Abstract
Objective: This study explored how chiropractic interns applied evidenced-based concepts, the sources of evidence they used, and how useful they perceived these sources to be in clinical decision making.
Methods: A questionnaire containing 13 items in a Likert 5-point scale was administered to 28 chiropractic interns to gather information on the evidence types they commonly accessed and their perceived usefulness of these sources in clinical decision making. The interns were in the 8th semester of the training program.
Results: There was a 93% (n = 26) response rate. Clinical guidelines were rated as the most helpful resource in clinical decision making (81%), followed by lecture materials (77%), journals (54%), databases (50%), and textbooks (35%). Students recognized scientific evidence as the most important aspect in clinical decision making. They found their personal experience and the views of their clinician to be equally important and patient preference the least.
Conclusion: Interns routinely employed high-quality levels of evidence in clinical decision making. They also considered their early, limited clinical experience as important as that of their clinical supervisor in decision making. This finding should be investigated further.
Key Indexing Terms: Evidence-Based Medicine, Chiropractic, Education, Clinical Decision Making
INTRODUCTION
Although the concepts of evidenced-based medicine (EBM) were originally developed and implemented within medical training programs, the basic 5-step framework for the generation of answerable clinical questions, the development of a search strategy, evaluation of the quality of the research, application, and self-evaluation in the process have now been widely adapted by other health professions.1 Chiropractic programs in North America began to implement the concepts of teaching and learning EBM in the early 2000s.2 Other international programs have followed, and EBM concepts are now part of all chiropractic curricula and are integral in program accreditation.3
The degree to which training within an evidenced-based framework influences the practice of chiropractic graduates remains unknown.4 At our university, evidenced-based practice principles are key components of several preclinical modules or courses. Modules in statistics and research methods provide training in research design, methodologies, and critical appraisal to facilitate EBM practice. Within the clinical setting, EBM learning objectives require interns to consider a broad range of research methodologies from guidelines to systematic analytical reviews and their application to specific patient care plans. While robust evidence does not exist for many aspects of chiropractic or allopathic medicine, clinical decision making can still take place within an evidence-based framework by considering clinician experience and patient expectations and values.5,6.
Although it was anticipated that this training approach should result in a broad application of EBM principles to patient care, the degree to which this has been achieved is currently unknown. This study sought to determine both the extent to which chiropractic interns apply evidenced-based concepts, in particular, the sources of evidence used in care planning, and how useful the chiropractic interns perceived these sources to be in developing a plan of care.
METHODS
This was a quantitative investigation that surveyed all 28 chiropractic interns of the university's first chiropractic cohort at the completion of their final (8th) semester. Prior to the commencement of data collection, the research proposal received full approval from the International Medical University (IMU) Joint Committee on Research and Ethics.
The questionnaire was generated by the authors and contained 12 Likert-type items, each with a 5-point response scale. The response categories were the same for all 12 questions: strongly agree, agree, neutral, disagree, and strongly disagree. There was also a single ranking question that asked participants to rank resources from 1st most important to 4th least important. The questionnaire was designed specifically for this study to explore the sources of evidence used by chiropractic interns to develop care plans during their internship training. The questionnaire contained 6 questions enquiring about the helpfulness of particular resources (Table 1) and 6 questions pertaining to how frequently those recourses were accessed (Table 2). In each section 2 questions were asked negatively. The results of the 4 negative questions were reversed so as to avoid disrupting the data analysis. The questionnaire was pilot tested among the university's chiropractic faculty.
Table 1.
The Helpfulness of Clinical Decision-making Resources (Helpfulness Group)
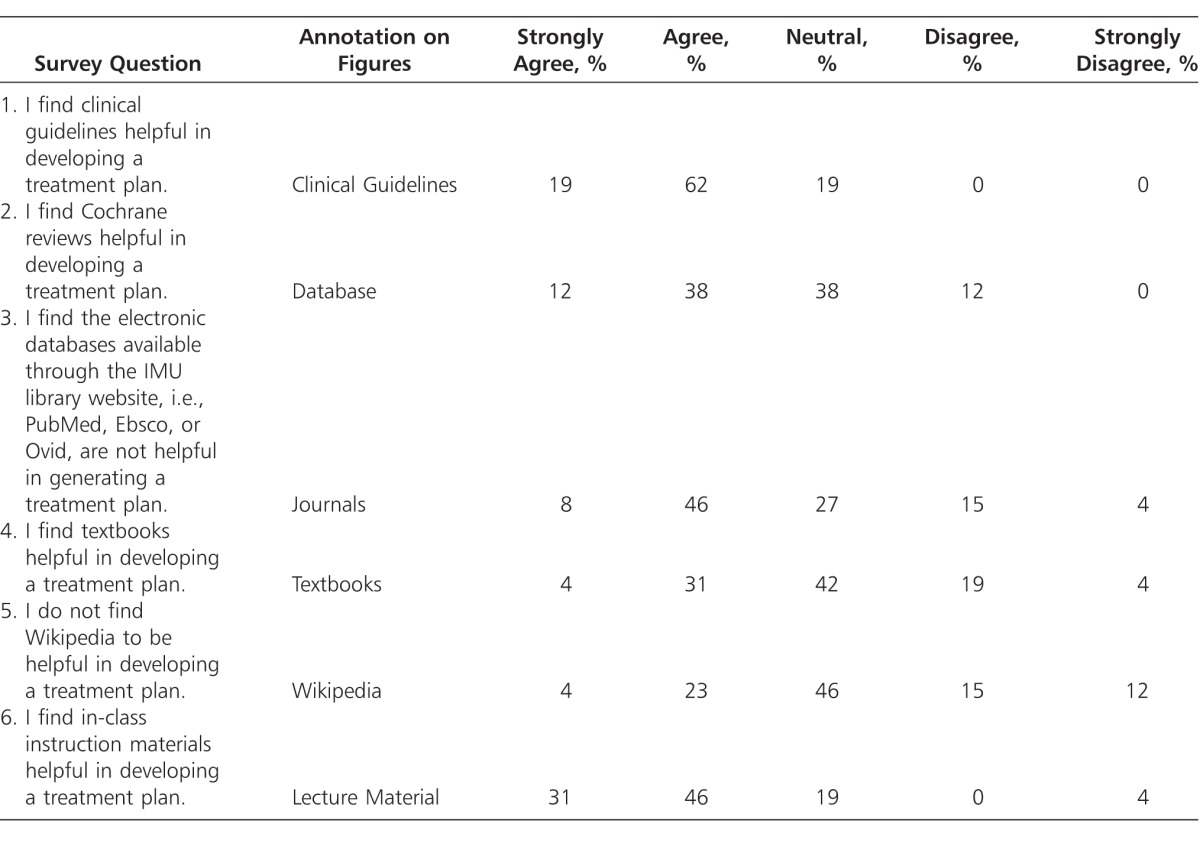
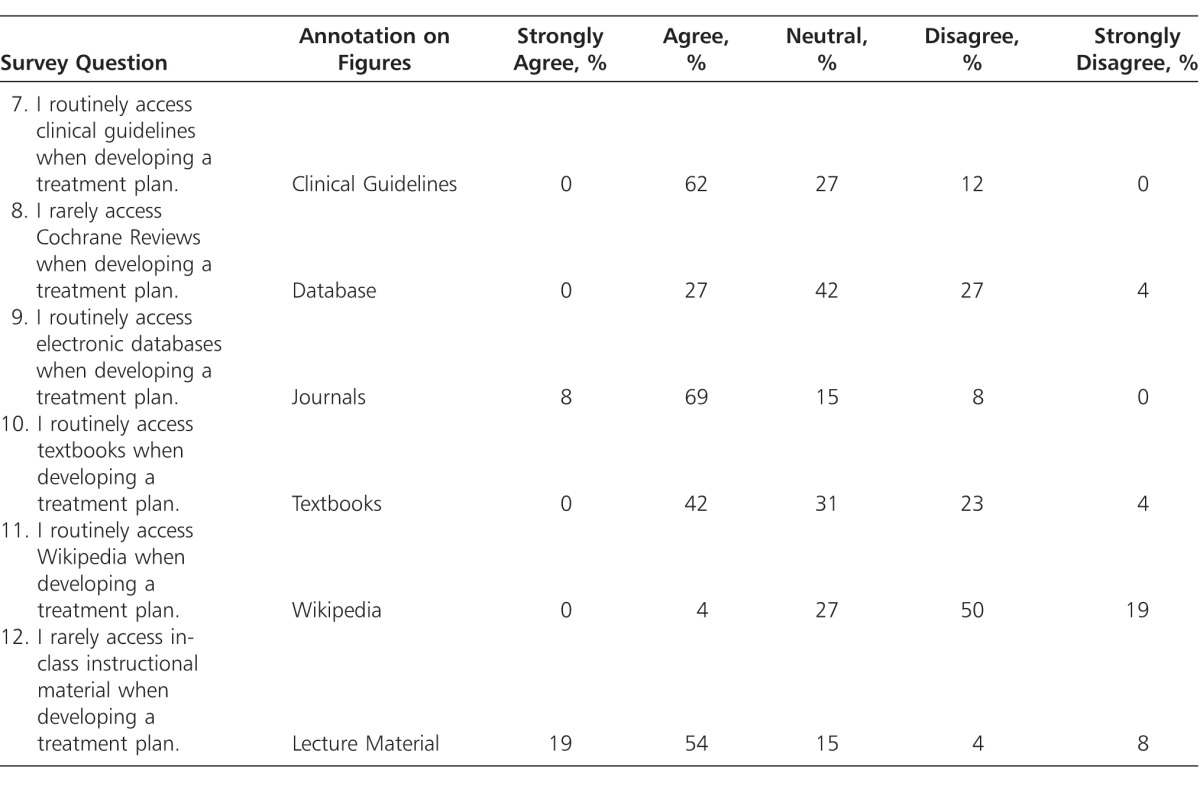
Table 2.
Resources Routinely Accessed for Clinical Decision Making (Usefulness/Accessibility Group)
The survey was distributed to the students during the final sign-out process from clinic. It was distributed in an envelope along with an information form outlining the purpose of the study and a consent form. Participation was voluntary. Study participants placed the completed questionnaire in an envelope and sealed the contents. To ensure anonymity, consent forms were placed in a similar envelope and sealed but kept separate from the surveys.
Questionnaire data were entered into Microsoft Excel (Microsoft Corp., Redmond, WA, USA), and descriptive statistics were used to tabulate the results.
RESULTS
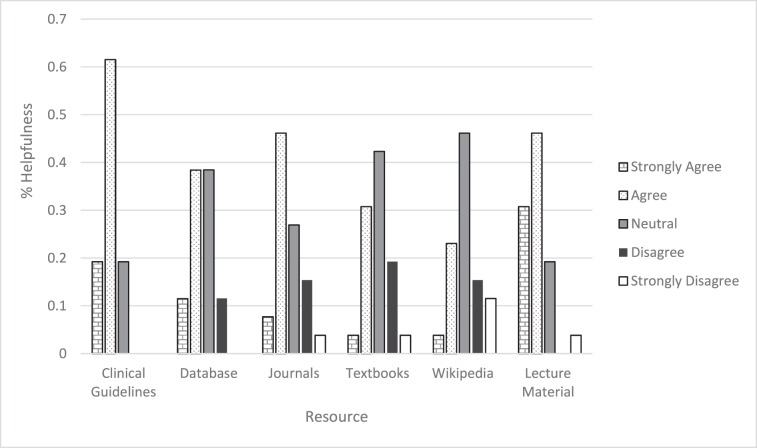
A total of 26 (93%) of 28 final-year semester 8 students completed the questionnaire. To discriminate between sources of information most frequently accessed versus those with the greatest helpfulness, students were asked to evaluate the same sources individually according to overall helpfulness and how frequently they were accessed in clinical decision making. The resources included clinical guidelines, library databases, journals, textbooks, lecture material, and Wikipedia. Positive responses to each question (strongly agree and agree) were collapsed to describe overall helpfulness. The most helpful resource in clinical decision making, with 81% of students strongly agreeing or agreeing, was found to be clinical guidelines (Fig. 1). Class lecture materials were considered to be the next most helpful (77%), followed by journals (54%), databases (50%), and textbooks (35%). Wikipedia was considered to be the least helpful, with a 27% positive response. Conversely, 27% also disagreed and disagreed strongly with the statement “I do not find Wikipedia to be helpful in developing a treatment plan.” It is possible that the negative wording of this question caused some confusion, however the second negative question in this category did not indicate a similar pattern. This will be discussed further in the limitations of this study.
Figure 1.
The helpfulness of clinical decision-making resources.
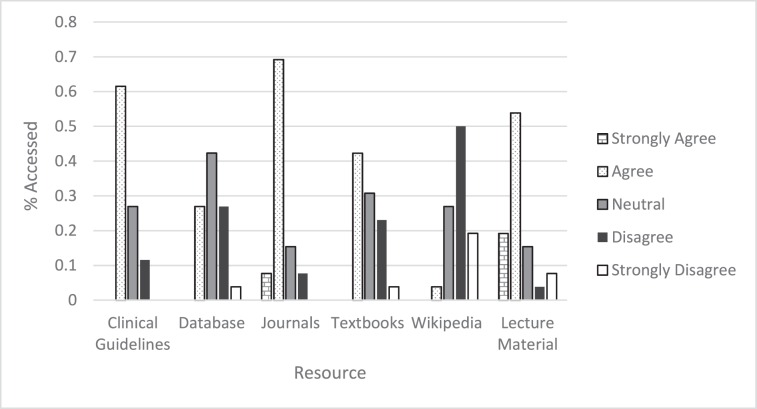
The students were then asked to prioritize individually a variety of different research types and sources. Using the same Likert scale, students were asked if they routinely or rarely accessed the various resources (Fig. 2). These individual ratings were then ranked to consider the most and least frequently accessed resources. The sum of the positive responses to each question (strongly agree and agree) was used to describe how frequently the resources were accessed. Overall, students most commonly accessed journals for clinical decision making (76%), closely followed by lecture material at 73%. Clinical guidelines (62%) and textbooks (42%) were both somewhat routinely accessed, while databases (27%) and Wikipedia (4%) were rarely accessed.
Figure 2.
Clinical decision-making resources routinely accessed.
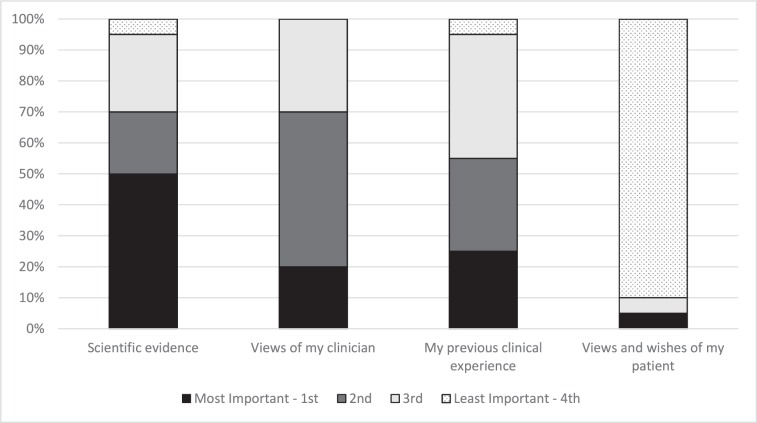
Finally, students were asked to rank in order of importance the 3 components of EBM, namely the best evidence, clinician experience, and patient expectations in care planning (Fig. 3). Because we were interested in the degree to which students' early experiences might shape their clinical decision making in the initial phases of training, they were asked to consider a fourth component, their experience. Students not surprisingly reported using scientific evidence most often in clinical decision making. Surprisingly, students more frequently considered their early clinical experiences equal to that of their more experienced clinical supervisors. Patients' expectations and values were considered least often when making decisions.
Figure 3.
Factors influencing clinical decision making.
DISCUSSION
We had a strong response to our survey, with 93% of the final-year interns completing the survey. While our sample group was small, it does give us a baseline for future comparisons. These data will allow us to assess changes that are currently being made to our curriculum. We will likely expand our survey to cover a broader spectrum of questions in the future. Currently, we are trying to weave EBM concepts throughout our curriculum to make it part of the majority of learning activities with the aim that, after graduation, interns will see research and evidence as playing a central role in all future care planning.
Our students appear to recognize a difference in the validity and utility of different clinical decision-making resources. This can be considered a positive reflection of the emphasis placed on EBM. Our students found the appropriate evidence-based resources more helpful and reported routinely using them during their internship. We are encouraged in that nonrefereed, non–peer-reviewed materials were least likely to be accessed and were the least useful.
In 2012, Shreeve queried the degree to which training within an evidenced-based framework influences the practice of chiropractic graduates. Results of this study suggest that, overall, the extent to which it influences practice after graduation remains largely unknown.4 Other studies that explored this relationship with health care students found that EBM concepts taught in standalone modules had little effect on actual clinical behavior of graduates.7,8 While evidence-based skills can be taught within the curriculum, they are not necessarily carried into private practice.9,10 Banzai suggests that a positive attitude toward evidence-based practice principles in health care education may be one of the first steps for motivating a health care professional student to later apply EBM principles in individual practice7. In our study, results suggest that students were routinely accessing and applying higher orders of evidence within their clinical training experiences. Whether this will translate into changes in practice behaviors early in their career will require additional study.
One key question in our survey explored the chiropractic intern's key source for clinical decision making. They were provided 3 options in ranking the order of importance of the 3 components of EBM, namely, the best evidence, clinician experience, and patient expectations and values in care planning. Once again because we were interested in the degree to which their own early clinical experience informed clinical decision making, they were asked to include in their ranking their own experiences. Surprisingly, students ranked their own early experiences as equal to the experience of their clinical supervisors.
According to Schon,11 professionals typically require up to 5 years before building confidence in their own experiences. The results of this study suggest that the students placed a high degree of importance on their own experiences much earlier than previously proposed. This raises a number of important considerations. First, without complementary reflective exercises, students may draw the wrong conclusions from limited experiences within the uncontrolled clinical environment. Second is the role of preprofessional identity and the informal curriculum. The degree to which preestablished beliefs might drive rigid views of best practice within chiropractic clinical training requires further consideration and may play a role in the outcomes of our survey. Third, there is the quality of the early clinical training experience. Poor-quality clinical training experiences may continue to perpetuate poor clinical decision making after graduation. Conversely, high-quality experiences may enhance clinical decision making and overall quality of patient care. And finally, it may simply be that students build on a broad range of experiences but continue to look to best evidence and patient expectations and values for decision making.
The final-year students reported their own personal clinical experience as equal to that of their clinical educators when making clinical decisions. Previous studies have considered medical/health care interns as having higher levels of self-confidence than actual knowledge in EBM.7,12,13 This shows a level of self-confidence that did not correlate with that of clinical supervisors. This is consistent with internal assessment conducted at IMU and the chiropractic program regarding work preparedness. Using the work readiness questionnaire as developed by Osterman,14 we identified that graduating students consistently rated their readiness to enter their workforce much higher than did the faculty. Our results suggest that, like medical students, chiropractic students tend to have higher levels of confidence in themselves than their supervisors have in the interns. Although not specifically explored in this study, the concepts are interrelated and should be considered in future research planning.
Limitations
Limitations of this study include the small sample size (n = 26). However, with a total of 28 students in this cohort, it does give us an excellent response rate. With such a high response rate, some bias will be negated that would have existed otherwise. Six of the 12 questions were asked in relation to helpfulness and a further 6 regarding the frequency of access. Within each category, 2 questions were asked in a negative manner. As many of our interns do not speak English as a first language it is possible that this may have caused some confusion in terms of agreeing and disagreeing with a negative question and with question repetition. Question number 5 was “I do not find Wikipedia to be helpful in developing a treatment plan.” While 27% of students replied positively (strongly agreed or agreed), the same percentage disagreed or strongly disagreed. This may be due to confusion over the wording of the question; however, the other 3 negative questions did not show the same pattern of results. In the frequency of access questions, the 2 defining words chosen in the questionnaire were “routinely” or “rarely.” It is possible that when students read a questionnaire quickly, these words may have caused confusion. Perhaps more dissimilar words may have been a better choice.
CONCLUSION
This study found that students routinely accessed and found useful higher levels of research. Lower-quality evidence was less frequently accessed and found to be less helpful. Students ranked scientific evidence as the most helpful in clinical decision making. Students ranked their own experience as equal to that of their more experienced clinical supervisors. They less frequently considered the expectations and values of patients. Further study is required to more deeply understand the high level of self-confidence in a student's early clinical training.
Supplementary Material
FUNDING AND CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare relevant to this work.
REFERENCES
- 1. Sackett DL Rosenber WMC Muir Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996; 312: 71– 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ruegg R, Crowther ER, Harris G. Integrating evidence based clinical practice into a chiropractic curriculum: the experiences of the Canadian Memorial Chiropractic College. Poster presented at: the Association of Chiropractic Colleges Tenth Annual Conference, March 13–16, 2003; New Orleans, LA. J Chiropr Educ. 2003; 17: 76– 77. [Google Scholar]
- 3. Council on Chiropractic Education Australasia. Home page. Australia. http://www.ccea.com.au. 2016. Accessed July 2014. [Google Scholar]
- 4. Shreeve MW. Evidence-based chiropractic education: are we equipping graduates for clinical practice with improved patient outcomes? J Chiropr Educ. 2012. 26: 184– 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. LeFebvre RP, Peterson DH, Haas M, et al. Educational research in action: training the evidence-based practitioner: University of Western States document on standards and competencies. J Chiropr Educ. 2011; 25: 30– 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haas M, Leo M, Peterson D, LeFebvre R, Vavrek D. Evaluation of the effects of an evidence-based practice curriculum on knowledge, attitudes, and self-assessed skills and behaviors in chiropractic students. J Manipulative Physiol Ther. 2012; 35 9: 701– 709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Banzai R, Derby DC, Long CR, Hondras MA. International web survey of chiropractic students about evidence-based practice: a pilot study. Man Ther. 2011: 19: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ. 2004; 329: 1– 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bradley P, Oterholt C, Herrin J, Nordheim L, Bjørndal A. Comparison of directed and self-directed learning in evidence-based medicine: a randomised controlled trial. Med Educ. 2005; 39: 1027– 1035. [DOI] [PubMed] [Google Scholar]
- 10. McGinn T, Seltz M, Korenstein D. A method for real-time, evidence-based general medical attending rounds. Acad Med. 2002; 77: 1150– 1152. [DOI] [PubMed] [Google Scholar]
- 11. Schon DA. The Reflective Practitioner: How Professionals Think in Action. New York, NY: Basic Books; 1983. [Google Scholar]
- 12. Caspi O, McKnight P, Kruse L, Cunningham V, Figueredo AJ, Sechrest L. Evidence-based medicine: discrepancy between perceived competence and actual performance among graduating medical students. Med Teach. 2006; 28 4: 318– 325. [DOI] [PubMed] [Google Scholar]
- 13. Wong JJ, Di Loreto L, Kara A, et al. Assessing the attitudes, knowledge and perspectives of medical students to chiropractic. J Can Chiropr Assoc. 2013; 57 1: 18– 31. [PMC free article] [PubMed] [Google Scholar]
- 14. Osterman T. Chiropractic perceptions of readiness for practice: preceptor and student perspectives. University of Minnesota Duluth. https://d-commons.d.umn.edu/bitstream/10792/349/1/Osterman,%20Terrence.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.