Summary
Background
Obesity is increasing in prevalence and placing an ever‐greater burden on individuals and healthcare resources alike. Obesity management is complex and, for many, elusive.
Aims and methods
This paper reviews the major factors that influence psychological well‐being in individuals with obesity and describes the means by which their impact on distress and other aspects of quality of life (QoL) can be quantified. The goal is to enable healthcare providers to set reasonable, achievable, maintainable weight loss targets that will improve the psychological well‐being and QoL of individuals living with obesity. PubMed and Web of Science searches were conducted to identify literature that addresses the key question: How can distress over obesity be measured and taken into account when tailoring weight loss interventions for a particular patient?
Discussion and conclusions
‘Distress over obesity’ is a key parameter that illustrates the psychological consequences of excess weight. Healthcare providers can draw on a range of obesity‐specific and non‐specific assessment tools to quantify distress as well as the other contributions of obesity to QoL and mental/emotional health. When physicians consider the psychological/QoL aspects of obesity and how these change with successful weight loss, it becomes possible to set achievable, realistic weight loss goals and develop a manageable plan to achieve them. Any future developments that make it easier to achieve these goals should be made widely available to all patients in need, in order to help them turn a vicious cycle of failure into a virtuous cycle of success.
Review criteria
PubMed searches were conducted for papers relating to distress over obesity, quality of life scales and the QoL/psychological impact of weight loss interventions. Forward searches on key papers were conducted through Web of Science.
With preference given to peer‐reviewed, randomised trial data, literature was selected to answer the key question: How can distress over obesity be measured and taken into account when tailoring weight loss interventions for a particular patient?
Message for the clinic
In order to set achievable, realistic goals and develop a manageable plan to achieve them, physicians should evaluate and consider patients’ distress over obesity and expectations about weight loss and associated QoL changes.
Introduction
Obesity: a growing health concern
Obesity is rapidly becoming one of the most important health concerns in developed countries worldwide. In Canada, the proportion of adults meeting the accepted criterion for obesity [Body mass index (BMI) ≥ 30 mg/m2] has more than doubled over the past 40 years, from 10% in 1970 to 26% in a 2009/2011 survey 1. Similar increases in rates of overweight and obesity (‘abnormal or excessive fat accumulation that may impair health’) have been observed in other industrialised countries 2.
The increasing prevalence of obesity places significant burdens on individuals and healthcare systems. Obesity is a risk factor for numerous medical conditions, including endocrine/metabolic disorders, certain cancers and cardiovascular disease 3, 4. More than half of cases of type 2 diabetes and more than a third of pulmonary embolisms are attributed to obesity, as are many cases of gallbladder disease, colorectal and pancreatic cancers, osteoarthritis and chronic back pain 3.
As a result of the primary effects of obesity and the health impact of these comorbidities, overall and cause‐specific mortality increases with BMI in the obese range. Meta‐analysis of prospective studies from North America and Western Europe suggests that a BMI between 30 and 45 confers a 2‐ to 10‐year decrease in life expectancy; individuals with a normal BMI had almost an 80% chance of living to age 70, compared with ~60% with BMI 35–40, and ~50% with BMI 40–50. Much of this excess mortality was attributable to obesity‐related complications including vascular causes, diabetes, and kidney or liver disease 5. Clearly, the management of obesity is of great clinical importance.
In addition to its clear clinical effects, obesity carries a substantial burden in personal terms, as measured by reduced daily functioning, and by general, health‐related and obesity‐specific quality‐of‐life (QoL) metrics. Individuals living with obesity are subject to considerable stigma, which they may internalise and experience as shame, depression and anxiety 6, 7. As argued below, patient affect is intimately connected to the success or failure of weight loss interventions and therefore needs to be acknowledged by clinicians and dealt with as part of a weight management programme. Here, I focus on one crucial dimension of this psychological burden, namely distress over obesity, which should be understood as the degree to which an individual is concerned and unhappy about his/her body and the impact of excess weight. I also introduce tools for evaluating a patient's experience of distress and offer suggestions about effective use of these tools in the clinical setting.
Obesity management means behaviour change
As obesity is a chronic and often progressive condition, its management requires long‐term behavioural change 8, 9, 10. Indeed, for all obesity intervention strategies (i.e. behavioural interventions, medication and surgery), an individual's commitment to new habits and practices is crucial to success. Behavioural intervention requires the individual to implement new behaviours and maintain them after initial weight loss is achieved 8, 10. Maintenance of behaviour change continues to be an issue even when other strategies are introduced. Currently available pharmacological treatments generally do not stand alone, but are used as part of an integrated strategy that includes behaviour change 11, 12. Medication adherence is a key behaviour that determines treatment success. Indeed, even with bariatric surgery, long‐term success in maintaining weight loss is influenced by behaviour postsurgery (e.g. emotional eating), and, in some cases, by the steps taken ahead of surgery to prepare for the procedure 13, 14. Thus, in all cases, it is essential to help the patient adopt the new behaviours (e.g. healthy eating, physical activity, medication adherence, protein supplementation following surgery) as part of their normal routine 8. Both in primary and specialty care, these efforts should be tailored to the patient's strengths and barriers, with a clear understanding of the distress that he or she experiences as a result of obesity.
Methods
Literature on psychological and behavioural issues in obesity treatment was queried using the following PubMed search terms: “distress over obesity”, “psychological/behavioural/social mediators of obesity”, “obesity‐specific quality of life scale” and the major weight management strategies (surgical, behavioural modification, pharmacological) along with “QoL” or “psychological impact”. For key papers, a forward search was conducted through Web of Science to identify additional literature building on relevant concepts.
Obesity and psychological health – a complex, bidirectional relationship
Psychological, social and behavioural mediators of obesity
The relationship between excess weight and psychological well‐being is complex, encompassing physical, social and psychological factors (Figure 1) 15. Furthermore, this relationship is bidirectional: living with obesity impairs QoL and increases the risk of psychiatric and affective disorders; conversely, patients with psychological troubles may become obese as a medication side effect and/or because they use food as a coping strategy 15, 16, 17, 18, 19, 20. Many individuals living with obesity experience self‐blame, low self‐esteem, and general negativity towards themselves and their situation 15. Managing distress over obesity has the potential to directly improve QoL and indirectly affect health behaviours such as treatment adherence. For this reason, distress should not be regarded as strictly a matter of mental health, but rather as a critical factor in successful long‐term weight management.
Figure 1.
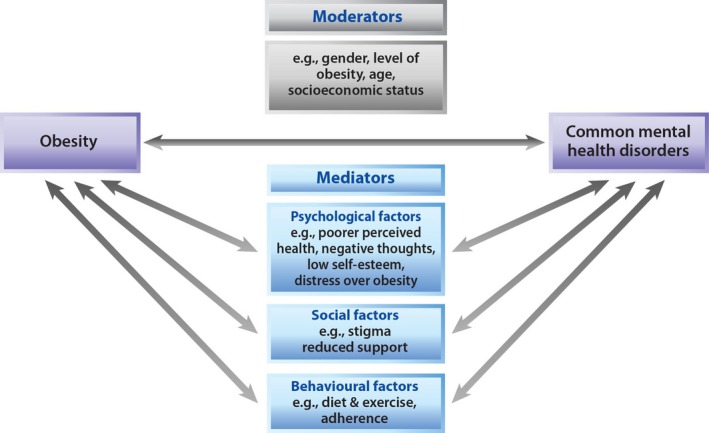
A model of the moderating and mediating psychological factors that contribute to the relationship between obesity and well‐being (Adapted from Gatineau and Dent 15)
The social aspects of obesity play important roles in distress over obesity. One of the most damaging is stigma, which in many cases is both external (i.e. stemming from others) and self‐directed. Pervasive negative attitudes towards people who are obese pose a significant challenge to individuals’ access to employment, education, social opportunities and healthcare 6. Many individuals living with obesity internalise these feelings of stigmatisation and feel shame or distress about their own size and habits; this can contribute to low self‐esteem, impaired work and social life, and diminished overall psychological well‐being 21.
Behaviours strongly tied to psychological and motivational attitudes also have a significant impact on weight loss outcomes. Many individuals with obesity get stuck in a cycle of ‘yo‐yo dieting,’ where any weight lost with a given intervention is soon regained. This cycle can be mediated for many by the distress associated with not achieving either the desired amount of weight loss or the desired body shape 22. These experiences often colour the patients’ attitudes towards and persistence with any future management strategies 9, especially as QoL may ‘yo‐yo’ along with weight 23. For individuals with obesity‐related conditions causing pain or mobility restrictions (e.g. osteoarthritis, cardiovascular disease, chronic back or joint pain), physical disability may contribute to a vicious cycle of inactivity, depressed mood and further weight gain 19, 24, 25.
Distress over obesity: a key mediator to appreciate and quantify
Distress over obesity is both a contributor to and a result of obesity, influences self‐esteem and the individual's motivation to initiate and maintain behavioural changes 21, 26, 27. As a general principle, it would be prudent for healthcare providers to assess the degree of negative impact of living with obesity on psychological functioning. Physicians can choose scales based on the relevance of the content of the scales (e.g. psychological distress vs. functional interference) to the clinical context.
In particular, scales that evaluate distress over obesity can contribute valuable insight into patients’ emotional experience of their condition and how it could motivate them to initiate and maintain change. A diverse set of scales can be used to evaluate the impact of obesity on patient function and QoL (Table 1), some designed specifically for use in people with obesity and/or studied and validated in this patient population. Of these, two validated tools are particularly useful for gauging distress over obesity and are brief and easily introduced into clinical care.
Table 1.
Scales for evaluating QoL in patients with obesity
| Scale | Reference | Key parameters measured |
|---|---|---|
| Scales incorporating measures of distress over obesity | ||
| Obesity Adjustment Survey (OAS) | Butler et al. 26 | Distress over obesity |
| Obesity‐related Coping (OCQ) and Obesity‐related Distress (ODQ) questionnaires | Ryden et al. 70 | Distress over obesity, coping mechanisms |
| Impact of Weight on QoL, short version (IWQOL‐Lite) | Kolotkin et al. 30 | Five domains: physical function, self‐esteem, sexual life, public distress, work |
| Quality of Life, Obesity and Dietetics (QOLOD) | Ziegler et al. 34 | Based on IWQOL‐Lite, with questions added specific to French culture and experiences |
| Laval Questionnaire | Therrien et al. 33 | Six domains: symptoms, activity/mobility, personal hygiene/clothing, emotions, social interactions (including public distress), sexual life |
| Scales assessing other aspects of psychosocial well‐being related to obesity | ||
| LEWIN‐TAG questionnaire | Mathias et al. 71 | Wide range of global and obesity‐specific domains |
| Obesity‐specific QoL instrument (OSQOL) | Le Pen et al. 72 | Four domains: physical state, vitality, social interactions, psychological state |
| Bariatric Analysis and Reporting Outcome System (BAROS) | Oria et al. 73 | Developed specifically for bariatric surgery patients; QoL dimensions include self‐esteem and daily activities |
| Obesity‐related Well‐being Questionnaire (ORWELL 97) | Mannucci et al. 74 | Psychological status, social adjustment, physical symptoms |
| Obesity and Weight‐loss QoL questionnaire (OWLQOL) and Weight‐related Symptom Measure (WRSM) | Niero et al. 75 | Two questionnaires intended to be used together to measure presence and impact of obesity symptoms on QoL |
| Obesity‐related Problems Scale (OP) | Karlsson et al. 76 | Psychosocial functioning |
| Moorehead–Ardelt QoL instrument (MAQOL) | Moorehead et al. 77 | Six domains: self‐esteem, physical well‐being, social relationships, work, sexuality, eating behaviour |
| Health‐related QoL (HRQL) | Mathus‐Vliegen et al. 50 | General well‐being, health distress, depression, self‐esteem, physical activities, social activities |
| BQL | Weiner et al. 78 | Developed specifically for bariatric surgery patients; includes QoL and symptom‐related scales |
| Weight Bias Internalization Scale (WBIS) | Hilbert et al. 79 | Assesses extent to which patient has internalised weight‐related stigma |
| Bariatric and Obesity‐Specific Survey (BOSS) | Tayyem et al. 80 | Developed specifically for bariatric surgery patients; six domains: incapacity, work and well‐being, social function, appearance and health, eating patterns, sexual health |
The Obesity Adjustment Survey (OAS) is a brief questionnaire designed for use in primary and specialist care to focus specifically on an individual's level of distress over obesity (Table 2). This tool was developed and validated in a morbidly obese population [either ≥100 lbs (45 kg) over ideal weight or 100% over ideal weight)], and can assess individuals’ overall distress levels at any point. When used to track QoL impacts of interventions 26, the tool's value is most evident in management. For instance, asking a patient to complete the OAS provides valuable information that the physician can share with the patient. Educating the patient about distress over obesity and supporting the patient in pursuing methods to achieve a healthier weight and address issues of obesity distress enables the physician to apply the self‐management support perspective – the dominant model in chronic disease management 28. As exemplified by large‐scale campaigns such as Dove's Campaign for Real Beauty and Movement for Self‐Esteem 29, a patient with low self‐esteem can be encouraged to resist comparing herself to societal norms.
Table 2.
The 20 items of the Obesity Adjustment Survey, Short Form (OAS‐SF)
| 1. I am so unhappy that I am too big to exercise as I would like to |
| 2. I avoid showing my body to my partner or close friend |
| 3. I cannot walk even short distances without becoming short of breath and getting very tired |
| 4. I do not avoid public situations like going to stores, parties, or the beach because of my present weight |
| 5. If I stay at the weight I am now, I will probably die sooner than if I weighed less |
| 6. Walking up stairs is especially difficult at my present weight |
| 7. My partner (or close friend) doesn't understand what I go through being overweight |
| 8. I always find a way to eat my favourite foods |
| 9. I avoid looking at my body in a full‐length mirror because of my present weight |
| 10. I hate the appearance of my body |
| 11. I believe that being at my present weight is one of the worst things that could happen to me |
| 12. My present weight prevents me from doing social activities that I would enjoy |
| 13. My present weight prevents me from moving around freely |
| 14. I feel more comfortable around people who are overweight than those who are not |
| 15. My sex life would be a lot better if I lost weight |
| 16. I am fat and ugly |
| 17. I am disgusted by my fascination with food |
| 18. I believe that being at my present weight is a sign of personal weakness |
| 19. It is depressing to be at my present weight |
| 20. As a child, I was very inactive and avoided sports or exercise at school |
Items are scored on a 5‐point Likert scale where 1 = not at all true, 2 = a little bit true, 3 = somewhat true, 4 = moderately true, 5 = extremely true. Items 1, 4, and 17 are reverse scored. Permission from Butler et al. 26.
A second tool, the IWQOL‐Lite (Impact of Weight on Quality of Life‐Lite), also incorporates a measure of distress over obesity. The IWQOL and IWQOL‐Lite have been validated in an overweight population and are commonly used in trials of weight loss interventions to assess public distress, as well as physical functioning, self‐esteem, sexual life and work life 30, 31. Their validity and applicability in patients with comorbid psychiatric disorders have also been established 32. Elements of the IWQOL – including assessment of public distress – have also been incorporated in other obesity‐specific QoL tools, including the Laval Questionnaire 33 from Canada and the QOLOD scale 34 from France. A systematic review of obesity‐specific QoL scales can be found in Stucki et al. 35.
It bears mentioning that there are many other QoL scales that provide an overall snapshot of psychological well‐being, not tied to obesity or other particular conditions. Some such non‐specific scales (e.g. the SF‐36 36 and the Beck Depression Inventory 37) have been validated in obese populations. Although they are not designed to highlight drivers of obesity‐related distress 31, these more general scales can be useful in screening for psychopathology or overall QoL. In such circumstances, if a person were to be screened as a ‘case’, the physician would need to explore the extent to which obesity determines or contributes to the symptoms identified.
Qualitative patient research
Additional insights into the lived experience of obesity can be gained through studies that take a qualitative approach to describing patients’ experiences in living with obesity. In this area, the DAWN/DAWN2 (Diabetes Attitudes, Wishes, and Needs) studies in individuals with type 1 and type 2 diabetes may serve as a useful model 38, 39. These studies collected patients’ self‐reports regarding their levels of diabetes self‐management, their experiences of distress in dealing with their condition, the quality of their relationships with healthcare providers and their satisfaction with treatment. Study populations included a high proportion of individuals with type 2 diabetes, most of whom were overweight or obese 8. In the Canadian arm of DAWN2, over 80% of obese respondents reported feeling very anxious about their weight; high levels of concern over weight were associated with lower self‐rated health, more diabetes‐related distress, poorer psychological well‐being and higher rates of psychological treatment compared with patients who were not distressed about their weight 40. Significant negative correlations were found between BMI and all QoL indicators, including self‐reported health status (EQ‐5D VAS), overall QoL (WHO‐QOL‐BREF) and psychological well‐being (WHO‐5). The questions and themes explored in DAWN/DAWN2 and the preliminary findings in the subpopulation of overweight respondents provide a framework that could easily be extended to the general population of individuals living with obesity, to provide a more comprehensive picture of the psychosocial implications of excess weight – in particular, psychosocial factors including distress over obesity, and the impact of weight management interventions on psychological well‐being.
Obesity management in clinical practice
Impact of weight management strategies on distress over obesity
As excess weight can have a significant and multi‐faceted impact on psychological well‐being, interventions leading to or helping maintain weight loss can improve various aspects of QoL. In trials of surgical and non‐surgical methods, weight loss is associated with improvements in overall scores for validated QoL instruments (e.g. SF‐36, IWQOL‐Lite) and in key subscales related to physical well‐being and public distress 13, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51. Behavioural interventions and bariatric surgery have also been shown to moderate distress over obesity along with depressive symptoms 13, 46, 47, 51.
The relationship between weight management and the key psychological parameter of distress over obesity is particularly illuminating, in that it has evolved along with our understanding of how best to assess the impact of obesity on patients’ psychological well‐being. In the past, patients with the greatest psychological burden (obesity‐related and otherwise) were specifically excluded from surgical and behavioural treatment 52, 53. The introduction of QoL scales specific to the concerns and circumstances of the obese population has allowed us to broadly stratify subjects into three groups (high, moderate or poor functioning) and compare outcomes after surgical or other management. We now know that baseline distress level does not affect the degree of weight loss achieved with bariatric surgery, and that patients in the most distressed group can see a normalisation of their distress scores to levels similar to those in higher functioning groups 48. The exclusion of patients with lower function at baseline was therefore based on a misunderstanding, and we now appreciate that obesity treatment should not be withheld because of psychological burden; indeed, doing so can be considered a form of obesity bias.
Limitations of the ‘minimally clinically important difference’
The relationship between the degree of weight loss and improvements in QoL (including psychological well‐being) is a subject of considerable debate. While some studies have suggested that the relationship is linear, in that a greater amount of lost weight yields a greater improvement in psychological well‐being 44, other analyses have found that surgical and non‐surgical interventions can produce QoL benefits, regardless of the degree of weight loss 46, 47. In particular, interventions that incorporate cognitive–behavioural strategies appear to improve depressive symptoms independently of weight loss, by encouraging self‐acceptance and self‐esteem 47.
The question of how much weight patients need to lose in order to experience improvements in psychological well‐being has been further complicated by a recent analysis 54. For many of the available QoL scales, the developers have calculated a ‘minimal clinically important difference’ score (MCID) – that is, the number of points of improvement (or deterioration) on a particular scale that a patient would have to experience to show a noticeable change in QoL. A recent study sought to define how much weight individuals living with obesity would have to lose to achieve these predefined MCIDs on the IWQOL‐Lite and several non‐obesity‐specific QoL scales. The findings showed that in order to achieve a clinically significant change, as defined by the MCIDs, subjects had to lose anywhere from 9% to 25% of their starting weight, depending on the QoL scale used. This degree of weight loss was routinely achieved over the 2‐year study by patients undergoing bariatric surgery, but seldom by those who underwent behavioural/diet counselling only 54. However, it should be noted that the only obesity‐specific scale evaluated was the IWQOL‐Lite and the scores on its subscales were not analysed; this could have masked important effects on specific concerns such as public distress. The MCIDs for the general QoL instruments have been calculated primarily in chronic medical conditions, where physical symptoms are treated with specific medications and a direct link can usually be made between the treatment effect (i.e. symptom relief) and QoL. Conversely, the links between obesity interventions, weight loss and psychological effects are more complex and indirect, and it is possible to improve self‐image and outlook independently of weight loss. For all these reasons, it is likely that the extent of weight loss required to achieve an ‘important clinical difference’ was overestimated in this study.
While the concept of MCID is reasonable in certain situations, it is not likely that this construct can be validly assessed until subjects’ expectations regarding weight loss can be brought into line with what is realistically achievable.
Setting appropriate expectations
A key factor for success in weight management is the setting of realistic, measurable targets for the magnitude and rapidity of weight loss. Indeed, this is a core element of the ‘5A's’ model of behavioural change (Ask, Assess, Advise, Agree, Arrange), an established framework that can be adapted for obesity management 8: the fourth ‘A’ consists of Agreement between healthcare providers and patients about key elements of the plan, including weight loss expectations and the sustainable behavioural changes required to reach those goals 55. Unless appropriate expectations are set, patients are likely to continue to experience distress over obesity when their expectations for weight and shape are not realised 56.
Setting reachable goals is particularly important because many individuals with obesity have unrealistic expectations about the amount of weight they can hope to lose. In a classic study from 1997, subjects defined their ‘ideal weight loss’ as an average 32% reduction in their starting weight, and most patients said they would be ‘disappointed’ with a 17‐kg weight loss; a 25‐kg loss would be considered ‘acceptable’ but not ideal 57. While this magnitude of weight loss may be possible for some patients undergoing bariatric surgery, not all surgical patients will achieve or maintain these types of improvements. Furthermore, these expectations are not accurately reflective of the weight loss potential of the currently available non‐surgical methods (e.g. behavioural interventions with or without adjunctive pharmacotherapy).
In many cases, excessive weight loss expectations and patients’ perceptions of unsatisfactory progress towards those over‐ambitious goals can lead to treatment discontinuation and failure to achieve or maintain an appreciable level of weight loss 58. Additionally, individuals who report lower overall psychological well‐being (as assessed by the mental health scales of the SF‐36) before starting their weight loss intervention tended to have still higher – and thus less reasonable – expectations about the degree to which weight loss would improve their QoL 59.
It is therefore important for healthcare providers to help their patients ground their expectations in reality and avoid ‘making the perfect the enemy of the good.’ Patients should be encouraged to appreciate that the clinical benefits of weight loss (including effects on comorbidities such as cardiovascular disease and diabetes) actually begin in the range of 5–10% loss of starting body weight 60, 61. This degree of weight loss is easier to achieve than patients might expect 62, and setting relatively modest weight loss targets in this range will increase the odds of success 9. Furthermore, patients who meet their own expectations with regard to the QoL effects of weight loss report greater improvements in overall well‐being than subjects whose expectations are not met 59.
Another important aspect to consider, apart from the absolute weight loss in kilograms, is the issue of body shape and body satisfaction. Individuals with obesity who are hopeful that they will achieve the body shape they most desire (e.g. turning a pear shape into an hour‐glass shape) are likely to be disappointed. Interventions based on the approaches of ‘health at every size’ are likely to help individuals with obesity to set reasonable expectations and successfully achieve their weight management goals 63.
Setting achievable weight loss goals has several important benefits for both physicians and individuals with obesity. First, it shifts the focus of weight management from weight loss towards stopping regain. Second, once an individual develops confidence in his or her ability to maintain previously lost weight, it becomes possible to set another achievable weight loss goal. This process can lead to repeated cycles of realistic weight loss followed by behavioural adaptation to protect this new weight. With three to four of these cyclical initiatives, substantial overall weight loss would be possible over an extended period. Physicians can play a major role in supporting patients as they adopt this ‘slow and steady’ approach to sustainable weight management.
The current US 64 and Canadian 10 guidelines recognise that a modest loss of 5–10% of starting body weight is beneficial for most patients and that in most cases this goal should be achievable through a loss of 0.5–1 kg of body weight per week over a period of 6 months. The long‐term goals should then be to maintain weight and avoid weight regain.
Unmet needs and future directions
To date, the most significant changes in distress over obesity and health‐related QoL in individuals living with obesity have been achieved through bariatric surgery 41, 43, 46. However, in most countries surgery is available and appropriate for only a small proportion of individuals struggling with obesity; most guidelines limit its use to individuals with a BMI 40 or higher, or ≥ 35 if there is at least one obesity‐related comorbidity 65. For many patients, behavioural interventions and/or pharmacological management will therefore play a dominant role, either on their own or as part of an integrated, multidisciplinary strategy. Obesity management guidelines support and recommend the use of multidisciplinary strategies, which combine behavioural approaches with pharmacologic or surgical interventions 64. With our ever‐evolving understanding of the behavioural, psychological and motivational challenges of obesity and how they affect QoL, physicians have a growing range of options from which to personalise the weight management approach for each individual, to maximise the chances of success and offer the patient a greater sense of agency.
The role of medications in weight management is an evolving one. Although several pharmacological agents have been introduced in recent years, the options to date have been only modestly effective, and some have had significant safety concerns such that they have been withdrawn from the market 66, 67. The pharmaceutical options currently available for long‐term obesity management in Canada are orlistat (Xenical®, Alli®) and liraglutide (Saxenda®) 68; the range of options in the United States is broader and includes these two medications as well as lorcaserin (Belviq®), phentermine/topiramate (Qsymia®) and bupropion/naltrexone (Contrave®). Medications could have an important role to play in an integrated weight loss plan, as a means to support and sustain the weight loss that patients achieve through behavioural changes.
Medications can enhance the impact of behavioural change in two specific aspects. First, if adding medication to behaviour change increases the magnitude of weight loss, this can be used as a motivational enhancement strategy. All behavioural choices are associated with potential benefits and pitfalls, or advantages and disadvantages 69. Increasing the amount of weight lost increases the advantages of engaging actively in weight management. In turn, this will directly help shift the decisional balance towards change. Adding medication to behaviour change can further reinforce this decisional balance as it clearly increases the advantages of change.
Second, increasing the amount of weight lost via behaviour change reinforces the value of those behaviours. In other words, people experience more pay‐off for their effort, which is positively reinforcing. Greater investment in the behaviours that produced the outcome increases self‐efficacy, which, in turn, predicts longer maintenance of behaviour over time. This can increase the likelihood that positive health behaviours will be maintained after the medication for weight loss is stopped. Thus, truly integrating behaviour change and weight loss medication has the potential to potentiate both treatments and might mitigate weight regain following stopping the medication.
When physicians consider patients’ distress over obesity and expectations about weight loss and associated QoL changes, it becomes possible to set achievable, realistic goals and develop a manageable plan to achieve them; this provides the framework to increase patient‐centred obesity management. Any future developments – either in medical management options, behavioural techniques or other insights into the psychological factors behind weight loss success – that make it easier to achieve these goals should be made widely available to all patients in need, in order to help them turn a vicious cycle of failure into a virtuous cycle of success.
Acknowledgements
The author acknowledges the unrestricted support of Novo Nordisk Canada for launching this project and thanks Sarah von Riedemann, MSc, and John Ashkenas, PhD, both from SCRIPT, Toronto, for writing and editorial support.
Disclosure
The author has no conflicts of interest to disclose.
References
- 1. Canadian Health Measures Survey . http://www.statcan.gc.ca/eng/survey/household/5071 (accessed February 2015).
- 2. World Health Organization . Fact Sheet #311: Obesity and overweight, accessed February 2015. http://www.who.int/mediacentre/factsheets/fs311/en/index.html (accessed February 2015).
- 3. Janssen I. The public health burden of obesity in Canada. Can J Diabetes 2013; 37: 90–6. [DOI] [PubMed] [Google Scholar]
- 4. Guh DP, Zhang W, Bansback N et al. The incidence of co‐morbidities related to obesity and overweight: a systematic review and meta‐analysis. BMC Public Health 2009; 9: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Whitlock G, Lewington S, Sherliker P et al. Body‐mass index and cause‐specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373: 1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health 2010; 100: 1019–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kirk SF, Price SL, Penney TL et al. Blame, shame, and lack of support: a multilevel study on obesity management. Qual Health Res 2014; 24: 790–800. [DOI] [PubMed] [Google Scholar]
- 8. Vallis M, Piccinini‐Vallis H, Sharma AM, Freedhoff Y. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician 2013; 59: 27–31. [PMC free article] [PubMed] [Google Scholar]
- 9. Westenhoefer J. The therapeutic challenge: behavioral changes for long‐term weight maintenance. Int J Obes Relat Metab Disord 2001; 25(Suppl. 1): S85–8. [DOI] [PubMed] [Google Scholar]
- 10. Lau DC, Douketis JD, Morrison KM et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007; 176: S1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scheen AJ. The future of obesity: new drugs versus lifestyle interventions. Expert Opin Investig Drugs 2008; 17: 263–7. [DOI] [PubMed] [Google Scholar]
- 12. Kushner RF. Weight loss strategies for treatment of obesity. Prog Cardiovasc Dis 2014; 56: 465–72. [DOI] [PubMed] [Google Scholar]
- 13. Kubik JF, Gill RS, Laffin M, Karmali S. The impact of bariatric surgery on psychological health. J Obes 2013; 2013: 837989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ray EC, Nickels MW, Sayeed S, Sax HC. Predicting success after gastric bypass: the role of psychosocial and behavioral factors. Surgery 2003; 134: 555–63; discussion 63–4. [DOI] [PubMed] [Google Scholar]
- 15. Gatineau M, Dent M. Obesity and Mental Health. National Obesity Observatory, 2011. [Google Scholar]
- 16. Becker ES, Margraf J, Turke V, Soeder U, Neumer S. Obesity and mental illness in a representative sample of young women. Int J Obes Relat Metab Disord 2001; 25(Suppl. 1): S5–9. [DOI] [PubMed] [Google Scholar]
- 17. Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: comparison and moderation by sex, age, and race. Int J Obes (Lond) 2006; 30: 513–9. [DOI] [PubMed] [Google Scholar]
- 18. Polivy J, Herman CP. Mental health and eating behaviours: a bi‐directional relation. Can J Public Health 2005; 96(Suppl. 3):S43–6, S9‐53. [PubMed] [Google Scholar]
- 19. Taylor VH, Forhan M, Vigod SN, McIntyre RS, Morrison KM. The impact of obesity on quality of life. Best Pract Res Clin Endocrinol Metab 2013; 27: 139–46. [DOI] [PubMed] [Google Scholar]
- 20. der van Merwe MT. Psychological correlates of obesity in women. Int J Obes (Lond) 2007; 31(Suppl. 2): S14–8; discussion S31‐2. [DOI] [PubMed] [Google Scholar]
- 21. Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the importance of obesity‐related social stigma and functional status. J Gen Intern Med 2012; 28: 231–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dulloo AG, Montani JP. Pathways from dieting to weight regain, to obesity and to the metabolic syndrome: an overview. Obes Rev 2015; 16(Suppl. 1): 1–6. [DOI] [PubMed] [Google Scholar]
- 23. Engel SG, Crosby RD, Kolotkin RL et al. Impact of weight loss and regain on quality of life: mirror image or differential effect? Obes Res 2003; 11: 1207–13. [DOI] [PubMed] [Google Scholar]
- 24. Forhan M, Risdon C, Solomon P. Contributors to patient engagement in primary health care: perceptions of patients with obesity. Prim Health Care Res Dev 2013; 14: 367–72. [DOI] [PubMed] [Google Scholar]
- 25. Jepsen R, Aadland E, Andersen JR, Natvig GK. Associations between physical activity and quality of life outcomes in adults with severe obesity: a cross‐sectional study prior to the beginning of a lifestyle intervention. Health Qual Life Outcomes 2013; 11: 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Butler GS, Vallis TM, Perey B et al. The Obesity Adjustment Survey: development of a scale to assess psychological adjustment to morbid obesity. Int J Obes Relat Metab Disord 1999; 23: 505–11. [DOI] [PubMed] [Google Scholar]
- 27. Vallis MT, Ross MA. The role of psychological factors in bariatric surgery for morbid obesity: identification of psychological predictors of success. Obes Surg 1993; 3: 346–59. [DOI] [PubMed] [Google Scholar]
- 28. Vallis M. Are behavioural interventions doomed to fail? Challenges to self‐management support in chronic disease. Can J Diabetes 2015; 39: 330–4. [DOI] [PubMed] [Google Scholar]
- 29. Dove® . The Dove® Campaign for Real Beauty. 2010. http://www.dove.us/Social-Mission/campaign-for-real-beauty.aspx
- 30. Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res 2001; 9: 102–11. [DOI] [PubMed] [Google Scholar]
- 31. van Nunen AM, Wouters EJ, Vingerhoets AJ, Hox JJ, Geenen R. The health‐related quality of life of obese persons seeking or not seeking surgical or non‐surgical treatment: a meta‐analysis. Obes Surg 2007; 17: 1357–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kolotkin RL, Crosby RD, Corey‐Lisle PK, Li H, Swanson JM. Performance of a weight‐related measure of quality of life in a psychiatric sample. Qual Life Res 2006; 15: 587–96. [DOI] [PubMed] [Google Scholar]
- 33. Therrien F, Marceau P, Turgeon N et al. The laval questionnaire: a new instrument to measure quality of life in morbid obesity. Health Qual Life Outcomes 2011; 9: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ziegler O, Filipecki J, Girod I, Guillemin F. Development and validation of a French obesity‐specific quality of life questionnaire: Quality of Life, Obesity and Dietetics (QOLOD) rating scale. Diabetes Metab 2005; 31: 273–83. [DOI] [PubMed] [Google Scholar]
- 35. Stucki A, Borchers M, Stucki G et al. Content comparison of health status measures for obesity based on the international classification of functioning, disability and health. Int J Obes (Lond) 2006; 30: 1791–9. [DOI] [PubMed] [Google Scholar]
- 36. Ware JE, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Med Care. 1992; 30: 473–83 [PubMed] [Google Scholar]
- 37. Hayden MJ, Brown WA, Brennan L, O'Brien PE. Validity of the Beck Depression Inventory as a screening tool for a clinical mood disorder in bariatric surgery candidates. Obes Surg 2012; 22: 1666–75. [DOI] [PubMed] [Google Scholar]
- 38. Nicolucci A, Kovacs Burns K, Holt RI et al. Diabetes attitudes, wishes and needs second study (DAWN2): cross‐national benchmarking of diabetes‐related psychosocial outcomes for people with diabetes. Diabet Med 2013; 30: 767–77. [DOI] [PubMed] [Google Scholar]
- 39. Peyrot M, Rubin RR, Lauritzen T et al. Psychosocial problems and barriers to improved diabetes management: results of the Cross‐National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med 2005; 22: 1379–85. [DOI] [PubMed] [Google Scholar]
- 40. Peyrot M, Skovlund SE, Landgraf R. Epidemiology and correlates of weight worry in the multinational diabetes attitudes, wishes and needs study. Curr Med Res Opin 2009; 25: 1985–93. [DOI] [PubMed] [Google Scholar]
- 41. Gloy VL, Briel M, Bhatt DL et al. Bariatric surgery versus non‐surgical treatment for obesity: a systematic review and meta‐analysis of randomised controlled trials. BMJ 2013; 347: f5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Julia C, Ciangura C, Capuron L et al. Quality of life after Roux‐en‐Y gastric bypass and changes in body mass index and obesity‐related comorbidities. Diabetes Metab 2013; 39: 148–54. [DOI] [PubMed] [Google Scholar]
- 43. Karlsen TI, Lund RS, Roislien J et al. Health related quality of life after gastric bypass or intensive lifestyle intervention: a controlled clinical study. Health Qual Life Outcomes 2013; 11: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kolotkin RL, Crosby RD, Williams GR, Hartley GG, Nicol S. The relationship between health‐related quality of life and weight loss. Obes Res 2001; 9: 564–71. [DOI] [PubMed] [Google Scholar]
- 45. Koohkan S, Schaffner D, Milliron BJ et al. The impact of a weight reduction program with and without meal‐replacement on health related quality of life in middle‐aged obese females. BMC Womens Health 2014; 14: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Strain GW, Kolotkin RL, Dakin GF et al. The effects of weight loss after bariatric surgery on health‐related quality of life and depression. Nutr Diabetes 2014; 4: e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Fabricatore AN, Wadden TA, Higginbotham AJ et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta‐analysis. Int J Obes (Lond) 2011; 35: 1363–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Vallis TM, Butler GS, Perey B et al. The role of psychological functioning in morbid obesity and its treatment with gastroplasty. Obes Surg 2001; 11: 716–25. [DOI] [PubMed] [Google Scholar]
- 49. Folope V, Hellot MF, Kuhn JM et al. Weight loss and quality of life after bariatric surgery: a study of 200 patients after vertical gastroplasty or adjustable gastric banding. Eur J Clin Nutr 2008; 62: 1022–30. [DOI] [PubMed] [Google Scholar]
- 50. Mathus‐Vliegen EM, de Weerd S, de Wit LT. Health‐related quality‐of‐life in patients with morbid obesity after gastric banding for surgically induced weight loss. Surgery 2004; 135: 489–97. [DOI] [PubMed] [Google Scholar]
- 51. Mathus‐Vliegen EM, de Wit LT. Health‐related quality of life after gastric banding. Br J Surg 2007; 94: 457–65. [DOI] [PubMed] [Google Scholar]
- 52. Bauchowitz AU, Gonder‐Frederick LA, Olbrisch ME et al. Psychosocial evaluation of bariatric surgery candidates: a survey of present practices. Psychosom Med 2005; 67: 825–32. [DOI] [PubMed] [Google Scholar]
- 53. Zimmerman M, Francione‐Witt C, Chelminski I et al. Presurgical psychiatric evaluations of candidates for bariatric surgery, part 1: reliability and reasons for and frequency of exclusion. J Clin Psychiatry 2007; 68: 1557–62. [DOI] [PubMed] [Google Scholar]
- 54. Warkentin LM, Majumdar SR, Johnson JA et al. Weight loss required by the severely obese to achieve clinically important differences in health‐related quality of life: two‐year prospective cohort study. BMC Med 2014; 12: 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Canadian Obesity Network , 2011. 5 A's of obesity management. www.obesitynetwork.ca (accessed February 2015).
- 56. Dalle Grave R, Calugi S, Molinari E et al. Weight loss expectations in obese patients and treatment attrition: an observational multicenter study. Obes Res 2005; 13: 1961–9. [DOI] [PubMed] [Google Scholar]
- 57. Foster GD, Wadden TA, Vogt RA, Brewer G. What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. J Consult Clin Psychol 1997; 65: 79–85. [DOI] [PubMed] [Google Scholar]
- 58. Dalle Grave R, Calugi S, Marchesini G. The influence of cognitive factors in the treatment of obesity: lessons from the QUOVADIS study. Behav Res Ther 2014; 63C: 157–61. [DOI] [PubMed] [Google Scholar]
- 59. Pristed SG, Omar HK, Kroustrup JP. Association between fulfilment of expectations and health‐related quality of life after gastric bypass. Appl Res Qual Life 2013; 8: 101–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Knowler WC, Barrett‐Connor E, Fowler SE et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Li G, Zhang P, Wang J et al. Cardiovascular mortality, all‐cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23‐year follow‐up study. Lancet Diabetes Endocrinol 2014; 2: 474–80. [DOI] [PubMed] [Google Scholar]
- 62. Orzano AJ, Scott JG. Diagnosis and treatment of obesity in adults: an applied evidence‐based review. J Am Board Fam Pract 2004; 17: 359–69. [DOI] [PubMed] [Google Scholar]
- 63. Gagnon‐Girouard MP, Begin C, Provencher V et al. Psychological impact of a “Health‐at‐Every‐Size” intervention on weight‐preoccupied overweight/obese women. J Obes 2010; 928097. doi: 10.1155/2010/928097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Jensen MD, Ryan DH, Apovian CM et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014; 129: S102–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Mechanick JI, Youdim A, Jones DB et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity 2013; 21(Suppl. 1): S1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Grunvald E. Medical management of obesity: a comprehensive review. Clin Obstet Gynecol 2014; 57: 465–84. [DOI] [PubMed] [Google Scholar]
- 67. Khan A, Raza S, Khan Y et al. Current updates in the medical management of obesity. Recent Pat Endocr Metab Immune Drug Discov 2012; 6: 117–28. [DOI] [PubMed] [Google Scholar]
- 68. Fujioka K. Safety and tolerability of medications approved for chronic weight management. Obesity 2015; 23(Suppl. 1): S7–11. [DOI] [PubMed] [Google Scholar]
- 69. Rossi JS, Rossi SR, Velicer WF. Motivational readiness to control weight In: Allison DB, ed. Handbook of Assessment Methods for Eating Behaviors and Weight‐related Problems: Measures, Theory, and Research. Thousand Oaks, CA: Sage Publications Inc, 1995. [Google Scholar]
- 70. Ryden A, Karlsson J, Persson LO et al. Obesity‐related coping and distress and relationship to treatment preference. Br J Clin Psychol 2001; 40: 177–88. [DOI] [PubMed] [Google Scholar]
- 71. Mathias SD, Williamson CL, Colwell HH et al. Assessing health‐related quality‐of‐life and health state preference in persons with obesity: a validation study. Qual Life Res 1997; 6: 311–22. [DOI] [PubMed] [Google Scholar]
- 72. Le Pen C, Lévy E, Loss F, Banzet MN, Basdevant A. “Specific” scale compared with “generic” scale: a double measurement of the quality of life in a French community sample of obese subjects. J Epidemiol Community Health 1998; 52: 445–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (BAROS). Obes Surg 1998; 8: 487–99. [DOI] [PubMed] [Google Scholar]
- 74. Mannucci E, Ricca V, Barciulli E et al. Quality of life and overweight: the obesity related well‐being (Orwell 97) questionnaire. Addict Behav 1999; 24: 345–57. [DOI] [PubMed] [Google Scholar]
- 75. Niero M, Martin M, Finger T et al. A new approach to multicultural item generation in the development of two obesity‐specific measures: the Obesity and Weight Loss Quality of Life (OWLQOL) questionnaire and the Weight‐Related Symptom Measure (WRSM). Clin Ther 2002; 24: 690–700. [DOI] [PubMed] [Google Scholar]
- 76. Karlsson J, Taft C, Sjostrom L, Torgerson JS, Sullivan M. Psychosocial functioning in the obese before and after weight reduction: construct validity and responsiveness of the obesity‐related problems scale. Int J Obes Relat Metab Disord 2003; 27: 617–30. [DOI] [PubMed] [Google Scholar]
- 77. Moorehead MK, Ardelt‐Gattinger E, Lechner H, Oria HE. The validation of the Moorehead‐Ardelt Quality of Life Questionnaire II. Obes Surg 2003; 13: 684–92. [DOI] [PubMed] [Google Scholar]
- 78. Weiner S, Sauerland S, Fein M et al. The Bariatric Quality of Life index: a measure of well‐being in obesity surgery patients. Obes Surg 2005; 15: 538–45. [DOI] [PubMed] [Google Scholar]
- 79. Hilbert A, Baldofski S, Zenger M et al. Weight bias internalization scale: psychometric properties and population norms. PLoS ONE 2014; 9: e86303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Tayyem RM, Atkinson JM, Martin CR. Development and validation of a new bariatric‐specific health‐related quality of life instrument ‘‘bariatric and obesity‐specific survey (BOSS)’’. J Postgrad Med 2014; 60: 357–61. [DOI] [PubMed] [Google Scholar]


