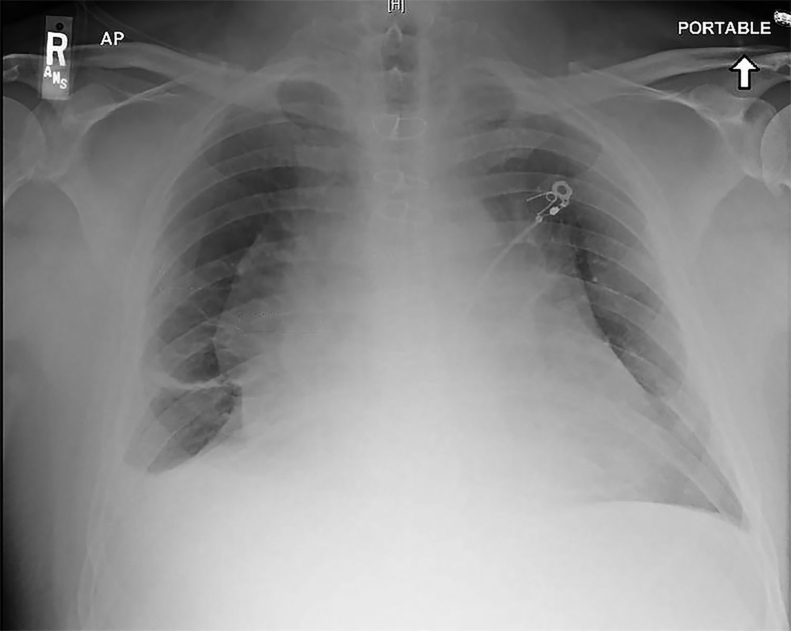
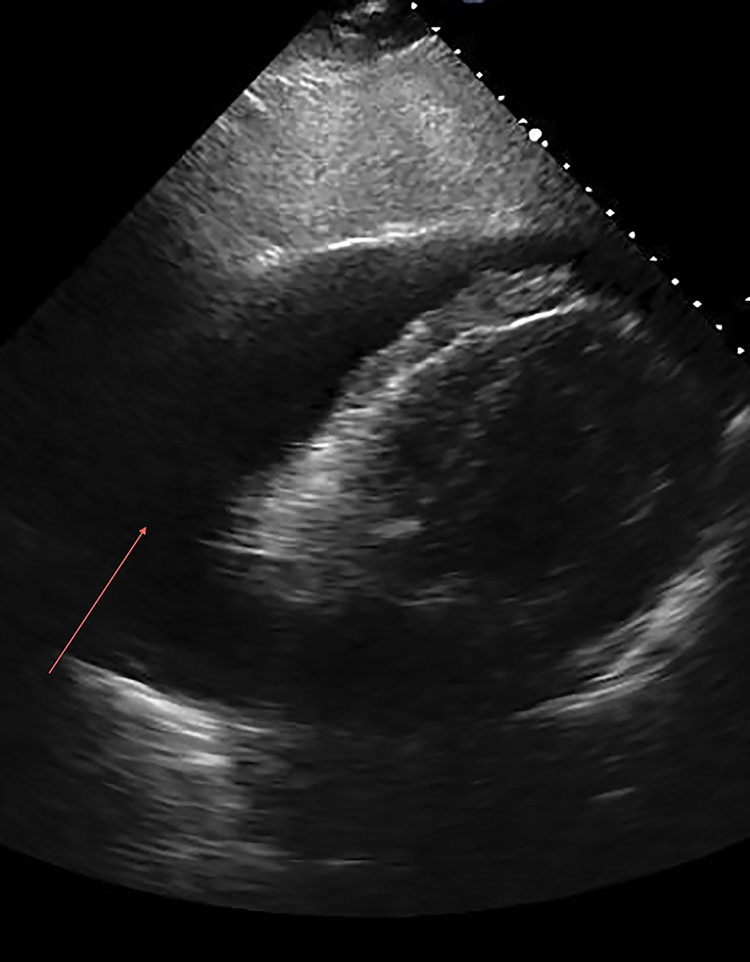
A 50-year-old male presented to the emergency department with dyspnea 6 days following surgery for mechanical aortic valve replacement (25-mm, St. Jude bileaflet valve) through a median sternotomy. Physical examination revealed jugular venous distention, diminished heart sounds, and blood pressure of 110/60 mmHg without obvious pulsus paradoxus. A chest X-ray showed cardiomegaly with widened mediastinum (Fig. 1). With concern for cardiac tamponade, a bedside ultrasound was performed revealing a large pericardial effusion with tamponade physiology (Fig. 2). Urgent echo-guided pericardiocentesis was performed. A total of 1800 mL of blood tinged, turbid (“strawberry shake-like”) pericardial fluid was removed with resolution of clinical signs and symptoms (Fig. 3). A pericardial drain was left in place. Fluid chemistries were diagnostic for chylopericardium (triglyceride level of 844 mg/dL, cholesterol/triglyceride <1, negative cultures).1 He was placed on a chyle diet and the drain was removed after 48 h without re-accumulation of the fluid.
Fig. 1.
Fig. 2.
Fig. 3.
The pathogenesis of chylopericardium is explained by the inevitable transection of the very small lymphatic channels in the pericardial reflections or by operative injury to tributaries of the thoracic duct that, if left untreated over time, can lead to cardiac tamponade.2 The standard approach to treatment of chylopericardium is through a chyle diet and pericardiocentesis, which is effective in 55% of patients.3 If conservative treatment fails, surgical intervention and octreotide injections should be considered. Surgical options include video-assisted thoracoscopic surgery, open thoracotomy, thoracic-duct ligation with a pericardial window, or pericardial–peritoneal shunting.3, 4, 5
Conflicts of interest
The authors have none to declare.
Contributor Information
Matthew Lippmann, Email: mlippmann@kumc.edu.
Kamal Gupta, Email: kgupta@kumc.edu.
References
- 1.Dib C., Tajik A.J., Park S., Kheir M.E., Khandieria B., Mookadam F. Chylopericardium in adults: a literature review over the past decade (1996–2006) J Thorac Cardiovasc Surg. 2008;136(3):650–656. doi: 10.1016/j.jtcvs.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 2.Gowani S.A., Khowaja A.A., Khan A., Fatimi S.H. Chylopericardium – a rare complication after ventricular septal defect repair. J Pak Med Assoc. 2008;58(4):218–219. [PubMed] [Google Scholar]
- 3.Chan B.B., Murphy M.C., Rodgers B.M. Management of chylopericardium. J Pediatr Surg. 1990;25(11):1185–1189. doi: 10.1016/0022-3468(90)90761-w. [DOI] [PubMed] [Google Scholar]
- 4.Tchervenkov C.I., Dobell A.R. Chylopericardium following cardiac surgery. Can J Surg. 1985;28:542–543. [PubMed] [Google Scholar]
- 5.Schiessler A., John A., Pallua N., Bucherl E.S. Chylopericardium following aorto-coronary bypass procedure. J Thorac Cardiovasc Surg. 1984;32:112–114. doi: 10.1055/s-2007-1023362. [DOI] [PubMed] [Google Scholar]