, Russia), coronary heart disease patients (n=30) with an elevated Lp(a) were randomized to weekly Lp(a) apheresis plus statin or statin alone. Following 18 months of treating only elevated Lp(a) (and not LDL-C), the apheresis group demonstrated a significant regression of coronary atherosclerosis (coronary angiography) compared with the control group.9
Safety, tolerability, and follow-up
LA is generally accepted as a safe therapeutic approach; however, particularly in female patients, venous puncture problems may arise. A part of the blood is outside of the body, and this explains why hypotensive episodes may occur. They can easily be handled with a saline infusion.
There is a danger of bleeding because an anticoagulant is always needed. We observed a major impact of the HELP system on coagulation in patients who were treated with oral anticoagulants. The citrate infusion may induce a decrease in calcium levels – oral intake of calcium is recommended and some patients need an additional calcium infusion. Technical problems are seldom seen – the providers offer easily accessible technical service.
At the Dresden LA center, the mean rate of AEs was 7.7%. Throughout the 23-year study period, ten different methods were employed in treating 268 patients for a total of 25,293 treatments (LA, immunoadsorption, and rheophoresis).39 AEs more often occurred after the initiation of the extracorporeal therapy.
With respect to the severity of adverse effects (Table 4), we observed mild AEs (no treatment was necessary) in 61.3%, moderate AEs (oral medication or infusion was given) in 37.0%, and severe AEs (emergency hospitalization was necessary) in 1.7% of the patients. Therapy had to be stopped prematurely in 1.5% of the treatments. No patient died during an extracorporeal session. Very rarely we saw a heparin allergy and were happy to offer those patients an LA method where heparin is not needed.
Table 4.
Adverse effects during extracorporeal LA therapy (listed according to frequency)
|
Abbreviation: LA, lipoprotein apheresis.
In a paper from a Bavarian LA center, 96.7% of all LA sessions were performed without any AEs, vascular access problems, or technical problems.34 The lower rate of AEs in comparison to Dresden data can be explained in that we also included immunoadsorption and rheophoresis, which are associated with a higher AEs rate.
Although in general no major blood loss occurs during LA treatment, several patients develop an iron deficiency – the regularly performed taking of blood to check the lipid concentrations may play a role. It is possible to replace the iron deficit with intravenous injections.40 Neither ACE inhibitors nor the neprilysin inhibitor sacubitril should be prescribed for LA patients – they may lead to a bradykinin syndrome, especially when a whole blood system is applied.
All so-called specific LA methods exert an impact on other (besides lipoproteins) protein concentrations.41 HELP and filtration methods effectively decrease fibrinogen concentrations. The slightest impact on total serum protein and on albumin was observed with the whole blood methods. A major effect was seen on the immunoglobulins when filtration methods were applied. The impact of filtration methods on ferritin may contribute to iron deficit.
When we start treating a patient with LA, we measure lipids before and after each LA session in order to optimize the treatment regime. We later check lipids only once per month, but at the start and then every 3 months we look at blood count, iron parameters, renal function, liver and muscle enzymes, protein concentrations, blood sugar, etc. In patients on oral anticoagulants, usual control parameters are checked regularly. In patients with clinical problems, control parameters are tested more often (eg, calcium).
Patient-focused perspectives such as quality of life, patient satisfaction/acceptability, adherence, and uptake
It has to be stressed that most patients for whom LA treatment is suggested are high-risk patients who suffered from (multiple) life-threatening cardiovascular events or invasive interventions (eg, coronary bypass operation and stenting). They often feel symptoms that are related to these events (eg, angina pectoris). They understand that their future life conditions and their life expectancy are in danger. This pressure motivates them to undergo more invasive therapeutic methods such as LA.
Before starting an LA therapy, the patient has to be informed about the requirements he or she has to fulfill: high degree of compliance (optimal lifestyle, regular drug intake, communicating about newly appearing further diseases, and hospital stays), adherence to the session schedule, time needed for an LA session, and appropriate attire during the sessions. Usually patients had a breakfast or lunch at home (we even offer lunch to the patients at the Dresden Apheresis center); it is not a major problem to determine lipids in a non-fasting state.42 Patients who are working have to coordinate the LA sessions with their work schedule.
In order to decrease the degree of anxiety, we usually invite new patients to visit the center and observe other patients on LA therapy. We also explain how effective the extracorporeal therapy will be – that we will likely be able to prevent new cardiovascular events but that there is no 100% guarantee.
In a cross-sectional study, we compared the psychological situation and the quality of life of LA patients (n=41) with patients on hemodialysis (HD; n=41) and healthy thrombocyte donors (n=29).43 LA and HD patients had similarly increased presence of psychological symptoms with concurrent decreased quality of life. Thus, an accompanying psychological treatment may be helpful.
In another recently published paper, 29 patients treated with LA showed lower quality-of-life scores regarding mental aspects and equal scores regarding physical aspects compared to the general population, analogous to the results of patients on HD.44 Their depression scores were higher than the general population. Compared to the preapheresis period, patients described an improvement in their physical and mental fitness, less angina pectoris, and no treatment-related pain (apheresis questionnaire). The authors conclude that LA treatment appears to reduce the subjective physical complaints of patients. The partly impaired mental health in patients undergoing LA may be attributed to the underlying severe cardiovascular disease. The procedure itself is generally tolerated without major complaints, suggesting that the benefits of LA exceed any negative effects on patient’s quality of life.
In general, LA therapy is a life-long therapy. There is no official age limit beyond which an LA should not be started, although in the daily practice 80 years appears to be a reasonable cutoff point.
When patients want to spend a holiday at another place, we usually agree but will insist that they should miss no more than two LA sessions. When patients suffer from an acute (severe) additional disease (eg, a flu), we try to minimize the number of missing LA sessions. Patients are required to inform the center of nonattendance in a timely manner; otherwise, the LA kits have to be thrown away unused (when no other patient who is on the same LA system is available). Contraindications against an LA therapy are listed in Table 5.
Table 5.
Contraindications against LA
|
Abbreviation: LA, lipoprotein apheresis.
The following are the reasons why patients stopped LA therapy: venous access was no longer possible, newly detected malignant tumors, severe cardiac insufficiency, extremely bad tolerability of LA, start of PCSK9 inhibitor therapy, and death. Noncompliance was never a reason to cease LA.
Being treated at an LA apheresis center also means that patients see a doctor each week. During these sessions, they have the opportunity to discuss all the complaints they have and to get medical advice. The patient’s general practitioner is usually informed about any suggestions the LA doctor may have in a letter.
Conclusions and future perspectives
LA has proven itself an effective, safe, and life-saving therapeutic tool for over 30 years. Particularly in Germany, the number of LA patients has increased over the past few years. In other countries, this number is much lower – LA is a costly and laborious procedure requiring special expertise.
In addition to financial resource concerns, the general attitude of the national health care system in a given country plays a role in the positioning of LA in the therapeutic armamentarium. When treating physicians become more aware of the significance of the risk factors, LDL-C and especially Lp(a), more patients to be treated with LA will emerge. Currently, some cardiologists repeat coronary stenting more than ten times and do not realize that it makes sense to treat the underlying metabolic abnormality.
One major problem is the saw-tooth effect on atherogenic lipoprotein concentrations, which makes it necessary to perform LA sessions weekly. On the other hand, lipid-lowering drugs induce a constantly low LDL-C level. However, clearly pleotropic effects differ between LA and lipid-modifying drugs – they probably contribute to the efficacy of LA.
Since the introduction of PCSK9 inhibitors into medical practice, it has become clear that in the future they will be used first in HCH patients before an LA therapy will be considered. According to the studies published with the available PCSK9 inhibitors alirocumab and evolocumab, the frequency of adverse effects is rather low. Mainly local injection-site reactions (≈5%), myalgia (≈5%), and neurocognitive disorders (≈1%) have been described. My (still limited) experience shows that there remain some patients who cannot tolerate these new drugs or for whom they are not effective enough. The latter is the case in patients with homozygous familial HCH. Thus, the number of HCH patients starting LA therapy will decrease, but some patients will still need LA. A few patients will be treated with both LA and PCSK9 inhibitor.
In Germany, the costs of PCSK9 inhibitor therapy amount to approximately €9,650 per year, while LA therapy costs approximately €50,000 per year. On the other hand, the number of patients with excessively elevated Lp(a) who need the extracorporeal therapy will increase. Lp(a) is still widely unknown among physicians, but the awareness of this risk factor is increasing. Germany is the only country where LA in these patients is officially being reimbursed. In the future, the antisense oligonucleotide against apo(a) may offer a new therapeutic approach. But it will take several years before outcome data with this new drug will be available.
Some critics claim that the efficacy of LA is simply explained by better medical care (regular contact with physicians, better lifestyle, and regular drug intake). The difference in the efficacy of LA with respect to the reduction in cardiovascular events between patients with normal and elevated Lp(a) could serve as an argument against this opinion – in all these patients the quality of medical care is not different at all.
In many LA centers, fewer than five patients are being treated. This is associated with two problems: 1) the experience of the medical staff is rather limited, and 2) only one LA method is used – patients cannot be switched to another LA method in case of necessity (either due to AEs or due to low efficiency of the applied LA method).45 Thus in the future, patients should preferably be concentrated in bigger LA centers.
Acknowledgments
The author thanks Kathy Eisenhofer for her help with the manuscript as a native speaker.
Footnotes
Disclosure
The author has received travel expenses from Diamed, Fresenius Medical Care, Kaneka; honoraria from Aegerion, Amgen, Chiesi, Sanofi, Kaneka, Diamed, and Fresenius Medical Care.
References
- 1.Catapano AL, Reiner Z, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) Atherosclerosis. 2011;217(Suppl 1):S1–S44. doi: 10.1016/j.atherosclerosis.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 2.Nordestgaard BG, Chapman MJ, Ray K, et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur Heart J. 2010;31(23):2844–2853. doi: 10.1093/eurheartj/ehq386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stroes ES, Thompson PD, Corsini A, et al. Statin-associated muscle symptoms: impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur Heart J. 2015;36(17):1012–1022. doi: 10.1093/eurheartj/ehv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gouni-Berthold I. PCSK9 antibodies: a new class of lipid-lowering drugs. Atheroscler Suppl. 2015;18:21–27. doi: 10.1016/j.atherosclerosissup.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Catapano AL, Ference BA. IMPROVE-IT and genetics reaffirm the causal role of LDL in cardiovascular disease. Atherosclerosis. 2015;241(2):498–501. doi: 10.1016/j.atherosclerosis.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Julius U. Niacin as antidyslipidemic drug. Can J Physiol Pharmacol. 2015;93(12):1043–1054. doi: 10.1139/cjpp-2014-0478. [DOI] [PubMed] [Google Scholar]
- 7.Tsimikas S, Viney NJ, Hughes SG, et al. Antisense therapy targeting apolipoprotein(a): a randomised, double-blind, placebo-controlled phase 1 study. Lancet. 2015;386(10002):1472–1483. doi: 10.1016/S0140-6736(15)61252-1. [DOI] [PubMed] [Google Scholar]
- 8.de Gennes JL, Touraine R, Maunand B, Truffert J, Laudat P. Homozygous cutaneo-tendinous forms of hypercholesteremic xanthomatosis in an exemplary familial case. Trial of plasmapheresis as heroic treatment. Bull Mem Soc Med Hop Paris. 1967;118(15):1377–1402. French. [PubMed] [Google Scholar]
- 9.Safarova MS, Ezhov MV, Afanasieva OI, et al. Effect of specific lipoprotein(a) apheresis on coronary atherosclerosis regression assessed by quantitative coronary angiography. Atheroscler Suppl. 2013;14(1):93–99. doi: 10.1016/j.atherosclerosissup.2012.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Stefanutti C, Di Giacomo S, Mazzarella B, Castelli A. LDL apheresis: a novel technique (LIPOCOLLECT 200) Artif Organs. 2009;33(12):1103–1108. doi: 10.1111/j.1525-1594.2009.00959.x. [DOI] [PubMed] [Google Scholar]
- 11.Moriarty PM. Lipoprotein apheresis: present and future uses. Curr Opin Lipidol. 2015;26(6):544–552. doi: 10.1097/MOL.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 12.Stefanutti C, Mazza F, Steiner M, et al. Relationship between sustained reductions in plasma lipid and lipoprotein concentrations with apheresis and plasma levels and mRNA expression of PTX3 and plasma levels of hsCRP in patients with hyperLp(a)lipoproteinemia. Mediators Inflamm. 2016;2016:4739512. doi: 10.1155/2016/4739512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Julius U, Milton M, Stoellner D, et al. Effects of lipoprotein apheresis on PCSK9 levels. Atheroscler Suppl. 2015;18:180–186. doi: 10.1016/j.atherosclerosissup.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 14.Terai N, Julius U, Haustein M, Spoerl E, Pillunat LE. The effect of low-density lipoprotein apheresis on ocular microcirculation in patients with hypercholesterolaemia: a pilot study. Br J Ophthalmol. 2011;95(3):401–404. doi: 10.1136/bjo.2010.180901. [DOI] [PubMed] [Google Scholar]
- 15.Kopprasch S, Bornstein SR, Schwarz PE, Bergmann S, Julius U, Graessler J. Single whole blood dextran sulfate adsorption favorably affects systemic oxidative balance in lipoprotein apheresis patients. Atheroscler Suppl. 2013;14(1):157–160. doi: 10.1016/j.atherosclerosissup.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Tamai O, Matsuoka H, Itabe H, Wada Y, Kohno K, Imaizumi T. Single LDL apheresis improves endothelium-dependent vasodilatation in hypercholesterolemic humans. Circulation. 1997;95(1):76–82. doi: 10.1161/01.cir.95.1.76. [DOI] [PubMed] [Google Scholar]
- 17.Morawietz H, Goettsch W, Brux M, et al. Lipoprotein apheresis of hypercholesterolemic patients mediates vasoprotective gene expression in human endothelial cells. Atheroscler Suppl. 2013;14(1):107–113. doi: 10.1016/j.atherosclerosissup.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Arai K, Orsoni A, Mallat Z, et al. Acute impact of apheresis on oxidized phospholipids in patients with familial hypercholesterolemia. J Lipid Res. 2012;53(8):1670–1678. doi: 10.1194/jlr.P027235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kassenärztliche Bundesvereinigung . Qualitätsbericht – Ausgabe 2015 – Berichtsjahr 2014. Berlin, Germany: Kassenärztliche Bundesvereinigung; 2015. Quality report – Edition 2015 – Reported year 2014. German. [Google Scholar]
- 20.Schwartz J, Padmanabhan A, Aqui N, et al. Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the writing committee of the american society for apheresis: the seventh special issue. J Clin Apher. 2016;31(3):149–162. doi: 10.1002/jca.21470. [DOI] [PubMed] [Google Scholar]
- 21.Emmrich U, Hohenstein B, Julius U. Actual situation of lipoprotein apheresis in Saxony in 2013. Atheroscler Suppl. 2015;18:215–225. doi: 10.1016/j.atherosclerosissup.2015.02.034. [DOI] [PubMed] [Google Scholar]
- 22.Schettler VJ, Neumann CL, Peter C, et al. First data from the German Lipoprotein Apheresis Registry (GLAR) Atheroscler Suppl. 2015;18:41–44. doi: 10.1016/j.atherosclerosissup.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Schettler VJ, Neumann CL, Peter C, et al. Impact of the German Lipoprotein Apheresis Registry (DLAR) on therapeutic options to reduce increased Lp(a) levels. Clin Res Cardiol Suppl. 2015;10:14–20. doi: 10.1007/s11789-015-0073-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee MK, Shigematsu H, Suh BY. 5(th) Asian PAD Workshop. Ann Vasc Dis. 2014;7(2):199–218. doi: 10.3400/avd.pad.14.01000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muso E, Mune M, Fujii Y, et al. Low density lipoprotein apheresis therapy for steroid-resistant nephrotic syndrome. Kansai-FGS-Apheresis Treatment (K-FLAT) Study Group. Kidney Int Suppl. 1999;71:S122–S125. doi: 10.1046/j.1523-1755.1999.07130.x. [DOI] [PubMed] [Google Scholar]
- 26.Suckfull M, Hearing Loss Study Group Fibrinogen and LDL apheresis in treatment of sudden hearing loss: a randomised multicentre trial. Lancet. 2002;360(9348):1811–1817. doi: 10.1016/S0140-6736(02)11768-5. [DOI] [PubMed] [Google Scholar]
- 27.Thompson GR, Seed M, Naoumova RP, et al. Improved cardiovascular outcomes following temporal advances in lipid-lowering therapy in a genetically-characterised cohort of familial hypercholesterolaemia homozygotes. Atherosclerosis. 2015;243(1):328–333. doi: 10.1016/j.atherosclerosis.2015.09.029. [DOI] [PubMed] [Google Scholar]
- 28.Julius U, Tselmin S, Fischer S, et al. Lipid apheresis after heart transplantation – the Dresden experience. Tx Med. 2010;22:355–362. [Google Scholar]
- 29.Schuff-Werner P, Gohlke H, Bartmann U, et al. The HELP-LDL-apheresis multicentre study, an angiographically assessed trial on the role of LDL-apheresis in the secondary prevention of coronary heart disease. II. Final evaluation of the effect of regular treatment on LDL-cholesterol plasma concentrations and the course of coronary heart disease. The HELP-Study Group. Heparin-induced extra-corporeal LDL-precipitation. Eur J Clin Invest. 1994;24(11):724–732. doi: 10.1111/j.1365-2362.1994.tb01068.x. [DOI] [PubMed] [Google Scholar]
- 30.Jaeger BR, Richter Y, Nagel D, et al. Longitudinal cohort study on the effectiveness of lipid apheresis treatment to reduce high lipoprotein(a) levels and prevent major adverse coronary events. Nat Clin Pract Cardiovasc Med. 2009;6(3):229–239. doi: 10.1038/ncpcardio1456. [DOI] [PubMed] [Google Scholar]
- 31.Rosada A, Kassner U, Vogt A, Willhauck M, Parhofer K, Steinhagen-Thiessen E. Does regular lipid apheresis in patients with isolated elevated lipoprotein(a) levels reduce the incidence of cardiovascular events? Artif Organs. 2014;38(2):135–141. doi: 10.1111/aor.12135. [DOI] [PubMed] [Google Scholar]
- 32.Leebmann J, Roeseler E, Julius U, et al. Lipoprotein apheresis in patients with maximally tolerated lipid-lowering therapy, lipoprotein(a)-hyper-lipoproteinemia, and progressive cardiovascular disease: prospective observational multicenter study. Circulation. 2013;128(24):2567–2576. doi: 10.1161/CIRCULATIONAHA.113.002432. [DOI] [PubMed] [Google Scholar]
- 33.Koziolek MJ, Hennig U, Zapf A, et al. Retrospective analysis of long-term lipid apheresis at a single center. Ther Apher Dial. 2010;14(2):143–152. doi: 10.1111/j.1744-9987.2009.00747.x. [DOI] [PubMed] [Google Scholar]
- 34.Heigl F, Hettich R, Lotz N, et al. Efficacy, safety, and tolerability of long-term lipoprotein apheresis in patients with LDL- or Lp(a) hyperlipoproteinemia: findings gathered from more than 36,000 treatments at one center in Germany. Atheroscler Suppl. 2015;18:154–162. doi: 10.1016/j.atherosclerosissup.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 35.von Dryander M, Fischer S, Passauer J, Muller G, Bornstein SR, Julius U. Differences in the atherogenic risk of patients treated by lipoprotein apheresis according to their lipid pattern. Atheroscler Suppl. 2013;14(1):39–44. doi: 10.1016/j.atherosclerosissup.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Mabuchi H, Koizumi J, Shimizu M, et al. Long-term efficacy of low-density lipoprotein apheresis on coronary heart disease in familial hypercholesterolemia. Hokuriku-FH-LDL-apheresis study group. Am J Cardiol. 1998;82(12):1489–1495. doi: 10.1016/s0002-9149(98)00692-4. [DOI] [PubMed] [Google Scholar]
- 37.Higashikata T, Mabuchi H. Long-term effect of low-density lipoprotein apheresis in patients with heterozygous familial hypercholesterolemia. Ther Apher Dial. 2003;7(4):402–407. doi: 10.1046/j.1526-0968.2003.00074.x. [DOI] [PubMed] [Google Scholar]
- 38.Kroon AA, Aengevaeren WR, van der Werf T, et al. LDL-Apheresis Atherosclerosis Regression Study (LAARS). Effect of aggressive versus conventional lipid lowering treatment on coronary atherosclerosis. Circulation. 1996;93(10):1826–1835. doi: 10.1161/01.cir.93.10.1826. [DOI] [PubMed] [Google Scholar]
- 39.Dittrich-Riediger J, Schatz U, Hohenstein B, Julius U. Adverse events of lipoprotein apheresis and immunoadsorption at the Apheresis Center at the University Hospital Dresden. Atheroscler Suppl. 2015;18:45–52. doi: 10.1016/j.atherosclerosissup.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Schatz U, Illigens BM, Siepmann T, et al. TIDILAP: treatment of iron deficiency in lipoprotein apheresis patients – a prospective observational multi-center cohort study comparing efficacy, safety and tolerability of ferric gluconate with ferric carboxymaltose. Atheroscler Suppl. 2015;18:199–208. doi: 10.1016/j.atherosclerosissup.2015.02.030. [DOI] [PubMed] [Google Scholar]
- 41.Julius U, Siegert G, Kostka H, Schatz U, Hohenstein B. Effects of different lipoprotein apheresis methods on serum protein levels. Atheroscler Suppl. 2015;18:95–102. doi: 10.1016/j.atherosclerosissup.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 42.Nordestgaard BG, Langsted A, Mora S, et al. Fasting is not routinely required for determination of a lipid profile: clinical and laboratory implications including flagging at desirable concentration cutpoints – a joint consensus statement from the European Atherosclerosis Society and European Federation of Clinical Chemistry and Laboratory Medicine. Eur Heart J. 2016;37(25):1944–1958. doi: 10.1093/eurheartj/ehw152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stasiewski E, Christoph M, Christoph A, Bittner A, Weidner K, Julius U. Mental symptoms and quality of life in lipoprotein apheresis patients in comparison to hemodialysis patients, platelet donors and normal population. Atheroscler Suppl. 2015;18:233–240. doi: 10.1016/j.atherosclerosissup.2015.02.035. [DOI] [PubMed] [Google Scholar]
- 44.Rosada A, Kassner U, Banisch D, Bender A, Steinhagen-Thiessen E, Vogt A. Quality of life in patients treated with lipoprotein apheresis. J Clin Lipidol. 2016;10(2):323–329. doi: 10.1016/j.jacl.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 45.Julius U, Fischer S, Schatz U, Passauer J, Bornstein S. Why an apheresis center should offer more than one lipoprotein apheresis method. Ther Apher Dial. 2013;17(2):179–184. doi: 10.1111/j.1744-9987.2012.01129.x. [DOI] [PubMed] [Google Scholar]
- 46.Julius U, Fischer S, Schatz U, Hohenstein B, Bornstein SR. Lipoprotein apheresis: an update. Clin Lipidol. 2013;8(6):693–705. [Google Scholar]
- 47.Bundesministerium für Gesundheit Bekanntmachung des Bundesausschusses der Ärzte und Krankenkassen über eine Änderung der Richtlinien über die Bewertung ärztlicher Untersuchungs- und Behandlungsmethoden gemäß § 135 Abs. 1 des Fünften Buches Sozialgesetzbuch (SGB V) (BUB-Richtlinien) BAnz. 2003;123:14486. German. [Google Scholar]
- 48.Bundesministerium für Gesundheit Bekanntmachung eines Beschlusses des Gemeinsamen Bundesausschusses über eine Änderung der Richtlinie Methoden vertragsärztliche Versorgung: Apherese bei isolierter Lp(a)-Erhöhung. BAnz. 2008;138:3321. German. [Google Scholar]
- 49.Kassenärztliche Bundesvereinigung . Qualitätsbericht – Ausgabe 2014 – Berichtsjahr 2013. Berlin: Kassenärztliche Bundesvereinigung; 2014. Quality report – Edition 2014 – Reported year 2013. German. [Google Scholar]