Serotonin-reuptake inhibitors (SRIs, SSRIs) and cognitive behavioral therapy (CBT) are currently considered the first-line treatments for body dysmorphic disorder (BDD). A practice guideline and a Cochrane review that recommend these treatments have been published,1,2 even though treatment research on BDD is still quite limited. The publication of these landmark documents underscores how important it is for clinicians to be knowledgeable about current treatment recommendations for BDD, which is a relatively common and often disabling disorder that is associated with high morbidity and mortality (see Didie et al, this issue).
Available data indicate that appropriate pharmacotherapy substantially improves core BDD symptoms, psychosocial functioning, suicidality, and other aspects of BDD in a majority of patients. Thus, medication is appropriate for patients who meet DSM-IV criteria for BDD. In the author's view, medication is essential for more severely ill and suicidal patients and for those with severe depressive symptoms.
This article reviews pharmacologic approaches for BDD. I first describe some essential groundwork for successful treatment of patients with medication. I then focus on SRIs, as they are currently considered first-line medications for BDD, including the delusional form of BDD. Practical issues such as SRI dosing, length of treatment, and augmentation strategies are discussed, as are other somatic treatments. Pharmacologic approaches to treating BDD are described in more detail elsewhere.1-3
This review and suggested treatment approaches are based on available evidence as well as clinical experience where indicated. First-line approaches (i.e., use of an SRI) have received more investigation than subsequent strategies (e.g., SRI augmentation) that may be needed, and no studies have examined treatment approaches for more highly treatment-refractory patients. The approaches suggested in this review are outlined in the algorithm in Figure 1. These approaches and the algorithm cannot necessarily be followed in a rigid or “cookbook” fashion, as individual patients may meaningfully differ (for example, in terms of comorbidity, co-occurring symptoms, past treatment response, tolerance of medication side effects, and access to medication). Thus, the general approaches discussed here may require some modification for individual patients. It should be noted that no medication has received FDA approval for the treatment of BDD, because a sufficient number of the type of studies needed to obtain FDA approval have not been done.
Figure 1.
Proposed Medication Treatment Algorithm for BDDa
a This is an abbreviated version of a proposed medication treatment approach to BDD; see the text for more detail. This algorithm incorporates and is consistent with scientific evidence, but because such evidence is currently limited, the algorithm is also based on clinical experience. The algorithm is for medication treatment only and does not include CBT, which appears effective for BDD (see article by Veale et al in this issue).
b In some cases (for example, for severe anxiety and suicidal thinking), consider combining a benzodiazepine or antipsychotic with an SRI as initial treatment.
c Has the highest SRI dose recommended by the pharmaceutical company or tolerated by the patient been reached and used for a minimum of 3 weeks, and has the total SRI trial duration been at least 12–16 weeks?
d Try to reach the highest SRI dose recommended by the pharmaceutical company or the highest dose tolerated for at least 3 weeks; continue the SRI for a total duration of 12–16 weeks to see if it will work.
e Options are discussed in the text
Under-recognition and underdiagnosis of BDD is a major impediment to successful pharmacologic treatment. Of particular relevance to this article, a study of 110 BDD subjects who had received psychotropic medication found that subjects revealed their BDD symptoms to only 41% of their pharmacotherapists.4 Patients may not spontaneously reveal their BDD symptoms because they are embarrassed and ashamed, fear they will be misunderstood and negatively judged (for example, as being vain), or for other reasons.3 It is important to diagnose BDD when present, because its treatment may differ somewhat from that of other disorders. In addition, comorbid disorders such as obsessive-compulsive disorder (OCD) may improve with a particular medication but BDD may not – or vice versa.5 Thus, clinicians are encouraged to use approaches such as those discussed elsewhere 3 (see Phillips and Feusner, this issue) to detect and diagnose BDD, and to specifically target BDD symptoms when providing pharmacotherapy.
ESSENTIAL GROUNDWORK FOR PHARMACOTHERAPY
The first essential step of treatment is to engage the patient and establish enough of an alliance that he or she is willing to try medication. This can be difficult to accomplish, as many patients are delusional, are rejection sensitive, prefer cosmetic treatment, or do not want other people (including a clinician) to see them because they are so “ugly.” Some patients resist a BDD diagnosis because they do not recognize that their appearance concerns are due to a mental illness;6 rather, they believe they truly are deformed and may desire cosmetic treatment instead (see Crerand and Sarwer, this issue). Other patients, however, welcome a diagnosis of BDD, as they are relieved to learn that they have a known and treatable disorder.
Some of the suggested approaches to screening and diagnosis discussed elsewhere in this issue may be helpful in establishing an alliance.3 It is important to listen to the patient's appearance concerns and take their distress seriously. Do not dismiss the patient's concerns as unimportant or trivial – but do not agree that there is something wrong with how they look. It is best not to try to convince patients that their view of their appearance is distorted, as this is unlikely to be successful. Instead, the clinician might say that people with BDD see themselves very negatively and differently from how other people see them for reasons that are not well understood.
Keep in mind that patients with BDD suffer tremendously, and try to empathize with their suffering. Focus on how the patient's appearance concerns are causing them to suffer and are impairing their functioning. When discussing treatment options, highlight the potential for medication to diminish the patient's distress and preoccupation and to improve their functioning and quality of life. Clinical experience suggests that motivational interviewing strategies that are modified for BDD may help to engage reluctant patients in treatment.7,8
It is important to provide psychoeducation about BDD and a rationale for recommended treatment. Some patients appreciate and benefit from recommended reading that provides accurate information about BDD. Clinicians need to provide information about recommended medication, the rationale for its use, and expected benefits (see below). It may be helpful to discuss the fact that SRIs are usually well tolerated, are not habit forming, and appear to normalize the brain. The likelihood of improvement, typical time course of improvement, potential side effects, and how side effects might be managed if they occur are other helpful topics to discuss before prescribing medication.
EFFICACY OF SRI's FOR BDD
SRIs are the best-studied medications for BDD and are currently considered the medication of choice for BDD.1-3,9 Available data consistently indicate that a majority of patients improve with SRI treatment that is appropriate for BDD.
Case reports from several decades ago suggested that fluoxetine and clomipramine improved BDD symptoms. e.g., 10-12 These reports led to larger clinical series,13,14 which in turn led to methodologically rigorous open-label studies.9 Two randomized, blinded, and controlled studies have been done (see Table 1).15,16 In all studies of SRIs, BDD symptoms significantly improved, with response rates of 53% to 73%. These response rates are based on conservative intention-to-treat analyses. Completer response rates (which include only those subjects who completed the study) were higher than intention-to-treat response rates.
Table 1.
Controlled and Open-Label SRI Studies in Body Dysmorphic Disordera
| Medication | Study Design | N | Trial Duration and Mean Dose (mg/day) | Resultsb | Reference |
|---|---|---|---|---|---|
| Clomipramine (Anafranil) vs desipramine | Randomized, double blind controlled cross-over trial | 40 entered; 29 randomized | - 16 weeks (8 weeks on each medication) - CMI: 138 ± 87 - DMI: 147 ± 80 |
Clomipramine was significantly more effective than desipramine for BDD symptoms and functional disability; response rate of 65% vs 35% on BDD-YBOCSc | Hollander et al., 1999 |
| Fluoxetine (Prozac) vs placebo | Randomized, double blind, placebo-controlled, parallel group trial | 74 entered; 67 randomized | - 12 weeks - 77.7 ± 8.0 range, 40-80) |
Fluoxetine was significantly more effective than placebo; response rate of 53% vs 18% on BDD-YBOCSd; effect size: d=.70 | Phillips et al., 2002 |
| Fluvoxamine (Luvox) | Open-label trial | 30 | - 16 weeks - 238.3 ± 85.8 (range, 50-300) |
63% of subjects responded to fluvoxamine on BDD-YBOCSd | Phillips et al., 1998 |
| Fluvoxamine (Luvox) | Open-label trial | 15 | - 10 weeks - 208.3 ± 63.4 (range, 100-300) |
10 subjects responded to fuvoxamine on the CGI | Perugi et al., 1996 |
| Citalopram (Celexa) | Open-label trial | 15 | - 12 weeks - 51.3 ± 16.9 (range, 10-60) |
73% of subjects responded to citalopram on BDD-YBOCSd; quality of life and functioning also significantly improved | Phillips and Najjar, 2003 |
| Escitalopram (Lexapro) | Open-label trial | 15 | - 12 weeks - 28.0 ± 6.5 (range, 10-30) |
73% of subjects responded to escitalopram on BDD-YBOCSd; quality of life and functioning also significantly improved | Phillips, 2006 |
Case reports, case series, and retrospective studies are not included in the table but are described in the text
Results are reported for an intent-to-treat analysis for all studies except for the clomipramine/desipramine trial, which used a minimum treatment analysis.
Response was defined as 25% or greater decrease in total BDD-YBOCS score; the BDD-YBOCS (Phillips et al., 1997) assessed BDD severity during the past week based on: (1) preoccupation with the perceived defect (time occupied, interference with functioning due to the preoccupation, distress, resistance, and control), (2) associated compulsive behaviors such as mirror checking (time spent, interference with functioning, distress if the behaviors are prevented, resistance, and control), (3) delusionality/insight, and (4) avoidance.
Response was defined as 30% or greater decrease in total BDD-YBOCS score
In a double-blind cross-over trial, the SRI clomipramine was more efficacious than the non-SRI antidepressant desipramine for BDD symptoms, depressive symptoms, and functional disability.15 Treatment efficacy was independent of the presence or severity of comorbid OCD, depression, or social phobia. This study's results are consistent with data from clinical series and retrospective studies which suggest that SRIs are more efficacious than a broad range of non-SRI medications for BDD (see below), although this important issue needs further study.
In a 12-week double-blind parallel-group placebo-controlled study (n=67 randomized subjects), fluoxetine was significantly more efficacious than placebo for BDD symptoms.16 Statistically significant separation of fluoxetine from placebo began at week 8. Response rates were 53% to fluoxetine and 18% to placebo. As in the above-mentioned clomipramine study, treatment efficacy was independent of the presence of comorbid major depressive disorder or OCD. In addition, BDD severity, BDD duration, or the presence of a personality disorder did not predict treatment response. Psychosocial functioning also improved to a significantly greater extent with fluoxetine than with placebo.17
Four systematic open-label SRI studies have been published (n=15-30), two with fluvoxamine, one with citalopram, and one with escitalopram.5,18-20 In intention-to-treat analyses, BDD response rates in these studies ranged from 63% to 83%, with statistically significant improvement in BDD severity in all four studies (see Table 1).
In the above studies, SRIs usually led to decreased preoccupation with the perceived appearance defects and less time performing BDD compulsions, as well as improved control over these thoughts and behaviors. BDD-related distress, insight, depressive symptoms, anxiety, anger-hostility, psychosocial functioning, and mental health-related quality of life significantly improved15-21 in all or most studies that examined these variables.
In a post-hoc analysis of data from the fluoxetine study,16 fluoxetine appeared to exert a protective effect against worsening of suicidality compared to placebo.22 Fluoxetine and placebo did not significantly differ with regard to emergence of suicidality.22 In the open-label escitalopram study, suicidal ideation significantly decreased (p<.001).19 These findings are important, given the high rates of suicide attempts and completed suicide reported for BDD.23-25
Different SRIs have not been directly compared to one another in a methodologically rigorous prospective study, so it is unclear whether they are differentially efficacious. However, in a chart-review study of 90 patients treated in the author's clinical practice, response rates were similar for each type of SRI (citalopram and escitalopram were not examined in this study).26 Overall, 63% (n=55) of adequate SRI trials led to clinically significant improvement.
SRIs also appear efficacious for children and adolescents, although data are far more limited. SRI efficacy has been reported in case reportse.g., 27-30 and in a series of 33 children and adolescents with BDD,31 a majority of whom had clinically significant improvement in BDD symptoms with SRI treatment. In this report, no non-SRI medications were effective for BDD.31
EFFICACY OF SRI's FOR DELUSIONAL BDD
Most of the studies discussed above included patients with delusional BDD beliefs (i.e., those who were completely convinced that their beliefs about their appearance were accurate) as well as patients with non-delusional BDD beliefs. All of these studies found that delusional patients significantly improved with SRI monotherapy and that delusional patients were as likely to respond to SRI monotherapy as non-delusional patients.14-16,19,20,32 In the placebo-controlled fluoxetine study, fluoxetine was as efficacious for subjects with delusional BDD as for those with nondelusional BDD, with 50% and 55%, respectively, responding.16 In the desipramine/clomipramine study, clomipramine was more efficacious than desipramine regardless of whether patients had insight or held their BDD beliefs with delusional intensity.15 In fact, clomipramine was even more effective for delusional patients than nondelusional patients. These findings are consistent with prior case reports,11,28,30 clinical series,14,31 and open-label trials,19,20,32 which also indicated that delusional patients have a high response rate to SRI monotherapy.
These findings are important because in the author's clinical experience, many patients with delusional BDD receive antipsychotic monotherapy. While antipsychotics have received only very limited investigation, available data suggest that they are not promising as monotherapy for either delusional BDD or non-delusional BDD (see below). Therefore, SRIs are recommended as the medication of choice for both delusional and non-delusional patients.
DOSING AND DURATION OF SRI TRIALS
Relatively High SRI Doses Are Often Needed
Methodologically rigorous studies have not compared SRI doses to determine the relative efficacy of different doses. However, clinical experience suggests that while some patients respond to a low or moderate dose of an SRI, on average BDD requires relatively high SRI doses.3,33 A retrospective study of subjects who had been treated primarily in the community sheds some light on this issue.4 In this study, SRI trials for individual patients that were considered optimal or at least minimally adequate for BDD were associated with greater improvement in BDD, and with less severe current BDD symptoms, than non-optimal or inadequate SRI trials.4 SRI trials were considered “optimal” for BDD if they were 12 weeks or longer in duration and used (or exceeded, for SSRIs) the maximum dose recommended by the manufacturer. The following daily SRI doses were considered minimally adequate: fluvoxamine 150 mg, fluoxetine 40 mg, paroxetine 40 mg, sertraline 150 mg, clomipramine 150 mg, citalopram 40 mg, and escitalopram 20 mg. Ten weeks was considered a minimally adequate SRI trial duration.
In the author's clinical practice, the mean daily SRI doses used are: fluoxetine: 67 ± 24 mg, clomipramine: 203 ± 53 mg, fluvoxamine: 308 ± 49 mg, sertraline: 202 ± 46 mg, paroxetine: 55 ± 13 mg, citalopram: 66 ± 36 mg, and escitalopram: 29 ± 12 mg.3 Some patients benefit from doses that exceed the maximum dose recommended by the pharmaceutical company (this approach is not advised for clomipramine, however). Doses that exceed the maximum recommended dose are best suited to patients who have not adequately improved with the highest dose recommended by the pharmaceutical company and are tolerating the medication well. This approach is more appealing for patients who have not responded to several prior SRIs or SRI augmentation trials, for whom remaining medication options are becoming more limited.
The author generally suggests quicker titration for very ill or suicidal patients. However, the titration rate must be individualized and take into account such factors as how well the patient is tolerating the medication, frequency of patient monitoring, and patient preference. A general recommendation is to attempt to reach the maximum SRI dose recommended by the pharmaceutical company by week 5 to 9 of treatment, if tolerated, unless a lower dose is efficacious.
A 12-16 Week SRI Trial Is Recommended to Determine Effectiveness
Response to an SRI usually develops gradually and may require 12 or, occasionally, even 14-16 weeks (while, in many cases, reaching a relatively high dose). In the above-noted fluoxetine and fluvoxamine studies, the mean time to BDD response was 6 to 9 weeks.5,16 The citalopram and escitalopram studies had a mean time to response of only 4.6 ± 2.6 weeks and 4.7 ± 3.7 weeks, respectively.19,20 All of these studies used a fairly rapid titration schedule, so more time may be needed for patients to respond when slower titration is used.
Before concluding that an SRI is ineffective, the author recommends trying the SRI for 12-16 weeks while, if necessary, reaching the highest dose recommended by the manufacturer or tolerated by the patient for at least 2-3 weeks of the 12-16 weeks.3 If tolerated, higher doses than those recommended by the manufacturer (excluding clomipramine) can be cautiously tried, if appropriate for a particular patient, to obtain or optimize a response. If this approach is not effective, SRI augmentation or switching to another SRI is indicated (see below).
SRI AUGMENTATION AND SWITCHING
SRI Augmentation
Only one controlled study has investigated SRI augmentation in BDD. This small double-blind randomized study (n=28) examined addition of pimozide versus addition of placebo to ongoing fluoxetine treatment, after patients had had an adequate fluoxetine trial to which they had not responded.34 Pimozide was not more efficacious than placebo, regardless of whether patients’ appearance beliefs were delusional or nondelusional. The response rate to pimozide was 18.2% versus 17.6% with placebo, and the effect size was small. In a small case series, olanzapine augmentation of SRIs was not efficacious for BDD symptoms.35 In a chart-review study of 90 patients treated in the author's clinical practice, only 15% (n=2) of trials in which an SRI was augmented with an antipsychotic led to response, although the effect size for atypical antipsychotics was large.26 In the author's experience, however, it is sometimes helpful to add an antipsychotic to an SRI, especially when the patient is delusional, has prominent delusions of reference, is very agitated, or appears at risk for suicidal or violent behavior. Clinical experience suggests that atypical (or second-generation) antipsychotics may be more helpful than typical antipsychotics (ziprasidone appears particularly promising), although research is needed.
Augmenting an SRI with buspirone, a 5HT1A partial agonist, is appealing because this medication is usually so well tolerated. In a small open study, among 13 patients who had buspirone added to an ineffective SRI, six subjects (46%) improved.36 In the above-noted chart-review study, 33.3% (n=12) of SRI augmentation trials with buspirone led to significant improvement, with a large effect size.26 The mean buspirone dose was 56.5 ± 15.2 mg/day.
Other SRI augmentation strategies have received less investigation. In the above-noted chart review study, some patients improved with addition of clomipramine to an SSRI (or vice versa),26 although this strategy should be used cautiously, with close monitoring of clomipramine levels, because SSRIs may unpredictably and sometimes dramatically increase blood levels of clomipramine, which has a low therapeutic index. Occasional patients respond to SRI augmentation with lithium, bupropion, or methylphenidate.26 Venlafaxine augmentation of SSRIs appears promising but has not been studied. An adjunctive benzodiazepine should be considered for patients with prominent anxiety, agitation, or insomnia.3
The optimal duration of an augmentation trial is unclear, although in the author's clinical experience 6-8 weeks is probably adequate (although it is probably best to use a 12-week trial for clomipramine or venlafaxine augmentation).
Switching to Another SRI
In the above-noted chart-review study, 43% of patients who did not respond to an initial adequate SRI trial responded to at least one subsequent adequate SRI trial, and 43.5% of all subsequent adequate SRI trials received by these patients were effective.26 In contrast, SRI augmentation (considering all types of augmenting medication) led to response in 33% of trials.26 SRI augmentation was more efficacious when the augmenting agent was added to a partially effective SRI (41% response rate) as opposed to an ineffective SRI (18% response rate).26 From a clinical perspective, if a patient has failed many SRI trials (for example, three trials) without an attempt at augmentation, augmentation may be preferable to switching. But if a patient has failed several augmentation strategies with one SRI, switching to another SRI may be preferable. Whether to switch or augment is a complex decision that requires clinical judgment. Clinicians should also consider CBT for patients who poorly tolerate or are not responsive to medications.
Patients who respond to one SRI appear very likely to respond to another SRI. In the chart-review study, 92% of patients who responded to one SRI responded to a subsequent SRI.26
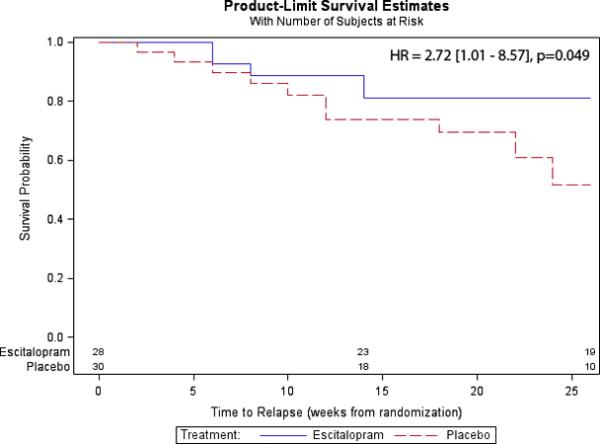
SRI CONTINUATION TREATMENT AND DISCONTINUATION
No published continuation or maintenance studies have been done. However, clinical experience suggests that many patients who respond to an SRI by 12 to 16 weeks of acute treatment continue to experience further gradual improvement with continuation of the SRI.
To the author's knowledge, the only available published data on relapse risk with SRI discontinuation is from the above-noted chart-review study in which 83% of patients relapsed after discontinuing an efficacious SRI.26 These preliminary data suggest that caution should be used if an SRI is discontinued. Suicide can occur following discontinuation of an effective SRI.3 If an effective SRI is discontinued, this should ideally be done when the patient is not highly stressed. It is probably better to slowly taper the SRI (e.g., over many months) rather than abruptly discontinuing it. It should not be assumed that receiving CBT during SRI discontinuation will reduce the relapse risk, as this issue has not been studied.
The author recommends continuing an effective SRI for several years, if not longer. The duration of SRI treatment needs to be individualized for each patient and based on clinical judgment. Patients who have previously relapsed after SRI discontinuation are candidates for longer-term SRI treatment. It is probably best for severely ill patients – especially those who have made numerous or potentially lethal suicide attempts – to continue an effective SRI for life.
OTHER MEDICATIONS AS MONOTHERAPY
In a small open-label trial of the antiepileptic medication levetiracetam, BDD symptoms, insight, depressive symptoms, and psychosocial functioning significantly improved.37 The mean endpoint dose was 2,044.1 ± 1,065.2 (range=250-3,000) mg/day. A small open-label trial (n=17) of venlafaxine suggested that this medication may be efficacious for BDD, although the primary analyses were for study completers rather than intention-to-treat.38 The results of both studies are promising, but until controlled studies are done these medications should not be considered first-line treatments for BDD.
A retrospective study of 50 patients found that 35 SRI trials resulted in improvement in BDD symptoms, whereas 18 non-SRI tricyclic antidepressant trials led to no overall improvement in BDD symptoms,39 a result similar to that in the prospective controlled study of clomipramine vs desipramine described above. Similarly, in a case series of 130 patients with BDD, who had received a total of 316 medication trials, only 15% of trials with non-SRI tricyclic antidepressants led to improvement.14,40 Of interest, 30% of 23 trials with MAO inhibitors were efficacious, suggesting that this approach might be considered for very treatment-refractory patients. Consistent with earlier case reports,12 antipsychotics were effective in only 1 of 49 trials, even though about half of the patients in this series had delusional BDD symptoms.14,40
OTHER SOMATIC TREATMENTS
BDD symptoms have been reported to respond to ECT in only two of approximately 25 cases.33 Careful clinical judgment is needed when considering use of ECT, however. ECT may be warranted, for example, when severe depressive symptoms do not appear to be entirely or largely due to BDD, or when depressive symptoms are life-threatening.
In case reports, improvement in BDD symptoms have been noted with a modified leucotomy,41 capsulotomy (P. Mindus, personal communication), bilateral anterior cingulotomy and subcaudate tractotomy (E. Cassem, personal communication), and anterior capsulotomy (S. Rasmussen, personal communication). In the author's view, neurosurgery should be considered only when a patient has not responded to many adequate medication trials and to CBT. It is an option to consider, however, for patients who are severely ill or appear at high risk of suicide.
CONCLUSIONS
Knowledge about effective pharmacotherapy for BDD has dramatically increased in recent years, and a majority of patients can improve with the approaches discussed in this review. However, additional pharmacotherapy research is greatly needed, including placebo controlled studies of SRIs and other medications, as well as augmentation studies, continuation studies, and relapse prevention studies. Research on the efficacy of medication for youth is a particularly pressing need. Also needed are studies that compare SRIs to CBT and studies of combined SRI/CBT treatment for BDD. Such research will greatly advance understanding of effective treatments for this severe and relatively common disorder.
REFERENCES
- 1.National Collaborating Centre for Mental Health Core interventions in the treatment of obsessive compulsive disorder and body dysmorphic disorder (a guideline from the National Institute for Health and Clinical Excellence, National Health Service) 2006 http://www.nice.org.uk/page.aspx?o=289817.
- 2.Ipser J, Sander C, Stein D. Pharmacotherapy and psychotherapy for body dysmorphic disorder. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD005332.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phillips KA. Understanding Body Dysmorphic Disorder: An Essential Guide. Oxford University Press; New York, NY: 2009. [Google Scholar]
- 4.Phillips KA, Pagano ME, Menard W. Pharmacotherapy for body dysmorphic disorder: treatment received and illness severity. Ann. Clin. Psychiatry. 2006;18:251–257. doi: 10.1080/10401230600948464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips KA, Dwight MM, McElroy SL. Efficacy and safety of fluvoxamine in body dysmorphic disorder. J. Clin. Psychiatry. 1998;59:165–171. doi: 10.4088/jcp.v59n0404. [DOI] [PubMed] [Google Scholar]
- 6.Eisen JL, Phillips KA, Coles ME, Rasmussen SA. Insight in obsessive compulsive disorder and body dysmorphic disorder. Compr. Psychiatry. 2004;45:10–15. doi: 10.1016/j.comppsych.2003.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilhelm S, Phillips KA, Steketee G. Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Modular Treatment Manual. Guilford Press, Inc.; New York: in press. [Google Scholar]
- 8.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. Guilford Press; New York, NY: 1991. [Google Scholar]
- 9.Phillips KA, Hollander E. Treating body dysmorphic disorder with medication: Evidence, misconceptions, and a suggested approach. Body Image. 2008;5:13–27. doi: 10.1016/j.bodyim.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brady KT, Austin L, Lydiard RB. Body dysmorphic disorder: the relationship to obsessive-compulsive disorder. J. Nerv. Ment. Dis. 1990;178:538–540. [PubMed] [Google Scholar]
- 11.Hollander E, Liebowitz MR, Winchel R, Klumker A, Klein DF. Treatment of body-dysmorphic disorder with serotonin reuptake blockers. Am. J. Psychiatry. 1989;146:768–770. doi: 10.1176/ajp.146.6.768. [DOI] [PubMed] [Google Scholar]
- 12.Phillips KA. Body dysmorphic disorder: the distress of imagined ugliness. Am. J. Psychiatry. 1991;148:1138–1149. doi: 10.1176/ajp.148.9.1138. [DOI] [PubMed] [Google Scholar]
- 13.Phillips KA, McElroy SL, Keck PE, Pope HG, Hudson JI. Body dysmorphic disorder: 30 cases of imagined ugliness. Am. J. Psychiatry. 1993;150:302–308. doi: 10.1176/ajp.150.2.302. [DOI] [PubMed] [Google Scholar]
- 14.Phillips KA, McElroy SL, Keck PE, Pope HG, Jr, Hudson JI. A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases. Psychopharmacol. Bull. 1994;30:179–186. [PubMed] [Google Scholar]
- 15.Hollander E, Allen A, Kwon J, et al. Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness. Arch. Gen. Psychiatry. 1999;56:1033–1039. doi: 10.1001/archpsyc.56.11.1033. [DOI] [PubMed] [Google Scholar]
- 16.Phillips KA, Albertini RS, Rasmussen SA. A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Arch. Gen. Psychiatry. 2002;59:381–388. doi: 10.1001/archpsyc.59.4.381. [DOI] [PubMed] [Google Scholar]
- 17.Phillips KA, Rasmussen SA. Change in psychosocial functioning and quality of life of patients with body dysmorphic disorder treated with fluoxetine: a placebo-controlled study. Psychosomatics. 2004;45:438–444. doi: 10.1176/appi.psy.45.5.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perugi G, Giannotti D, Di Vaio S, Frare F, Saettoni M, Cassano GB. Fluvoxamine in the treatment of body dysmorphic disorder (dysmorphophobia). Int. Clin. Psychopharmacol. 1996;11:247–254. doi: 10.1097/00004850-199612000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Phillips KA. An open-label study of escitalopram in body dysmorphic disorder. Int. Clin. Psychopharmacol. 2006;21:177–179. doi: 10.1097/01.yic.0000194378.65460.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phillips KA, Najar F. An open-label study of citalopram in body dysmorphic disorder. J. Clin. Psychiatry. 2003;64:715–720. doi: 10.4088/jcp.v64n0615. [DOI] [PubMed] [Google Scholar]
- 21.Phillips KA, Siniscalchi JM, McElroy SL. Depression, anxiety, anger, and somatic symptoms in patients with body dysmorphic disorder. Psychiatric Q. 2004;75:309–320. doi: 10.1023/b:psaq.0000043507.03596.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Phillips KA, Kelly MM. Suicidality in a placebo-controlled fluoxetine study of body dysmorphic disorder. Int. Clin. Psychopharmacol. 2009;24:26–28. doi: 10.1097/YIC.0b013e32831db2e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Veale D, Boocock A, Gournay K, Dryden W. Body dysmorphic disorder: a survey of fifty cases. Br. J. Psychiatry. 1996;169:196–201. doi: 10.1192/bjp.169.2.196. [DOI] [PubMed] [Google Scholar]
- 24.Phillips KA, Coles ME, Menard W, Yen S, Fay C, Weisberg RB. Suicidal ideation and suicide attempts in body dysmorphic disorder. J. Clin. Psychiatry. 2005;66:717–725. doi: 10.4088/jcp.v66n0607. [DOI] [PubMed] [Google Scholar]
- 25.Phillips KA, Menard W. Suicidality in body dysmorphic disorder: a prospective study. Am. J. Psychiatry. 2006;163:1280–1282. doi: 10.1176/appi.ajp.163.7.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips KA, Albertini RS, Siniscalchi JM, Khan A, Robinson M. Effectiveness of pharmacotherapy for body dysmorphic disorder: a chart-review study. J. Clin. Psychiatry. 2001;62:721–727. doi: 10.4088/jcp.v62n0910. [DOI] [PubMed] [Google Scholar]
- 27.Albertini RS, Phillips KA, Guevremont D. Body dysmorphic disorder in a young child (letter). J. Am. Acad. Child Adolesc. Psychiatry. 1996;35:1425–1426. doi: 10.1097/00004583-199611000-00010. [DOI] [PubMed] [Google Scholar]
- 28.El-khatib HE, Dickey T. Sertraline for body dysmorphic disorder. J. Am. Acad. Child Adolesc. Psychiatry. 1995;34:1404–1405. doi: 10.1097/00004583-199511000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Heimann SW. SSRI for body dysmorphic disorder. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:868. doi: 10.1097/00004583-199707000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Sondheimer A. Clomipramine treatment of delusional disorder-somatic type. J. Am. Acad. Child Adolesc. Psychiatry. 1988;27:188–192. doi: 10.1097/00004583-198803000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Albertini RS, Phillips KA. Thirty-three cases of body dysmorphic disorder in children and adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 1999;38:453–459. doi: 10.1097/00004583-199904000-00019. [DOI] [PubMed] [Google Scholar]
- 32.Phillips KA, McElroy SL, Dwight MM, Eisen JL, Rasmussen SA. Delusionality and response to open-label fluvoxamine in body dysmorphic disorder. J. Clin. Psychiatry. 2001;62:87–91. doi: 10.4088/jcp.v62n0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phillips KA. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder (Revised and Expanded Edition) Oxford University Press; New York, NY: 2005. [Google Scholar]
- 34.Phillips KA. Placebo-controlled study of pimozide augmentation of fluoxetine in body dysmorphic disorder. Am. J. Psychiatry. 2005;162:377–379. doi: 10.1176/appi.ajp.162.2.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips KA. Olanzapine augmentation of fluoxetine in body dysmorphic disorder (letter). Am. J. Psychiatry. 2005;162:1022–1023. doi: 10.1176/appi.ajp.162.5.1022-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phillips KA. An Open study of buspirone augmentation of serotonin-reuptake inhibitors in body dysmorphic disorder. Psychopharmacol. Bull. 1996;32:175–180. [PubMed] [Google Scholar]
- 37.Phillips KA, Menard W. A Prospective pilot study of levetiracetam for body dysmorphic disorder. CNS Spectr. 2009;14:252–260. doi: 10.1017/s1092852900025414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Allen A, Hadley SJ, Kaplan A, et al. An Open-label trial of venlafaxine in body dysmorphic disorder. CNS Spectr. 2008;13:138–144. doi: 10.1017/s1092852900016291. [DOI] [PubMed] [Google Scholar]
- 39.Hollander E, Cohen LJ, Simeon D, Rosen J, deCaria CM, Stein D. Fluvoxamine treatment of body dysmorphic disorder. J. Clin. Psychopharmacol. 1994;14:75–77. [PubMed] [Google Scholar]
- 40.Phillips KA. Pharmacologic treatment of body dysmorphic disorder. Psychopharmacol. Bull. 1996;32:597–605. [PubMed] [Google Scholar]
- 41.Hay G. Dysmorphophobia. Br. J. Psychiatry. 1970;116:399–406. doi: 10.1192/bjp.116.533.399. [DOI] [PubMed] [Google Scholar]


