Abstract
Ramsay Hunt Syndrome (RHS) is a rare complication of latent varicella-zoster virus (VZV) infection that can occur in immunocompetent host. It usually involves ipsilateral facial paralysis, ear pain and facial vesicles. Disseminated herpes zoster is another complication of VZV infection typically seen in immunocompromised hosts. We describe a patient with relapsed chronic lymphocytic leukemia (CLL) who presented simultaneously with RHS and disseminated herpes zoster. While other complications have been documented to coexist with RHS, to our knowledge, this is the first reported case in the literature of concurrent RHS with disseminated herpes zoster.
Abbreviations: RHS, Ramsay Hunt syndrome; VZV, varicella-zoster virus; PCR, polymerase chain reaction; CLL, chronic lymphocytic leukemia; CTCL, cutaneous T-cell lymphoma
Keywords: Ramsay Hunt syndrome, Varicella zoster virus, Chronic lymphocytic leukemia
Introduction
Ramsay Hunt syndrome (RHS) is a rare complication of latent varicella-zoster virus (VZV) infection that typically occurs in immunocompetent host. The infection in this syndrome involves the facial nerve, although other cranial nerves are susceptible, including the trigeminal nerve, vestibulocochlear nerve, glossopharyngeal nerve, vagal nerve, as well as some cranial-spine ganglia [1], [2]. It is usually identified clinically as a triad of facial paralysis, ear pain and herpetiform vesicles in any cranial dermatome [3]. Other clinical manifestations include tinnitus, hearing loss, hyperacusis, vertigo, dysgeusia (abnormal taste sensations) and decreased tearing [1]. Diagnosis is made clinically based on history and neurological exam and further confirmed with MRI using a cranial nerve protocol or detection of VZV in exudate by polymerase chain reaction (PCR) [4], [5]. In a prospective study of 185 patients diagnosed with RHS, diagnosis was confirmed by PCR in only 25% of the patients, whereas in 75% of the cases viral testing was not performed and diagnosis was made clinically [6]. Due to the common features of ear pain and drainage, it can sometimes also be confused with otitis media [4], [5].
Disseminated herpes zoster is another complication of latent VZV infection, which can be seen in immunocompromised hosts [7], [8], [9]. Diagnosis is made clinically based on characteristic vesicular lesions seen on physical examination. In cases where the diagnosis is unclear, diagnosis can be confirmed with PCR of skin lesions or selected body fluids, direct fluorescent antibody of skin lesions and less preferably viral culture of skin lesion [10], [11]
Previously the literature described cases of RHS concurrent with VZV encephalitis [12], syndrome of inappropriate secretion of antidiuretic hormone [13], and laryngitis [14], but to our knowledge no previous cases of concurrent RHS and disseminated herpes zoster have been reported. Here, we describe a patient with relapsed chronic lymphocytic leukemia (CLL) being treated with ibrutinib (a selective inhibitor of Bruton's tyrosine kinase) who presented with concurrent RHS and disseminated herpes zoster.
Case report
A 63-year-old male diagnosed with CLL two years prior, presented to the emergency room (ER) with left ear pain and drainage. He suffered a CLL relapse after initial treatment with rituximab (a monoclonal antibody against CD20) and bendamustine (an alkylating agent), and was placed on ibrutinib after this relapse. His CLL course was complicated by pleural hematoma requiring left thoracotomy and decortication as well as a subsequent diagnosis of cutaneous T-cell lymphoma (CTCL) one year ago. The patient had a 6-day hospitalization two weeks prior to his current presentation for neutropenic fever treated with cefepime, metronidazole and filgrastim (a granulocyte colony stimulating factor analog). At the end of that hospitalization, he began having left ear pain and swelling. One day prior to his current presentation, he presented to the ER with several days of drainage from his left ear. He was diagnosed with serous otitis media and discharged home with amoxicillin/clavulanate. Nevertheless, the ear pain worsened.
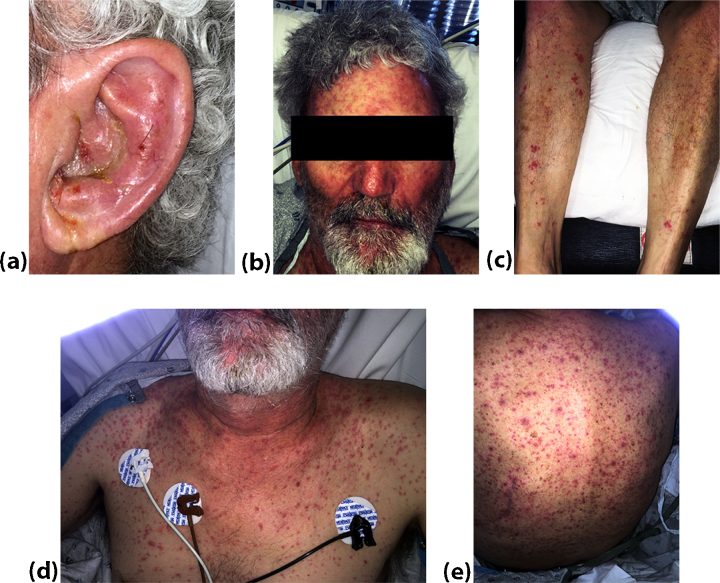
Upon representation, he complained of several episodes of non-bloody, non-bilious emesis along with fatigue, decreased appetite, night sweats, sore throat and dizziness on standing. He was found to have bullous lesions behind his tympanic membrane. Over the next 24 h, he developed erythematous papules with vesicles on his left ear (Fig. 1(a)) and along his left face, scalp, neck, chest, abdomen, back, and leg (Fig. 1(b)–(e)). On neurological exam, the patient had blurred vision in his left eye.
Fig. 1.
Varicella rash first seen in (a) left ear, followed by disseminated rash on (b) face, (c) legs, (d) chest, and (e) back.
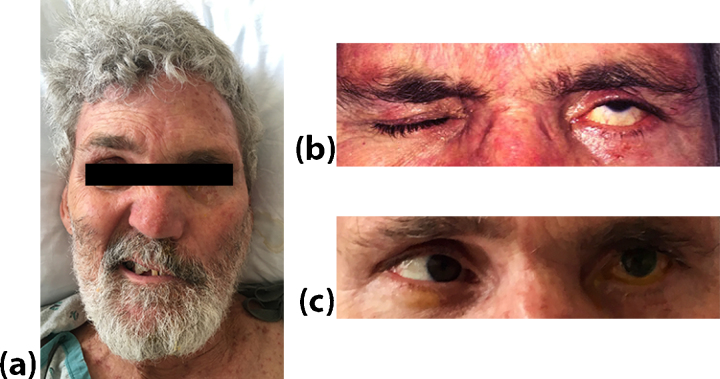
He had weakness of both upper and lower facial muscles suggesting lower motor facial nerve palsy (Fig. 2(a)–(b)). He also had decreased hearing in his left ear suggesting acoustic nerve involvement. Initial laboratory studies showed normal complete blood cell count, complete metabolic and coagulation panels. His blood cultures were negative and his sputum culture showed contamination with upper respiratory flora.
Fig. 2.
Cranial nerve deficits associated with Ramsay Hunt syndrome. Patient (a) trying to smile and raise eyebrows suffers from paralysis on left side, (b) trying to close both eyes but unable to fully close left eye, and (c) unable to abduct left eye past midline when looking to left.
A swab of his draining vesicle grew mixed skin microorganisms, with few polymorphonuclear leukocytes, but PCR of the swab was negative for VZV and herpes simplex virus. The patient was given a diagnosis of disseminated herpes zoster and RHS based on his clinical history, physical and neurological examination, despite the negative PCR results. Of note, about a month after the patient’s current presentation, he had a punch biopsy of a vesicular lesion on his left leg that was positive for VZV on immunohistochemical stain. After clinical diagnosis, he was started on acyclovir 750 mg IV q8 h and ciprofloxacin/dexamethasone drops for his ear, as well as oral ciprofloxacin 500 mg bid. For his blurred vision, ophthalmology consultants thought it was concerning for exposure keratopathy and recommended management with eye lubrication and moisture goggles.
Computed tomography (CT) of the chest, abdomen and pelvis showed interval worsening of lymphadenopathy representing progression of CLL. Patient’s hospital course was complicated by laryngitis requiring monitoring in the intensive care unit. Ibrutinib was briefly discontinued during this time for concern of bleeding but was resumed when he stabilized. He also developed new diplopia secondary to a new left abducens nerve palsy with lateral rectus dysfunction (Fig. 2(c)). Additionally the patient developed numbness on the left side of his face, suggesting a trigeminal nerve involvement. Brain MRI was obtained and showed no cranial nerve involvement but a new enhancing lesion in the right frontoparietal region was consistent with progression of CLL. Repeat brain MRI a month from the initial MRI showed unchanged nodule with interval decrease in surrounding vasogenic edema. On PET, this single brain lesion was too small to characterize.
Discussion
To our knowledge this is the first case reported of concurrent RHS and disseminated herpes zoster. While RHS can occur in an immunocompetent host, disseminated herpes zoster typically occurs in an immunocompromised host [11]. The patient had two main factors that contributed to an immunocompromised state and increased his risk for disseminated herpes zoster, namely his history of relapsed CLL [15] and his exposure to ibrutinib, which has been shown to be associated with an increased risk of infections, neutropenia, and thrombocytopenia [16]. Our patient indeed presented with neutropenia in the weeks leading up to his current presentation. Although disseminated herpes zoster can have visceral organ involvement [17], there was no evidence of such involvement in this case. Exactly which factors resulted in this unusual presentation of concurrent RHS and disseminated VZV is unclear but we believe going forward, it will be prudent for clinicians to always entertain this rare possibility in patients with RHS who develop a rash.
There are a few findings in this case that are worth discussing further. First, the patient initially tested negative for VZV on PCR of the vesicle swab. Often PCR is not sent as the diagnosis of disseminated VZV is primarily made clinically [6]; PCR is usually positive but may be negative in 20% of cases. Despite the initial negative PCR testing of vesicle for VZV, the pattern and appearance of rash as seen in Fig. 1 was characteristic for herpes zoster. The diagnosis was supported by a later positive immunohistochemistry stain in skin biopsy for VZV. Second thing of note is that the patient was initially diagnosed with otitis media. However, the patient’s presentation of RHS was similar to other previously reported cases [18], where ear pain and drainage were initially attributed entirely to otitis media. Third, the patient continued to have ear pain and drainage despite treatment with acyclovir and even after the resolution of his herpes zoster rash. There was possibly a superimposed bacterial infection, and the patient was treated with ciprofloxacin/dexamethasone eardrops as well as oral ciprofloxacin.
Antiviral agents such as acyclovir for herpes zoster are indicated for all patients if they are immunocompromised, or for immunocompetent patients over 50 years old, with moderate-severe pain, severe rash, or involvement of eye or ear [19]. The use of corticosteroids for herpes zoster is controversial [19], however our patient also developed serious laryngitis accompanied with stridor. The etiology of the laryngitis was unclear, and it could have been caused by patient’s underlying CLL, a drug reaction, or herpes zoster. In a previous case or herpes zoster laryngitis and RHS, combination therapy with steroids and antiviral agents was recommended [14]. Given the severity and the lack of clarity of the etiology of laryngitis, our patient was treated with high dose corticosteroids in addition to acyclovir therapy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
None.
Contributor Information
Ishita Chen, Email: ishita.chen@wustl.edu.
Raymond B. Fohtung, Email: rfohtung@wustl.edu.
Hanadi Ajam Oughli, Email: ajamoughlih@wustl.edu.
Robert Bauer, Email: rbauer@wustl.edu.
Caline Mattar, Email: cmattar@wustl.edu.
William G. Powderly, Email: wpowderly@wustl.edu.
Mark S. Thoelke, Email: mthoelke@wustl.edu.
References
- 1.Adour K.K. Otological complications of herpes zoster. Ann Neurol. 1994;35(Suppl):S62–S64. doi: 10.1002/ana.410350718. [DOI] [PubMed] [Google Scholar]
- 2.Wagner G., Klinge H., Sachse M.M. Ramsay Hunt syndrome. J Dtsch Dermatol Ges. 2012;10(4):238–244. doi: 10.1111/j.1610-0387.2012.07894.x. [DOI] [PubMed] [Google Scholar]
- 3.Sweeney C.J., Gilden D.H. Ramsay Hunt syndrome. J Neurol Neurosurg Psychiatry. 2001;71(2):149–154. doi: 10.1136/jnnp.71.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinoshita T., Ishii K., Okitsu T., Okudera T., Ogawa T. Facial nerve palsy: evaluation by contrast-enhanced MR imaging. Clin Radiol. 2001;56(11):926–932. doi: 10.1053/crad.2001.0730. [DOI] [PubMed] [Google Scholar]
- 5.Murakami S., Honda N., Mizobuchi M., Nakashiro Y., Hato N., Gyo K. Rapid diagnosis of varicella zoster virus infection in acute facial palsy. Neurology. 1998;51(4):1202–1205. doi: 10.1212/wnl.51.4.1202. [DOI] [PubMed] [Google Scholar]
- 6.Robillard R.B., Hilsinger R.L., Jr., Adour K.K. Ramsay Hunt facial paralysis: clinical analyses of 185 patients. Otolaryngol Head Neck Surg. 1986;95(3 Pt. 1):292–297. doi: 10.1177/01945998860953P105. [DOI] [PubMed] [Google Scholar]
- 7.Angit C., Daly B.M. Disseminated varicella zoster infection in a patient with rheumatoid arthritis treated with methotrexate. Clin Exp Dermatol. 2009;34(7):e453–e454. doi: 10.1111/j.1365-2230.2009.03500.x. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Doval I., Perez-Zafrilla B., Descalzo M.A., Rosello R., Hernandez M.V., Gomez-Reino J.J. Incidence and risk of hospitalisation due to shingles and chickenpox in patients with rheumatic diseases treated with TNF antagonists. Ann Rheum Dis. 2010;69(10):1751–1755. doi: 10.1136/ard.2009.125658. [DOI] [PubMed] [Google Scholar]
- 9.Kunz A.N., Rajnik M. Disseminated cutaneous varicella zoster virus infections during infliximab therapy for Crohn's disease: case report of two pediatric patients at one institution. Clin Pediatr (Phila) 2011;50(6):559–561. doi: 10.1177/0009922810380452. [DOI] [PubMed] [Google Scholar]
- 10.Chan E.L., Brandt K., Horsman G.B. Comparison of Chemicon SimulFluor direct fluorescent antibody staining with cell culture and shell vial direct immunoperoxidase staining for detection of herpes simplex virus and with cytospin direct immunofluorescence staining for detection of varicella-zoster virus. Clin Diagn Lab Immunol. 2001;8(5):909–912. doi: 10.1128/CDLI.8.5.909-912.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmutzhard J., Merete Riedel H., Zweygberg Wirgart B., Grillner L. Detection of herpes simplex virus type 1, herpes simplex virus type 2 and varicella-zoster virus in skin lesions. Comparison of real-time PCR, nested PCR and virus isolation. J Clin Virol. 2004;29(2):120–126. doi: 10.1016/s1386-6532(03)00113-6. [DOI] [PubMed] [Google Scholar]
- 12.Kin T., Hirano M., Tonomura Y., Ueno S. Coexistence of Ramsay Hunt syndrome and varicella-zoster virus encephalitis. Infection. 2006;34(6):352–354. doi: 10.1007/s15010-006-5669-4. [DOI] [PubMed] [Google Scholar]
- 13.Kageyama Y., Nakamura M., Sato A., Sato M., Nakayama S., Komatsuzaki O. Syndrome of inappropriate secretion of antidiuretic hormone (SIADH) associated with Ramsay Hunt syndrome: report of a case and review of the literature. Jpn J Med. 1989;28(2):219–222. doi: 10.2169/internalmedicine1962.28.219. [DOI] [PubMed] [Google Scholar]
- 14.Lee D.H., Yoon T.M., Lee J.K., Joo Y.E., Lim S.C. Herpes zoster laryngitis accompanied by Ramsay Hunt syndrome. J Craniofac Surg. 2013;24(5):e496–e498. doi: 10.1097/SCS.0b013e3182a12f95. [DOI] [PubMed] [Google Scholar]
- 15.Wadhwa P.D., Morrison V.A. Infectious complications of chronic lymphocytic leukemia. Semin Oncol. 2006;33(2):240–249. doi: 10.1053/j.seminoncol.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 16.Kokhaei P., Jadidi-Niaragh F., Sotoodeh Jahromi A., Osterborg A., Mellstedt H., Hojjat-Farsangi M. Ibrutinib-A double-edge sword in cancer and autoimmune disorders. J Drug Target. 2016;24(5):373–385. doi: 10.3109/1061186X.2015.1086357. [DOI] [PubMed] [Google Scholar]
- 17.Patel N., Singh D., Patel K., Ahmed S., Anand P. Atypical presentation of disseminated zoster in a patient with rheumatoid arthritis. Case Rep Med. 2015;2015:124840. doi: 10.1155/2015/124840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mortada R.A., El Fakih R.O., Assi M. Unusual presentation of Ramsay Hunt syndrome in renal transplant patients: case report and literature review. Transpl Infect Dis. 2009;11(1):72–74. doi: 10.1111/j.1399-3062.2008.00353.x. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J.I. Herpes zoster. N Engl J Med. 2013;369(18):1766–1767. doi: 10.1056/NEJMc1310369. [DOI] [PMC free article] [PubMed] [Google Scholar]