Abstract
We present a 62-year-old lady admitted in our hospital with two episodes of acute ischemic stroke about 2 weeks apart. She was evaluated for acute ischemic stroke and was thrombolysed for recent stroke in right MCA territory first time. On further evaluation, she was found to have a RVOT mass. A transthoracic and transesophageal echocardiogram revealed a PFO and a large, 5.1 cm × 2.3 cm, ovoid, well circumscribed, echogenic mass in the right ventricle outflow tract attached by small pedicle to the ventricular side of anterior tricuspid leaflet, partly obstructing the right ventricular outflow tract and protruding through the pulmonic valve during systole. She was scheduled for surgery (right ventricular mass excision and PFO closure) after 3 weeks due to the risk of secondary hemorrhage in the infarcted area following thrombolysis and anticoagulation and so was discharged with medications after full neurologic recovery after about a week of hospital stay.
She was readmitted 7 days after discharge, before the scheduled date of surgery with history of weakness of right upper limb, slurred speech and mild breathing difficulty lasting for about 20 min following which she improved slowly (transient ischemic attack). The tumor was completely removed with the stalk using cardiopulmonary bypass support. The histopathological findings confirmed the diagnosis of myxoma.
Abbreviations: RV, right ventricle; RVOT, right ventricle outflow tract; TIA, transient ischemic attack; MCA, middle cerebral artery; MRI, magnetic resonance imaging; HPE, histo pathologic examination; PFO, patent foramen ovale
Keywords: Cerebral artery, Magnetic resonance imaging, Histopathologic examination, Patent foramen
1. Introduction
Primary tumors of the heart are rare with the incidence of 0.02–0.05%.1 Cardiac myxomas are rare benign tumors, which account for nearly 50% of all adult primary cardiac tumors.2
Approximately 75–80% of myxomas are located in the left atrium, 10–20% are in the right atrium, and 5–10% are in both atria or either ventricle.3
Typically, solitary, pedunculated, and arising in the vicinity of the fossa ovalis, they may on occasion be multicentric, sessile, or attached to other areas of endocardium. Myxomas arising from the right ventricle are extremely rare.4, 5
Clinically they present with symptoms of hemodynamic obstruction, embolization or constitutional changes. Diagnosis at present is established most appropriately with two dimensional echocardiography.6 Prompt excision using cardiopulmonary bypass, first carried out by Crafoord in 1954,7 has been established as the only acceptable mode of treatment for these tumors.8
The surgeon must try to prevent fragmentation and intraoperative embolization of the tumor, postoperative recurrence and the missing of an occasional multicentric lesion. During the past five decades multiple centers have shown excellent surgical therapy results with a decreasing mortality.
We reported a patient with myxoma located in the right ventricle resulting in paradoxical embolization and recurrent stroke.
2. Case report
We present a 62-year-old lady admitted in our hospital with history of weakness of left upper limb and slurred speech which lasted for about 20 min. She was evaluated for acute ischemic stroke. Neurological examination revealed conscious, oriented patient with mild dysarthria, left upper limb weakness with power 4/5. Clinical examination revealed systolic murmur at the left upper sternal border. She was investigated to find the cause for stroke like ECG, 2-D echo, coronary angiogram, carotid Doppler, EEG, coagulation profile, ultrasound abdomen, which were reported as normal. Ventilation perfusion scan was not done as patient did not show signs of oxygen desaturation at the time of this event.
MRI brain revealed an acute infarct in the right MCA territory and on further cardiac evaluation was found to have a right ventricular mass and a small patent foramen ovale; mitral valve proplase (PML proplapse) with moderate mitral regurtitation and good left ventricular function. She was thrombolysed with recombinant tissue plasminogen activator and was scheduled for surgery (right ventricular mass excision and PFO closure) after 3 weeks due to the risk of secondary hemorrhage in the infracted area following thrombolysis and anticoagulation and so was discharged with medications after full neurologic recovery after about a week of hospital stay.
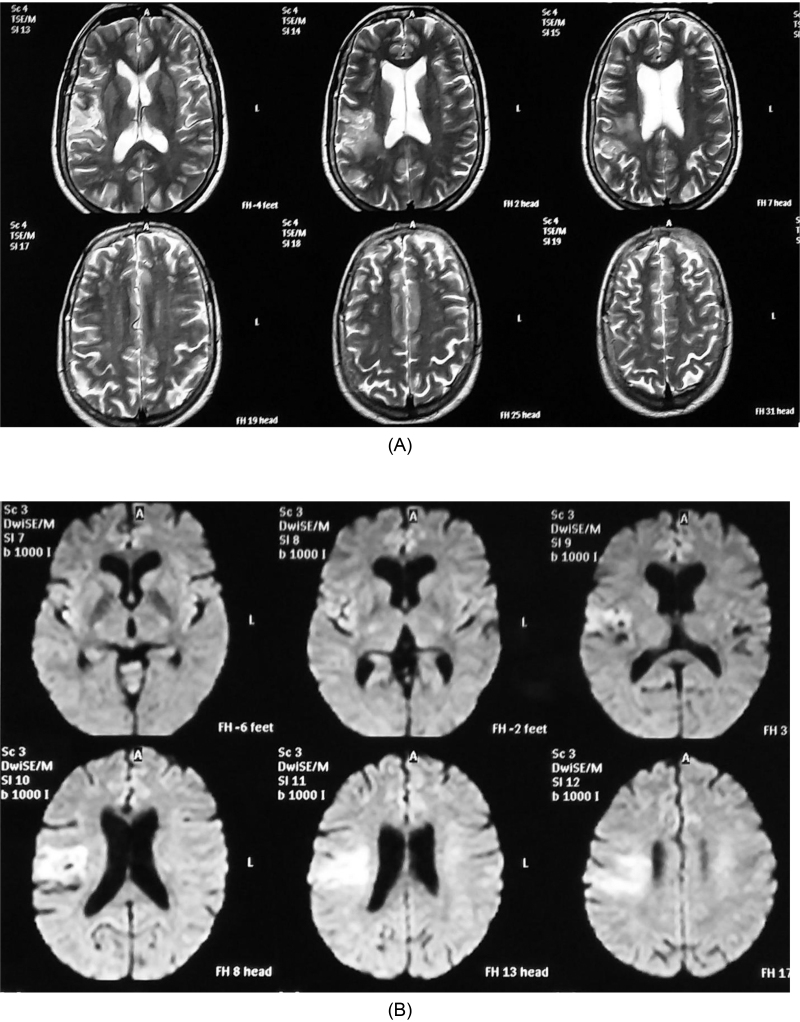
She was readmitted 7 days after discharge, before the scheduled date of surgery with history of weakness of right upper limb, slurred speech and mild breathing difficulty lasting for about 20 min following which she improved slowly (transient ischemic attack). MRI brain (Fig. 1) showed T2 FLAIR images (A) showed hyperintense signals in right pre- and post-central gyri with corresponding restricted diffusion on diffusion weighted images (B) suggestive of acute infarct. We decided to go ahead with the surgery after second episode of stroke.
Fig. 1.
MRI shows hyperintense signals in pre- and post-central gyri.
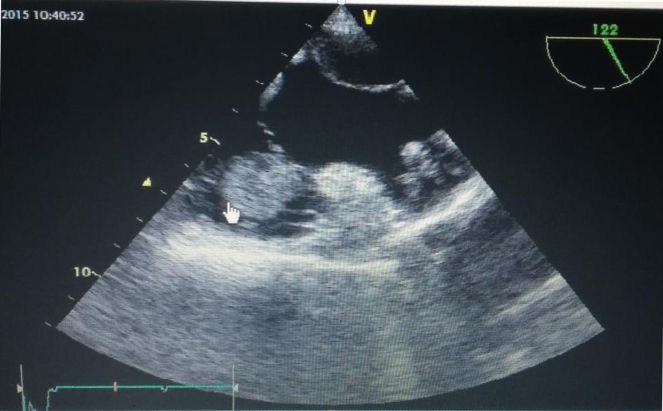
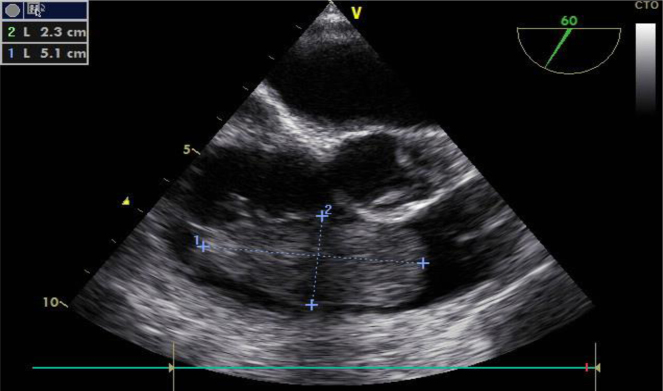
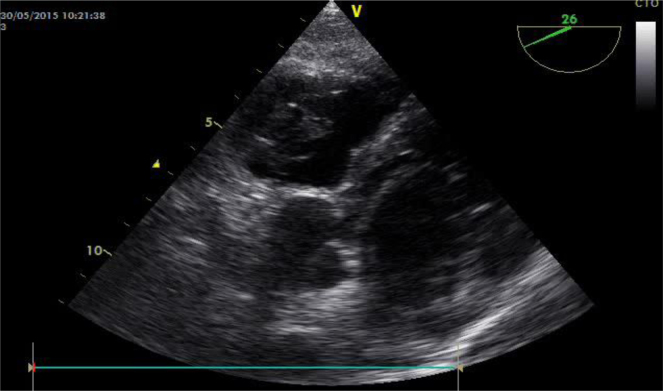
This lady presented with recurrent stroke probably due to paradoxical embolization of tumor tissue through PFO. Transesophageal echo (Fig. 2, Fig. 3, Fig. 4, Fig. 5) revealed attachment of right ventricular myxoma to the ventricular side of anterior tricuspid leaflet close to PFO which could have embolized to brain resulting in stroke. Intraoperatively, it was noted that PFO was significantly large about 1 cm2 as compared to TEE finding hence, was closed with a pericardial patch and was situated close to the fragile tumor tissue attached to tricuspid leaflet. An event like coughing, sneezing or straining could have triggered a right to left shunt across the PFO resulting from high intrathoracic pressure and raised central venous pressure leading to a possible paradoxical embolization of fragile tumor tissue.
Fig. 2.
Deep transgastric RV outflow view: RV myxoma obstructing RVOT and protruding into pulmonary valve during systolae.
Fig. 3.
Modified bicaval view: PFO with RV myxoma attachment to tricuspid leaflet.
Fig. 4.
TEE-RV inflow–outflow view: large oval shape myxoma in RV extending from tricuspid valve to pulmonary valve.
Fig. 5.
Deep transgastric RV apical view: RV myxoma attachment to anterior tricuspid leaflet by a stalk.
The patient was operated on using the extracorporeal circulation. Cardiopulmonary bypass was instituted with the bicaval cannulation; returning blood to the ascending aorta. Both venae cavae were snared and right atrium was opened. The tumor was excised in multiple fragments (gelatinous grayish-brown tissue) together with the stalk and tumor base was thermocauterized and the resultant rent in the anterior leaflet of the tricuspid valve was sutured using 6 ‘o’ prolene. Tricuspid valve coaptation and competence was checked and found intact. Saline wash and lavage of the chambers was done.
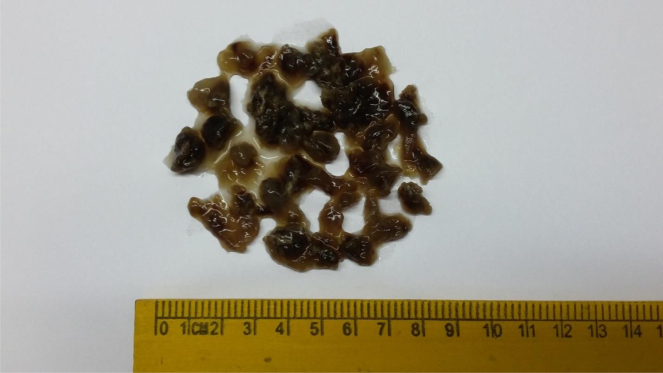
Patent foramen ovale was closed with the pericardial patch using 4 ‘o’ prolene and thereupon the right atrium was sutured. The patient was weaned from cardiopulmonary bypass and the chest was closed routinely. Postoperative course was uneventful. Pathologically, the macroscopic specimen demonstrated the jelly like mass with hemorrhagic areas (Fig. 6). The histopathological findings confirmed the diagnosis of myxoma (Fig. 7). Our patient had no episodes of stroke/TIA after nearly 1 year of follow up following surgery and has full neurological recovery.
Fig. 6.
Gross appearance: macroscopic specimen demonstrated the jelly like mass with hemorrhagic areas.
Fig. 7.
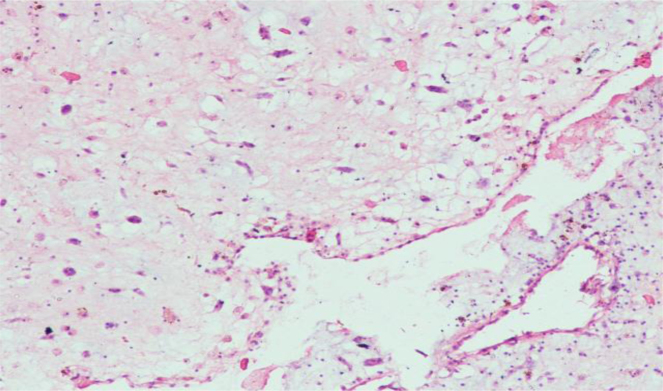
HPE of specimen HPE of the specimen showed loose myxoid areas, composed of spindle cells with myxomatous matrix around them. No evidence of pleomorphism, mitosis or other features suggestive of malignancy.
3. Discussion
Primary heart tumors are rare and the majority of them are atrial myxomas. Only sporadic cases of myxomas arising from the right ventricular outflow tract have been reported in the literature.9, 10 Clinical symptoms of myxomas depend on its position and size, are atypical and vary to a large extent in terms of general symptoms, heart symptoms and embolic events.
A higher frequency of embolization up to 30–40% was reported in western series.11, 12 The majority of patients have a variety of different and a typical symptom. That is why some authors call myxomas “the great masque rader”. Asymptomatic cases are rare. Screening for myxoma is important in cases of family history, in complex myxoma, or Carney disease.13
Patent foramen ovale (PFO) is a common finding in general population; it is not classified as an atrial septal defect. It is anatomically tunnel-like structure between the upper rim of the fossa ovalis limb and the fossa ovalis valve, and is the result of the lack of fusion of the septum primum and septum secundum. The length of the tunnel varies, ranging from 3 to 24 mm, with the mean length of 9 mm.27, 28
PFO in adults does not usually produce a significant shunt. Its potential risk is that it allows paradoxical embolism into the systemic vascular bed in the presence of venous thrombosis or right atrial thrombosis or thrombosis directly inside the PFO tunnel or atrial septal aneurysm, in hypercoagulation state or when using hormonal contraception.
A right-to-left shunt may be transient or intermittent: it is caused by increased right atrial pressure in pulmonary embolism or lung disease but, also, in cough, Valsalva maneuver or diving, and it may also be dependent on a change in position.29
Our patient had atypical symptoms and the diagnosis was made by echocardiography. Echocardiography is non-invasive and allows preoperative diagnosis with fair degree of accuracy. It can rule out tumor in other chambers and there is no risk of tumor embolization. Transthoracic echocardiography can generally be used to determine the location, size, shape, attachment and mobility of a tumor.
The transesophageal approach is particularly helpful in detecting the site of insertion and morphological features of atrial and ventricular myxomas.14 We have come to rely solely on two dimensional echocardiography for preoperative diagnosis and believe that catheterization, a potentially harmful procedure in myxoma, is not indicated for diagnosis.11
However, if coronary artery disease is suspected, or patient's age is greater than 40 years, coronary arteriography is advised to evaluate the coronary arteries. Once the diagnosis of cardiac myxoma is made, the operation should be carried out without delay.15 Surgical excision of right ventricular myxomas must be accomplished as soon as possible after the diagnosis has been established to prevent serious complications such are valvular obstruction, pulmonary embolization and syncope.
Surgical intervention offers the cure for patients with sporadic intracardiac myxomas. Recurrence of a sporadic myxoma is unusual, occurring in 1–3% of cases.16, 17 The risk of recurrence after surgery is correlated with young age, family history of myxoma,18, 19 inadequate resection, intraoperative implantation or multicentre growth. Recently, interleukin-620 and endothelial growth factor21 have been identified as markers of these tumors. The average recurrence occurs about 30 months after removal of the first myxoma.22 Familial myxomas have greater tendency to recur, even many years after the operation. Although only several cases of recurrence of the right ventricular myxoma have been reported so far,23, 24 routine echocardiography control after the operation is advised.
HPE of the specimen showed loose myxoid areas, composed of spindle cells with myxomatous matrix around them. No evidence of pleomorphism, mitosis or other features suggestive of malignancy.
A regular follow up of all patients by non-invasive method is mandatory because the recurrence of myxoma have been documented at various intervals and are not clearly predictable.25 A high incidence of arrythmias and conduction disturbances, both early and late, have been reported by Bateman and colleagues.26 Although the pathophysiology of this was unclear, they were thought to be related to a possible surgical injury to the conduction pathways (biatrial approach) or excessive retraction of the heart (atrial approach). Operative mortality and morbidity is low as reported by others.10, 13, 16
4. Conclusion
The presented case illustrates the usefulness of transesophageal echo-cardiography both in diagnosing and planning surgical approach in patients with the myxomas. It also stresses the importance of surgical excision of the tumor as soon as possible following the diagnosis to prevent serious complications.
These tumors can be excised with a low rate of morbidity and mortality. The prognosis for patients after surgical resection is excellent. This is probably the first case of RV myxoma presenting as recurrent stroke. Our patient had no episodes of stroke/TIA after nearly 1 year of follow up following surgery and has full neurological recovery.
Conflicts of interest
The authors have none to declare.
References
- 1.Thiene G., Valente M., Lombardi M., Basso C. Tumours of the heart. In: Camm A.J., Luscher T.F., Serruys P.W., editors. The ESC Textbook of Cardiovascular Medicine. 2nd ed. Oxford University Press; Oxford: 2009. pp. 735–762. [Google Scholar]
- 2.Mc Allister H.A., Fenoglio J.J. Armed Forces Institute of Pathology; Washington, DC: 1978. Tumours of the Cardiovascular System. Atlas of Tumour Pathology. Second Series. Fascicle 15; pp. 1–25. [Google Scholar]
- 3.Bjessmo S., Ivert T. Cardiac myxoma: 40 years’ experience in 63 patients. Ann Thorac Surg. 1997;63:697–700. doi: 10.1016/s0003-4975(96)01368-9. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez A., Altieri P.I., Marquez E.U., Cox R.A., Castillo M. Massive pulmonary embolism associated with a right ventricular myxoma. Am J Med. 1980;69(5):795–798. doi: 10.1016/0002-9343(80)90455-6. [DOI] [PubMed] [Google Scholar]
- 5.Karagounis A., Sarasam M. Myxoma of free wall of the right ventricle: a case report. J Card Surg. 2005;20(1):73–76. doi: 10.1111/j.0886-0440.2005.05006.x. [DOI] [PubMed] [Google Scholar]
- 6.DePace N.L., Soulen R.L., Kotler M.N., Mintz G.S. Two dimensional echocardiographic detection of intraatrial masses. Am J Cardiol. 1981;48:954–960. doi: 10.1016/0002-9149(81)90364-7. [DOI] [PubMed] [Google Scholar]
- 7.Chitwood W.R., Jr. Clarence Crafoord and the first successful resection of a cardiac myxoma. Ann Thorac Surg. 1992;54:997–998. doi: 10.1016/0003-4975(92)90676-u. [DOI] [PubMed] [Google Scholar]
- 8.Castenada A.R., Varco R.L. Tumours of the heart: surgical considerations. Am J Cardiol. 1968;21:357–362. doi: 10.1016/0002-9149(68)90139-2. [DOI] [PubMed] [Google Scholar]
- 9.Mukadam M.E., Kulkarni H.L., Kumar C.J., Tendolkar A.G. Right ventricular myxoma presenting as right-ventricular outflow tract obstruction: case report and review of the literature. Thorac Cardiovasc Surg. 1994;42(4):243–246. doi: 10.1055/s-2007-1016497. [DOI] [PubMed] [Google Scholar]
- 10.Paraskevaidis I.A., Triantafilou K., Karatzas D., Kremastinos D.T. Right ventricular multiple myxomas obstructing right ventricular outflow tract. J Thorac Cardiovasc Surg. 2003;126(3):913–914. doi: 10.1016/s0022-5223(03)00356-8. [DOI] [PubMed] [Google Scholar]
- 11.Dein J.R., Frist W.H., Stinson E.B. Primary cardiac neoplasms: early and late results of surgical treatment in 42 patients. J Thorac Cardiovasc Surg. 1987;93:502–511. [PubMed] [Google Scholar]
- 12.Larrieu A.J., Jamieson W.R., Tyers G.F. Primary cardiac tumours: experience with 25 cases. J Thorac Cardiovasc Surg. 1982;83:339–348. [PubMed] [Google Scholar]
- 13.Goldstein M.M., Casey M., Carney J.A., Basson C.T. Molecular genetic diagnosis of the familial myxoma syndrome (Carney complex) Am J Med Genet. 1999;86:62–65. doi: 10.1002/(sici)1096-8628(19990903)86:1<62::aid-ajmg12>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 14.Obeid A.I., Marvasti M., Parker F., Rosenberg J. Comparison of transthoracic and transesophageal echocardiography in diagnosis of left atrial myxomas. Am J Cardiol. 1989;63:1006–1008. doi: 10.1016/0002-9149(89)90162-8. [DOI] [PubMed] [Google Scholar]
- 15.Chitwood W.R., Jr. Cardiac neoplasms: current diagnosis, pathology and therapy. J Card Surg. 1988;3:119–154. doi: 10.1111/j.1540-8191.1988.tb00232.x. [DOI] [PubMed] [Google Scholar]
- 16.Centofanti P., Di Rosa E., Deorsola L. Primary cardiac tumours: early and late results of surgical treatment in 91 patients. Ann Thorac Surg. 1999;68:1236–1241. doi: 10.1016/s0003-4975(99)00700-6. [DOI] [PubMed] [Google Scholar]
- 17.Kabbani S.S., Jokhadar M., Meada R. Atrial myxoma: report of 24 operations using biatrial approach. Ann Thorac Surg. 1994;58:483–488. doi: 10.1016/0003-4975(94)92234-9. [DOI] [PubMed] [Google Scholar]
- 18.Farah M.G. Familial cardiac myxomas: a study of relatives of patients with myxoma. Chest. 1994;105:65–68. doi: 10.1378/chest.105.1.65. [DOI] [PubMed] [Google Scholar]
- 19.Van Gelder H.M., O’Brien D.J., Staples E.D., Alexander J.A. Familial cardiac myxoma. Ann Thorac Surg. 1992;53:419–424. doi: 10.1016/0003-4975(92)90261-2. [DOI] [PubMed] [Google Scholar]
- 20.Mendoza C.E., Rosado M.F., Bernal L. The role of interleukin-6 in cases of cardiac myxoma: clinical features, immunologic abnormalities, and a possible role in recurrence. Tex Heart Inst J. 2001;28:3–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Bennet K.R., Gu J.W., Adair T.H., Heath B.J. Elevated plasma concentration of vascular endothelial growth factor in cardiac myxoma. J Thorac Cardiovasc Surg. 2001;122:193–194. doi: 10.1067/mtc.2001.113744. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy P.M., Piehler J.M., Schaff H.V. Significance of multiple, recurrent and complex cardiac myxomas. J Thorac Cardiovasc Surg. 1986;91:389–396. [PubMed] [Google Scholar]
- 23.Segal O.R., Robinson N.M., Timmis A.D. Images in cardiology: recurrent myxoma of the right ventricle. Heart. 2000;84(6):652. doi: 10.1136/heart.84.6.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keeling I.M., Oberwalder P., Anelli-Monti M. Cardiac myxomas: 24 years of experience in 49 patients. Eur J Cardiothorac Surg. 2002;22(6):971–977. doi: 10.1016/s1010-7940(02)00592-4. [DOI] [PubMed] [Google Scholar]
- 25.Hanson E.C., Gili C.C., Razavi M., Loop F.D. Surgical treatment of atrial myxomas: clinical experience and late results in 33 patient's. J Thorac Cardiovasc Surg. 1985;89:298–303. [PubMed] [Google Scholar]
- 26.Bateman T.M., Gray R.J., Raymond M.J., Chaux A., Czer L.S., Matlof J.M. Arrhythmias and conduction disturbances following cardiac operations for removal of LA myxomas. J Thorac Cardiovasc Surg. 1983;86:601–607. [PubMed] [Google Scholar]
- 27.Marshall A.C., Lock J.E. Structural and compliant anatomy of the patent foramen ovale in patients undergoing transcatheter closure. Am Heart J. 2000;140:303–307. doi: 10.1067/mhj.2000.108236. [DOI] [PubMed] [Google Scholar]
- 28.Sievert H., Horvath K., Zadan E. Patent foramen ovale closure in patients with transient ischemic attack/stroke. J Interv Cardiol. 2001;14(2):261–266. doi: 10.1111/j.1540-8183.2001.tb00745.x. [DOI] [PubMed] [Google Scholar]
- 29.Meier B., Lock J.E. Contemporary management of patent foramen ovale. Circulation. 2003;107:5–9. doi: 10.1161/01.cir.0000046073.34261.c1. [DOI] [PubMed] [Google Scholar]