Abstract
Spermatogenesis is sustained by the proliferation and differentiation of spermatogonial stem cells (SSCs). However, the molecules controlling these processes remain largely unknown. Here, we developed a simplified high concentration serum-containing system for the culture of mouse SSCs. Analysis of SSCs markers and transplantation results revealed that the cultured spermatogonia retained stem cell characteristics after long-term in vitro propagation. Using this culture system, the expression and function of bone morphogenetic protein 4 (BMP4) were explored. Immunostaining showed that BMP4 was predominantly expressed in germ cells and that its level increased as spermatogenesis progresses. BMP4 receptors BMPR1A and BMPRII were present in spermatogonia, spermatocytes, and round spermatids. Moreover, despite the mRNAs of these two genes being present in mouse Sertoli cells, only BMPRII was detected by using Western blotting assays. While exogenous BMP4 by itself did not induce the expression of Stra8 and c-Kit, two marker genes of differentiating spermatogonia, a significant cooperative effect of BMP4 and retinoic acid (RA) was observed. Moreover, pretreatment of cultured spermatogonia with the BMP4 antagonist Noggin could inhibit RA-induced expression of these two marker genes. In conclusion, BMP4 may exert autocrine effects and act cooperatively with RA to induce the differentiation of spermatogonia in vivo.
1. Introduction
Mammalian spermatogenesis is a highly productive and organised process of cell proliferation and differentiation, resulting in the production of virtually unlimited number of spermatozoa throughout the life of the male [1]. This system roots in SSCs, which are capable of both self-renewal and differentiation dependent on the extrinsic and intrinsic cues [2]. Taking advantage of the discovery that GDNF stimulates SSC survival and proliferation in vivo [3], two groups first established the long-term cultures of mouse SSCs [4, 5]. In most studies, the initiation of SSCs cultures requires low concentration of foetal calf serum (FCS) in addition to several key growth factors [6]. Although a serum-free and feeder-free culture system has been established recently, the inclusion of serum products such as BSA and fetuin, which may contain other contaminated substances, not only resulted in variable passage timing and colony morphology but also raised the question whether a true chemically defined system was feasible for the culture of SSCs [7, 8]. Remarkably, several studies have demonstrated that SSCs can also be reprogrammed to ES-like pluripotent stem cells that contribute to the three embryonic germ layers with germ line transmission under certain culture conditions of high concentration of FCS without the introduction of exogenous genes [9–11]. However, the reprogramming efficiency and the reproducibility are low and the underlying mechanisms are unknown. In the present study, we report that SSCs could be cultured in embryonic stem cell (ESC) medium supplemented with GDNF and bFGF for as long as 33 passages (6 months) without the observation of ESC-like clones.
Bone morphogenetic proteins (BMPs), which belong to the TGF-β superfamily, are widely expressed during mouse embryogenesis and in adults and play key roles in male reproductive biology [12]. The TGF-β superfamily members function as homodimers or heterodimers by binding to heterogenic receptor complexes containing type I and type II serine-threonine kinase receptors [13], both of which are essential for signal transduction [13–18]. Bone morphogenetic protein 4 (BMP4) is known to be important for germ cell differentiation and survival [19–21]. In mouse, targeted knockout of the BMP4 gene results in failure of formation of primordial germ cells (PGCs) [22, 23]. BMP4 is also necessary for the localization of PGCs to genital ridge and the survival of the genital ridge [24]. In the postnatal testis, one report showed that BMP4 was expressed in Sertoli cells and stimulates the expression of c-Kit in cultured spermatogonia [25], whereas another study indicated that BMP4 was predominantly expressed in spermatogonia and RA initiates the resumption of spermatogenesis through the suppression of BMP4 expression in vitamin A-deficient (VAD) mice [19]. Hu et al. found that BMP4 mRNA is localized primarily in spermatocytes and in other cells, including Sertoli cells, to a less extent [26, 27]. These discrepancies warrant further clarification of the localization BMP4 in postnatal mouse testis as well as its function in spermatogenesis.
Germ cells in embryos are bipotential at the beginning, and their final fates are determined by RA produced by mesonephric duct [28, 29]. Retinoic-degrading enzyme CYP26B1 prevents germ cells from initiating meiosis in male mouse gonad during embryogenesis [28, 30]. In VAD mouse, only germ cells at early stages are present [19] and the differentiation of the aligned type A (Aal) spermatogonia is inhibited [31–33]. Importantly, the capability of Aal spermatogonia to differentiate is restored upon administration of RA.
Given that both RA and BMP4 play important roles in various biological processes, it is not surprising that they interact in vitro and in vivo in several systems. For example, BMP2 and BMP4 have been shown to interact with RA signalling to induce apoptosis of P19 embryonic carcinoma cells [34, 35]. In foetal vertebrate limbs, BMP signalling is also known to mediate RA-induced interdigital cell apoptosis [36]. While it is evident that both RA and BMP4 are necessary for the male reproductive capacity, whether these signalling pathways interact with each other in the germ cells is yet to be determined. In this study, we examined the expression of BMP4 and its receptors in postnatal germ cells and Sertoli cells. Furthermore, we aimed to investigate whether BMP4 and RA could cooperatively regulate the expression of Stra8, a gene that is stimulated by RA for the initiation of meiosis [37] and c-Kit whose expression is activated in differentiating spermatogonia [38] by using cultured mouse spermatogonia.
2. Materials and Methods
2.1. Reagents and Experimental Animals
Recombinant rat GDNF and bFGF, recombinant human BMP4 factors, and mouse anti-BMP4 primary antibody were from R&D Systems (Minneapolis, MN, USA). RA was purchased from Sigma (Sigma-Aldrich). Rabbit anti-human RET (SC-167) and GFRa-1 (H-70), goat anti-human BMPRII (G-17) and β-actin polyclonal antibodies, FITC- and TRITC-conjugated anti-rabbit, and goat secondary antibodies were from by Santa Cruz (Santa Cruz, CA, USA). Mouse against PLZF mAb, DNase I, and collagenase type IV were from Calbiochem (Merck KGaA, Darmstadt, Germany). Goat against human vimentin polyclonal antibody and FCS (ES cell-qualified) and ESGRO LIF were from Chemicon (Billerica, MA, USA). Rabbit against BMPR1A and DAZL antibodies were from Abcam, and rabbit against p-Smad1/5/8 antibody was from Cell Signalling Technology (Beverly, MA, USA). High glucose DMEM was from Hyclone, while DPBS and 0.25% Trypsin-EDTA were from Gibco (Carlsbad, CA, USA). DBA/C57 F1 mice were obtained from Beijing Weitong River Laboratory Animal Inc., China. Ub-eGFP-lentivirus was bought from Shanghai GeneChem Company (GeneChem, Shanghai, CN). All protocols were approved by the Animal Care and Use Committee of the Institute of Zoology, Chinese Academy of Sciences.
2.2. Cell Culture Conditions
ESC medium consisted of DMEM (4.5 g/liter glucose) supplemented with 15% FCS, 1x NEAA, 50 μM 2-mercaptoethanol, 1x sodium pyruvate, 2 mM L-glutamine, 100 units/mL penicillin, 100 units/mL streptomycin, and 103 units/mL LIF, stored at 4°C and could be used for up to 3 weeks. 40 ng/mL GDNF and 10 ng/mL bFGF were added to the ESC medium shortly before use to make the SSC medium. Mouse embryonic fibroblast (MEF) cells were isolated from 13.5-day CD1 mouse embryo and cultured in DMEM medium supplemented with 10% FCS, 50 μM 2-mercaptoethanol, 2 mM L-glutamine, and antibiotics. For preparation of feeder layer, MEF cells were treated with mitomycin C (10 μg/mL, Roche) for 2.5 hours and then plated at a density of 5 × 104 cells/mL in wells precoated with 0.2% gelatin (Sigma-Aldrich). All cells were maintained at 37°C with an atmosphere of 5% CO2. MEF cells can be used after 24 hours of plating and are viable for one week.
2.3. Isolation and Collection of Mouse Spermatogonia
Spermatogonia from 4-5-day-old pup mice were prepared by following the two-step enzymatic digestion protocol [39] with some modifications. Briefly, decapsulated testis tissue was treated with 1 mg/mL collagenase type IV and 1 mg/mL DNase I for 5 min with gentle agitation in DPBS and then centrifuged at 50 ×g for 2 min followed by 3 washes with DPBS to remove the interstitial cells. Collected specimens were then treated with 0.25% Trypsin-EDTA and 1 mg/mL DNase I for another 5 min in 37°C with gentle agitation. Subsequently, FCS was added at a final concentration of 15% to terminate the digestion. Cells were then washed twice by centrifugation at 600 ×g for 5 min in DPBS. The pellet was resuspended in SSCs growth medium, plated on 0.2% (w/v) gelatin-coated tissue culture dish with a density of 2 × 105 cells per cm2 and cultured for 36–48 hours. Then, the medium was removed and cells were washed once with DPBS, pipetted gently to detach the spermatogonial germ cells from the attached somatic cells, and centrifuged at 600 ×g for 5 min. Germ cells were resuspended in SSCs culture medium and plated on the MEF feeder layer.
2.4. BMP4 and RA Treatment of Cultured Spermatogonia
About 2000 cells were cultured on laminin-coated plate with 15% or 1% FCS-containing medium in the presence of GDNF and bFGF for 24 hours and serum starvation for 6 hours before BMP4 treatment. Spermatogonia were stimulated with 100 ng/mL BMP4 for 1 hour and fixed with 4% PFA for further analysis. About 2 × 105 cells were cultured on MEF and treated the same way and protein was collected for Western blotting analysis. For the detection of BMP4- and/or RA-induced spermatogonial differentiation, about 2 × 104 spermatogonia were plated on MEF feeder and treated with BMP4 for 24 hours and then RA was added in the presence of BMP4 to continue culture for indicated time. Cells were collected for RNA preparation and real-time PCR analysis.
2.5. Transplantation and Analysis
DBA/ICR F1 hybrid male mice were used as recipients. First, 4–6-week-old mice were treated with 40 mg/kg busulfan to deplete the endogenous germ cells in the testis [40, 41]. For lentivirus infection, lentivirus was added into the medium at 20 MOI (multiplicity of infection) with 5 μg/mL polybrene. The medium was changed at 8–10 hours after transfection and the cells were maintained in vitro for proliferation. For testis transplantation, approximately 40 μL of virus transfected donor cells suspension (6 × 105 cells) was injected into the testis seminiferous tubules of the recipient mouse through the efferent duct [39], filling about 70% of the tubules. Six months after transplantation, testes were collected for analysis.
2.6. Preparation of Spermatocyte, Round Spermatid Cell, and Sertoli Cells
Highly enriched mouse spermatocyte and round spermatid cells were isolated from adult mouse testicular cell suspensions using cell-size fractionation by sedimentation through a bovine serum albumin gradient at unit gravity following Belle's protocol (see Figure S4A–C in Supplementary Material available online at http://dx.doi.org/10.1155/2016/9536192) [42]. The Sertoli cells were cultured by following the procedure published previously [43].
2.7. Immunostaining
For IFA staining, cells were fixed with 4% PFA followed by treatment with 0.1% Triton X-100 and blocked with BSA. Samples were then incubated at 4°C with indicated primary antibodies overnight. Nonspecific IgG was used as negative control. Then, samples were washed thrice with PBST and incubated with FITC- or TRITC-conjugated secondary antibody. Nuclei of the cells were stained with DAPI. For immunostaining with paraffin sections, after deparaffinization and antigen retrieval, following the protocol as described above. Fluorescent images were captured under Olympus IX 71 microscope, and images were combined and processed in Adobe Photoshop 7.0.
2.8. RNA Extraction, RT-PCR, and Real-Time RT-PCR
Total RNA was extracted using TIANGEN RNA Pre Micro kit according to the manufacturer's instruction. Reverse transcription was performed using oligo (dT) priming and M-MLV reverse transcriptase (Promega) following the manufacturer's instructions. PCR primers were listed in Table 1. PCR products were separated by electrophoresis on 1.5% agarose gels. Real-time RT-PCR were performed on ABI 7500 sequence detection system and analysed with ABI 7500 software.
Table 1.
PCR primer sequences and product size.
| Gene | Forward primer (5′–3′) | Reverse primer (5′–3′) | Product size |
|---|---|---|---|
| BMP4 | TCGTTACCTCAAGGGAGTGG | GGCGACGGCAGTTCTTATTC | 159 bp |
| BMPR1A | GGGTCGTTACAACCGTGAT | CAACCTGCCGAACCATCT | 164 bp |
| BMPR1B | TCAATGTCGTGACACTCCCATTCCT | TGCTGTACCGAGGTCGGGCT | 245 bp |
| ActRIIB | CGAGCGCTTCACCCACTTG | CACCACGACACCACGGCAC | 650 bp |
| ActRII | CCGGAGATGGAAGTCACA | CACATCCACACTGGTGCC | 432 bp |
| BMPRII | AGGCCCAATTCTCTGGATCT | CACTGCCATTGTTGTTGACC | 207 bp |
| Actin | CAGCCTTCCTTCTTGGGTAT | TGGCATAGAGGTCTTTACGG | 100 bp |
| Stra8 | ACAAGAGTGAGGCCCAGCAT | CCTCTGGATTTTCTGAGTTGCA | 71 bp |
| c-Kit | GCCACGTCTCAGCCATCTG | GTCGGGATCAATGCACGTCA | 119 bp |
2.9. Western Blotting Analysis
Cells were harvested and homogenised at 4°C in lysis buffer containing preformed protease inhibitors mixture (P8340, Sigma). Total proteins were transferred to polyvinylidene difluoride membranes after SDS-PAGE, blocked with 5% fat-free milk then hybridized with primary antibodies. After hybridization with HRP-conjugated secondary antibody, immune-complexes were detected using Supersignal West Pico detection reagent (Pierce).
2.10. Statistical Analyses
All experiments were repeated at least thrice unless otherwise stated. Densitometry of Western blotting was conducted using the Quantity One software with GAPDH as internal control. Values were presented as mean ± standard deviation (SD) of three separate experiments. Statistically significant differences (P < 0.05 or P < 0.01) among groups were determined by ANOVA and Tukey posttests using SPSS statistical software (SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Establishment of a Simplified Long-Term Culture System for Mouse Spermatogonia
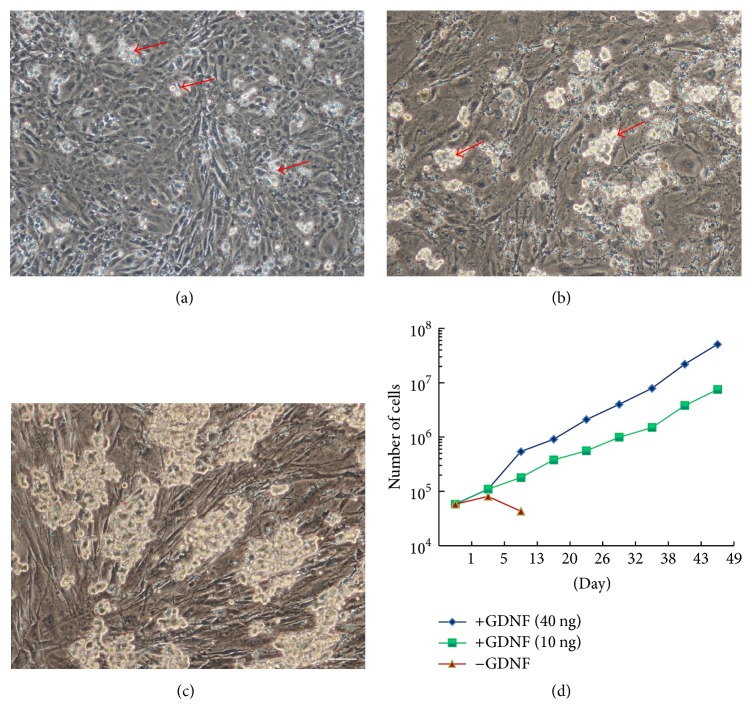
To establish SSC cultures in vitro, testicular cells were isolated using a modified two-step enzymatic digestion method [39]. After 24–36 hours of incubation in ESC medium supplemented with 40 ng/mL GDNF, somatic cells adhered tightly to the gelatin-coated dish and the germ cells, distinguished by their large size, attached loosely to the somatic cells. Germ cells at this stage were considered as Passage 0 (P0) of the spermatogonia culture (Figure 1(a)). The germ cells were then transferred to mouse embryonic fibroblast (MEF) feeder cells in a second culture dish by gentle pipetting; germ cells at this stage were cultured in ESC medium supplemented with GDNF, FGF2, and LIF and were considered as Passage 1 (P1). Cells at later passages were maintained in the same medium. Although most somatic cells can be removed at this step, some of them still remained. Therefore, spermatogonial clumps were mechanically collected and plated onto fresh feeder layers for the first 2-3 passages (Figure S1A). At this stage, the remaining somatic cells adhered tightly to the feeder layer and germ cells formed small clumps (Figure 1(b)). From the third passage, germ cells were passaged using 0.25% Trypsin-EDTA in a 1 : 3 dilution once every 5–7 days onto MEF feeders. By 2-3 weeks, cultures reached a relatively steady state and continued to generate clumps of similar morphology. Two strains of spermatogonia have been passaged for 6 months (P33) in vitro (Figure 1(c)). This method could be used to establish cultures from 4-5-day-old animals of the DBA/C57 F1 or DBA/ICR F1 mice. Consistent with previous reports, GDNF was indispensable for the long-term culture of mouse spermatogonia and it, at a concentration of 10 ng/mL in the medium, was enough to support the long-term proliferation of spermatogonia (Figure 1(d)).
Figure 1.
Establishment of mouse spermatogonial cultures in vitro. (a) Single spermatogonium or small spermatogonial clumps (red arrow) were observed 36 hours after culture in vitro. (b) At Passage 3 (P3), cells began to form stable colonies (red arrow) on MEF. (c) Spermatogonial clumps formed on MEF at day 180 in vitro. (d) Proliferation curves of spermatogonial cultures. Within 7-week period, spermatogonia expanded approximately 750-fold with 40 ng/mL GDNF and 500-fold with 10 ng/mL GDNF. Scale bar: 20 μm.
3.2. Characterization of Cultured Mouse Spermatogonia
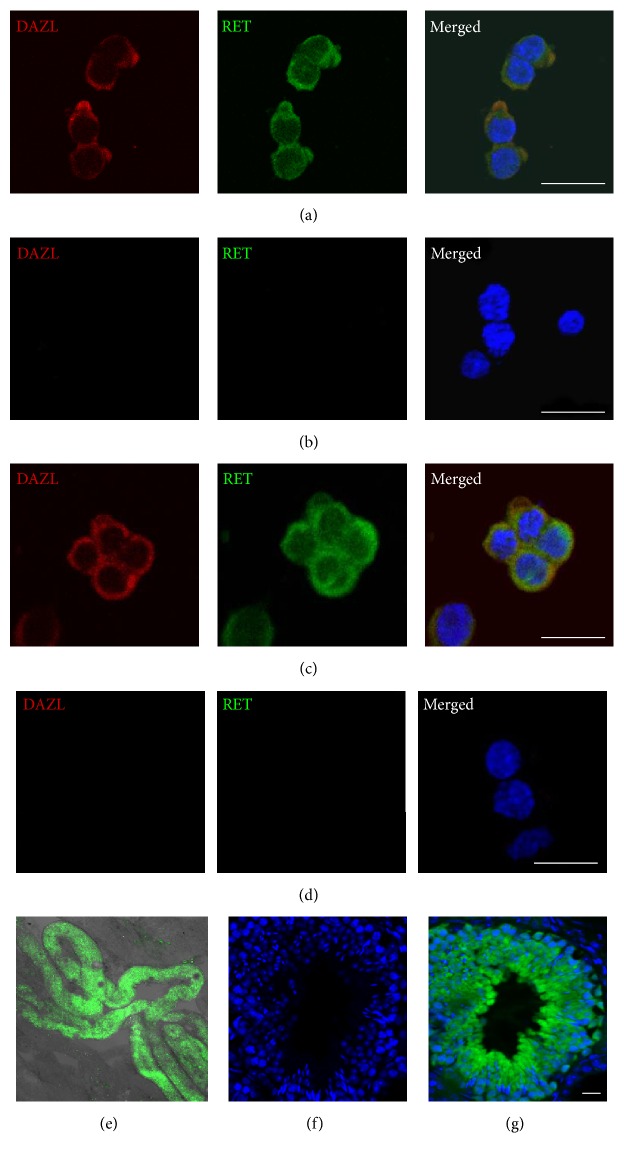
Immunostaining was employed to characterize the cultured spermatogonia. Clumps formed in early (P3) (Figures 2(a) and 2(b)) and long-term cultures (6 months in vitro, P33) (Figures 2(c), 2(d), S1B, and C) were positive for DAZL, a germ cell marker [44], and RET, a SSCs marker [45]. To further confirm the stem cell activity of these cultured spermatogonia, 6 × 105 GFP-expressing SSCs were injected into the testes of busulfan-treated adult recipient mice. Six months after transplantation, the recipient mice were sacrificed for analysis. The green spermatogonia could colonize the seminiferous tubules and restore spermatogenesis (Figure 2(e)). Importantly, the green spermatogonia in the seminiferous tubules could differentiate into germ cells at different stages (Figures 2(f), 2(g), and S2). These results confirmed the existence of SSCs in the spermatogonial cultures using the mouse ESC culture medium supplied with GDNF and FGF2.
Figure 2.
Characterization of cultured spermatogonia by examining SSC marker gene expression and transplantation assays. (a-b) P3 (6 days in vitro) culture of spermatogonia stained with antibodies against DAZL and RET (a) and nonspecific IgG (b). (c-d) P33 (180 days in vitro) culture of spermatogonia stained with antibodies against DAZL and RET (c) and nonspecific IgG (d). (e) Fluorescent image of seminiferous tubules of a recipient testis at 6 months after receiving Ub-EGFP-lentivirus infected spermatogonia. Note the extensive recolonization of green cells in the seminiferous tubules. (f-g) Cross-section of a seminiferous tubule recolonized by green germ cells at various differentiating stages. Scale bar: 20 μm.
3.3. Expression of BMP4 and Its Receptor Subunits in Germ Cells
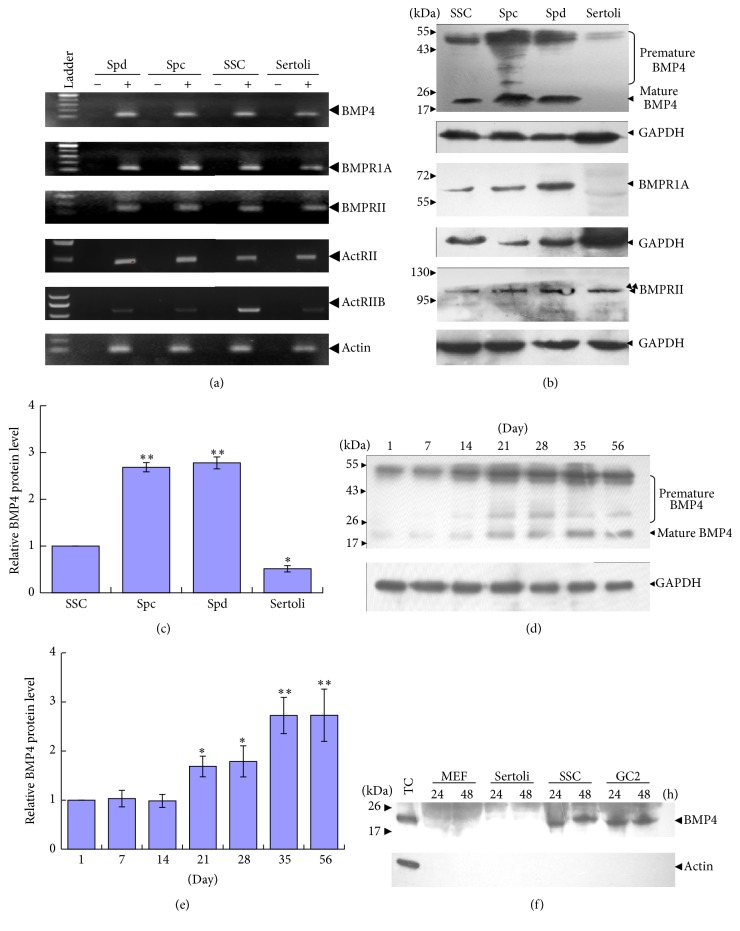
Using the simplified spermatogonial culture system, we decided to study the function of BMP4 in SSC differentiation in vitro. RT-PCR analysis first showed the mRNAs of BMP4 and its receptors BMPR1A, BMPRII, ActRII, and ActRIIB were present in cultured spermatogonia, Sertoli cells, and isolated adult spermatocytes as well as round spermatids (Figure 3(a)). Western blotting results further revealed that the premature and mature forms of BMP4 protein were predominantly expressed in spermatogenic cells, especially in adult spermatocytes and round spermatids (Figures 3(b) and 3(c)). Interestingly, BMPRII protein but not BMPR1A was present in Sertoli cells, which implies the absence of an intact BMP4 signalling pathway in these cells. Moreover, Western blotting analysis also showed the increased BMP4 protein expression as mouse testis development progresses through 1 to 56 days after birth (Figures 3(d) and 3(e)).
Figure 3.
Expression of BMP4 and its receptor subunits in testicular cells. (a) RT-PCR analyses of the expression of BMP4 and its receptors BMPR1A, BMPRII, ActRII, ActRIIB, and actin in isolated spermatocytes (Spc) and round spermatids (Spd), as well as in cultured spermatogonia (Spg) and Sertoli cells (Sertoli). RNA samples without RT but with PCR amplification were used as negative control. (b-c) Western blotting analysis of the expression of BMP4 and its receptors in 4-5-day-old mouse Spg, adult Spc and Spd, and Sertoli cells (b) and quantification of BMP4 protein in these cells (c). The premature and mature forms of BMP4 were labelled. (d-e) Western blotting analysis of BMP4 protein in mouse testis at indicated development stages (d) and quantification (e). (f) Western blotting analyses of secreted BMP4 in the medium from different cell cultures. Adult mouse testicular cells lysate (TC) was used as positive control. The data is presented as means ± SD from at least three independent experiments. Statistically significant differences among groups are indicated by asterisks, ∗ P < 0.05 or ∗∗ P < 0.01.
To test whether cultured spermatogonia could secrete BMP4 factor into culture medium, the media of MEF, Sertoli cell, spermatogonia, and an immortalised preleptotene spermatocyte cell line GC-2 [46] were collected for Western blotting analysis (Figure 3(f)). The results showed that cultured spermatogonia and GC-2 but not MEF and Sertoli cells could secrete BMP4 protein into the medium.
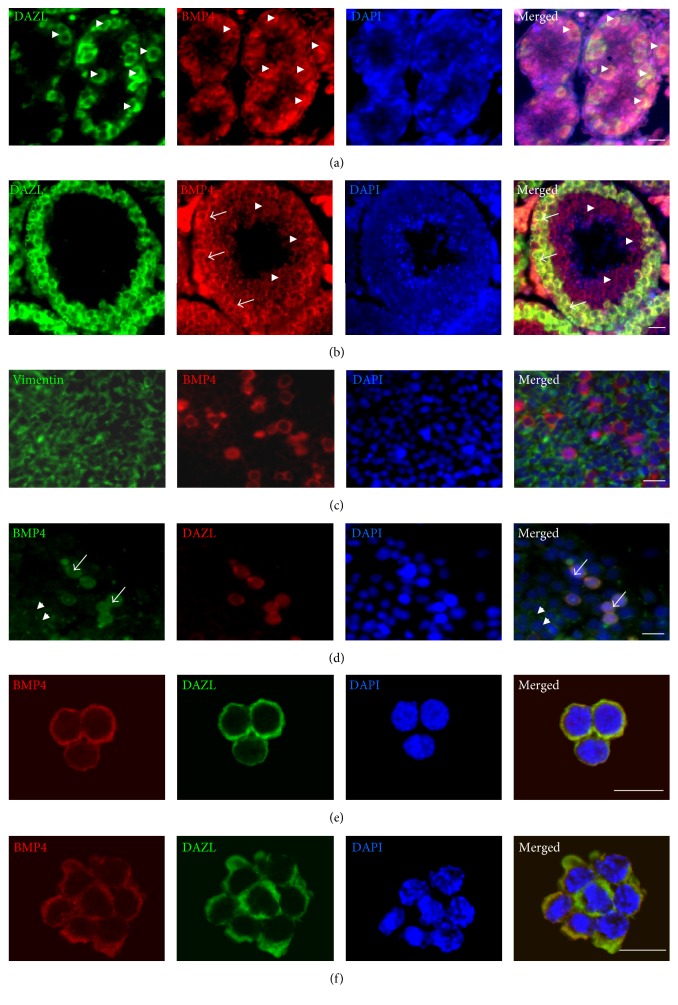
The expression of BMP4 in mouse testis sections, cultured testicular cells, and spermatogonia was subsequently examined by immunofluorescence staining. In 7-day-old mouse testis sections, BMP4 protein was mainly localized in DAZL-positive germ cells (Figure 4(a), arrow head), while, in adult mouse testis sections, BMP4 was predominantly expressed in spermatocytes (Figure 4(b), arrow) and round spermatids (Figure 4(b), arrow head). Surprisingly, in isolated 4-5-day mouse testicular cells, BMP4 was mainly coexpressed in DAZL-positive cells (Figures 4(c) and 4(d), arrow) and to a less extent in Sertoli cells (Figure 4(d), arrow head). BMP4 protein was also expressed in P3 (Figure 4(e)) and P33 (Figure 4(f)) cultured spermatogonia. These results indicate that BMP4 is mainly produced by germ cells in mouse testis.
Figure 4.
BMP4 protein is mainly expressed in mouse germ cells. (a) IFA analysed the localization of BMP4 and DAZL in 7-day mouse testis section (arrow head). (b) In adult mouse testis section, BMP4 was predominantly expressed in spermatocytes (arrow) and round spermatids (arrow head). (c-d) In testicular cells isolated from 4-5-day mice, BMP4 was predominantly expressed in germ cells (arrow) and, to a less extent, in Sertoli cells (arrow head). (e-f) BMP4 was also expressed in P3 (e) and P33 (f) cultured spermatogonia. Scale bar: 20 μm.
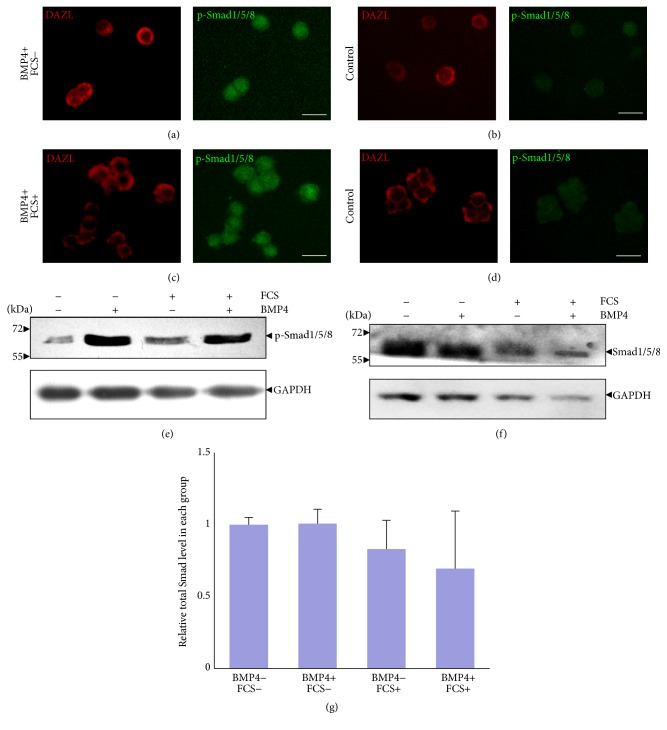
3.4. Cultured Spermatogonia Respond to BMP4 Stimulation with Smad1/5/8 Activation
Previous studies reported that BMPs induce the phosphorylation of R-Smads (Smad1, Smad5, and Smad8) to exert its function [47]. To evaluate the response of cultured spermatogonia to BMP4 stimulation in the current culture system, cells were treated with 100 ng/mL BMP4 factor for 1 hour. Immunofluorescent assay (IFA) revealed that BMP4 could activate and induce nuclear accumulation of phosphorylated Smad1/5/8 in both serum-free (Figures 5(a) and 5(b)) and 15% serum-containing (Figures 5(c) and 5(d)) medium. Western blotting analysis further confirmed the IFA results while the p-Smad1/5/8 level was significantly increased after BMP4 treatment; the total proteins level was not clearly changed when normalized to the internal GAPDH control (Figures 5(e)–5(g)). Together, these results showed the existence of an intact BMP4 signalling pathway in cultured spermatogonia.
Figure 5.
BMP4 activates Smad signalling pathway in cultured spermatogonia. (a-b) IFA analyses of spermatogonia cultured in serum-free medium using antibodies against phosphorylated Smad1, Smad5, and Smad8 in the presence of BMP4 (a) or control (b). (c-d) IFA analysis of spermatogonia cultured in 15% serum-containing medium in the presence of BMP4 (c) or control (d). (e-f) Western blotting analysis of phosphorylated (e) and total (f) Smad1/5/8 in spermatogonia under different culture conditions. (g) Relative total Smad1/5/8 level in each group in (f) after normalization to the internal control. Scale bar: 20 μm.
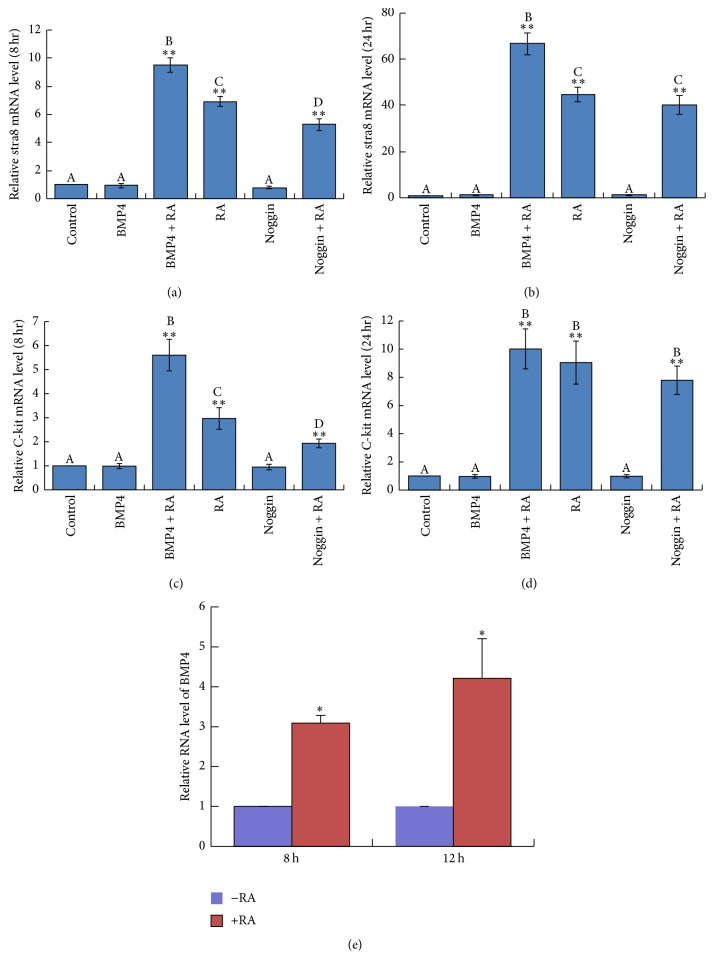
3.5. BMP4 Cooperates with RA in the Induction of Stra8 and c-Kit Expression in Cultured Spermatogonia
We next explored the differentiation-inducing function of BMP4 in cultured spermatogonia. Real-time PCR analyses were first employed to evaluate the expression of Stra8 and c-Kit in these cells treated with BMP4. Unexpectedly, BMP4 treatment for either 24 or 48 hours did not increase the expression of Stra8 and c-Kit in cultured spermatogonia (Figure S3A–D). Since RA is necessary for spermatogonial maturation and entry into meiotic prophase in postnatal testes [48, 49], we then analysed the effect of RA treatment on the expression of these differentiation markers. As anticipated, RA treatment could significantly increase Stra8 and c-Kit expression compared with that in control group (Figures 6(a)–6(d)). Intriguingly, pretreatment of spermatogonia with BMP4 for 24 hours and then stimulation with RA, the expression of Stra8 was significantly increased at 8 and 24 hours compared with the RA only groups (Figures 6(a)-6(b)). Similarly, the expression of c-Kit in the BMP4 plus RA group was also significantly higher than that in the RA only group at 8 hours after RA stimulation (Figure 6(c)). Importantly, pretreatment of spermatogonia with Noggin, a BMP4 antagonist [50, 51], could clearly reduce RA-induced Stra8 (Figure 6(a)) and c-Kit (Figure 6(c)) expression compared with RA only groups at 8 hours after stimulation. Finally, real-time PCR method was employed to evaluate whether RA treatment could alter the expression of BMP4 in cultured spermatogonia (Figure 6(e)). The results showed that BMP4 expression was significantly promoted by RA stimulation. This finding is consistent with the Western blots results in Figure 3(d), which showed that BMP4 is higher in more differentiated germ cells. These results suggest that BMP4 could act cooperatively with RA in inducing the expression of spermatogonial differentiation markers Stra8 and c-Kit.
Figure 6.
BMP4 induces the expression of Stra8 and c-Kit cooperatively with RA in cultured spermatogonia. (a-b) Real-time PCR analysis of Stra8 expression in cultured spermatogonia pretreated with BMP4 or Noggin and followed by RA stimulation for 8 hours (a) or 24 hours (b). (c-d) Real-time PCR analysis of c-Kit expression in cultured spermatogonia pretreated with BMP4 or Noggin and followed by RA stimulation for 8 hours (c) or 24 hours (d). (e) Real-time PCR analysis of BMP4 mRNA expression in cultured spermatogonia followed by RA alone stimulation for 8 hours and 12 hours. The columns were labelled with A, B, C, and D, which means values are significantly different (P < 0.05) among differently labelled groups; ∗ P < 0.05 or ∗∗ P < 0.01.
4. Discussions
Researchers have long dreamed of producing sperm in culture dishes not only to correct certain types of male infertility but also to study the mechanism of spermatogenesis in a more convenient way [52]. There are two major obstacles for the accomplishment of this goal—the proliferation and induced differentiation of SSCs in vitro. The medium for spermatogonial culture described in current standard protocols contained many components, the roles of which have not been fully elucidated [4, 5]. Some studies claimed that the quality of some agents, such as serum, BSA, and lipid, are critical for the success of SSC cultures [5–7, 53]. Unfortunately, there is no guarantee to get the right batches of these agents commercially; therefore quality control of the culture system is troublesome. The serum-free and feeder-free culture system reported recently still uses serum-derived products such as BSA and fetuin, the possible contaminants in which remain as concerns for mechanistic studies and potential applications [8]. Since products from serum are inevitable, we decided to establish a simplified system, which included high concentration serum but not the other components such as BSA and lipids. We used DMEM supplemented with 15% FCS, three growth factors (LIF, GDNF, and bFGF), and some common nongrowth factor components, such as nonessential amino acids, glutamine. This is equivalent to the mouse ESC culture medium supplemented with GDNF and bFGF. Long-term spermatogonial cultures could be routinely established, with a maximum culture period of 33 passages over 6 months. The long-term cultured spermatogonia contained stem cells as indicated by transplantation assays. Most studies use low concentration serum (0.04–1%) for spermatogonial culture [4, 6, 53, 54] and some even report a detrimental effect of serum on SSCs [5, 55] while others claimed the appearance of ESC-like clones in ESC medium containing high concentration serum. Since we were able to culture SSCs with high concentration serum, we conclude that it may be the quality instead of the concentration of serum that determines the success of SSCs culture. Moreover, we never observed any ESC-like colonies during our whole experimental period, suggesting that this reprogramming process is indeed a rare event. In summary, our system is a much simplified one compared with other systems while it is comparable with the others in terms of GDNF dependency, long-term culture period, and the maintenance of stem cell activities.
While several secreted protein factors have been reported to enhance the proliferation of SSCs [4, 5, 56–59], the spermatogonia differentiation-inducing factors have been poorly defined. The expression of BMP4 in testes is still poorly defined. While one study showed that BMP4 mRNAs were detected in Sertoli cells of the 4–7 dpp mice but not in spermatogonia at the same stage, another one showed that it, in adult mouse testis, was predominantly expressed in early stage germ cells, including spermatogonia and early spermatocytes, but absent from Sertoli cells [19, 25]. Hu et al. found that BMP4 mRNA was localized in pachytene spermatocytes and, to a less extent, in other germ cells [26]. In the present study, we confirmed that BMP4 mRNAs are present in germ cells including spermatogonia, spermatocytes, and round spermatids as well as in the somatic Sertoli cells, while the protein was predominantly expressed in adult germ cells and marginally in Sertoli cells. Therefore, the expression of Bmp4 in testicular cells is developmentally regulated and the major cell source changes from Sertoli cells to germ cells, and its low level expression in certain cell types may be neglected by previous studies due to the use of insensitive detecting methods.
The TGF-β superfamily members function as homodimers or heterodimers by binding to heteromeric receptor complexes that contain type I and type II serine-threonine kinase receptors [26]. The study by Pellegrini et al. showed that mRNAs of BMP4 receptors BMPR1A and BMPRII were only detectable in 4- and 7-day-old mouse spermatogonia [25]. In the present study, we detected the expression of BMPR1A and BMPRII at both mRNA and protein levels in neonatal mouse SSCs, adult spermatocytes, and round spermatids. While BMPR1A, BMPRII, ActRII, and ActRIIB mRNAs expression were also detected in 4-5-day-old mouse Sertoli cells, BMPRII but not BMPR1A protein was detected by Western blotting. Pellegrini et al. showed that mRNAs of BMPRIA could not be detected by Northern blotting in the Sertoli cells of 4 dpp mice [25]. It is likely that BMPRIA mRNA level is very low and can only be detected by RT-PCR but not Northern blotting and consequently its protein cannot be detected by Western blotting readily. Taken together, it appears that, in adult mice, BMP4, which is majorly produced by germ cells, executes an autocrine function by binding to its receptor complex on germ cells.
BMP4 is well-documented to be necessary for the generation and survival of PGCs and might therefore be involved in the regulation of spermatogenesis [22, 24, 25, 60]. Whereas BMP4 alone is unable to induce the formation of PGCs, BMP8b is required for BMP4-induced PGC formation in cultured epiblasts [61]. In human endometrial stromal cells, TGF-β cooperates with RA to induce the expression of VEGF [62]. For VAD mouse, retinol, probably by being converted to its active metabolite RA, initiates the resumption of spermatogenesis through the suppression of BMP4 expression in spermatogonia [19]. In the immune system, synergy between RA and TGF-β induced Foxp3+ T cells at least 3 times higher than those induced by TGF-β alone [63]. A previous study also showed that RA and BMP4 synergistically induced the apoptosis of P19 embryonic carcinoma cells [64, 65]. These studies indicate that the cooperative interactions of RA and TGF-β family members are involved in diverse developmental processes.
An important observation in the present study was that BMP4 and RA cooperatively induced the mRNA expression of Stra8 and c-Kit, two genes involved in spermatogonial differentiation and meiosis initiation [66, 67]. One previous study reported that BMP4 treatment of germ cell-enriched cultures from day 4 mouse testes induced increased kinase activity of c-Kit, suggesting an increased protein level of c-Kit [25]. As we were unable to detect an increase in the mRNA level of c-Kit following BMP4 treatment of our cultured mouse SSCs, BMP4 seems to regulate the translation instead of transcription of c-Kit. Our observation that the mRNA levels of c-Kit and Stra8 were upregulated by RA was consistent with the study by Zhou et al. [68]. More importantly, pretreatment of SSCs with BMP4 could increase the mRNA expression of Stra8 and c-Kit to significantly higher levels compared with the RA only group. BMP4 by itself is probably unable to induce spermatogonial differentiation but just prepares the cells to be responsive to other environmental signal(s) such as RA, the production of which is regulated in a rather complex manner in vivo [69, 70]. Otherwise, the SSCs pool could be exhausted shortly after birth because of the differentiation-inducing signals of the autocrine BMP4. The present study offers new insights into understanding the roles of autocrine and environmental factors that regulate the differentiation of SSCs during mammalian spermatogenesis.
Supplementary Material
Supplemental Data Supplemental Data including 4 figures can be found with this article online.
Acknowledgments
The authors thank Dr. Qiang Wang (Institute of Zoology, CAS) for providing antibody against phosphorylated Smad1/5/8. This study was supported by the National Basic Research Program of China (2015CB943002, 2012CB966702, and 2013CB945001) and the National Natural Science Foundation of China (31271379 and 31471349).
Disclosure
Yongguang Yang current address is Department of Cancer Biology, Vontz Center for Molecular Studies, University of Cincinnati College of Medicine, Cincinnati, OH 45267, USA.
Competing Interests
All the authors have declared no conflict of interests.
Authors' Contributions
Yongguang Yang and Yanmin Feng contributed equally to the work.
References
- 1.Russell L. D., Ettlin R. A., Sinha Hikim A. P., Clegg E. D. Mammalian spermatogenesis . In: Russell L. D., Ettlin R. A., Sinha Hikim A. P., Clegg E. D., editors. Histological and Histopathological Evaluation of the Testis. Clearwater, Fla, USA: Cache River Press; 1990. pp. 1–40. [Google Scholar]
- 2.Oatley J. M., Brinster R. L. Spermatogonial stem cells. Methods in Enzymology. 2006;419:259–282. doi: 10.1016/S0076-6879(06)19011-4. [DOI] [PubMed] [Google Scholar]
- 3.Meng X., Lindahl M., Hyvönen M. E., et al. Regulation of cell fate decision of undifferentiated spermatogonia by GDNF. Science. 2000;287(5457):1489–1493. doi: 10.1126/science.287.5457.1489. [DOI] [PubMed] [Google Scholar]
- 4.Kanatsu-Shinohara M., Ogonuki N., Inoue K., et al. Long-term proliferation in culture and germline transmission of mouse male germline stem cells. Biology of Reproduction. 2003;69(2):612–616. doi: 10.1095/biolreprod.103.017012. [DOI] [PubMed] [Google Scholar]
- 5.Kubota H., Avarbock M. R., Brinster R. L. Growth factors essential for self-renewal and expansion of mouse spermatogonial stem cells. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(47):16489–16494. doi: 10.1073/pnas.0407063101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanatsu-Shinohara M., Takehashi M., Shinohara T. Brief history, pitfalls, and prospects of mammalian spermatogonial stem cell research. Cold Spring Harbor Symposia on Quantitative Biology. 2008;73:17–23. doi: 10.1101/sqb.2008.73.033. [DOI] [PubMed] [Google Scholar]
- 7.Kanatsu-Shinohara M., Inoue K., Ogonuki N., Morimoto H., Ogura A., Shinohara T. Serum- and feeder-free culture of mouse germline stem cells. Biology of Reproduction. 2011;84(1):97–105. doi: 10.1095/biolreprod.110.086462. [DOI] [PubMed] [Google Scholar]
- 8.Kanatsu-Shinohara M., Ogonuki N., Matoba S., Morimoto H., Ogura A., Shinohara T. Improved serum- and feeder-free culture of mouse germline stem cells. Biology of Reproduction. 2014;91(4, article 88) doi: 10.1095/biolreprod.114.122317. [DOI] [PubMed] [Google Scholar]
- 9.Kanatsu-Shinohara M., Inoue K., Lee J., et al. Generation of pluripotent stem cells from neonatal mouse testis. Cell. 2004;119(7):1001–1012. doi: 10.1016/j.cell.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Guan K., Nayernia K., Maier L. S., et al. Pluripotency of spermatogonial stem cells from adult mouse testis. Nature. 2006;440(7088):1199–1203. doi: 10.1038/nature04697. [DOI] [PubMed] [Google Scholar]
- 11.Seandel M., James D., Shmelkov S. V., et al. Generation of functional multipotent adult stem cells from GPR125+ germline progenitors. Nature. 2007;449(7160):346–350. doi: 10.1038/nature06129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itman C., Loveland K. L. SMAD expression in the testis: an insight into BMP regulation of spermatogenesis. Developmental Dynamics. 2008;237(1):97–111. doi: 10.1002/dvdy.21401. [DOI] [PubMed] [Google Scholar]
- 13.Hogan B. L. M. Bone morphogenetic proteins: multifunctional regulators of vertebrate development. Genes and Development. 1996;10(13):1580–1594. doi: 10.1101/gad.10.13.1580. [DOI] [PubMed] [Google Scholar]
- 14.Nellen D., Affolter M., Basler K. Receptor serine/threonine kinases implicated in the control of Drosophila body pattern by decapentaplegic . Cell. 1994;78(2):225–237. doi: 10.1016/0092-8674(94)90293-3. [DOI] [PubMed] [Google Scholar]
- 15.Ruberte E., Marty T., Nellen D., Affolter M., Basler K. An absolute requirement for both the type II and type I receptors, punt and thick veins, for Dpp signaling in vivo. Cell. 1995;80(6):889–897. doi: 10.1016/0092-8674(95)90292-9. [DOI] [PubMed] [Google Scholar]
- 16.Weis-Garcia F., Massagué J. Complementation between kinase-defective and activation-defective TGF-β receptors reveals a novel form of receptor cooperativity essential for signaling. The EMBO Journal. 1996;15(2):276–289. [PMC free article] [PubMed] [Google Scholar]
- 17.Han C., Wang Q., Yang Y., Liu H., Shi Y., Liao S. GDNF stimulates sertoli cell proliferation through pathways from NCAM. Biology of Reproduction. 2008;78(1, supplement):p. 186. [Google Scholar]
- 18.Zhou L., Xu M., Yang Y., et al. Activation of β-catenin signaling in CD133-positive dermal papilla cells drives postnatal hair growth. PLoS ONE. 2016;11(7) doi: 10.1371/journal.pone.0160425.e0160425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baleato R. M., Aitken R. J., Roman S. D. Vitamin A regulation of BMP4 expression in the male germ line. Developmental Biology. 2005;286(1):78–90. doi: 10.1016/j.ydbio.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Li Y., Zhang Y., Zhang X., Sun J., Hao J. BMP4/Smad signaling pathway induces the differentiation of mouse spermatogonial stem cells via upregulation of Sohlh2. The Anatomical Record. 2014;297(4):749–757. doi: 10.1002/ar.22891. [DOI] [PubMed] [Google Scholar]
- 21.Neumann J. C., Chandler G. L., Damoulis V. A., et al. Mutation in the type IB bone morphogenetic protein receptor alk6b impairs germ-cell differentiation and causes germ-cell tumors in zebrafish. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(32):13153–13158. doi: 10.1073/pnas.1102311108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawson K. A., Dunn N. R., Roelen B. A. J., et al. Bmp4 is required for the generation of primordial germ cells in the mouse embryo. Genes and Development. 1999;13(4):424–436. doi: 10.1101/gad.13.4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ying Y., Liu X.-M., Marble A., Lawson K. A., Zhao G.-Q. Requirement of Bmp8b for the generation of primordial germ cells in the mouse. Molecular Endocrinology. 2000;14(7):1053–1063. doi: 10.1210/me.14.7.1053. [DOI] [PubMed] [Google Scholar]
- 24.Fujiwara T., Dunn N. R., Hogan B. L. M. Bone morphogenetic protein 4 in the extraembryonic mesoderm is required for allantois development and the localization and survival of primordial germ cells in the mouse. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(24):13739–13744. doi: 10.1073/pnas.241508898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pellegrini M., Grimaldi P., Rossi P., Geremia R., Dolci S. Developmental expression of BMP4/ALK3/SMAD5 signaling pathway in the mouse testis: a potential role of BMP4 in spermatogonia differentiation. Journal of Cell Science. 2003;116(16):3363–3372. doi: 10.1242/jcs.00650. [DOI] [PubMed] [Google Scholar]
- 26.Hu J., Chen Y.-X., Wang D., et al. Developmental expression and function of Bmp4 in spermatogenesis and in maintaining epididymal integrity. Developmental Biology. 2004;276(1):158–171. doi: 10.1016/j.ydbio.2004.08.034. [DOI] [PubMed] [Google Scholar]
- 27.Choi Y. S., Zhang Y., Xu M., et al. Distinct functions for Wnt/β-catenin in hair follicle stem cell proliferation and survival and interfollicular epidermal homeostasis. Cell Stem Cell. 2013;13(6):720–733. doi: 10.1016/j.stem.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bowles J., Knight D., Smith C., et al. Retinoid signaling determines germ cell fate in mice. Science. 2006;312(5773):596–600. doi: 10.1126/science.1125691. [DOI] [PubMed] [Google Scholar]
- 29.Bowles J., Koopman P. Retinoic acid, meiosis and germ cell fate in mammals. Development. 2007;134(19):3401–3411. doi: 10.1242/dev.001107. [DOI] [PubMed] [Google Scholar]
- 30.White J. A., Ramshaw H., Taimi M., et al. Identification of the human cytochrome P450, P450RAI-2, which is predominantly expressed in the adult cerebellum and is responsible for all-trans-retinoic acid metabolism. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(12):6403–6408. doi: 10.1073/pnas.120161397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Pelt A. M. M., De Rooij D. G. The origin of the synchronization of the seminiferous epithelium in vitamin A-deficient rats after vitamin A replacement. Biology of Reproduction. 1990;42(4):677–682. doi: 10.1095/biolreprod42.4.677. [DOI] [PubMed] [Google Scholar]
- 32.van Pelt A. M. M., de Rooij D. G. Synchronization of the seminiferous epithelium after vitamin A replacement in vitamin A-deficient mice. Biology of Reproduction. 1990;43(3):363–367. doi: 10.1095/biolreprod43.3.363. [DOI] [PubMed] [Google Scholar]
- 33.van Pelt A. M. M., van Dissel-Emiliani F. M. F., Gaemers I. C., Van Der Burg M. J. M., Tanke H. J., De Rooij D. G. Characteristics of A spermatogonia and preleptotene spermatocytes in the vitamin A-deficient rat testis. Biology of Reproduction. 1995;53(3):570–578. doi: 10.1095/biolreprod53.3.570. [DOI] [PubMed] [Google Scholar]
- 34.Glozak M. A., Rogers M. B. Specific induction of apoptosis in P19 embryonal carcinoma cells by retinoic acid and BMP2 or BMP4. Developmental Biology. 1996;179(2):458–470. doi: 10.1006/dbio.1996.0275. [DOI] [PubMed] [Google Scholar]
- 35.Glozak M. A., Rogers M. B. Retinoic acid- and bone morphogenetic protein 4-induced apoptosis in P19 embryonal carcinoma cells requires p27. Experimental Cell Research. 2001;268(2):128–138. doi: 10.1006/excr.2001.5281. [DOI] [PubMed] [Google Scholar]
- 36.Rodriguez-Leon J., Merino R., Macias D., Gañan Y., Santesteban E., Hurle J. M. Retinoic acid regulates programmed cell death through BMP signalling. Nature Cell Biology. 1999;1(2):125–126. doi: 10.1038/10098. [DOI] [PubMed] [Google Scholar]
- 37.Anderson E. L., Baltus A. E., Roepers-Gajadien H. L., et al. Stra8 and its inducer, retinoic acid, regulate meiotic initiation in both spermatogenesis and oogenesis in mice. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(39):14976–14980. doi: 10.1073/pnas.0807297105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prabhu S. M., Meistrich M. L., McLaughlin E. A., et al. Expression of c-Kit receptor mRNA and protein in the developing, adult and irradiated rodent testis. Reproduction. 2006;131(3):489–499. doi: 10.1530/rep.1.00968. [DOI] [PubMed] [Google Scholar]
- 39.Ogawa T., Aréchaga J. M., Avarbock M. R., Brinster R. L. Transplantation of testis germinal cells into mouse seminiferous tubules. International Journal of Developmental Biology. 1997;41(1):111–122. [PubMed] [Google Scholar]
- 40.Brinster R. L., Zimmermann J. W. Spermatogenesis following male germ-cell transplantation. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(24):11298–11302. doi: 10.1073/pnas.91.24.11298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brinster R. L., Avarbock M. R. Germline transmission of donor haplotype following spermatogonial transplantation. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(24):11303–11307. doi: 10.1073/pnas.91.24.11303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bellve A. R. Purification, culture, and fractionation of spermatogenic cells. Methods in Enzymology. 1993;225:84–113. doi: 10.1016/0076-6879(93)25009-Q. [DOI] [PubMed] [Google Scholar]
- 43.Yang Y., Han C. GDNF stimulates the proliferation of cultured mouse immature Sertoli cells via its receptor subunit NCAM and ERK1/2 signaling pathway. BMC Cell Biology. 2010;11, article 78 doi: 10.1186/1471-2121-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ruggiu M., Speed R., Taggart M., et al. The mouse Dazla gene encodes a cytoplasmic protein essential for gametogenesis. Nature. 1997;389(6646):73–77. doi: 10.1038/37987. [DOI] [PubMed] [Google Scholar]
- 45.Naughton C. K., Jain S., Strickland A. M., Gupta A., Milbrandt J. Glial cell-line derived neurotrophic factor-mediated RET signaling regulates spermatogonial stem cell fate. Biology of Reproduction. 2006;74(2):314–321. doi: 10.1095/biolreprod.105.047365. [DOI] [PubMed] [Google Scholar]
- 46.Hofmann M.-C., Hess R. A., Goldberg E., Millán J. L. Immortalized germ cells undergo meiosis in vitro. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(12):5533–5537. doi: 10.1073/pnas.91.12.5533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen D., Zhao M., Mundy G. R. Bone morphogenetic proteins. Growth Factors. 2004;22(4):233–241. doi: 10.1080/08977190412331279890. [DOI] [PubMed] [Google Scholar]
- 48.Ghyselinck N. B., Vernet N., Dennefeld C., et al. Retinoids and spermatogenesis: lessons from mutant mice lacking the plasma retinol binding protein. Developmental Dynamics. 2006;235(6):1608–1622. doi: 10.1002/dvdy.20795. [DOI] [PubMed] [Google Scholar]
- 49.Vernet N., Dennefeld C., Guillou F., Chambon P., Ghyselinck N. B., Mark M. Prepubertal testis development relies on retinoic acid but not rexinoid receptors in Sertoli cells. The EMBO Journal. 2006;25(24):5816–5825. doi: 10.1038/sj.emboj.7601447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hiller M., Liu C., Blumenthal P. D., Gearhart J. D., Kerr C. L. Bone morphogenetic protein 4 mediates human embryonic germ cell derivation. Stem Cells and Development. 2011;20(2):351–361. doi: 10.1089/scd.2010.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pachori A. S., Custer L., Hansen D., Clapp S., Kemppa E., Klingensmith J. Bone morphogenetic protein 4 mediates myocardial ischemic injury through JNK-dependent signaling pathway. Journal of Molecular and Cellular Cardiology. 2010;48(6):1255–1265. doi: 10.1016/j.yjmcc.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 52.Yokonishi T., Ogawa T. Cryopreservation of testis tissues and in vitro spermatogenesis. Reproductive Medicine and Biology. 2016;15(1):21–28. doi: 10.1007/s12522-015-0218-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guan K., Wolf F., Becker A., Engel W., Nayernia K., Hasenfuss G. Isolation and cultivation of stem cells from adult mouse testes. Nature Protocols. 2009;4(2):143–154. doi: 10.1038/nprot.2008.242. [DOI] [PubMed] [Google Scholar]
- 54.Ogawa T., Ohmura M., Tamura Y., et al. Derivation and morphological characterization of mouse spermatogonial stem cell lines. Archives of Histology and Cytology. 2004;67(4):297–306. doi: 10.1679/aohc.67.297. [DOI] [PubMed] [Google Scholar]
- 55.Kubota H., Avarbock M. R., Brinster R. L. Culture conditions and single growth factors affect fate determination of mouse spermatogonial stem cells. Biology of Reproduction. 2004;71(3):722–731. doi: 10.1095/biolreprod.104.029207. [DOI] [PubMed] [Google Scholar]
- 56.Oatley J. M., Oatley M. J., Avarbock M. R., Tobias J. W., Brinster R. L. Colony stimulating factor 1 is an extrinsic stimulator of mouse spermatogonial stem cell self-renewal. Development. 2009;136(7):1191–1199. doi: 10.1242/dev.032243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zuping H., Jiji J., Kokkinaki M., Dym M. Nodal signaling via an autocrine pathway promotes proliferation of mouse spermatogonial stem/progenitor cells through Smad2/3 and Oct-4 activation. STEM CELL. 2009;27(10):2580–2590. doi: 10.1002/stem.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang S., Wang X., Wu Y., Han C. IGF-1R signaling is essential for the proliferation of cultured mouse spermatogonial stem cells by promoting the G2/M progression of the cell cycle. Stem Cells and Development. 2015;24(4):471–483. doi: 10.1089/scd.2014.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gu H., Overstreet A.-M. C., Yang Y. Exosomes biogenesis and potentials in disease diagnosis and drug delivery. Nano LIFE. 2014;4(4) doi: 10.1142/s1793984414410177.1441017 [DOI] [Google Scholar]
- 60.Zhang L., Yang Y., Song Y., et al. Nanoparticle delivery systems reduce the reproductive toxicity of docetaxel in rodents. Nano LIFE. 2014;4(4) doi: 10.1142/s1793984414410128.1441012 [DOI] [Google Scholar]
- 61.Ying Y., Qi X., Zhao G. Q. Induction of primordial germ cells from pluripotent epiblast. TheScientificWorldJournal. 2002;2:801–810. doi: 10.1100/tsw.2002.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sidell N., Feng Y., Hao L., et al. Retinoic acid is a cofactor for translational regulation of vascular endothelial growth factor in human endometrial stromal cells. Molecular Endocrinology. 2010;24(1):148–160. doi: 10.1210/me.2009-0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moore C., Sauma D., Morales J., Bono M. R., Rosemblatt M., Fierro J. A. Transforming growth factor-β and all-trans retinoic acid generate ex vivo transgenic regulatory T cells with intestinal homing receptors. Transplantation Proceedings. 2009;41(6):2670–2672. doi: 10.1016/j.transproceed.2009.06.130. [DOI] [PubMed] [Google Scholar]
- 64.Fujita E., Soyama A., Kawabata M., Momoi T. BMP-4 and retinoic acid synergistically induce activation of caspase-9 and cause apoptosis of P19 embryonal carcinoma cells cultured as a monolayer. Cell Death & Differentiation. 1999;6(11):1109–1116. doi: 10.1038/sj.cdd.4400585. [DOI] [PubMed] [Google Scholar]
- 65.Wang Y., Cui H., Yang Y., et al. Mechanism study of gene delivery and expression in PK-15 cells using magnetic iron oxide nanoparticles as gene carriers. Nano LIFE. 2014;4(4) doi: 10.1142/s1793984414410189.1441018 [DOI] [Google Scholar]
- 66.Bowles J., Koopman P. Sex determination in mammalian germ cells: extrinsic versus intrinsic factors. Reproduction. 2010;139(6):943–958. doi: 10.1530/rep-10-0075. [DOI] [PubMed] [Google Scholar]
- 67.Mithraprabhu S., Loveland K. L. Control of KIT signalling in male germ cells: what can we learn from other systems? Reproduction. 2009;138(5):743–757. doi: 10.1530/rep-08-0537. [DOI] [PubMed] [Google Scholar]
- 68.Zhou Q., Li Y., Nie R., et al. Expression of stimulated by retinoic acid gene 8 (Stra8) and maturation of murine gonocytes and spermatogonia induced by retinoic acid in vitro. Biology of Reproduction. 2008;78(3):537–545. doi: 10.1095/biolreprod.107.064337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Endo T., Romer K. A., Anderson E. L., Baltus A. E., de Rooij D. G., Page D. C. Periodic retinoic acid-STRA8 signaling intersects with periodic germ-cell competencies to regulate spermatogenesis. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(18):E2347–E2356. doi: 10.1073/pnas.1505683112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu Q., Hao W., Yang Y., et al. Effects of size and dispersity of microcrystalline celluloses on size, structure and stability of nanocrystalline celluloses extracted by acid hydrolysis. Nano LIFE. 2014;4(4) doi: 10.1142/s1793984414410141.1441014 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Data Supplemental Data including 4 figures can be found with this article online.