Abstract
Cardiac rhythm abnormalities have been uncommonly observed in dengue fever and most of them have been reported in children. We discuss a 30-year-old female with dengue fever, who presented with repeated symptomatic episodes of high degree atrioventricular block with ventricular asystole, which responded to intravenous atropine and oral orciprenaline without recurrence on 6 months follow-up.
Keywords: Atrioventricular block, Dengue, Asystole, Bradyarrhythmias
1. Introduction
Dengue fever is an important emerging infectious disease, especially in South-East Asia region. Though shock and intravascular hypovolemia is the most documented cardiovascular complication associated with dengue, various specific cardiac manifestations such as myocarditis, myocardial dysfunction, and arrhythmias have also been less commonly described.1 Majority of the cardiac rhythm abnormalities in dengue fever have been reported in children with only a few recent case reports from adults.2, 3, 4, 5 We report a case of transient symptomatic episodes of high degree atrioventricular (AV) block with ventricular asystole in an adult with dengue fever.
2. Case report
A 30-year-old female was admitted in ICU with complaints of fever with chills since 2 weeks, one episode of seizure 2 days prior and vomiting since 1 day before admission. The seizure was described as jerky movements of all four limbs associated with unconsciousness and fall, lasting for 10–15 s and with immediate recovery without any post-ictal drowsiness/bowel-bladder incontinence. There was no past history of arrhythmia, cardiac disease, or seizures. On examination patient was afebrile, clinically stable with relative bradycardia with pulse rate of 58/min regular, BP of 100/60 mmHg; systemic examination was normal. ECG on admission showed sinus bradycardia (Fig. 1). On investigations, patient had pancytopenia with Hb – 7.6 g%, Hct – 24.2, WBC count – 2200/mm3, platelet count – 64,000/mm3. CT brain – normal. Liver enzymes were raised (SGOT – 306 IU/L, SGPT – 138 IU/L). Patient was started on intravenous antibiotics and supportive treatment. Patient was worked up for pancytopenia. In view of history of 2-week fever with pancytopenia on admission our differential diagnoses were (1) toxemia with enteric fever, (2) hemophagocytic lymphohistiocytosis (HLH) secondary to viral infection, (3) connective tissue disorder, and (4) hematological disorder. Patient was investigated for these and was found to have elevated serum ferritin, serum triglycerides, and occasional hemophagocytes on bone marrow aspirate. Dengue IgM titres and NS1 antigen were positive and ultrasonogram showed mild hepatomegaly with pseudothickening of gall bladder, mild ascites, and mild right sided pleural effusion, suggestive of Dengue fever. Hence a diagnosis of HLH as post-sequelae to dengue fever was made and the patient was given intravenous gamma globulins as part of treatment of HLH. Patient was afebrile throughout the hospital stay. On day 4 of admission patient had 1 episode of vomiting followed by high degree AV block with ventricular asystole on the cardiac monitor, lasting for 11 s which responded to IV atropine, after which the patient had persistent sinus bradycardia with pulse rate remaining 50/min (Fig. 2). On the same day patient had a similar repeat episode of giddiness and vomiting associated with high degree AV block with ventricular asystole, while at rest which responded to IV atropine. Temporary transvenous pacing could not be done because of low platelet counts. Serum potassium, calcium and magnesium, thyroid profile, and 2D-ECHO were normal. In the presence of rhythm disturbances, the patient was further investigated for underlying myocarditis. The creatinine phosphokinase (CPK) and lactate dehydrogenase levels were slightly raised, however Troponin-T and CPK-MB levels were normal, with Troponin-T hs – 0.012 ng/ml (normal range <0.100 ng/ml) and CPK-MB – 1.47 ng/ml (normal range up to 2.88 ng/ml). She was hemodynamically stable with persistent sinus bradycardia (heart rate – 48 to 60/minute). She was started on tablet orciprenaline (10 mg) qds (to accelerate the sinus rate) and was counseled about the SOS need for temporary cardiac pacing. On day 6 again patient had similar episode of high degree AV block with ventricular asystole associated with syncope lasting for a few seconds and which responded to IV atropine. On day 7, the heart rate improved and was remaining between 70 and 75 beats/min. Orciprenaline was continued, there were no further episodes of AV block or syncope and heart rate remained between 70 and 90/minute. The patient was discharged on day 10 on orciprenaline, which was continued for 1 month. On follow-up after 1 month, heart rate was normal and the patient had no history of any further syncopal episodes, ECG was normal, orciprenaline was stopped and she was asked to follow-up. On close follow-up of 6 months, there was no recurrence of the bradyarrhythmia on monitoring with external loop recorder for 7 days.
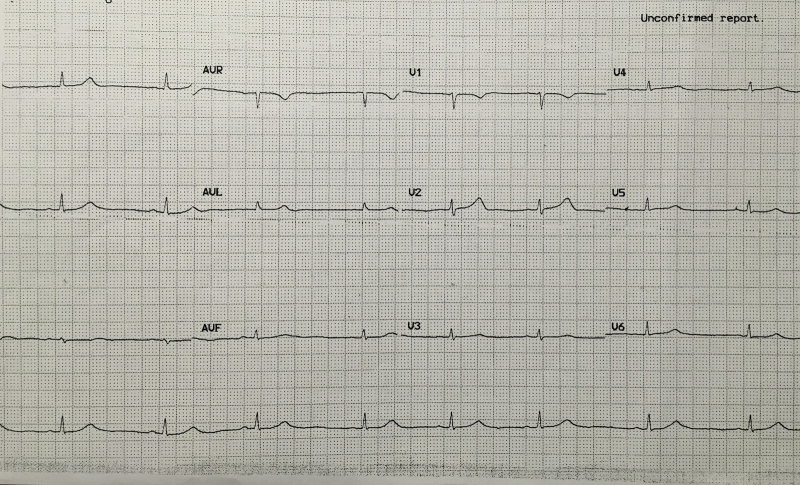
Fig. 1.
ECG on admission showing sinus bradycardia.
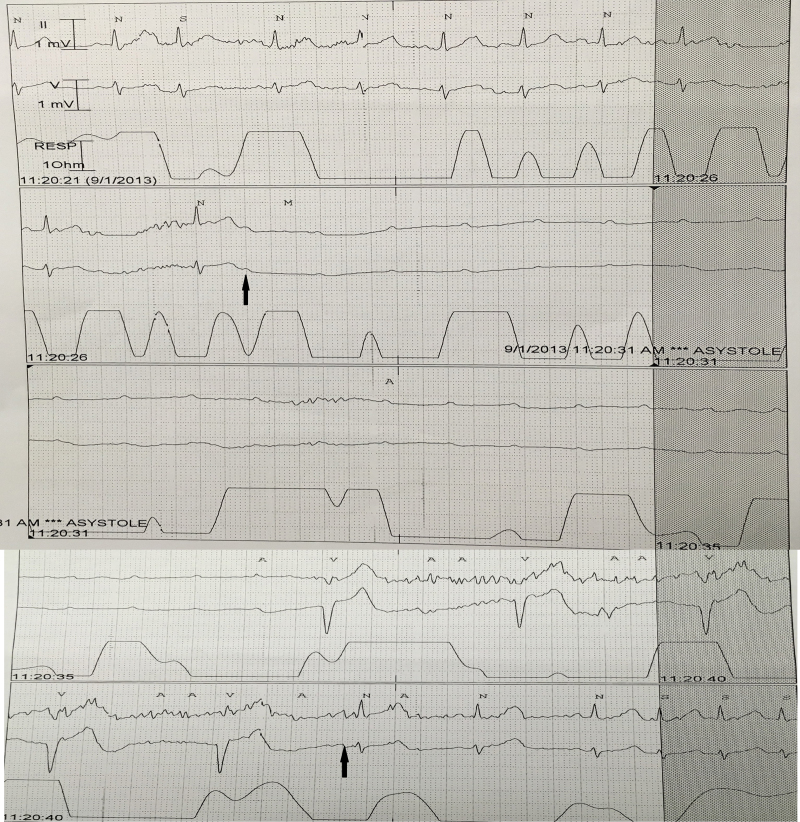
Fig. 2.
Rhythm strip during the episode of high degree AV block with ventricular asystole (solid black arrows showing the beginning and termination of AV block).
3. Discussion
Dengue is an important infectious disease and a major cause of morbidity and mortality in the South East Asia region. Hemorrhage and shock are the most common causes of death. Cardiac manifestations of dengue fever, though rare, should be known to physicians as they could influence the outcome of the disease.3
ECG alterations reported in dengue are often transient and nonspecific, including sinus bradycardia, atrioventricular block, T wave, and ST-segment abnormalities.1, 6 They are now known to occur during any phase of the disease, being observed in 30–44% of hospitalized dengue patients.1 The association between dengue and bradyarrhythmias was highlighted in a study from Singapore.1
Rhythm abnormalities reported in dengue fever include complete AV block,7 first degree AV block,3 atrial fibrillation,1 Mobitz type I and type II second-degree AV block,3, 4 complete heart block,5 ventricular arrhythmia,3 and sinus node dysfunction.1 Majority of these are self-limited; one case recovered after 5 months3 and one case required a permanent pacemaker.5 Lim et al. recently reported a 20-year-old male with dengue fever with complete heart block due to myocarditis.5
In a 24 h Holter monitoring study of 35 children in the recovery phase of dengue, 29% had ECG abnormalities,8 primarily bradyarrhythmias such as first and second degree heart block, as well as atrial and ventricular ectopic beats. Our patient was in the critical/convalescent phase of dengue.
The pathophysiological mechanisms behind these conduction abnormalities in dengue fever are not well understood and further studies are required for the same.
Dengue myocarditis leading to arrhythmias and episodes of syncope/sudden death have been reported.4 Though myocarditis was excluded in our case by normal cardiac markers, there is still a possibility of subclinical myocarditis and since the AV block in our patient responded to atropine altered autonomic tone could also be one of the possible mechanisms.1
Patients with high grade AV block may present with seizures.9 This may explain the seizure that occurred one day before admission in our patient; however there was no documentation of the arrhythmia. Misreporting of syncopal attack as seizure is also likely.
The high degree AV block in our case responded to atropine and orciprenaline, as has been described earlier.6
As seen in our case, the rhythm abnormalities in dengue fever tend to be self-limited, with normal cardiac biomarkers and echocardiograms and resolve in the majority of patients at discharge or on follow-up.3 However symptomatic patients with advanced AV blocks may rarely require a temporary pacing. The clinical relevance of ECG alterations in dengue remains speculative, but a bradyarrhythmia occurring in the presence of hypovolemia can impair cardiac output due to inability to mount an appropriate heart rate response, and can add to hemodynamic instability. Thus very careful attention to fluid balance and hemodynamic monitoring is warranted in these patients.
Dengue being a major infectious disease in India, it is important for the clinicians to be aware of these cardiac rhythm abnormalities associated with it. In dengue patients presenting clinically with shock or atypical symptoms such as presyncope, syncope, and convulsions, it is important to keep myocarditis and/or arrhythmias in mind, so that unnecessary extensive evaluation can be avoided and close monitoring is ensured to pick up these rhythm abnormalities.
Conflicts of interest
The authors have none to declare.
References
- 1.Jacob S., Wertheim H., Simmons C.P., Screaton G., Wills B. Cardiovascular manifestations of the emerging dengue pandemic. Nat Rev Cardiol. 2014;11:335–345. doi: 10.1038/nrcardio.2014.40. [DOI] [PubMed] [Google Scholar]
- 2.Gulati S., Maheshwari A. Atypical manifestations of dengue. Trop Med Int Health. 2007;12:1087–1095. doi: 10.1111/j.1365-3156.2007.01891.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaushik J.S., Gupta P., Rajpal S., Bhatt S. Spontaneous resolution of sinoatrial exit block and atrioventricular dissociation in a child with dengue fever. Singapore Med J. 2010;51:e146–e148. [PubMed] [Google Scholar]
- 4.Nigam A.K., Singh O., Agaarwal A., Singh A.K., Yadav S. Transient 2nd degree Av block Mobitz type II: a rare finding in dengue haemorrhagic fever. J Clin Diagn Res. 2015;9:OD12–OD13. doi: 10.7860/JCDR/2015/12406.5942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim S.M.S., Hoo F.K., Sulaiman W.A.W. A case of dengue hemorrhagic fever with myocarditis and complete heart block. Rawal Med J. 2014;39:104–106. [Google Scholar]
- 6.La-Orkhun V., Supachokchaiwattana P., Lertsapcharoen P., Khongphatthanayothin A. Spectrum of cardiac rhythm abnormalities and heart rate variability during the convalescent stage of dengue virus infection: a Holter study. Ann Trop Paediatr. 2011;31:123–128. doi: 10.1179/1465328111Y.0000000008. [DOI] [PubMed] [Google Scholar]
- 7.Kularatne S.A., Pathirage M.M., Kumarasiri P.V., Gunasena S., Mahindawanse S.I. Cardiac complications of a dengue fever outbreak in Sri Lanka, 2005. Trans R Soc Trop Med Hyg. 2007;101:804–808. doi: 10.1016/j.trstmh.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Kannankeril P.J., Fish F.A. Disorders of cardiac rhythm and conduction. In: Allen H.D., Driscoll D.J., Shaddy R.E., Feltes T.F., editors. Moss and Adams’ Heart Diseases in Infants, Children, and Adolescents Including Fetus and Young Adults. 7th ed. Wolter-Kluwer/Lippincott Williams & Wilkins; Philadelphia: 2008. pp. 293–341. [Google Scholar]
- 9.Sahin I., Karabulut A., Kizkapan F., Okuyan E. Epileptic seizures secondary to high degree atrioventricular block without escape rhythm. Turk Kardiyol Dern Ars (Turkey) 2014;42:655–657. doi: 10.5543/tkda.2014.20050. [DOI] [PubMed] [Google Scholar]