Abstract
Prediction of left main coronary artery (LMCA) or equivalent disease is important with regard to selecting the appropriate treatment strategy. The classical electrocardiographic pattern of LMCA disease includes ST elevation (STE) in lead aVR in the presence of extensive ST depression (most prominent in leads I, II, and V4–6) with the STE in aVR ≥ V1. Patients with these findings may potentially require early coronary angiography and coronary bypass surgery; therefore selected patients with these findings on exercise testing might benefit from more urgent or expedited angiography.
Keywords: Electrocardiography, Left main coronary artery stenosis, Exercise testing
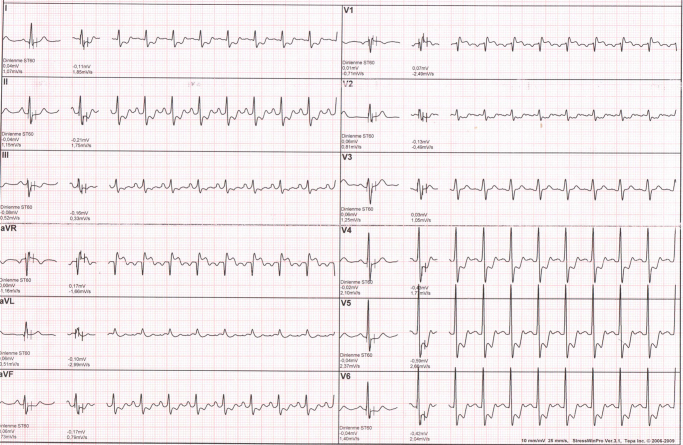
Prediction of left main coronary artery (LMCA) disease (occlusion or stenosis/obstruction) is important with regard to selecting the appropriate treatment strategy, because acute LMCA occlusion usually causes severe hemodynamic deterioration, resulting in a less favorable prognosis.1, 2 Indeed, some authors argue that using the term “LMCA occlusion” is inaccurate, as most of these patients have at least some flow in their LMCA stenosis/obstruction (i.e. subtotal occlusion of LMCA). Over the past 2 decades, multiple studies have examined the utility of ST elevation (STE) in aVR for predicting severe LMCA or LMCA equivalent disease and mortality in patients with acute coronary syndromes1, 2, 3 and those undergoing exercise stress testing.3, 4, 5, 6 The classical electrocardiographic (ECG) pattern of LMCA disease includes STE in lead aVR in the presence of extensive ST depression (most prominent in leads I, II, and V4–6) with the STE in aVR ≥ V1 (Fig. 1).7 Patients with these findings may potentially require early coronary angiography and coronary bypass surgery.1 Since lead aVR is electrically opposite to the left-sided leads I, II, aVL, and V4–6; ST depression in these leads will produce reciprocal ST elevation in aVR. Indeed, STE in aVR is postulated to result from two possible mechanisms: (a) diffuse subendocardial ischaemia, with ST depression in the lateral leads producing reciprocal change in aVR or (b) infarction of the basal septum, i.e. a STE myocardial infarction involving aVR.8 Whereas STE in aVR ≥ 1 mm indicates severe LMCA or LMCA equivalent disease, the STE in aVR ≥ V1 differentiates LMCA from proximal left anterior descending artery occlusion.7 The absence of STE in aVR almost entirely excludes a significant LMCA lesion.9 In addition to an acute coronary syndrome, STE in aVR during exercise stress testing also predicts LMCA or ostial LAD stenosis.10, 11 Selected patients with these findings on exercise testing (Fig. 1) might benefit from more urgent or expedited angiography.1
Fig. 1.
12 lead electrocardiogram during exercise testing showing ST elevation in lead aVR in the presence of extensive ST depression (most prominent in leads I, II and V4–6) with the ST elevation in aVR ≥ V1 taken from patient with angiographically confirmed left main coronary artery disease.
Conflicts of interest
The authors have none to declare.
References
- 1.Kosuge M., Ebina T., Hibi K. An early and simple predictor of severe left main and/or three-vessel disease in patients with non-ST-segment elevation acute coronary syndrome. Am J Cardiol. 2011;107:495–500. doi: 10.1016/j.amjcard.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Wong C.K., Gao W., Stewart R.A. The prognostic meaning of the full spectrum of aVR ST-segment changes in acute myocardial infarction. Eur Heart J. 2012;33:384–392. doi: 10.1093/eurheartj/ehr301. [DOI] [PubMed] [Google Scholar]
- 3.Barrabes J.A., Figueras J., Moure C., Cortadellas J., Soler-Soler J. Prognostic value of lead aVR in patients with a first non-ST-segment elevation acute myocardial infarction. Circulation. 2003;108:814–819. doi: 10.1161/01.CIR.0000084553.92734.83. [DOI] [PubMed] [Google Scholar]
- 4.Gorgels A.P., Vos M.A., Mulleneers R., de Zwaan C., Bar F.W., Wellens H.J. Value of the electrocardiogram in diagnosing the number of severely narrowed coronary arteries in rest angina pectoris. Am J Cardiol. 1993;72:999–1003. doi: 10.1016/0002-9149(93)90852-4. [DOI] [PubMed] [Google Scholar]
- 5.Michaelides A.P., Psomadaki Z.D., Aigyptiadou M.N. Significance of exercise-induced ST changes in leads aVR, V5, and V1. Discrimination of patients with single- or multivessel coronary artery disease. Clin Cardiol. 2003;26:226–230. doi: 10.1002/clc.4960260506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kosuge M., Kimura K., Ishikawa T. Predictors of left main or three-vessel disease in patients who have acute coronary syndromes with non-ST-segment elevation. Am J Cardiol. 2005;95:1366–1369. doi: 10.1016/j.amjcard.2005.01.085. [DOI] [PubMed] [Google Scholar]
- 7.Yamaji H., Iwasaki K., Kusachi S. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography. ST segment elevation in lead aVR with less ST segment elevation in lead V(1) J Am Coll Cardiol. 2001;38:1348–1354. doi: 10.1016/s0735-1097(01)01563-7. [DOI] [PubMed] [Google Scholar]
- 8.Knotts R.J., Wilson J.M., Kim E., Huang H.D., Birnbaum Y., Diffuse S.T. depression with ST elevation in aVR: is this pattern specific for global ischemia due to left main coronary artery disease? J Electrocardiol. 2013;46:240–248. doi: 10.1016/j.jelectrocard.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 9.Kuhl J.T., Berg R.M. Utility of lead aVR for identifying the culprit lesion in acute myocardial infarction. Ann Noninvasive Electrocardiol. 2009;14:219–225. doi: 10.1111/j.1542-474X.2009.00300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uthamalingam S., Zheng H., Leavitt M. Exercise-induced ST-segment elevation in ECG lead aVR is a useful indicator of significant left main or ostial LAD coronary artery stenosis. JACC Cardiovasc Imag. 2011;4:176–186. doi: 10.1016/j.jcmg.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Michaelides A.P., Psomadaki Z.D., Richter D.J. Significance of exercise-induced simultaneous ST-segment changes in lead aVR and V5. Int J Cardiol. 1999;71:49–56. doi: 10.1016/s0167-5273(99)00115-1. [DOI] [PubMed] [Google Scholar]