Abstract
Introduction
The termination of unwanted pregnancies up to 12 weeks’ gestation became legal in Nepal in 2002. Many interventions have taken place to expand access to comprehensive abortion care services. However, comprehensive abortion care services remain out of reach for women in rural and remote areas. This article describes a training and support strategy to train auxiliary nurse‐midwives (ANMs), already certified as skilled birth attendants, as medical abortion providers and expand geographic access to safe abortion care to the community level in Nepal.
Methods
This was a descriptive program evaluation. Sites and trainees were selected using standardized assessment tools to determine minimum facility requirements and willingness to provide medical abortion after training. Training was evaluated via posttests and observational checklists. Service statistics were collected through the government's facility logbook for safe abortion services (HMIS‐11).
Results
By the end of June 2014, medical abortion service had been expanded to 25 districts through 463 listed ANMs at 290 listed primary‐level facilities and served 25,187 women. Providers report a high level of confidence in their medical abortion skills and considerable clinical knowledge and capacity in medical abortion.
Discussion
The Nepali experience demonstrates that safe induced abortion care can be provided by ANMs, even in remote primary‐level health facilities. Post‐training support for providers is critical in helping ANMs handle potential barriers to medical abortion service provision and build lasting capacity in medical abortion.
Keywords: auxiliary nurse‐midwives (ANMs), medical abortion, Nepal, primary care
INTRODUCTION
Despite significant reductions in maternal mortality in Nepal, complications due to unsafe abortion remained a leading cause of maternal death in the new century. After years of advocacy, Nepali women were granted legal permission in 2002 to terminate unwanted pregnancies up to 12 weeks’ gestation and beyond that under certain conditions. Efforts to increase access to abortion services were launched across Nepal, and by 2009, comprehensive abortion care services were expanded to district hospitals and primary health care centers all over the country.1
Despite rapid expansion, comprehensive abortion care services remain out of reach for many, particularly women in rural or remote areas. In 2009, abortion service provision was limited to physicians and staff nurses using manual vacuum aspiration. After conducting a pilot study to assess the feasibility of introducing medical abortion, a national scale‐up strategy was developed to increase access to safe medical abortion services among women in rural and underserved areas.2, 3 In particular, the government of Nepal committed to expanding comprehensive abortion care availability at health posts and sub–health posts by training auxiliary nurse‐midwives (ANMs) already certified as skilled birth attendants in provision of medical abortion. In Nepal, ANM education comprises either 1) completion of 8th grade plus 2 years of preservice training or 2) completion of 10th grade and School Leaving Certification, plus 18 months of preservice training. After preservice training, which prepares them to assist women in normal births and identify complications during pregnancy, ANMs can participate in a 2‐month in‐service course for skilled birth attendant certification. In comparison, certified nurse‐midwives/certified midwives in the United States have a graduate‐level degree and are trained to provide primary care as well as reproductive care to women and their families.4 Medical abortion provision by ANMs has been demonstrated to be safe and effective at the primary health level in Nepal.5, 6
This article highlights the efforts undertaken by the government of Nepal, with support from Ipas, a global nongovernmental organization dedicated to ending preventable deaths and disabilities from unsafe abortion, to train ANMs as medical abortion providers and expand geographic access to safe abortion care to the community level. Specifically, it describes the critical steps in scaling up abortion care through ANMs: 1) policy change, 2) curriculum development and training center preparation, and 3) a comprehensive training and support strategy.
-
✦
Training auxiliary nurse‐midwives (ANMs) who are local to their community to provide medical abortion is an effective way to expand access to safe induced abortion in rural and underserved areas.
-
✦
A comprehensive posttraining support system, integrated into the existing health system, provides programmatic and clinical support to ANMs as needed.
-
✦
Taking the time and resources to create a supportive, enabling environment among supervisors and key stakeholders at district and facility levels is a crucial step.
-
✦
Applying a client‐oriented provider‐efficient (COPE) approach results in facilities addressing issues of concern in a reasonable time frame.
BACKGROUND AND TRAINING
Policy Change
Advocates in Nepal worked closely with the Ministry of Health and Population over many years to draft and pass the Muluki Ain 11th Amendment Bill containing language to liberalize access to abortion.7 An Abortion Task Force was formed to draft a national safe abortion policy and translate the policy into a legal procedural order. A detailed description of the processes for facility certification, clinical procedures, and provider eligibility are provided elsewhere.1 Of particular relevance to this article is that requirements in the procedural order for provider eligibility were inclusive of ANMs. Providers were required to have 18 months preservice midwifery training, registration by respective professional councils, attendance at in‐service training on postabortion care, and either experience in insertion of intrauterine devices (IUDs) or skilled birth attendance.1 The Ministry of Health, with the support of the Nepal Society of Obstetricians and Gynecologists and through technical support of the Technical Committee for Implementation of Comprehensive Abortion Care, embarked on a path of incremental, evidence‐based expansion of eligible comprehensive abortion care providers. Nurses and ANMs had been authorized and trained to provide postabortion care several years prior to the abortion law change, equipping them with the expertise and experience with manual vacuum aspiration needed to transition into induced abortion care.8 Next came the introduction of medical abortion by both physicians and staff nurses, followed by the initiative described in this article of medical abortion provision by ANMs who have received skilled birth attendant or IUD insertion training and are working at government hospitals, primary health care centers, and health posts. After training, providers are eligible to offer safe induced medical abortion services for unintended pregnancy up to 9 weeks’ gestation.9
Curriculum Development and Training Center Preparation
The Ministry of Health and Population mechanism for providing in‐service training on safe abortion care was adapted for ANMs during the early implementation planning. The comprehensive abortion care curriculum was adapted for the specific needs of ANMs (ie, to allow additional time for questions and discussion) from a 3‐day into a 5‐day intensive training focused only on medical abortion. After review and endorsement by both the Family Health Division and National Health Training Center, the training curriculum was officially adopted by the Training Center. Medical abortion trainers were drawn from the pool of comprehensive abortion care providers who had received Clinical Training Skills certification from the National Health Training Center. A refresher workshop is offered to approximately 32 trainers each year to ensure skill standardization and knowledge update.
Eight of the 12 comprehensive abortion care training centers were selected to offer medical abortion training based on quality and caseload. Two days of theoretical sessions include instruction on the national medical abortion protocol: taking medical history, conducting bimanual examination, and providing counseling based on gestational age. For women with pregnancies greater than or equal to 63 days' gestation, 200 mg mifepristone is provided orally, followed 24 hours later by 4 tablets (200 mcg each) of misoprostol given sublingually or vaginally. Sessions focus on medical abortion service delivery; client follow‐up; risk management (problems and complications); special needs of young, unmarried women; recording and reporting abortion service data; and site policies and procedures to ensure woman‐centered abortion care. Comprehensive abortion care includes postabortion contraception counseling and method provision. As such, postabortion contraception counseling and method provision is included in each stage of the comprehensive training and support strategy. During training, attention is paid to providers’ knowledge and skills with contraceptive counseling and service, and posttraining support includes review of logbook data, ensuring regular supply of commodities and equipment, and updating knowledge and skills of service providers. After the theory classes, participants are engaged in 3 days of clinical training with real clients under continuous supervision of trainers.
Comprehensive Training and Support Strategy
The training strategy was designed not only to equip individual providers with clinical skills for provision of medical abortion, but also to create an enabling environment for the providers’ success through specific pretraining, training, and posttraining activities. Figure 1 presents an overview of the conceptual framework for the comprehensive training and support strategy.
Figure 1.
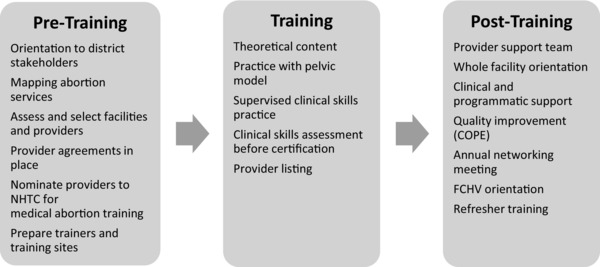
Conceptual Framework for Ipas's Comprehensive Training and Support Strategy
Pretraining: Site/Provider Selection and Preparation
Site selection was done through a district‐level participatory approach. District public health officers, public health nurses, and other district public health office staff were oriented to the safe abortion program in Nepal, including the importance of safe abortion services, legal conditions for induced abortion, the national scale‐up strategy, and the overall process of selecting eligible providers and sites. Participants undertook a mapping exercise to see where safe induced abortion services were available and enumerated potential facilities and eligible ANMs trained as skilled birth attendants for participation in training. Site and provider selection was done through a site visit using standardized assessment tools. Based on the findings of the assessments, district public health staff selected ANMs for training and sent the list of service providers and their associated health facilities to the Department of Health Services, Family Health Division.
Training and Provider/Site Certification
Selected providers were invited by the National Health Training Center to participate in the 5‐day training in medical abortion. Invited ANMs had to agree to: provide medical abortion services to all women regardless of age and marital status, keep and share accurate records, and work with members of the provider support team and Ipas to ensure high‐quality medical abortion services. Of particular interest was ensuring that ANMs would provide services to all women. Previous research indicates that for young, unmarried women, sexual relationships, contraceptive use, and access to abortion is highly stigmatized in Nepal, and this affects their ability to access safe abortion services.10 Participants needed a score of 85% or more in their final evaluation to be considered clinically competent to provide medical abortion services. Those ANMs scoring less than 85% would be required to complete additional clinical practice before receiving their training certificate. Once a provider received her training certificate and submitted other documents required by the Safe Abortion Service Program Implementation Guidelines, she was eligible to be listed as a safe abortion provider by the Ministry of Health and Population. However, listed ANMs are only allowed to perform medical abortion services at their government health facility posting.
Posttraining: Provider, Site, and District Support
Evidence in the literature shows that training alone is not sufficient to ensure provision of a new service after training.11 In response, this intervention includes a multifaceted posttraining support model that is integrated into the existing health system. Components of the posttraining support model include creation of a provider support team, a whole‐site orientation, individual provider support, quality improvement through the client‐oriented provider‐efficient (COPE) approach (a performance improvement strategy), and community awareness–raising activities, including training female community health volunteers in each intervention district in early pregnancy detection and referral programs. More information on the community strategies is provided elsewhere.12
A provider support team is designed to provide ongoing support to medical abortion providers and facilities for managing logistics and drug supply at the site, referring women with unwanted pregnancies to the service sites, managing complications, and managing client flow at the site. Members of the provider support team initiate regular contact with ANMs for check‐ins and targeted support; they are also available to be called upon by ANMs, as needed. Programmatic and clinical support is offered to ANMs over time as much and as often as needed. After training, ANMs receive need‐based follow‐up by clinical and program mentors (from their provider support team) based on request, support team observation, and provider performance as recorded in the clinic's abortion logbook.
A whole‐site orientation is conducted within 3 to 4 weeks of ANM training in each facility by one to 2 members of the provider support team, most often facilitated by the district public health nurse. All providers, staff, the person in charge of each facility, selected female community health volunteers, and members of the health facility management committee participate in values clarification exercises and are introduced to effective strategies for implementing safe abortion services at the facility. Participants come to consensus about initiating medical abortion services, typical fees for services, and provision of and eligibility for free abortion services and are introduced to the performance improvement strategy. Female community health volunteers and community leaders participate in the orientation to gain information about service availability and to provide community perspective on unintended pregnancy and need for safe abortion services.
The National Safe Abortion Policy prioritizes development of a quality assurance process in line with the national safe abortion service program implementation guidelines and protocol. Ipas has used the staff‐driven COPE for comprehensive abortion care approach for facility‐level quality improvement.13 Based on experiences implementing COPE for comprehensive abortion care, Ipas developed COPE guidelines in Nepali in early 2013. Staff at all levels are involved and develop a sense of ownership of quality services and the processes needed to improve quality. This quality improvement approach recognizes that clients have rights, needs, and expectations. At the same time, staff need a supportive work environment, training, and sufficient supplies and equipment to deliver a quality service. The COPE approach focuses on identifying problems in service‐delivery processes and systems, not on specific people. District public health office supervisors receive an orientation on the COPE approach, and then the Ipas district coordinator and district public health staff conduct a 2‐day orientation on COPE in each facility. All staff and members from the health facility management committee participate in the orientation, complete a self‐assessment, and develop an associated action plan. In addition, each facility creates a quality improvement team to support implementation of the action plan. The comprehensive abortion care quality improvement team, which may include facility‐level members of the provider support team, meets monthly to review the status of the action plan. The whole staff meet quarterly to repeat the self‐assessment and update the facility action plan.
Each year, district‐level networking meetings are held that convene trained ANMs, health facility supervisors, clinical mentors, district public health staff, and other stakeholders to share their experiences and challenges with medical abortion service provision. Facilitated by district public health staff, the district public health nurse and district statisticians, with support from Ipas, the networking meetings included 1) sharing findings from client exit interviews; 2) providing technical updates on medical abortion skills and quality of care; 3) sharing medical abortion site service statistics based on logbooks; and 4) recommendations and suggestions for improving medical abortion care in areas such as referral linkages, postabortion care, and supply chain issues. During some networking meetings, providers also developed action plans to address ongoing challenges to medical abortion implementation.
METHODS
This was a descriptive program evaluation of the introduction of medical abortion by ANMs. Human participants (institutional review board [IRB]) approval was obtained from the Nepal Health Research Council. The expansion of medical abortion services through ANMs was implemented in a phased approach over a 4‐year period (December 2010 through June 2014); each year focused on a different set of districts in which eligible sites and providers were selected for scale‐up. Participating districts represent all 5 development regions and include plains, hills, and one mountain area.
Baseline site assessments were conducted in 25 districts. The data captured in the baseline questionnaire included demographics, previous uterine evacuation training/experience, and previous training on medical abortion, as well as provider's willingness to provide services to youth and unmarried women. A baseline site assessment was also completed to ensure minimum facility requirements for provision of medical abortion (including availability of qualified staff, client‐friendly environment, availability of functioning toilet, availability of counseling room or area with adequate privacy, availability of examination room with required instruments, contraceptive supply and counseling, adequate infection prevention practices, drug supply, and client record and reporting system in place); the team assessed several other factors previously identified as critical to successful facility‐level introduction of medical abortion services.2 Facilities that did not meet all requirements at the initial assessment, but had a highly motivated facility manager and commitment from the district health office, received additional support to ensure that the facility was prepared to provide the services. If a selected health facility did not meet all the requirements for service provision, Ipas and district public health staff worked to address identified gaps before training occurred.
At the conclusion of the 5‐day training, evaluation of knowledge and skills was done through a clinical skills assessment checklist and a written posttest. The checklist assessed the ANM's skills in screening clients, providing preprocedure counseling, infection prevention measures, technical ability, and provision of postabortion contraceptives.
Evaluation of the posttraining support model was conducted using provider progress reports, collected at each contact by a member of the provider support team, and quarterly site progress reports. Provider progress reports collected data on how uterine evacuation services were being implemented and identified challenges, if any, of successful service provision as well as support needed. Site progress reports collected data on site infrastructure, service provision, commodity supply (for medical abortion and contraception), adverse events, quality improvement activities, and community outreach. These data were linked to the COPE process and used to evaluate needs. Based on the data, support was provided to ensure regular availability of drugs, equipment, and training. In addition, 98 of the 116 ANMs trained between July 2011 and June 2012 were interviewed 12 to 18 months after their training using a standard tool to get their perspectives on the training and provider support model.
Monitoring of Services
Service provision was monitored as recorded in the HMIS‐11, the government's Safe Abortion Service Register. The register captures data on all uterine evacuation cases, including client demographics, gestation, abortion type (surgical vs medical), pain management, postabortion family planning, and overall outcome. Data were routinely entered and analyzed monthly to identify and address gaps in medical abortion service provision and quality. Findings were reviewed at the national, district, site, and provider level with the intent to ensure accessible, high‐quality medical abortion services for women.
RESULTS
The baseline assessments indicated that service sites tended to have a bias against providing services to young or unmarried women. These issues were addressed through values clarification training during the whole‐site orientation 3 to 4 weeks after ANM training. Improvements were also needed in quality of care and recordkeeping and reporting. These were addressed during training and in posttraining follow‐up.
During the period from December 2010 to June 2014, 463 ANMs from 290 primary public facilities in 25 districts participated in the medical abortion training (Table 1). All participants demonstrated clinical competence and received their training certificate at the conclusion of training, and all obtained their listing as safe abortion providers.
Table 1.
Intervention Sites, Providers Trained, and Posttraining Support Provided Through June 2014 by Training Cohorta
| December 2010– | July 2011– | July 2012– | July 2013– | Cumulative | |
|---|---|---|---|---|---|
| June 2011 | June 2012 | June 2013 | June 2013 | Total | |
| Intervention sites, n | 76 | 66 | 82 | 66 | 290 |
| Total providers trained, n | 122 | 114 | 127 | 100 | 463 |
| Total providers contacted, n | 104 | 109 | 111 | 92 | 416 |
| Total contacts, n | 234 | 505 | 296 | 259 | 1,294 |
| Role of Contact Person,b n (%) | |||||
| Clinical mentor | 140 (60) | 259 (51) | 79 (27) | 55 (21) | 533 (41) |
| On‐site supervisor | 0 (0) | 104 (21) | 1 (0) | 0 (0) | 105 (8) |
| Program coordinator | 3 (1) | 89 (18) | 92 (31) | 26 (10) | 210 (16) |
| Ipas/staff consultant | 91 (39) | 53 (11) | 124 (42) | 178 (69) | 446 (34) |
| Type of Inputs,b, c n (%) | |||||
| Instruction | 168 (72) | 324 (64) | 138 (47) | 50 (19) | 680 (53) |
| Demonstration | 89 (38) | 122 (24) | 32 (11) | 43 (17) | 286 (22) |
| Observation | 138 (59) | 198 (39) | 51 (17) | 44 (17) | 431 (33) |
| Coaching | 154 (66) | 133 (26) | 70 (24) | 42 (16) | 399 (31) |
| Case review | 126 (54) | 153 (30) | 39 (13) | 31 (12) | 349 (27) |
| Joint problem solving | 78 (33) | 75 (15) | 45 (15) | 49 (19) | 247 (19) |
| Encouragement | 164 (70) | 416 (82) | 239 (81) | 229 (88) | 1048 (81) |
| Swap visit | 15 (6) | 11 (2) | 0 (0) | 0 (0) | 26 (2) |
| Resolving equipment/supplies issues | 20 (9) | 142 (28) | 53 (18) | 71 (27) | 286 (22) |
| Recommend service delivery improvements | 30 (13) | 109 (22) | 86 (29) | 85 (33) | 310 (24) |
| Facilitate support from others | 33 (14) | 149 (30) | 51 (17) | 57 (22) | 290 (22) |
| Other | 2 (1) | 4 (1) | 4 (1) | 16 (6) | 26 (2) |
Column percentage totals may not add up to exactly 100% due to rounding.
Denominator is total number of contacts.
Percentage totals may add to more than 100% because more than one input could be provided per contact.
Posttraining Support
The ANMs trained between July 2011 and June 2012 identified the importance of supportive supervision and continued technical assistance in successful provision of medical abortion services. Table 1 also shows the types of posttraining support provided to ANMs over the course of the implementation scale‐up. Most support was programmatic in nature and included encouragement, instruction, observation, and coaching. Clinical mentoring was provided as needed (41% of all contacts) and would have been required for any provider who scored less than 85% on the final training assessment (note: this was not an issue among our training participants). Program support was often aimed at resolving supply or service delivery issues and creating an enabling environment for the ANMs. On average, ANMs received 3.1 contacts (standard deviation [SD], 1.70) posttraining by their provider support team.
The opportunity to share experiences and receive technical updates through district‐level networking meetings granted medical abortion providers from different districts an invaluable opportunity to help each other problem‐solve and plan for improved abortion services. In a 2013 evaluation of ANMs, 83% reported attending a networking meeting and the vast majority of those surveyed found the experience to be “very useful.”
The COPE approach was found to be working well. Beginning in fiscal year 2013, COPE for comprehensive abortion care has been implemented in 78 facilities, successfully engaging health facility staff and health management committee members in improving service quality. Approximately two‐thirds of issues identified in facility action plans in FY13 were resolved within 3 months.
Women Served
Ninety‐three percent (n = 429) of ANMs provided comprehensive medical abortion care services after training. The most frequently cited reasons for nonperformance included lack of women seeking services (33%) and lack of equipment, supplies, or medication for service delivery (32%). On average, 3.8 women received medical abortion services per site per month, resulting in 25,187 women served by June 2014. As shown in Figure 2, there is some seasonal variation in the medical abortion caseload; however, overall caseload has increased over time as the number of ANMs trained and the number of intervention sites have increased. Nearly all women received pain management as part of their comprehensive abortion care service, per the national protocol: 400 mg ibuprofen taken at the time of misoprostol administration and then every 6 to 8 hours, as needed.
Figure 2.
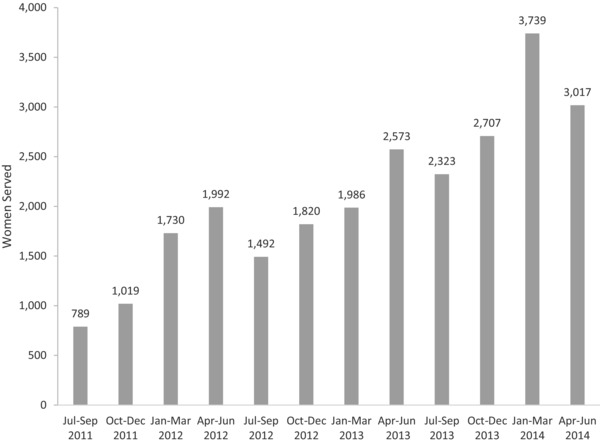
Women Provided with Medical Abortion Services by Auxiliary Nurse‐midwives, July 2011–June 2014
Source: Facility logbooks (HMIS‐11).
Postabortion Contraception
As shown in Figure 3, overall postabortion contraception uptake after medical abortion was high (85%); however, after excluding the use of condoms only, 53% of medical abortion clients received a method. Contraceptive method mix analysis reveals a heavy reliance on short‐term methods (59% of women received condoms or oral contraceptives), with limited use of implants (3%), intrauterine contraception device (2%), or sterilization (0.5%). There was no significant difference in short‐term method acceptance by age: 94.3% of women aged 24 years or younger accepted a short‐term method, compared to 93.7% of women aged 25 years and older. There was no significant variation in uptake or method mix over time.
Figure 3.
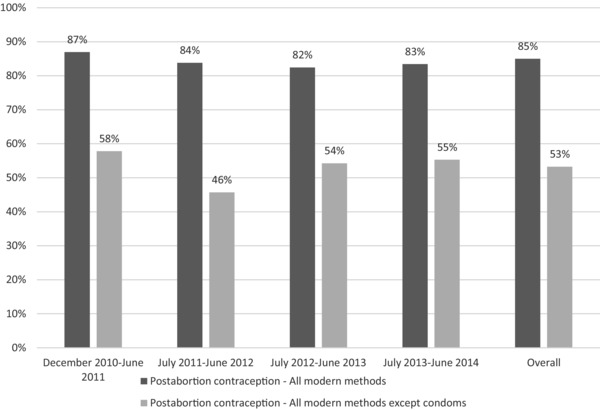
Postabortion Contraception Uptake after Medical Abortion Services by Auxiliary Nurse‐Midwives Provided Through June 2014 by Training Cohort (N = 25,187 Women Served)
Source: Facility logbooks (HMIS‐11).
Midway through the project period, new research confirmed the safety and efficacy of placing implants on the first day of medical abortion.14 While the Nepali abortion guidelines require ANMs to receive skilled birth attendant training (including IUD provision) to qualify for medical abortion training, no prerequisite for implant was included. In response, in December 2013, Ipas piloted a modified training program to incorporate implant insertion into the medical abortion curriculum. A total of 17 combined medical abortion and contraceptive implant trainings were conducted with 96 skilled birth attendant–trained ANMs from the 3 districts of Ittahari, Jhapa, and Morang. All participating ANMs achieved 85% or higher on the skills competency assessment; hands‐on practice providing both medical abortion and implants further raised their competence and confidence levels. However, a comparison of the 2 training strategies found no difference in provision of postabortion implants (P > .05). Challenges to successful provision of implants included unmet need for posttraining clinical support for implants, supply with government‐procured implants and associated infection prevention practices, limited counseling approach, and women's lack of knowledge and familiarity with implants.15
Medical Abortion: Completion and Safety
There were high levels of successful completion of medical abortion, consistent with other projects documenting women accessing medical abortion in Nepal.16, 17, 18, 19, 20, 21 Among the 25,187 women who received a medical abortion in this program, 12,537 (50%) returned to their initial facility for a 2‐week follow‐up visit; 12,352 (98.52%) had a documented successful abortion. Only 1% of medical abortion clients had reported complications after medical abortion provision by ANMs at primary health care centers, health posts, and sub–health posts. Three women (0.01%) had undiagnosed ectopic pregnancy; 83 (0.33%) had ongoing pregnancy (medical abortion failure); and 56 (0.22%) had bleeding and cramping. The majority were treated with manual vacuum aspiration by staff nurses and/or physicians (78 of 142 [55%]). One woman had a serious adverse event, developing heavy bleeding due to retained product of conception about 2 weeks after the medical abortion. She was managed at a referral center with uterine evacuation using manual vacuum aspiration and received a blood transfusion and intravenous fluids and was discharged from the hospital one week later.
DISCUSSION
Providing health services to women in remote and rural areas is often a challenge, and finding sustainable strategies is of utmost importance to help countries reduce maternal deaths due to unsafe abortion. The experience of scaling up medical abortion through ANMs in Nepal using a comprehensive training and support strategy yielded a number of lessons on the successes and challenges of providing abortion care.
Successes
Choosing to work with ANMs was important for sustainability because they are local to their communities and less frequently transferred by the health system compared to physicians. This leads to more consistent availability of induced abortion services at the primary level. It was also important to work with the Ministry of Health and Population systems for training, logistics supply, provider support, and health management information systems in establishing services to create the potential for long‐term sustainability. Laying the groundwork for the expansion of medical abortion services by taking time and resources to create a supportive, enabling environment among supervisors and key stakeholders at district and facility levels was a crucial step. In addition, going beyond a one‐time training and developing a team of local stakeholders dedicated to providing ongoing support to providers was essential in helping ANMs handle potential barriers to medical abortion service provision and build lasting capacity in medical abortion. Establishing a team‐based approach to quality improvement and institutionalization of provider support through the COPE approach created ownership by the health facility management committee and relied on the existing health system, strengthening linkages with the district public health office. Finally, it was important to create awareness and demand for medical abortion services. Lack of women seeking services was one of the main reasons for lack of performance by ANMs.
Challenges
Despite improved reach and availability of medical abortion services, several key community and system barriers remain. Many women need further knowledge on the legal indications for induced abortion and service availability. In addition, stigma about abortion may dissuade women from seeking abortion care in the public facilities. There is continued room for improvement in service availability as well; health posts with only one medical abortion provider will have some days/times when these services are unavailable. Given the lack of accessibility for women, it is also important to improve contraceptive method uptake, particularly for long‐acting reversible contraceptives. Only about half the women received a method other than condoms, and highly effective methods were less likely to be chosen. Providing posttraining support for clinical skills, comprehensive counseling, and availability of quality contraceptive commodities may improve postabortion family planning uptake.
Clinical Implications
Training ANMs as medical abortion providers in Nepal has been a great success to date. To maintain and multiply the gains made so far, the following steps are recommended: 1) continue to scale‐up ANM provision of medical abortion services in remaining districts of Nepal to meet need, particularly in rural and remote areas where access is limited and complications from unsafe abortions are highest; 2) improve training for skilled birth attendants on manual vacuum aspiration and medical abortion by including medical abortion and manual vacuum aspiration skills as part of regular training programs; 3) encourage the use of ANMs as abortion providers by integrating ANM medical abortion training into skilled birth attendant training; 4) improve contraceptive method choice by ensuring ANMs have requisite skills to provide implants through improved integrated implant and medical abortion training or a separate implant training for ANMs trained in medical abortion; 5) expand training and strengthen referral mechanisms to equip ANMs to provide misoprostol for postabortion care; 6) determine feasibility of medical abortion service provision by paramedics without bimanual examination at sub–health post facilities and medical shops; and 7) identify the key components of our pre‐ and posttraining support and facilitate integration into the government's training and national safe abortion program.
The Nepali experience demonstrates that safe induced abortion care can be successfully provided by ANMs, even in remote primary‐level health facilities. Continuing to support providers after training and implementation of the quality improvement COPE process at facilities can build sustainable capacity for provision of medical abortion in Nepal.
AUTHORS
Kathryn L. Andersen, MS, PhD, is the Research and Evaluation Manager based in Chapel Hill, North Carolina, and Senior Advisor to Ipas programs in Asia.
Indira Basnett, MPH, MD, is the Country Program Director for Ipas in Kathmandu, Nepal.
Dirgha Raj Shrestha, MPHM, is the Program Manager at Ipas in Kathmandu, Nepal.
Meena Kumari Shrestha, BN, MPA, MA, is a Nurse and Health System Advisor at Ipas in Kathmandu, Nepal.
Mukta Shah, MS, is a Research and Evaluation Advisor at Ipas in Kathmandu, Nepal.
Shilu Aryal, MD, is the Section Chief for Safe Motherhood and Newborn Health at the Family Health Division, Department of Health Services, Ministry of Health and Population in Kathmandu, Nepal.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
REFERENCES
- 1. Samandari G, Wolf M, Basnett I, Hyman A, Andersen K. Implementation of legal abortion in Nepal: a model for rapid scale‐up of high‐quality care. Reprod Health. 2012;9(7):1742‐1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ipas Nepal . A Comprehensive Report on Implementatoin of Medical Abortion Services in Six Pilot Districts of Nepal. Kathmandu, Nepal: Ipas; 2009. [Google Scholar]
- 3.Ministry of Health and Population, Family Health Division, Department of Health Services. Medical Abortion Scale‐Up Strategy and Implementation Guidelines. Government of Nepal; 2009. [Google Scholar]
- 4. American College of Nurse‐Midwives . Essential Facts About Midwives. Silver Spring, MD: ACNM; 2014. [Google Scholar]
- 5. KC NP, Basnett I, Sharma SK, Bhusal CL, Parajuli RR, Andersen KL. Increasing access to safe abortion services through auxiliary nurse midwives trained as skilled birth attendants. Kathmandu Univ Med J. 2011;9(36):260‐266. [DOI] [PubMed] [Google Scholar]
- 6. Puri M, Tamang A, Shrestha P, Joshi D. The role of auxiliary nurse‐midwives and community health volunteers in expanding access to medical abortion in rural Nepal. Reprod Health Matters. 2014;43 (Supplement):1‐10. [DOI] [PubMed] [Google Scholar]
- 7. Government of Nepal . Muluki Ain (Eleventh Amendment) 2059 No 28a Chapter on Life (unofficial translation on file with Center for Reproductive Rights). 2002.
- 8. Basnett I, Clapham S, Shakya G, McCall M. Evolution of the Post‐abortion Care Program in Nepal: the contribution of the Safe Motherhood Project. Int J Gynaecol Obstet. 2004;86:98‐108. [DOI] [PubMed] [Google Scholar]
- 9. Ministry of Health and Population . CAC Implementation Guideline. Government of Nepal; 2011. [Google Scholar]
- 10. Andersen KL, Khanal RC, Teixeira A, et al. Marital status and abortion among young women in Rupandehi, Nepal. BMC Womens Health. 2015;15(1):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rowe AK, Rowe SY, Peters DH, Holloway KA, Chalker J, Ross‐Degnan D. Early results of a systematic review of strategies to improve health worker performance in low‐ and middle‐ income countries. 4th Annual NIH Conference on the Science of Dissemination & Implementation: Policy & Practice. Bethesda, MD; 2011. [Google Scholar]
- 12. Andersen K, Singh A, Shrestha MK, Shah M, Pearson E, Hessini L. Early pregnancy detection by female community health volunteers in Nepal facilitated referral for appropriate reproductive health services. Glob Health Sci Pract. 2013;1(3):372‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. EngenderHealth, Ipas, Reducing Maternal Mortality and Morbidity Project Ghana . COPE for Comprehensive Abortion Care Services: A Toolbook to Accompany the COPE® Handbook. New York, NY: EngenderHealth; 2009. [Google Scholar]
- 14. Sonalkar S, Hou MY, Borgatta L. Administration of the etonogestrel contraceptive implant on the day of mifepristone for medical abortion: a pilot study. Contraception. 2013;88(5):671‐673. [DOI] [PubMed] [Google Scholar]
- 15. Ipas Nepal . Integrating Medical Abortion and Implant Training for ANMs in Nepal. Lessons Learned from a Pilot Project in Five Districts (Not published); 2013.
- 16. Warriner IK, Wang D, Huong NTM, et al. Can midlevel health‐care providers administer early medical abortion as safely and effectively as doctors? A randomised controlled equivalence trial in Nepal. Lancet. 2011;377(9772):1155‐1161. [DOI] [PubMed] [Google Scholar]
- 17. Karki C, Pokharel H, Kushwaha A, Manandhar D, Bracken H, Winikoff B. Acceptability and feasibility of medical abortion in Nepal. Int J Gynaecol Obstet. 2009;106(1):39‐42. [DOI] [PubMed] [Google Scholar]
- 18. Panta O, Bhattarai D, Parajuli N. Medical abortion versus manual vacuum aspiration in a hilly district hospital of eastern Nepal: a comparative study. Kathmandu Univ Med J. 2013;11(43):206‐209. [DOI] [PubMed] [Google Scholar]
- 19. Giri A, Tuladhar H, Maharjan M, Dhakal N. Prospective study of medical abortion in Nepal Medical College Teaching Hospital (NHCTH): A one year experience. Nepal Med Coll J. 2011;13(3):213‐215. [PubMed] [Google Scholar]
- 20. Chuni N, Chandrashekhar T. Early pregnancy termination with a simplified mifepristone‐medical abortion outpatient regimen. Kathmandu Univ Med J. 2009;7(27):209‐212. [DOI] [PubMed] [Google Scholar]
- 21. Basnett I. Personal Communication. September 2012.


