Abstract
Objective:
To determine patient and hospital characteristics associated with not providing IV tissue plasminogen activator (tPA) to eligible patients with acute ischemic stroke (AIS) in clinical practice.
Methods:
We performed a retrospective cohort study of patients with AIS arriving within 2 hours of onset to hospitals participating in Get With The Guidelines–Stroke without documented contraindications to IV tPA from April 2003 through December 2011, comparing those who received tPA to those who did not. Multivariable generalized estimating equation logistic regression modeling identified factors associated with not receiving tPA.
Results:
Of 61,698 eligible patients with AIS presenting within 2 hours of onset (median age 73 years, 51% female, 74% non-Hispanic white, median NIH Stroke Scale score 11, interquartile range 6–18), 15,282 (25%) were not treated with tPA within 3 hours. Failure to give tPA decreased over time from 55% in 2003 to 2005 to 18% in 2010 to 2011 (p < 0.0001). After adjustment for all covariates, including stroke severity, factors associated with failure to treat included older age, female sex, nonwhite race, diabetes mellitus, prior stroke, atrial fibrillation, prosthetic heart valve, NIH Stroke Scale score <5, arrival off-hours and not via emergency medical services, longer onset-to-arrival and door-to-CT times, earlier calendar year, and arrival at rural, nonteaching, non–stroke center hospitals located in the South or Midwest.
Conclusions:
Overall, about one-quarter of eligible patients with AIS presenting within 2 hours of stroke onset failed to receive tPA treatment. Thrombolysis has improved dramatically over time and is strongly associated with stroke center certification. Additionally, some groups, including older patients, milder strokes, women, and minorities, may be undertreated.
IV tissue plasminogen activator (tPA) has been demonstrated to improve outcome in select patients with acute ischemic stroke (AIS), and numerous guidelines have promoted its use in the United States.1–6 As a result, IV tPA use has increased dramatically over the past decade, yet approximately one-third of potentially eligible patients are not receiving treatment.7,8 The factors associated with not treating otherwise eligible patients have not been well characterized in a large, national registry reflective of recent clinical practice. We hypothesized that a number of specific patient and hospital factors will be associated with a lower likelihood of treatment with tPA, some of which may be modifiable, leading to improved treatment rates in the future.
Get With The Guidelines (GWTG)–Stroke is an ongoing, voluntary, national registry and quality-improvement initiative. Since its inception in 2003, >1,800 hospitals have entered >2.5 million patient records into the GWTG-Stroke database, and prior reports have demonstrated that the registry is representative of the US population hospitalized for AIS.8–11 Appropriate and efficient use of IV tPA for AIS is a major objective of the GWTG-Stroke initiative, and sites are expected to provide the rationale for nontreatment from a prespecified list of potential contraindications and warnings. We sought to better understand the patient and hospital characteristics associated with not using IV tPA in otherwise eligible patients.
METHODS
Within the GWTG-Stroke dataset, we identified all patients who presented within 2 hours of onset of ischemic stroke and had no documented contraindications to thrombolysis, and we then compared patient- and hospital-level factors for patients who received tPA to those who did not receive tPA. Several previous publications have provided detailed descriptions of the GWTG-Stroke program.12,13 In brief, GWTG-Stroke is a national stroke quality-improvement program available to any hospital in the United States since the beginning in April 2003. Participating hospitals are instructed to collect deidentified patient-level data on clinical and demographic characteristics, diagnostic testing, treatments, the reason for not treating with tPA, adherence to quality measures, and in-hospital outcomes and discharge disposition in consecutive patients hospitalized with stroke. Trained hospital personnel identify patients admitted with stroke prospectively by clinical diagnosis or retrospectively using International Classification of Diseases, Ninth Revision discharge codes. The eligibility of each acute stroke is confirmed at chart review before abstraction, and the specificity of included patients and data accuracy have been demonstrated to be high.14 After abstraction by trained personnel at each hospital, deidentified patient data are entered into the GWTG-Stroke database with the use of a web-based patient management tool (Outcome, A Quintiles Company, Cambridge, MA). Data elements abstracted include patient demographics, medical history and comorbidities, initial brain imaging findings, in-hospital treatment and events, discharge disposition, ambulatory status, and mortality.
Standard protocol approvals, registrations, and patient consents.
All participating institutions were required to comply with local regulatory and privacy guidelines and to secure institutional review board approval if required. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule. The Duke Clinical Research Institute (Durham, NC) served as the data analysis center, and institutional review board approval was granted to analyze aggregate deidentified data for research purposes.
Data.
The GWTG-Stroke dataset was queried to identify all patients admitted with AIS who arrived within 2 hours from the time they were last known well and had no documented contraindications to IV tPA. Over a period extending from April 2003 through December 2011, GWTG-Stroke enrolled 1,138,157 patients admitted with AIS to 1,783 hospitals. In 2009, the American Heart Association/American Stroke Association published a scientific advisory supporting the use of tPA within the 3- to 4.5-hour window, and GWTG-Stroke disseminated this information to participating hospitals and added a new quality measure to monitor patients who presented within 3.5 hours from the onset of stroke symptoms and were treated by 4.5 hours.15 For this analysis, we excluded the 3,422 patients who arrived within 2 hours and were treated with tPA after 3 hours because we were interested in identifying factors associated with failure to treat, not delayed treatment. We also excluded patients with stroke occurring after hospital admission (26,008); patients treated with investigational use of thrombolytics (1,632); those with uncertain time of onset to arrival (598,611) or time of tPA treatment (527); those with time of onset to arrival >2 hours (304,898); patients treated with IV tPA at a non-GWTG hospital before transfer (16,973); patients treated at a site with <10 patients per year (809); and those with missing door-to-CT time, door-to-CT time beyond 2 hours, or door-to-CT-time after tPA treatment (7,558).
Statistical analyses.
Descriptive statistics, including frequency numbers and percentages for categorical variables and medians with interquartile ranges describing the 25th and 75th percentiles for continuous variables, were generated. The relationships between individual patient and hospital characteristics and nontreatment with IV tPA were assessed in univariable analyses with the Pearson χ2 test for categorical variables and Wilcoxon rank-sum test for continuous/ordinal variables. To determine independent factors associated with tPA nontreatment, we performed multivariable logistic regression modeling using a generalized estimating equation to account for hospital clustering. All hospital-level factors were analyzed at the patient level. Because the NIH Stroke Scale (NIHSS) score was missing in a large number of cases (23.9% overall), separate models were constructed with all patients (i.e., including those without NIHSS score) and in only those with NIHSS score documented, given its importance in quantifying stroke severity and predicting outcomes.16 The functional form of continuous variables with tPA treatment was explored with restricted cubic spline plots. The models incorporated all the covariates described in table e-1 at Neurology.org. Patient variables other than NIHSS had <7% missing values and were imputed to the most common category. Models excluded observations with missing hospital characteristics (<2%). For the models that included NIHSS score, we used a categorical variable (0–4, 5–9, 10–14, 15–20, 21+). All hypothesis tests are 2 sided, with values of p < 0.05 considered statistically significant. All analyses were conducted by the GWTG-Stroke statistical analysis center at the Duke Clinical Research Institute (Durham, NC) with SAS software version 9.3 (SAS Institute, Cary, NC).
RESULTS
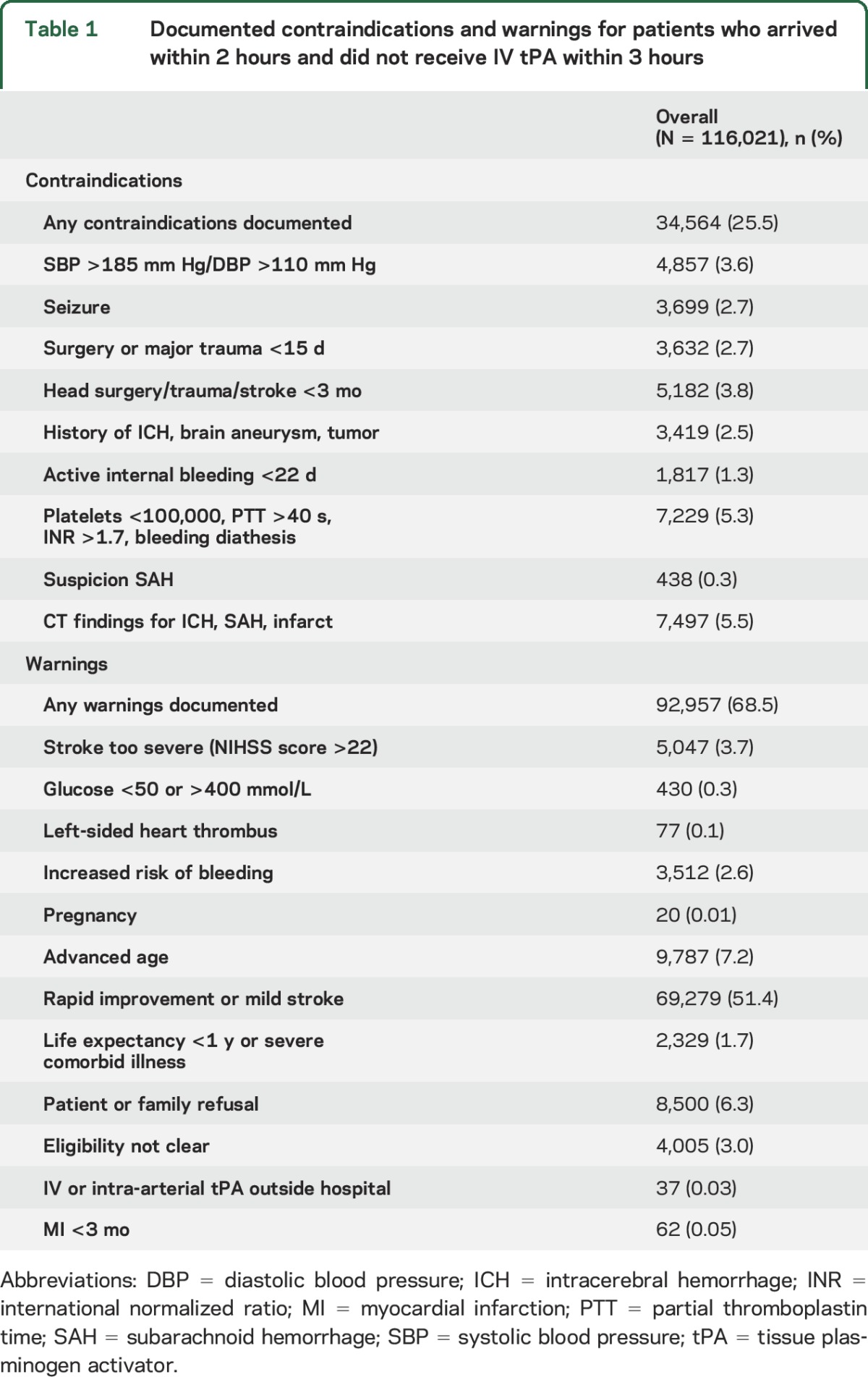
Among the 177,719 patients who arrived within 2 hours of onset and met all other inclusion criteria, 116,021 (65%) had a documented contraindication to or warning for tPA use. As described in table 1, the most common documented reasons for not treating with tPA were mild or rapidly improving symptoms (51%); advanced age (7%); patient or family refusal (6%); CT findings of major infarct signs, intracerebral hemorrhage, or subarachnoid hemorrhage (6%); and platelets <100,000, partial thromboplastin time >40 seconds, international normalized ratio >1.7, or bleeding diathesis (5%). Patient or family refusal did not differ between teaching and nonteaching hospitals, rural and urban locations, hospital sizes, regions of the country, or average annual volumes of stroke patients (p > 0.05 for each).
Table 1.
Documented contraindications and warnings for patients who arrived within 2 hours and did not receive IV tPA within 3 hours
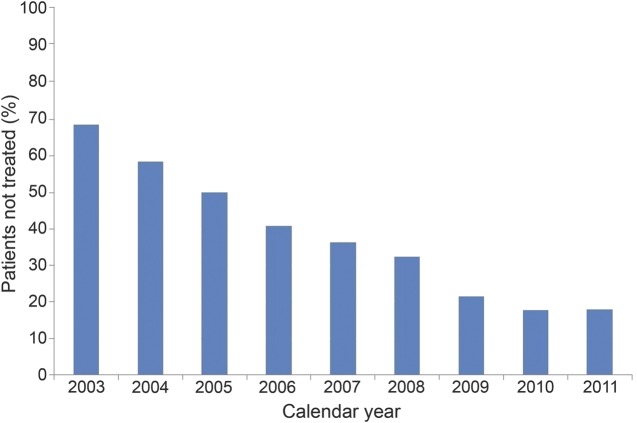
There were 61,698 patients from 1,564 sites eligible for the GWTG-Stroke achievement measure of IV recombinant t-PA arrive by 2 hours with treatment by 3 hours (i.e., patients who had an onset-to-arrival time of ≤120 minutes and did not have any documented IV tPA contraindication or warning), of whom 15,282 (25%) did not receive tPA while the remaining 46,416 (75%) received tPA within 3 hours of onset. Nonuse of tPA among eligible patients decreased over time from 55% in 2003 to 2005 to 18% in 2010 to 2011 (figure).
Figure. Percentage of eligible acute ischemic stroke patients who did not receive IV tissue plasminogen activator, over time.
Table 2 presents the univariable analyses of patient and hospital characteristics of the cohort, overall and dichotomized by treatment with IV tPA. Compared with those treated with tPA, patients not treated with tPA were older, white, and female. They more often had vascular risk factors, including coronary artery disease (CAD), carotid stenosis, diabetes mellitus, hypertension, peripheral vascular disease, a prosthetic heart valve, and prior stroke/TIA, although they were less likely to have atrial fibrillation and to be a smoker. They arrived less frequently by emergency medical services (EMS), experienced a longer delay in door-to-CT time, and more often had an undocumented NIHSS score, and, when measured, their median NIHSS score was lower. Compared with those treated with tPA in the study period, patients not treated with tPA presented to hospitals that had a smaller number of beds, were less often teaching hospitals or Joint Commission–certified primary stroke centers, were more often in the South or Midwest, documented the NIHSS score less frequently overall, and had fewer annual ischemic stroke admissions.
Table 2.
Univariate analysis of patient and hospital characteristics overall and dichotomized by IV tPA treatment


After full adjustment for all covariates, there was no longer an association between white race and higher odds of not being treated; instead, black race and other race were associated with higher odds of not being treated (table 3). Additional patient-specific factors associated with nontreatment included older age, history of carotid stenosis, peripheral vascular disease, diabetes mellitus, CAD/myocardial infarction, stroke/TIA, and presence of a prosthetic heart valve. Method and timing of hospital arrival also were important, with patients with admission during an earlier calendar year, non-EMS arrival, arrival after work hours, or arrival at a longer duration after stroke onset (i.e., last known well time) having lower odds of receiving IV tPA. Several hospital characteristics were also independently associated with not providing tPA at the patient level. Hospitals that documented the NIHSS score less frequently in all patients, were not Joint Commission primary stroke centers or teaching hospitals, had lower annualized volumes of stroke patients, were located in the South or Midwest, or were located in rural locations were less likely to treat eligible patients with IV tPA. A sensitivity analysis using multiple imputation to account for missing data (excluding NIHSS score) found no meaningful differences in these results (table e-2).
Table 3.
Adjusted multivariable logistic regression for selected patient and hospital characteristics associated with nontreatment with IV tPA in acute ischemic stroke patients arriving within 2 hours of onset and without documented contraindications or warnings
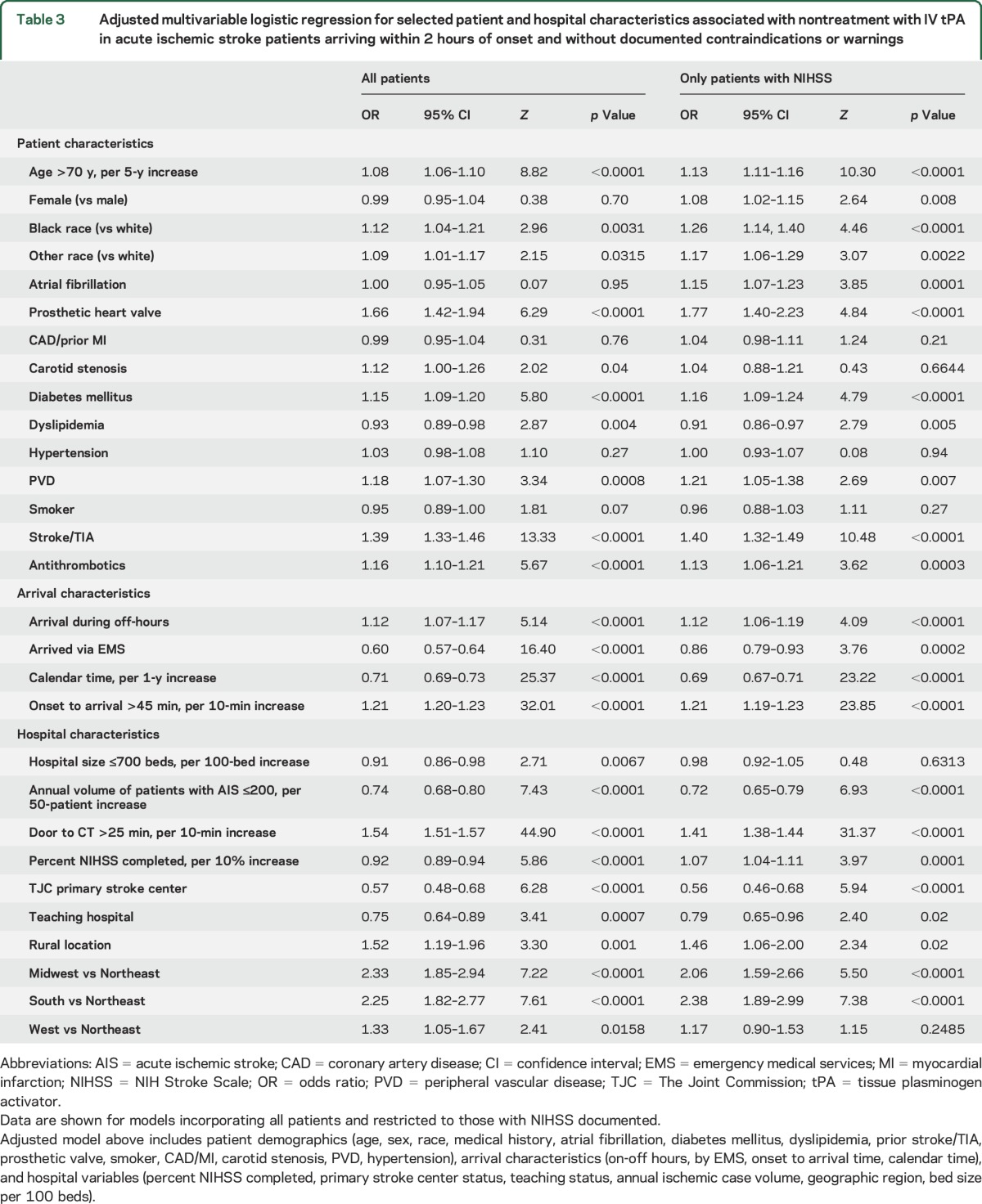
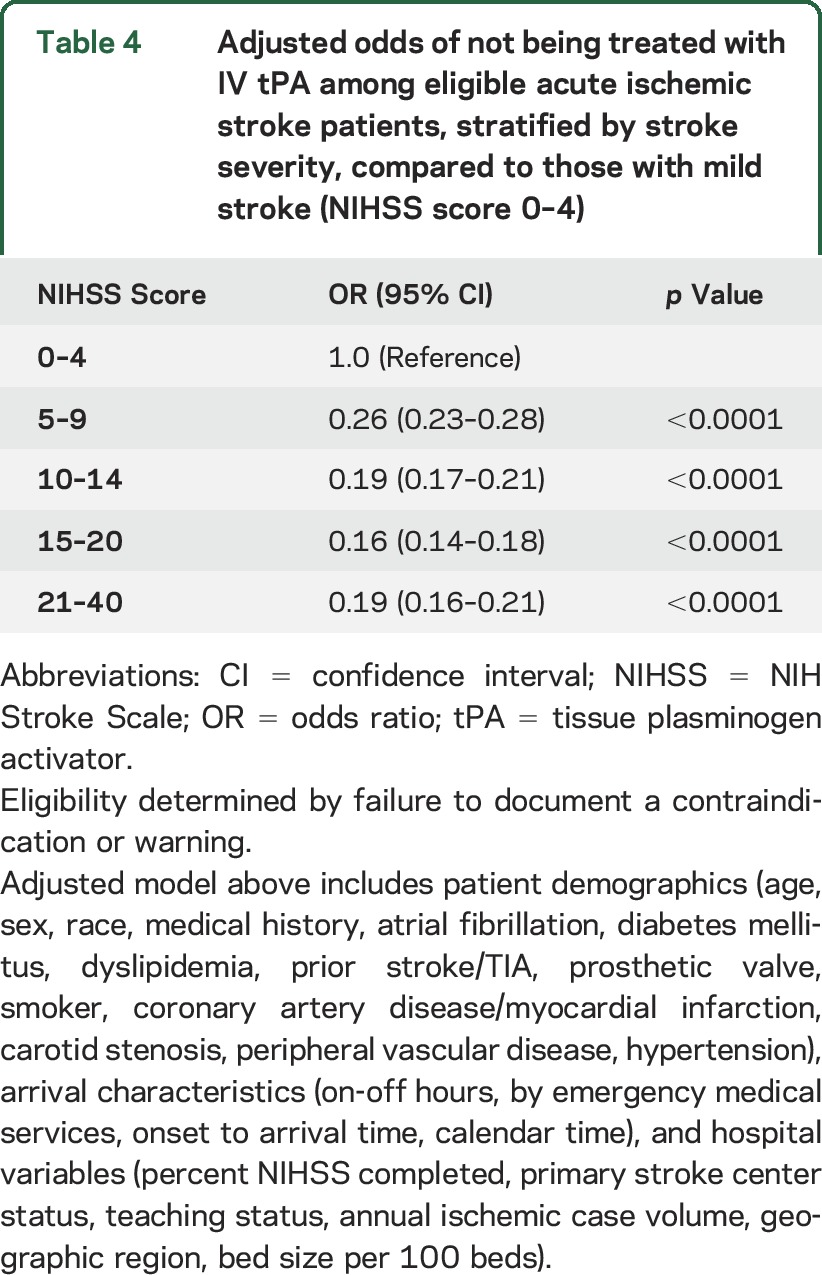
Patients who had a documented NIHSS score had notable differences compared to those who did not have one documented (table e-3). When the model was confined to the 73.5% of patients in whom NIHSS score had been documented, women and patients with atrial fibrillation were less likely to receive IV tPA, and smaller hospital size was no longer significant. Table 4 presents the adjusted odds of being treated with tPA across strata of stroke severity. Compared to those with mild stroke (NIHSS score 0–4), patients with an NIHSS score ≥5 were more likely to receive treatment. Confining the analysis to patients with an NIHSS score ≥5 resulted in no meaningful changes to the findings (table e-4).
Table 4.
Adjusted odds of not being treated with IV tPA among eligible acute ischemic stroke patients, stratified by stroke severity, compared to those with mild stroke (NIHSS score 0–4)
DISCUSSION
As reported in prior studies, tPA treatment in GWTG-Stroke–participating hospitals has increased dramatically over time.8,11 Nevertheless, even recently, up to 1 in 5 potentially eligible patients were not being treated. In this large cohort, several patient and hospital factors were independently associated with a lower likelihood of receiving IV tPA in eligible patients with AIS, many of which may be modifiable. As has been reported previously, treatment at a primary stroke center is one of the strongest predictors of tPA use.17 Thus, to improve thrombolysis rates, continued development of systems of care for stroke should remain a high priority.
Underscoring a statement from the American Heart Association/American Stroke Association calling for an end to inequities in stroke care, we found that after adjustment for stroke severity, minorities and, to a lesser degree, women remained modestly more likely to not receive treatment when tPA eligible.18 These findings are consistent with several prior publications including data from GWTG-Stroke.19–26 Our current study includes more contemporary treatment data and more extensive adjustment for potential known confounders than many prior studies.
In addition to race and sex differences, we found that older patients were less likely to receive tPA treatment despite having no documented contraindication. Again, these findings are consistent with prior analyses.27,28 A recent survey of neurologists reported that 4 of 5 were less likely to administer IV tPA to patients with dementia, and many were less likely to treat patients from nursing homes, with more severe strokes, or >80 years of age.29 Although the benefit to older patients has been uncertain in the past because many were excluded from the early IV tPA trials, the International Stroke Trial 3 (IST3) and recent meta-analyses have demonstrated no upper age limit for benefit of IV tPA.30–33
Several other patient factors were associated with less treatment, including carotid stenosis, peripheral vascular disease, diabetes mellitus, CAD/myocardial infarction, stroke/TIA, and presence of a prosthetic heart valve. These represent opportunities for more targeted education to patients with these risk factors on the need for rapid medical attention and available treatment when stroke symptoms occur. Consistent with prior publications, we found that arrival during off-hours, at later times within 2 hours, or via other modes of transport other than via EMS reduced the odds of treatment.17,18 Multiple hospital characteristics were also independently associated with not receiving tPA, including failure to routinely document the NIHSS score, not being a Joint Commission primary stroke center or a teaching hospital, having a lower annual volume of stroke cases, and being located in the South or Midwest.
This analysis also contributes the description of the prespecified contraindications and warnings that excluded patients from treatment. By far the most common reason cited, reported in more than half of the patients, was mild or rapidly improving symptoms. Among patients without a documented reason for not receiving tPA, mild stroke symptoms, defined as NIHSS score <5, were strongly associated with a lower likelihood of being treated. Prior studies have found that this is the most common reason given for not treating otherwise eligible patients with IV tPA, yet multiple cohorts have found that up to one-third of patients with mild stroke symptoms at presentation will have poor long-term outcomes.34–37 Patients with mild stroke symptoms were largely excluded from prior randomized tPA trials until the IST3 randomized controlled trial of tPA up to 6 hours from symptom onset. Subgroup analysis suggested that patients with mild stroke did not appear to benefit from treatment, although a post hoc analysis restricted to treatment within 3 hours suggested a benefit, and the most recent meta-analysis of tPA studies, including IST3, suggests a potential benefit in mild stroke.32,33,38 It is likely that patients with a low NIHSS score and clearly disabling symptoms such as a visual field deficit or isolated aphasia benefit from tPA. Uncertainty remains about the efficacy of tPA in mild stroke patients (i.e., those with low NIHSS scores and deficits that are not clearly disabling). Phase III trials are underway to test IV tPA in mild stroke patients in the United States (clinicaltrials.gov NCT02072226) and to test IV tenecteplase in patients with TIA or mild stroke with visualized intracranial occlusion in Canada (clinicaltrials.gov NCT02398656).
Many factors independently associated with lack of IV tPA use relate to the rapidity of the evaluation, including arrival via EMS, arrival during regular workday weekday hours, and time from onset to arrival. Thus, patient, family, and medical caregiver education about acute stroke symptoms, the importance of the use of EMS in this setting, and interventions that expedite the evaluation of potentially eligible stroke patients would likely increase treatment rates. A recent study showed that prehospital notification by EMS, taking the patients directly from the ambulance to the CT scanner, and initiating tPA in the CT suite led to a dramatic 42% reduction in door-to-needle times during regular workday hours.39 In the past, treatment times in GWTG-Stroke have been below stated goals, and the Target: Stroke initiative was created to address this issue, resulting in shorter treatment times and clear improvements in survival, patients discharged home, and symptomatic intracerebral hemorrhage.40
The GWTG-Stroke registry is among the largest available datasets of hospitalized stroke patients in the world and represents a mix of academic and nonacademic hospitals of various sizes from all the regions of the United States. The GWTG-Stroke orientation and continuing education for participating centers emphasize the need to document why patients are not receiving treatment. It is representative of the Medicare fee-for-service population with ischemic stroke, and the specificity of included patients and data accuracy have been demonstrated to be high.10,14 However, there are important limitations to this study. First, it is possible that increases in tPA treatment rates may reflect improved documentation of contraindications over time. However, documentation of the rationale for nontreatment with tPA has been a key data point of GWTG-Stroke since its inception, and a prior analysis reported that the percentage of patients with documented contraindications has remained static over time while treatment rates have risen dramatically.41 A related concern is that some factors associated with not treating with IV tPA were in fact associated with failure to document that specific contraindication to treatment. In addition, the effect of time factors may have been underestimated, given that we focused on the GWTG-Stroke quality measure and included only patients who presented within 2 hours of stroke onset. Similarly, we excluded patients who were treated beyond 3 hours of onset because we were focusing on failure to treat. Delays in treatment are a very important topic that we did not assess. In addition, the assignment of race/ethnicity in hospitals may underestimate nonwhite or Hispanic populations and is often not based on interrogation of the patient during emergency visits. Our findings regarding mild stroke defined by low NIHSS score should be interpreted with caution, given the large number of untreated patients missing these data. The data from GWTG-Stroke depend on the accuracy and completeness of clinical documentation, and there are limited data addressing the reliability and data quality in GWTG-Stroke. Finally, residual measured and unmeasured confounding variables may have influenced the findings.
Although tPA rates have increased over the past decade, about one-quarter of eligible patients are not receiving treatment. To improve treatment rates, patients with stroke risk factors and their families should be educated about potential stroke symptoms and encouraged to call EMS if stroke is suspected. Continued efforts to develop stroke systems of care and establish stroke centers, to implement standardized protocols for stroke recognition by EMS dispatchers and providers, and to accelerate triage in emergency departments with an emphasis on rapid brain imaging may also improve treatment rates and timing. Older patients, women, and nonwhites, as well as patients with milder strokes, may be undertreated. Additional studies should be taken to address this potential disparity in care for patients with AIS.
Supplementary Material
GLOSSARY
- AIS
acute ischemic stroke
- CAD
coronary artery disease
- EMS
emergency medical services
- GWTG
Get With The Guidelines
- IST3
International Stroke Trial 3
- NIHSS
NIH Stroke Scale
- TPA
tissue plasminogen activator
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Steven R. Messé, MD: drafting and revising the manuscript, interpreting the data. Pooja Khatri, MD, MSc: study concept, critical revision of the manuscript for important intellectual content. Mathew J. Reeves, PhD, Eric E. Smith, MD, MPH, Jeffrey L. Saver, MD, and Deepak L. Bhatt, MD, MPH: interpreting the data, critical revision of the manuscript for important intellectual content. Maria V. Grau-Sepulveda, MD, MPH, and Margueritte Cox, MS, MGIST: analysis of data. Eric D. Peterson, MD, MPH, and Gregg C. Fonarow, MD: interpreting the data, critical revision of the manuscript for important intellectual content. Lee H. Schwamm, MD: interpreting the data, critical revision of the manuscript for important intellectual content, supervision of the study.
STUDY FUNDING
The GWTG-Stroke program is supported, in part, by unrestricted educational grants to the American Heart Association by Pfizer, Inc (New York, NY) and the Merck‐Schering Plough Partnership (North Wales, PA), which did not participate in the design, analysis, manuscript preparation, or approval.
DISCLOSURE
S. Messé is a member of the GWTG Steering Committee and Stroke Clinical Work Group. He receives modest research support from WL Gore & Associates and significant research support from Glaxo Smith Kline and the NIH. P. Khatri's Department of Neurology receives funding for her research efforts from Genentech (PRISMS Trial Lead principal investigator), Penumbra (THERAPY Trial Neurology principal investigator), and NIH/National Institute of Neurological Disorders and Stroke (StrokeNET regional coordinating center principal investigator and national coordinating center coprincipal investigator). She receives consultation fees from Grand Rounds Experts, Inc and medicolegal work. She has received royalties from UpToDate, Inc (online publication). M. Reeves reports no disclosures relevant to the manuscript. E. Smith reports having received travel expenses and honoraria for lectures and educational activities from the American Heart Association, Alzheimer's Association, and Canadian Conference on Dementia; has served on a Data Safety Monitoring Board for Massachusetts General Hospital; is an assistant editor of Stroke; is a member of the Editorial Board of the Journal of the American Heart Association; and has received research funding from the National Institute of Neurological Disorders and Stroke (R01 NS062028), Canadian Institutes of Health Research, Alberta Innovates–Health Solutions, Canadian Partnership Against Cancer, Heart and Stroke Foundation of Alberta, and the Alzheimer Society of Canada. J. Saver is an employee of the University of California. Dr. Saver has served as an unpaid site investigator in multicenter trials run by Medtronic, Stryker, and Lundbeck, for which the University of California regents received payments on the basis of clinical trial contracts for the number of participants enrolled. Dr. Saver serves as an unpaid consultant to Genentech advising on the design and conduct of the PRISMS trial; neither the University of California nor Dr. Saver received any payments for this voluntary service. The University of California has patent rights in retrieval devices for stroke. Dr. Saver receives funding for services as a scientific consultant regarding trial design and conduct to Medtronic/Covidien, Stryker, Neuravi, BrainsGate, Pfizer, Squibb, Boehringer Ingelheim (prevention only), ZZ Biotech, and St. Jude Medical. D. Bhatt discloses the following relationships: Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Duke Clinical Research Institute, Harvard Clinical Research Institute, Mayo Clinic, Population Health Research Institute; honoraria: American College of Cardiology (senior associate editor, Clinical Trials and News, ACC.org), Belvoir Publications (editor in chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), Harvard Clinical Research Institute (clinical trial steering committee), HMP Communications (editor in chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (guest editor; associate editor), Population Health Research Institute (clinical trial steering committee), Slack Publications (chief medical editor, Cardiology Today's Intervention), Society of Cardiovascular Patient Care (secretary/treasurer), WebMD (CME steering committees); other: Clinical Cardiology (deputy editor), NCDR-ACTION Registry Steering Committee (vice-chair), VA CART Research and Publications Committee (chair); research funding: Amarin, AstraZeneca, Bristol-Myers Squibb, Eisai, Ethicon, Forest Laboratories, Ischemix, Medtronic, Pfizer, Roche, Sanofi Aventis, The Medicines Company; royalties: Elsevier (editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); site coinvestigator: Biotronik, Boston Scientific, St. Jude Medical; trustee: American College of Cardiology; unfunded research: FlowCo, PLx Pharma, Takeda. M. Grau-Sepulveda and M. Cox are employees of the Duke Clinical Research Institute, which serves as the American Heart Association GWTG data coordinating center. E. Peterson reports receiving research grants from Lilly, Johnson & Johnson, Bristol-Myers Squibb, SanofiAventis, and Merck-Schering Plough partnership, and serving as principal investigator of the American Heart Association GWTG data analytic center. G. Fonarow reports serving as a member of the GWTG steering committee; receiving significant research support from the NIH; Patient-Centered Outcomes Research Institute; and being an employee of the University of California, which holds a patent on retriever devices for stroke. L. Schwamm serves as a volunteer for the American Heart Association as chair of the stroke clinical workgroup for GWTG-Stroke and chair of the Healthcare Accreditation Science Committee. He serves as the principal investigator of a National Institute of Neurological Disorders and Stroke–funded SPOTRIAS network trial, MR WITNESS, which is a phase 2 safety study of alteplase delivered in an extended time window with MR-guided patient selection (NC 01282242). The study is funded primarily by the National Institute of Neurological Disorders and Stroke, and alteplase is provided by Genentech to Massachusetts General Hospital for distribution to sites, as well as modest per-patient supplemental site payments. Genentech has no control over study design, analysis, or publication. He reports receiving significant research support from the Patient-Centered Outcomes Research Institute; serving as a stroke systems consultant to the Massachusetts Department of Public Health; and serving as a scientific consultant regarding trial design and conduct to Lundbeck (international steering committee, DIAS3, 4 trial), Medtronic (steering committees REACT AF, STROKE-AF), and Penumbra (data and safety monitoring committee, Separator 3D trial). Go to Neurology.org for full disclosures.
REFERENCES
- 1.rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke: the National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–1587. [DOI] [PubMed] [Google Scholar]
- 2.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317–1329. [DOI] [PubMed] [Google Scholar]
- 3.Wardlaw JM, Murray V, Berge E, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet 2012;379:2364–2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lansberg MG, O’Donnell MJ, Khatri P, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e601S–e636S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870–947. [DOI] [PubMed] [Google Scholar]
- 6.Edlow J, Smith E, Stead L, et al. Clinical policy: use of intravenous tPA for the management of acute ischemic stroke in the emergency department. Ann Emerg Med 2013;61:225–243. [DOI] [PubMed] [Google Scholar]
- 7.Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: a doubling of treatment rates over the course of 5 years. Stroke 2011;42:1952–1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With The Guidelines-Stroke hospitals. Circ Cardiovasc Qual Outcomes 2013;6:543–549. [DOI] [PubMed] [Google Scholar]
- 9.Lin CB, Peterson ED, Smith EE, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. J Am Heart Assoc 2012;1:e002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reeves MJ, Fonarow GC, Smith EE, et al. Representativeness of the Get With The Guidelines-Stroke Registry: comparison of patient and hospital characteristics among Medicare beneficiaries hospitalized with ischemic stroke. Stroke 2012;43:44–49. [DOI] [PubMed] [Google Scholar]
- 11.Messe SR, Fonarow GC, Smith EE, et al. Use of tissue-type plasminogen activator before and after publication of the European Cooperative Acute Stroke Study III in Get With The Guidelines-Stroke. Circ Cardiovasc Qual Outcomes 2012;5:321–326. [DOI] [PubMed] [Google Scholar]
- 12.LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the “Get With The Guidelines” program. Arch Intern Med 2008;168:411–417. [DOI] [PubMed] [Google Scholar]
- 13.Schwamm LH, Fonarow GC, Reeves MJ, et al. Get With the Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation 2009;119:107–115. [DOI] [PubMed] [Google Scholar]
- 14.Xian Y, Fonarow GC, Reeves MJ, et al. Data quality in the American Heart Association Get With The Guidelines-Stroke (GWTG-Stroke): results from a national data validation audit. Am Heart J 2012;163:392–398, 398.e391. [DOI] [PubMed] [Google Scholar]
- 15.Del Zoppo GJ, Saver JL, Jauch EC, Adams HP Jr. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke 2009;40:2945–2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fonarow GC, Saver JL, Smith EE, et al. Relationship of National Institutes of Health Stroke Scale to 30-day mortality in Medicare beneficiaries with acute ischemic stroke. J Am Heart Assoc 2012;1:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fonarow GC, Liang L, Smith EE, et al. Comparison of performance achievement award recognition with primary stroke center certification for acute ischemic stroke care. J Am Heart Assoc 2013;2:e000451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:2091–2116. [DOI] [PubMed] [Google Scholar]
- 19.Johnston SC, Fung LH, Gillum LA, et al. Utilization of intravenous tissue-type plasminogen activator for ischemic stroke at academic medical centers: the influence of ethnicity. Stroke 2001;32:1061–1068. [DOI] [PubMed] [Google Scholar]
- 20.Reed SD, Cramer SC, Blough DK, Meyer K, Jarvik JG. Treatment with tissue plasminogen activator and inpatient mortality rates for patients with ischemic stroke treated in community hospitals. Stroke 2001;32:1832–1840. [DOI] [PubMed] [Google Scholar]
- 21.Giralt D, Domingues-Montanari S, Mendioroz M, et al. The gender gap in stroke: a meta-analysis. Acta Neurol Scand 2012;125:83–90. [DOI] [PubMed] [Google Scholar]
- 22.Towfighi A, Markovic D, Ovbiagele B. Sex differences in revascularization interventions after acute ischemic stroke. J Stroke Cerebrovasc Dis 2013;22:e347–e353. [DOI] [PubMed] [Google Scholar]
- 23.Nasr DM, Brinjikji W, Cloft HJ, Rabinstein AA. Racial and ethnic disparities in the use of intravenous recombinant tissue plasminogen activator and outcomes for acute ischemic stroke. J Stroke Cerebrovasc Dis 2011;22:154–160. [DOI] [PubMed] [Google Scholar]
- 24.Reeves M, Bhatt A, Jajou P, Brown M, Lisabeth L. Sex differences in the use of intravenous rt-PA thrombolysis treatment for acute ischemic stroke: a meta-analysis. Stroke 2009;40:1743–1749. [DOI] [PubMed] [Google Scholar]
- 25.Reeves MJ, Fonarow GC, Zhao X, Smith EE, Schwamm LH. Quality of care in women with ischemic stroke in the GWTG program. Stroke 2009;40:1127–1133. [DOI] [PubMed] [Google Scholar]
- 26.Schwamm LH, Reeves MJ, Pan W, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation 2010;121:1492–1501. [DOI] [PubMed] [Google Scholar]
- 27.Hills NK, Johnston SC. Why are eligible thrombolysis candidates left untreated? Am J Prev Med 2006;31:S210–S216. [DOI] [PubMed] [Google Scholar]
- 28.Rost NS, Smith EE, Pervez MA, Mello P, Dreyer P, Schwamm LH. Predictors of increased intravenous tissue plasminogen activator use among hospitals participating in the Massachusetts Primary Stroke Service Program. Circ Cardiovasc Qual Outcomes 2012;5:314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shamy MC, Jaigobin CS. The complexities of acute stroke decision-making: a survey of neurologists. Neurology 2013;81:1130–1133. [DOI] [PubMed] [Google Scholar]
- 30.Mishra NK, Ahmed N, Andersen G, et al. Thrombolysis in very elderly people: controlled comparison of SITS International Stroke Thrombolysis Registry and Virtual International Stroke Trials Archive. BMJ 2010;341:c6046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mishra NK, Diener HC, Lyden PD, Bluhmki E, Lees KR. Influence of age on outcome from thrombolysis in acute stroke: a controlled comparison in patients from the Virtual International Stroke Trials Archive (VISTA). Stroke 2010;41:2840–2848. [DOI] [PubMed] [Google Scholar]
- 32.Sandercock P, Wardlaw JM, Lindley RI, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the Third International Stroke Trial [IST-3]): a randomised controlled trial. Lancet 2013;379:2352–2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001;56:1015–1020. [DOI] [PubMed] [Google Scholar]
- 35.Kleindorfer D, Kissela B, Schneider A, et al. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: a population-based study. Stroke 2004;35:e27–e29. [DOI] [PubMed] [Google Scholar]
- 36.Khatri P, Conaway MR, Johnston KC. Ninety-day outcome rates of a prospective cohort of consecutive patients with mild ischemic stroke. Stroke 2011;43:560–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith EE, Abdullah AR, Petkovska I, Rosenthal E, Koroshetz WJ, Schwamm LH. Poor outcomes in patients who do not receive intravenous tissue plasminogen activator because of mild or improving ischemic stroke. Stroke 2005;36:2497–2499. [DOI] [PubMed] [Google Scholar]
- 38.Khatri P, Tayama D, Cohen G, et al. Effect of intravenous recombinant tissue-type plasminogen activator in patients with mild stroke in the Third International Stroke Trial-3: post hoc analysis. Stroke 2015;46:2325–2327. [DOI] [PubMed] [Google Scholar]
- 39.Meretoja A, Weir L, Ugalde M, et al. Helsinki model cut stroke thrombolysis delays to 25 minutes in Melbourne in only 4 months. Neurology 2013;81:1071–1076. [DOI] [PubMed] [Google Scholar]
- 40.Fonarow GC, Zhao X, Smith EE, et al. Door-to-needle times for tissue plasminogen activator administration and clinical outcomes in acute ischemic stroke before and after a quality improvement initiative. JAMA 2014;311:1632–1640. [DOI] [PubMed] [Google Scholar]
- 41.Reeves MJ, Grau-Sepulveda MV, Fonarow GC, Olson DM, Smith EE, Schwamm LH. Are quality improvements in the Get With The Guidelines: Stroke program related to better care or better data documentation? Circ Cardiovasc Qual Outcomes 2011;4:503–511. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.