Abstract
The use of Complementary and Alternative Medicine (CAM; 補充與替代醫學 bǔ chōng yǔ tì dài yī xué) has been rapidly increasing among cancer patients. However, this pervasiveness is still largely unexplored among Malaysian cancer patients. The current study aimed to evaluate the patterns of CAM use among cancer patients from a local hospital in Malaysia. In addition, the study focused on the information-seeking behavior and CAM use disclosure to doctors. Of 393 patients, 184 (46.1%) had used CAM for their cancers. CAM usage was significantly associated with gender (p = 0.021), level of education (p = 0.001), employment status (p = 0.02), and monthly income (p < 0.001). Among frequently used CAM were nutritional supplements (n = 77, 41.8%), natural products (n = 74, 40.2%), and multivitamin (n = 62, 33.6%). Friends and family members were the most common source of CAM information (n = 139, 75.5%). Seventy-nine (43%) reported to disclose their CAM use to the health care providers. The most common (n = 63, 34.2%) reason of nondisclosure was “it is not important to discuss it with oncologist.” This study confirmed that CAM use is common among Malaysian cancer patients, thus highlighting a greater need for patient education regarding CAM therapies and their potential interactions with conventional therapies. Although some types of CAM therapies may help patients to cope with emotional distress and improve quality of life, CAM, with no proven efficacy, may pose dangers to patients' health due to interactions with conventional therapies. Doctors and other health care providers including nurses and pharmacists should engage cancer patients in an open nonjudgmental dialog to ascertain CAM use disclosure to their health care providers.
Keywords: alternative medicines, cancer, complementary therapies, disclosure, Malaysia
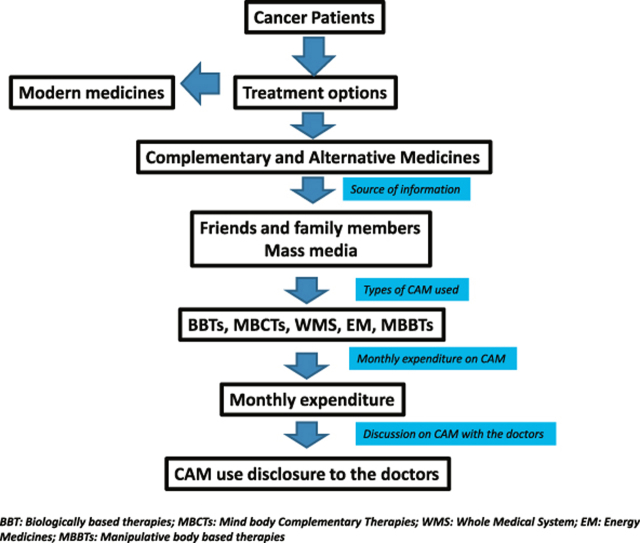
Graphical abstract
1. Introduction
In Malaysia, use of Complementary and Alternative Medicine (CAM; 補充與替代醫學 bǔ chōng yǔ tì dài yī xué) for health maintenance, disease prevention and treatment is prevalent among healthy individuals as well as patients with chronic diseases.1, 2 Particular to cancer, numerous studies reported a significantly high degree of CAM use among the Malaysian population.3, 4 At the same time approximately 80% of the population in African and Asian countries reported CAM as a primary source to cure and prevent disease.5 The cumulative incidence rate of CAM use among cancer patients is in the wide range of 14.5–91%.6, 7 The wide variation is often due to a lack of agreement on definition and dimensions of CAM.8 The National Centre of CAM defines CAM as “a group of diverse medical and healthcare systems, practices, and products that are not currently part of conventional medicine.”9 The use of CAM may be prompted by various factors that eventually direct cancer patients towards CAM. Emotional impact of cancer diagnosis, fear of side effects due to conventional therapies, lack of communication with doctors, and the need of personal control are among the factors associated with CAM use.10, 11 Despite the fact that CAM is used by an increasing number of Malaysians, little information is available regarding the perceptions towards the effectiveness of CAM over conventional therapies, source of information, and disclosure of CAM to the health care providers. This cross-sectional study aimed to determine the use of CAM among cancer patients, sources from where CAM related information is retrieved and CAM disclosure to the health care providers. At the same time evaluating numerous traditional therapies specific to Malaysian culture would be valuable to inform future research priorities.
2. Methods
2.1. Design and settings
The study was designed as a questionnaire based, cross-sectional analysis. A prevalence based sample of 393 cancer patients12 attending the oncology ward at Penang General Hospital, Penang, Malaysia was hereby selected for the study. Adult patients (age > 18 years), having been diagnosed with cancer (any type) at least 6 months ago and not > 5 years postdiagnosis, able to read or understand Malay (national language of Malaysia) or the English language were recruited for 4 months. The survey questionnaire with a cover letter explaining the aims of the study was used for data collection. Each participant was asked to fill in a consent form prior to responding to the survey questionnaire. Each participant was asked, “Have you ever used CAM for your cancer?” This question was considered as a screening question. Participants were than instructed verbally to follow the instructions on the questionnaire. The contents of the cover letter assured patients that refusal to participate in the study or information regarding the CAM use will not be disclosed to their physicians.
2.2. Ethical approval
Ethical approval was obtained by the Medical Research Ethics Committee, Ministry of Health, Malaysia.
2.3. Study tool development
For an in depth and rational analysis, two qualitative studies exploring patients' beliefs towards cancer, treatment seeking behavior, perceptions towards CAM effectiveness for cancer, and reasons of CAM use13, 14 were undertaken prior to the commencement of the current study. The study questionnaire was thus constructed by the research team through an extensive literature review and results from the qualitative phases.15, 16, 17 However, the biggest challenge faced by the research team was in acquiring a complete and well defined list of CAM used in cancer. CAM is a very broad term and getting patients' response for each CAM was exhausting and time consuming. Therefore, a simple list of CAM modalities were provided in the questionnaire; however, patients were given the opportunity to add in any “out of the list” CAM during the study. The final questionnaire was comprised of demographic and disease characteristics, monthly CAM expenditure and CAM recommendations, and CAM disclosure to the doctors. The study questionnaire was initially developed in English. Since the Malay language is widely spoken by Malaysians, the questionnaire was than translated into Malay language by using standard translation procedure.18 The face and content validity of the questionnaire was established by experts from School of Pharmaceutical Sciences, Universiti Sains Malaysia. Internal consistency was assessed by using Cronbach α (α = 0.7) and was found to be in acceptable ranges.19 The contents, clarity of language, ease of administration, and appropriateness of the items in line with the study's objectives were assessed prior to the pilot study. The study questionnaire was piloted among 20 cancer patients for its acceptability and consistency. Little modification in the questionnaire was needed after the pilot study. Data from the pilot study was not added to the final analysis. As the consistency and validity of the study questionnaire was stabilized, the instrument was made available for data collection.
2.4. Measures
The study questionnaire comprised four sections including demographics and disease characteristics, details of CAM use, source of CAM information, and disclosure of CAM to the doctors. CAM users were defined as patients continually using at least one form of CAM therapy for at least 1 month after the diagnosis of cancer.
2.5. Data analysis
Descriptive statistics were used for types of CAM, prevalence of CAM use, and CAM disclosure to the doctors. Chi-square test was applied to estimate the association among independent study variables and CAM utilization. For all statistical analysis, p < 0.05 was considered as significant. Data were analyzed by using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Demographic and disease characteristics
The mean age ± standard deviation of the respondents was 53.92 ± 13.0 years. Of these respondents, the cohort was dominated by women 254 (64.6%). Respondents were split between Malay 190 (48.3%), Chinese 136 (34.6%), and Indian 60 (15.3%) ethnic groups. The demographic and disease related characteristics of the study participants are summarized in Table 1. Only 82 (20.9%) patients reported having a private medical insurance. All of the study participants were receiving treatments in government hospitals where most of the treatment are provided free of charge. The top three primary cancer sites were breast cancer, gastrointestinal cancers (colon, rectum, stomach, and intestine) and gynecological cancers (ovarian, cervical, uterine etc.). A total of 268 (68.18%) participants reported their cancer stage to be between slightly advanced to very advance at the time of interview. In addition 134 (34%) received chemotherapy, surgery, and radiotherapy; 67 (17%) received surgery and chemotherapy; and 57 (14.5%) were on chemotherapy alone. Among all the demographic variables, CAM usage was significantly associated with gender (p = 0.021) level of education (p = 0.001), employment status (p = 0.02), and monthly income (p < 0.001).
Table 1.
Demographic and disease characteristics of the participants.
| Variables | CAM users n = 184 |
CAM nonusers n = 209 |
χ² p |
|---|---|---|---|
| n (%) | n (%) | ||
| Age (y), mean ± SD = 53.92 ± 13.0 | |||
| 18–27 | |||
| 28–37 | 7 (3.8) | 5 (2.3) | 0.383 |
| 38–47 | 13 (7.0) | 16 (7.6) | |
| 48–57 | 38 (20.6) | 35 (16.7) | |
| 58–67 | 57 (30.9) | 61 (29.1) | |
| 68–77 | 53 (28.8) | 56 (26.7) | |
| 78–88 | 16 (8.6) | 36 (17.2) | |
| Gender | |||
| Male | 52 (28.2) | 82 (40.1) | 0.021 |
| Female | 132 (71.7) | 128 (59.8) | |
| Race | |||
| Malay | 91 (49.4) | 99 (47.3) | 0.127 |
| Chinese | 70 (38.0) | 66 (31.5) | |
| Indian | 20 (10.8) | 40 (19.1) | |
| Others | 3 (1.6) | 4 (1.9) | |
| Religion | |||
| Islam | 94 (51.0) | 100 (47.8) | 0.051 |
| Buddhism | 62 (33.6) | 63 (30.1) | |
| Hinduism | 16 (8.6) | 36 (17.2) | |
| Christianity | 10 (5.4) | 4 (1.9) | |
| Others | 1 (0.5) | 3 (1.4) | |
| Atheist | 1 (0.5) | 3 (1.4) | |
| Educational status | |||
| Primary | 42 (22.8) | 71 (33.9) | 0.001 |
| Secondary | 91 (49.4) | 100 (47.8) | |
| Diploma/matriculation | 19 (10.3) | 9 (4.3) | |
| University degree | 17 (9.2) | 5 (2.3) | |
| Postgraduate degree | 3 (1.6) | 2 (0.9) | |
| Never go to school | 12 (6.5) | 22 (10.5) | |
| Marital status | |||
| Unmarried | 19 (10.3) | 22 (10.5) | 0.549 |
| Married | 155 (84.2) | 170 (81.3) | |
| Divorced | 4 (2.17) | 3 (1.4) | |
| Widowed | 6 (3.2) | 13 (6.2) | |
| Others | 0 (0) | 1 (0.4) | |
| Employment status | |||
| Employed | 60 (32.6) | 45 (21.5) | 0.021 |
| Unemployed | 43 (23.3) | 76 (36.3) | |
| Retired | 38 (20.6) | 36 (17.2) | |
| Home maker | 39 (21.1) | 48 (22.9) | |
| Student | 2 (1.0) | 4 (1.9) | |
| Others | 2 (1.0) | 0 (0) | |
| Monthly income in MYR/month | |||
| No income | 95 (51.6) | 155 (74.1) | <0.001 |
| < 1000 | 29 (15.7) | 27 (12.9) | |
| 1000–3000 | 40 (21.7) | 24 (11.4) | |
| > 3000 | 20 (10.8) | 3 (1.4) | |
| Primary cancer site | |||
| Don't know | 0 (0) | 2 (0.9) | 0.245 |
| Breast | 79 (42.9) | 64 (30.6) | |
| GIT cancersa | 38 (20.6) | 50 (23.9) | |
| Gynaecological cancersb | 16 (8.6) | 21 (10.0) | |
| Lung | 13 (7.0) | 21 (10.0) | |
| Nasopharynx | 12 (6.5) | 11 (5.2) | |
| Prostate gland | 7 (3.8) | 8 (3.8) | |
| Thyroid | 3 (1.6) | 5 (2.3) | |
| Othersc | 16 (8.6) | 27 (12.9) | |
| Duration of disease (y), mean ± SD = 2.0 ± 0.89 | |||
| 0.5–1 | 63 (34.2) | 84 (40.1) | 0.147 |
| 1–3 | 66 (35.8) | 83 (39.7) | |
| 3–5 | 43 (23.3) | 31 (14.8) | |
| Don't know/not sure | 12 (6.5) | 11 (5.2) | |
| Cancer stage | |||
| Very advanced | 52 (32.6) | 41 (20.5) | 0.051 |
| Slightly advanced | 85 (38.5) | 101 (44.9) | |
| Not advanced at all | 31 (16.3) | 34 (16.7) | |
| Undetermined | 8 (4.3) | 14 (6.2) | |
| Don't know/not sure | 8 (4.3) | 19 (11.4) | |
CAM = complementary and alternative medicines; SD = standard deviation.
Gastrointestinal tract cancers include colon, rectum, stomach, and intestine.
Gynaecological cancers include cervix, uterine and ovarian cancers.
Other cancer sites include carcinoma of tongue, germ cell, skin, bone, brain, and lymphoma.
3.2. CAM use
Out of 393 respondents, 184 (46.1%) had used CAM for their condition. More than half of the CAM users 126 (68.5%) were actively reported to use one or more types of CAM at the time of interview. The number of CAM therapies used by the participants ranged from a minimum of one to a maximum of eight therapies at one time. Beside patients' own initiative [33 (17.9%) patients] to search and decide to use specific CAM, friends and family members were among the most important sources of information for CAM, [139 (75.5%) patients]. Only 21 (11.4%) patients reported that they obtained information from the oncologists regarding CAM. An estimation of monthly expenditure and sources of information on CAM is summarized in Table 2. When asked about any side effects suffered due to CAM therapies only 24 (13%) patients reported “yes”, and 145 (78.8%) patients reported “no”, while 15 (8.2%) patients stated “difficult to judge” as the side effects were due to CAM therapies or the conventional therapies, or are the symptoms of cancer itself. The nature and severity of side effects due to CAM were not recorded, so no inferential conclusion can be made on potential harmful effects of specific CAM therapies on cancer patients.
Table 2.
Monthly complementary and alternative medicine (CAM) expenditure and source of information (n = 184).
|
n = 184 n (%) |
|
|---|---|
| Monthly expenditure on CAM in MYR | |
| < 50 | 18 (9.8) |
| 50–100 | 26 (14.1) |
| 101–500 | 43 (23.4) |
| 501–1000 | 13 (7.1) |
| > 1000 | 4 (2.2) |
| Not sure | 80 (43.5) |
| Sources of information about CAMa | |
| Friends or family | 139 (75.5) |
| Own free will | 33 (17.9) |
| Mass media | 23 (12.5) |
| Health care providers | 21 (11.4) |
| Cancer survivors | 13 (2.2) |
| CAM vendors | 4 (7.9) |
MYR = Malaysian Ringgit.
Total percentage may not be 100% due to the choice given for multiple responses.
3.3. Types of CAM used by study participants
Nutritional supplements (n = 77, 41.8%), herbal products (n = 74, 40.2%) and multivitamin (n = 62, 33.6%) were the most frequent CAM used by the patients. The types of CAM utilized by the study participants are summarized in Table 3. Among herbs, Sabah snake grass (Clinathanus nutans), and betel nut (Areca catechu)/betel leaf (Piper betle) were identified the most common herbs used by the participants. Prayers for health reasons were used by 51 (27.7%) patients. However, 20 (10.8%) respondents reported visiting spiritual or religious healers as CAM.
Table 3.
Types of complementary and alternative medicines (CAM) utilized by the study participants.a
| CAM categories |
n = 184 n (%) |
|---|---|
| Biologically based therapies | |
| Nutritional supplements (vitamins, mineral, enzymes) | 134 (72.8) |
| Special diet (herbs, animal products, juices) | |
| Mind–body medicines | |
| Prayers for health reasons/spirituality | 75 (40.8) |
| Others (meditation, T'ai chi (太極拳 tài jí quán), music, yoga, Qigong (氣功 qì gōng), hypnotherapy, Reiki) | |
| Whole medical system | |
| Traditional Chinese medicine (中醫 zhōng yī; TCM) | 68 (36.9) |
| Traditional Malay therapies | |
| Homeopathy | |
| Ayurveda | |
| Energy medicines | |
| Light therapy, Ozone therapy | 3 (1.6) |
| Manipulative and body-based therapies | |
| Massage, herbal baths (藥浴 yào yù)/aromatherapy | 2 (1.0) |
Total percentage may not be 100% due to the choice given for multiple responses.
3.4. Disclosure of CAM use to oncologists
Although CAM disclosure rate was 43%, only 62 (33.7%) of the respondents reported that their doctors had specifically asked about CAM use. The reasons of CAM disclosure and response of doctors upon CAM disclosure are summarized in Table 4. The most common reason given for nondisclosure by the respondents was “it is not important for the doctors to know about CAM use” (n = 63, 34.2 %).
Table 4.
CAM disclosure to the health care providers.
| Variables | n (%) |
|---|---|
| Did your doctors asked you about your CAM use? (n = 184) | |
| Yes | 62 (33.7) |
| No | 117 (63.6) |
| Not sure | 5 (2.7) |
| Did you disclose your CAM use to your doctors? (n = 184) | |
| Yes | 79 (43) |
| No | 105 (57.1) |
| How did you doctor respond upon your CAM disclosure? (n = 79) | |
| Agreed of CAM use | 28 (35.4) |
| Disagreed of CAM use | 15 (18.9) |
| Neutral about CAM use | 36 (45.5) |
| Most important reasons of CAM non-disclosure (n = 105) | |
| Not important for doctors to know about CAM use | 67 (63.8) |
| They never ask, I never tell | 15 (14.2) |
| Doctors have little knowledge about CAM | 9 (8.5) |
| Fear of CAM use disapproval by the doctors | 8 (7.6) |
| Fear of termination of conventional therapies | 6 (5.7) |
4. Discussion
The purpose of this study was to discern the pattern of CAM use among Malaysian cancer patients. About 46.1% of the participants reported using CAM which is similar to what has been found among cancer patients in other studies.20, 21 Although there are studies that have reported a prevalence that is double the figure reported in this study,7, 22 this could be due to a difference of study instrument (e.g., differences in the classification of CAM) and the study sample. The majority of participants were diagnosed with cancer during 2011: perhaps they may not have had enough opportunity or time to think about CAM use. Keeping this limitation in mind, the percentage of CAM use may change if the same patients are interviewed after 1 year or 2 years.
From our sample, female breast cancer patients were the highest among CAM users. Monthly income, employment, and educational status were significantly associated with CAM use in the current study. These results are in accordance to what was reported from previous studies.17, 18, 19 Although no significant association was found between the stage of cancer and CAM use, the percentage use of CAM was high among patients who had more advanced disease. This may be explained by the fact that patients at the terminal stages are often desperate to survive and usually try every possible method available to cure the cancer.23 Several studies have reported patients of Malay ethnicity amongst the highest of CAM for cancer3, 4; however, no significant association was found between ethnicity and CAM use, although female Malay patients reported the highest CAM usage for cancer.
Vitamins and dietary supplements were the most frequent types of CAM used by the study participants. The majority of them were using megavitamin and health supplements such as “fit for life”, MegaV, etc. Cancer patients reported to utilize vitamin and health supplements to reduce cancer symptoms, unwanted effects of chemotherapies such as anemia, and for health maintenance.22, 24, 25 Chemotherapy induced anemia and its impact on cancer patients' quality of life have been studied previously.26, 27 Blood transfusion and epoietin are among the few remedies to reduce the effects of chemotherapy on patients' hemoglobin (Hb) levels28; however, the potential dangers of blood transfusion are important to consider prior to making decisions. In such condition, use of multivitamin and food supplements rich in iron contents may benefit cancer patients to reduce chemotherapy-induced side effects, in particular low Hb levels. Patients can be encouraged to use products with proven efficacy to improve Hb levels. At the same time patients should be reminded that these supplements do not guaranties a cure to cancer. During the past decade, enforcement activities conducted by the Traditional and Complementary Medicine division, of the Malaysian Ministry of Health have reported that false claims have been made on numerous CAM therapies available in Malaysian markets.29 As the majority of CAM users perceived CAM to be an effective agent to cure cancer, it is important to ensure the validity and reliability of the claims made by the manufacturers.
At present herbal products are gaining popularity in the treatment and prevention of various diseases. Specific to cancer, studies reported that herbal products are mainly used to slow down the disease progression and to relive symptoms.30, 31 Similarly, numerous local herbs such as Sabah snake grass (C. nutans), betel nut (A. catechu), betel leaf (P. betle) were used by the study participants. For example, Sabah snake grass abundantly grows in Malaysia and local traditions claims a cure to cancer.32, 33 However, this Thai medicinal plant is well documented for its anti-inflammatory34 actions as well as activities against herpes virus.35 Abundant use of this plant by Malaysian cancer patients may offer opportunities to ethnopharmacology researchers to evaluate the efficacy and safety of this herb for cancer.
There is a growing interest towards the beneficial effects of mind body therapies such as meditation, yoga, and faith-healing practices to relieve symptoms such as anxiety, emotional distress, nausea, and pain, and to rejuvenate mentally.36 Prayers for health reasons are not commonly included as CAM therapies; however, studies that have categorized prayers as CAM have shown a higher percentage of CAM use among cancer patients.37, 38 The inclusion of spiritual practices as CAM may reflect either spiritual beliefs towards the causes of cancer or the easy access to spiritual therapies with minimal cost or both.14, 39 The emotional impact of a cancer diagnosis, uncertainty, and fear of death may lead patients to turn to spiritual help as a way of coping or to derive comfort. Malaysian policy on integrative medicines encourages the use of noninvasive mind body soul therapies such as hypnotherapy and psychotherapy therapies to help patients cope with the psychological effects of cancer.29 To date, nine government hospitals all over the country offer traditional and complementary therapies to the patients with chronic diseases including cancer. Despite oncologists' negative attitude towards CAM, it is evident that some of the CAM therapies such as acupuncture, chiropractic, and massage therapies receive recognition by physicians to relive symptoms of cancer.40, 41 However, oncologists' perceptions towards CAM integration have never been evaluated in Malaysian culture. There is an immediate need to evaluate health care workers' use and attitude to CAM in Malaysia to support government efforts towards integrative medicines.
As reported previously, friends and family members were the common source of receiving advice and recommendations about CAM among the study participants.42 Although health care providers should be the most preferable source of information regarding CAM.43, 44 only a few participants reported seeking advice from them. The physicians' willingness to talk about CAM, and their readiness to respond to patients' queries regarding CAM have yet to be evaluated in Malaysia. CAM disclosure rate in this study was 43%, which is slightly higher than what was reported previously.45 The reason of nondisclosure highlights the lack of importance placed on the physicians' role in dealing with CAM as only in very few cases did the physician initiate the dialogue of CAM use. It also indicates patients' lack of knowledge regarding harmful interactions of CAM with conventional therapies. This could indicate that there may be inadequate information available about CAM for Malaysian health care providers. A reluctance to discuss CAM openly with patients can result in a less than optimal health care delivery because interactions between CAM and conventional therapies may be missed.
4.1. Limitations
The study has some limitations. It focused on patients already receiving conventional treatment for cancer. Investigating prevalence of CAM use among patients who have decided to forgo conventional therapies in favor of CAM may highlight different issues regarding perceived effectiveness of CAM and conventional therapies. Furthermore, the study was conducted in one hospital of Penang state and further research is required to generalize the findings to the entire Malaysian population. The results are subjected to recall bias for CAM use and its disclosure to the health care providers.
5. Conclusion
This study confirmed that CAM use is common among Malaysian cancer patients thus highlighting a greater need of patient education regarding CAM therapies and their potential interactions with biomedical treatment. The results also identified some local herbs claimed to cure cancer, which opens the platform to more research and investigation to prove the safety and efficacy of these herbs to cure cancer. Reasons of CAM nondisclosure to the health care providers demands a need to promote an open nonjudgmental discussion by the health care professionals. Health care providers must be aware of patients' concerns regarding CAM.
Conflict of interest
All contributing authors declare no conflict of interest.
Acknowledgments
We thank all the patients who participated in the study. We would also like to thank all students who helped in data collection.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Siti Z.M., Tahir A., Farah A.I. Use of traditional and complementary medicine in Malaysia: a baseline study. Complement Ther Med. 2009;17:292–299. doi: 10.1016/j.ctim.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Ganasegeran K., Rajendran A.K., Al-Dubai S.A.R. Psycho-socioeconomic factors affecting complementary and alternative medicine use among selected rural communities in Malaysia: a cross-sectional study. PloS One. 2014;9:e112124. doi: 10.1371/journal.pone.0112124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lua P.L. The role of complementary indigenous Malay therapies. Perspectives from palliative care patients. J Complement Integr Med. 2011;8:16. doi: 10.2202/1553-3840.1369. [DOI] [PubMed] [Google Scholar]
- 4.Hamidah A., Rustam Z.A., Tamil A.M., Zarina L.A., Zulkifli Z.S., Jamal R. Prevalence and parental perceptions of complementary and alternative medicine use by children with cancer in a multi-ethnic Southeast Asian population. Pediatr Blood Cancer. 2009;52:70–74. doi: 10.1002/pbc.21798. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (WHO) December 2008. Media Centre. Traditional Medicine, Fact sheet N134.http://www.who.int/mediacentre/factsheets/2003/fs134/en/ Available from: Accessed November 2011. [Google Scholar]
- 6.Sibbritt D., Adams J., Easthope G., Young A. Complementary and alternative medicine (CAM) use among elderly Australian women who have cancer. Support Care Cancer. 2003;11:548–550. doi: 10.1007/s00520-003-0490-4. [DOI] [PubMed] [Google Scholar]
- 7.Yates J.S., Mustian K.M., Morrow G.R. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Support Care Cancer. 2005;13:806–811. doi: 10.1007/s00520-004-0770-7. [DOI] [PubMed] [Google Scholar]
- 8.Shih V., Chiang J.Y.L., Chan A. Complementary and alternative medicine (CAM) usage in Singaporean adult cancer patients. Ann Oncol. 2009;20:752–757. doi: 10.1093/annonc/mdn659. [DOI] [PubMed] [Google Scholar]
- 9.National Centre for Complementary and Alternative Medicine. Expanding Horizons of Health Care. What is CAM? Available from: http://nccam.nih.gov/health/.Accessed November 2011.
- 10.Sirois F.M., Gick M.L. An investigation of the health beliefs and motivations of complementary medicine clients. Soc Sci Med. 2002;55:1025–1037. doi: 10.1016/s0277-9536(01)00229-5. [DOI] [PubMed] [Google Scholar]
- 11.Verhoef M.J., White M.A. Factors in making the decision to forgo conventional cancer treatment. Cancer Pract. 2002;10:201–207. doi: 10.1046/j.1523-5394.2002.104002.x. [DOI] [PubMed] [Google Scholar]
- 12.Daniel W.W. 7 ed. John Wiley & Sons; New York: 1999. Biostatistics: A Foundation for Analysis in the Health Sciences. [Google Scholar]
- 13.Farooqui M., Hassali M.A., Shatar A.K., Shafie A.A., Seang T.B., Farooqui M.A. A qualitative exploration of Malaysian cancer patients' perspectives on cancer and its treatment. BMC Public Health. 2011;11:525. doi: 10.1186/1471-2458-11-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farooqui M., Hassali M.A., Abdul Shatar A.K., Shafie A.A., Seang T.B., Farooqui M.A. Complementary and alternative medicine (CAM) use by Malaysian oncology patients. Complement Ther Clin Pract. 2012;18:114–120. doi: 10.1016/j.ctcp.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Boon H., Stewart M., Kennard M.A. Use of complementary/alternative medicine by breast cancer survivors in Ontario: prevalence and perceptions. J Clin Oncol. 2000;18:2515. doi: 10.1200/JCO.2000.18.13.2515. [DOI] [PubMed] [Google Scholar]
- 16.Yates P.T., Beadle G., Clavarino A. Patients with terminal cancer who use alternative therapies: their beliefs and practices. Social Health Illn. 1993;15:199–216. [Google Scholar]
- 17.Hyodo I., Amano N., Eguchi K. Nationwide survey on complementary and alternative medicine in cancer patients in Japan. J Clin Oncol. 2005;23:2645–2654. doi: 10.1200/JCO.2005.04.126. [DOI] [PubMed] [Google Scholar]
- 18.Behling O., Law K.S. Sage Publications, Inc.; London: 2000. Translating Questionnaires and Other Research Instruments: Problems and Solutions. [Google Scholar]
- 19.Santos J.R.A. Cronbach's alpha: a tool for assessing the reliability of scales. J Extension. 1999;37:1–5. [Google Scholar]
- 20.Swisher E.M., Cohn D.E., Goff B.A. Use of complementary and alternative medicine among women with gynecologic cancers. Gynecol Oncol. 2002;84:363–367. doi: 10.1006/gyno.2001.6515. [DOI] [PubMed] [Google Scholar]
- 21.Helyer L., Chin S., Chui B. The use of complementary and alternative medicines among patients with locally advanced breast cancer—a descriptive study. BMC Cancer. 2006;6:39. doi: 10.1186/1471-2407-6-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kremser T., Evans A., Moore A. Use of complementary therapies by Australian women with breast cancer. Breast. 2008;17:387–394. doi: 10.1016/j.breast.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 23.Shen J., Andersen R., Albert P. Use of complementary/alternative therapies by women with advanced-stage breast cancer. BMC Complement Altern Med. 2002;2:8. doi: 10.1186/1472-6882-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Micke O., Bruns F., Glatzel M. Predictive factors for the use of complementary and alternative medicine (CAM) in radiation oncology. Eur J Integ Med. 2009;1:19–25. [Google Scholar]
- 25.Sewitch M.J., Rajput Y. A literature review of complementary and alternative medicine use by colorectal cancer patients. Complement Ther Clin Pract. 2010;6:52–56. doi: 10.1016/j.ctcp.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Glaspy J. Anemia and fatigue in cancer patients. Cancer. 2001;92:1719–1724. doi: 10.1002/1097-0142(20010915)92:6+<1719::aid-cncr1503>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 27.Groopman J.E., Itri L.M. Chemotherapy-induced anemia in adults: incidence and treatment. J Natl Cancer Inst. 1999;91:1616–1634. doi: 10.1093/jnci/91.19.1616. [DOI] [PubMed] [Google Scholar]
- 28.Estrin J.T., Schocket L., Kregenow R., Henry D.H. A retrospective review of blood transfusions in cancer patients with anemia. Oncologist. 1999;4:318–324. [PubMed] [Google Scholar]
- 29.Ministry of Health Malaysia. National Policy on Traditional/Complementary Medicine. Available from: http://tcm.moh.gov.my/v4/. Accessed November 2011.
- 30.Afifi F.U., Wazaify M., Jabr M., Treish E. The use of herbal preparations as complementary and alternative medicine (CAM) in a sample of patients with cancer in Jordan. Complement Ther Clin Pract. 2010;16:208–212. doi: 10.1016/j.ctcp.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Ali-Shtayeh M.S., Jamous R.M., Jamous R.M. Herbal preparation use by patients suffering from cancer in Palestine. Complement Ther Clin Pract. 2011;17:235–240. doi: 10.1016/j.ctcp.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Sabah Snake Grass. Available from: http://www.sabahsnakegrassherb.com/2013/03/present-for-nutans-also-known-as-sabah.html. Accessed December 2013.
- 33.Herbal Cancer Treatment: Sabah Snake Grass. Available from: http://goodguy.hubpages.com/hub/Herbal-cure-for-cancer. Accessed February 2012.
- 34.Wanikiat P., Panthong A., Sujayanon P., Yoosook C., Rossi A.G., Reutrakul V. The anti-inflammatory effects and the inhibition of neutrophil responsiveness by Barleria lupulina and Clinacanthus nutans extracts. J Ethnopharmacol. 2008;116:234–244. doi: 10.1016/j.jep.2007.11.035. [DOI] [PubMed] [Google Scholar]
- 35.Yoosook C., Panpisutchai Y., Chaichana S., Santisuk T., Reutrakul V. Evaluation of anti-HSV-2 activities of Barleria lupulina and Clinacanthus nutans. J Ethnopharmacol. 1999;67:179–187. doi: 10.1016/s0378-8741(99)00008-2. [DOI] [PubMed] [Google Scholar]
- 36.Vadiraja H.S., Rao M.R., Nagarathna R. Effects of yoga program on quality of life and affect in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Complement Ther Med. 2009;17:274–280. doi: 10.1016/j.ctim.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Rezaei M., Adib-Hajbaghery M., Seyedfatemi N., Hoseini F. Prayer in Iranian cancer patients undergoing chemotherapy. Complement Ther Clin Pract. 2008;14:90–97. doi: 10.1016/j.ctcp.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 38.Chui P.L., Abdullah K.L., Wong L.P., Taib N.A. Prayer-for-health and complementary alternative medicine use among Malaysian breast cancer patients during chemotherapy. BMC Complement Altern Med. 2014;14:425. doi: 10.1186/1472-6882-14-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mao J.J., Farrar J.T., Xie S.X., Bowman M.A., Armstrong K. Use of complementary and alternative medicine and prayer among a national sample of cancer survivors compared to other populations without cancer. Complement Ther Med. 2007;15:21–29. doi: 10.1016/j.ctim.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 40.Johnstone P.A. Acupuncture as cancer symptom therapy: what a difference a decade makes. J Acupunct Meridian Stud. 2011;4:209–213. doi: 10.1016/j.jams.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 41.Corbin Winslow L., Shapiro H. Physicians want education about complementary and alternative medicine to enhance communication with their patients. Arch Intern Med. 2002;162:1176–1181. doi: 10.1001/archinte.162.10.1176. [DOI] [PubMed] [Google Scholar]
- 42.Algier L.A., Hanoglu Z., Ozden G., Kara F. The use of complementary and alternative (non-conventional) medicine in cancer patients in Turkey. Eur J Oncol Nurs. 2005;9:138–146. doi: 10.1016/j.ejon.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 43.Verhoef M., Trojan L., Armitage G., Carlson L., Hilsden R.J. Complementary therapies for cancer patients: assessing information use and needs. Chronic Dis Can. 2009;29:80–88. [PubMed] [Google Scholar]
- 44.Little C.V. Simply because it works better. Exploring motives for the use of medical herbalism in contemporary UK health care. Complement Ther Med. 2009;17:300–308. doi: 10.1016/j.ctim.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 45.Thomson P., Jones J., Evans J.M., Leslie S.L. Factors influencing the use of complementary and alternative medicine and whether patients inform their primary care physician. Complement Ther Med. 2012;20:45–53. doi: 10.1016/j.ctim.2011.10.001. [DOI] [PubMed] [Google Scholar]