Abstract
BACKGROUND: Small intestinal neuroendocrine neoplasm (SI-NEN) proliferation is quantified by Ki67 measurements which capture G1-G2M phases of the cell cycle. G0 and early G1 phases, typical of slow-growing cells, can be detected by minichromosome maintenance protein (MCM) expression. We hypothesized that these replication licensing markers may provide clinically relevant information to augment Ki67 in low-grade neuroendocrine neoplasia. METHODS: Immunohistochemical staining (IHC), Western blot analysis, quantitative polymerase chain reaction, and copy number variations of MCM2, MCM3, and Ki67 were undertaken in SI-NENs (n = 22). MCM and Ki67 expression was compared by Kaplan-Meier survival analysis (tissue microarray, independent set [n = 55]). Forty-three pancreatic NENs and 14 normal tissues were included as controls. RESULTS: In SI-NENs, MCM2 (mean: 21.2%: range: 16%-25%) and MCM3 (28.7%: 22%-34%) were detected in significantly more cells than Ki67 (2.3%: 0%-7%, P < .01). MCM2 mRNA correlated with Ki67 IHC (P < .05). MCM3 protein expression was higher in metastases (38-fold) than in normal small intestine (P = .06) and was largely absent in normal neuroendocrine cells. There was considerable variation at the MCM copy number level (0-4 copies). MCM3 expression in proliferating cells significantly predicted overall survival (P < .002). Combinations of Ki67 and MCM2/3 in algorithms differentiated low and higher proliferative lesions (overall survival: 12 vs 6.1 years, P = .06). MCM expression was not informative in pancreatic NENs. CONCLUSION: MCMs are expressed in a higher proportion of NEN cells than Ki67 in slow-growing small intestinal lesions and correlate with survival. Assessment can be used to augment Ki67 to improve prognostic classification in these low-grade tumors.
Introduction
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) are increasing in incidence and prevalence [1] and exhibit significant heterogeneity in outcome, so prognostic tools are of critical importance. Currently, the most useful prognostic clinicopathological variable is tumor cell proliferation. Assessment of proliferative indices is well accepted and forms the basis for the current grading classification [2]. The Ki67% is prognostic for survival in pancreatic NENs [3], [4] and has value in SI-NENs [2], [5]. Although the index can predict disease progression in the latter [6], G1 and G2 grading is not always clearly distinguishable [7]. One reason for this may be that the proportion of cells that are “positive” is low in both measures, i.e., the lowest-grade NET G1 is defined by <2 mitosis per 10 high-powered fields or ≤2% Ki67-positive cells per 2000 tumor cells [2]. There is consequently a loss of discriminative sensitivity at the lower end of the index. The requirement to detect single positive cells in several high-powered fields is difficult and can significantly alter grade assessment, thereby influencing therapeutic strategy. Although digital approaches to quantitating the Ki67 index are available and are expected to play a role in the future [8], there remains a need to identify proliferative markers that are expressed in a higher proportion of cells. This will confer added accuracy to the grading of tumors with a low proliferative index.
Minichromosome maintenance (MCM) proteins are proliferative markers whose function has been well described [9], [10]. MCMs (2, 3, 4, 5, 6, and 7) combine to form the MCM complex which has a crucial role in the replication of DNA; it is required both for the initiation of transcription forks at DNA replication origins and for the maintenance of the transcription fork as the genome is duplicated [9]. Mitosis can only progress once the MCM complex is unbound, which ensures that a single copy of DNA segregates into each daughter cell [11]. MCMs have a second, related function; they assist in chromatin unwinding at the replication forks prior to transcription due to their inherent helicase activity [10]. These well-characterized functions contrast with our understanding of Ki67 whose function remains poorly known [12].
MCM expression has been examined as a prognostic [10] and proliferative [13], [14] marker in many epithelial malignancies and compared to Ki67. Correlations between Ki67 and MCM using immunohistochemistry (IHC) have been demonstrated for MCM2 in colorectal [15], [16], [17], lung [18], and esophageal cancers [19] as well as in endocrine cancers such as adrenocortical [20] and thyroid carcinoma [21]. MCM3 expression has been associated with Ki67 in melanoma [22] and ovarian cancer [23]. These results support MCMs as proliferative markers. MCM2/3 expression is prognostic for survival in both renal carcinoma [24] and cutaneous T-cell lymphomas [25].
We hypothesized that MCMs would be detectable in NENs and provide prognostic information, particularly in slow-growing tumors. We therefore examined MCM2 and MCM3 expression in GEP-NENs and in normal neuroendocrine cells from which these tumors are derived [26]. The aims were to determine, firstly, whether expression was elevated in NENs compared to normal neuroendocrine cells and, secondly, whether this information was prognostic of survival. In addition, we sought to compare its predictive values with the current clinical standard, Ki67.
Material and Methods
All samples were collected with permission of the Ethics Committees of Yale University School of Medicine (USA) and the University of Heidelberg (Germany).
Small Intestinal NENs
Fresh frozen tumor tissue was collected from 22 SI NENs and normal small intestinal mucosa (n = 14) for the assessment of MCM mRNA, copy number, and protein expression (set 1). These included 13 primary tumors and 9 metastases and were graded as G1 (n = 16) and G2 NETs (n = 6) [2]. Samples were predominantly Caucasians (95%), with a similar gender distribution (M:F 12:10). The average age at diagnosis was 53.2 years (range: 35-66). A tissue microarray (TMA) including 55 SI-NENs (previously described in detail [27]) was included as an independent set (set 2) to quantify immunostaining using the Automated Quantitative Analysis (AQUA) protocol [27], [28] and evaluate whether expression correlated with overall survival (OS). Samples on the TMA were predominantly obtained from Caucasians (84%), with an even gender distribution (M:F 27:28). The average age at diagnosis was 62.1 years (range: 40-89), and the median follow-up was 6.9 years (range: 6 days to 26.3 years). All tumors were grade 1 (Ki67 ≤ 2%).
Pancreatic NENs
The pancreatic NEN data set of fresh frozen tumor tissue (n = 43, 38 primaries, 5 metastases) has been described [29]. Samples were predominantly female (65%); the average age at diagnosis was 59.1 years (range: 13-74). Tumors were nonfunctional (63%); one was MEN-1 (insulinoma). Tumors were graded as G1 (n = 18), G2 (n = 23), and G3 (n = 3). These samples, as well as normal pancreatic tissue (n = 10), were also evaluated for MCM expression (set 3).
RNA isolation and reverse transcription
Messenger RNA was extracted and converted to cDNA from each tissue sample (set 1 and set 3) as described [29] using TRIZOL (Invitrogen, Carlsbad, CA), the RNeasy kit (Qiagen, Valencia, CA), and the High-Capacity cDNA Archive Kit (Life Technologies, Carlsbad, CA). Quantitative reverse transcriptase polymerase chain reaction (PCR) was performed using Assays-on Demand and the ABI 7900 Sequence Detection System (Life Technologies). Primer sets (MCM2: Hs01091564_m1, MCM3: Hs00172459_m1, Ki67: Hs00267195_m1) were obtained from Life Technologies. PCR data were normalized using the ∆∆CT method; ALG9 was used as a housekeeping gene [30].
Copy number variation (CNV) analysis
Genomic DNA was isolated as described [31] from set 1 and set 3. CNV was measured using PCR-Taqman Copy Number Reference Assay from Life Technologies according to the manufacturer's instructions using the primer sets Hs00575269_cn and Hs02422238_cn (MCM2) and Hs00378664_cn (MCM3). CNVs of each gene were normalized to telomerase reverse transcriptase. The results were analyzed with CopyCaller v2.0 software (www.appliedbiosystems.com).
Immunostaining
This was performed as described [27], [31] using a 1:100 dilution of rabbit anti-MCM2 or -MCM3 (#4007 and 4102; Cell Signaling Technology, Beverly, MA), anti-Ki67 (ab15580; Abcam, Cambridge, MA), and anti–chromogranin A (A0430; DAKO, Glostrup, Denmark) antibodies in set 2. The TMA was examined by AQUA after immunofluorescent staining [32] and by a pathologist (B. K.) after DAB staining (blinded to tissue labels). For automated analysis, neuroendocrine tumor cells or normal mucosal epithelia were identified using a fluorescently tagged mouse anti-cytokeratin antibody cocktail (AE1/AE3; DAKO), nuclei were visualized by 4′,6-diamidino-2-phenylindole, and targets were visualized with a fluorescent chromogen (Cy-5-tyramide; NEN Life Science Products, Boston, MA). AQUA expression values were quantified as low (below median) or high expression (above median).
Protein extraction and western blot analysis
Pieces of tissue (1 × 2 mm) (set 1 and set 3) were processed [29] using manual homogenization with RIPA lysis buffer (Millipore, Temecula, CA), BCA-based protein quantitation (Thermo Fisher Scientific, Rockford, IL), denaturation, and separation of total protein lysates (15 μg) on 10% SDS-PAGE gels (Invitrogen, Carlsbad, CA). Membranes were probed with anti-MCM2 and anti-MCM3 (antibodies as for IHC). Protein levels were confirmed with β-actin (Sigma-Aldrich, St. Louis, MO). The optical density of the appropriately sized band was measured using ImageJ software 1.47 (NIH, Bethesda, MD).
Statistical evaluation
All statistical analyses were performed using Microsoft Excel and Prism 6.0 (GraphPad Software, San Diego, CA) using nonparametric methods. Multiple group comparisons were performed using the Kruskal-Wallis test followed by the Dunn post hoc test where appropriate. Binary comparisons were made using a two-tailed Mann-Whitney test. Correlations were undertaken using Spearman correlation. Survival analysis was conducted by Kaplan-Meier curves after grouping staining results by low and high (cut points approximating the median were chosen to maximize prognostication) normalized AQUA scores, and significance was determined by the log-rank statistic using GraphPad Prism 6.0 software (GraphPad Software Inc., La Jolla, CA). A P value of < .05 was designated as significant.
Results
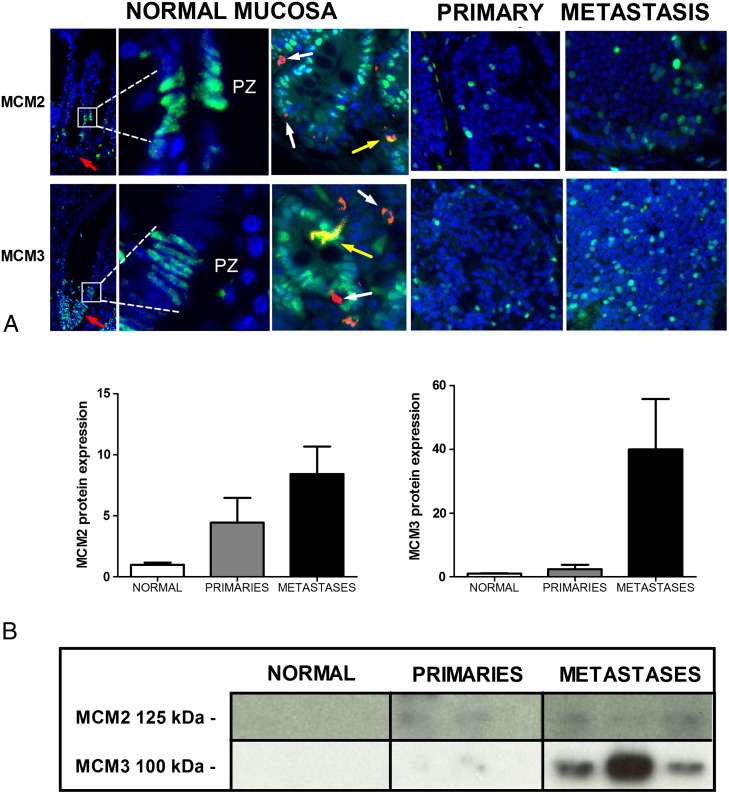
Protein Expression of MCM2 and MCM3 in Normal Mucosa and SI NENs (Set 1)
MCM2 and 3 protein expression was assessed in normal small intestinal mucosa using IHC (Figure 1A). Less than 2% of neuroendocrine cells (visualized by dual staining with chromogranin A) were MCM positive, identifying low replication potential (and proliferation rates) of those cells. In normal epithelial cells, MCMs were predominantly localized to the “proliferative zone” [33] of the small intestinal crypts (Figure 1A). SI NENs tended to exhibit higher MCM expression by Western blot than normal proliferating intestine (Figure 1B, MCM2: P = .15, MCM3: P = .06, Kruskal-Wallis test).
Figure 1.
Protein expression of MCM2 and MCM3 in small intestinal mucosa and SI-NENs (primaries and metastases).
Immunohistochemistry (A): MCM2 and MCM3 were identified in crypts associated with the proliferative zone (PZ) (inset) which is the site of cells involved in renewing mucosa where the highest mitosis rates are expected. Additional cells were MCM3 positive at the base of crypts; these cells were not stained by MCM2 (red arrows). Dual staining with chromogranin A identified only a few (<2%) normal neuroendocrine cells to be MCM2 or MCM3 positive (yellow arrows). Both primary tumor and metastasis exhibited nuclear expression of MCM2 and MCM3, and expression of both proteins tended to be higher in metastasis in comparison to the primary tumor. This overexpression was also identified by Western blot (B), especially for MCM3, but this was not statistically significant (Kruskal-Wallis, MCM3: P = .06, MCM2: P = .15).
DAPI: nuclei (blue), FITC: target marker (green), Cy5: chromogranin A (red-white arrows), dual-stained cells (yellow). PZ = proliferative zone. Mean ± SD.
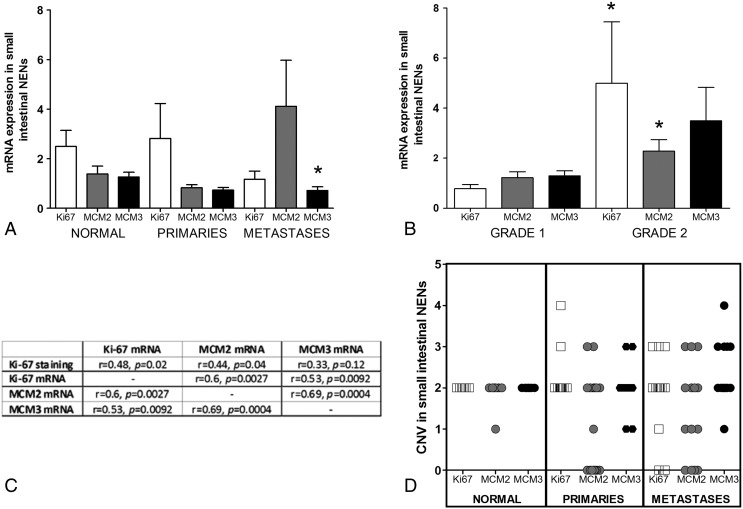
Clinical Relevance of MCM mRNA Expression in SI-NENs (Set 1)
Levels of MCM mRNA were similar in primaries and metastases. However, MCM mRNA showed lower expression in metastases than in normal mucosa (Figure 2A, P < .05). As expected, higher-grade tumors (G2) were associated with elevated Ki67 and MCM2 mRNA expression (P < .05, Figure 2B) than low-grade tumors (G1). MCM3 was also elevated, but this did not reach significance (three-fold, P = .26). A comparison between Ki67 staining and mRNA expression of Ki67, MCM2, and MCM3 (Figure 2C) identified that the Ki67%, as anticipated, was correlated with Ki67 mRNA in SI NENs (r = 0.48, P < .05). The Ki67% was also correlated with MCM2 mRNA levels (r = 0.44, P < .05), but there was no correlation with MCM3 mRNA (Figure 2C). At an mRNA level, strong correlations were noted between Ki67 and both MCMs (r = 0.53-0.6, P < .01). Analysis of copy number identified that normal tissues exhibited two stable copies of MCM2 and MCM3 genes, whereas SI NENs demonstrated wide variation (0-4 copies) (Figure 2D). This variation in copy number was not directly correlated with differences in mRNA or protein expression, e.g., in the Western blot analyses (Figure 1B).
Figure 2.
Clinical relevance of MCM and Ki67 expression in SI-NENs. (A) MCM expression in normal mucosa tended to be higher than in neoplastic small intestinal tumors, whereas Ki67 was not significantly different between any tissue type (*P < .05 versus normal mucosa). (B) Ki67 and MCM2 expression was significantly increased (*P < .05) in grade 2 compared to grade 1 tumors. MCM3 was also increased, but this did not achieve statistical significance. (C) Correlation between MCM mRNA expression and Ki67 staining identified a relationship for MCM2 (r2 = 0.44, P < .05) but not for MCM3. Expression of either MCM significantly correlated with Ki67 mRNA expression (MCM2: r = 0.6, P = .0027, MCM3: r = 0.53, P = .0092) and with each other (r = 0.69, P = .004). (D) High copy number variance was noted for all three markers in both primary tumors and in metastases; this was not seen in normal mucosa. Mean ± SD.
Expression and Correlation with Survival (Set 2)
We next evaluated Ki67 and MCM2/3 immunostaining to determine the proportion of tumors that expressed each marker. An evaluation of Ki67 staining identified that 25 (37%) of 55 samples were positive for Ki67, with the remainder showing no Ki67-positive tumor cells in the examined fields. In contrast, at least some MCM2 and 3 positivity was identified in all lesions (χ2 38.55, P < .0001). Analysis of individual cell counts identified significantly more MCM3-positive cells (mean: 28.7% [range 22%-34%]) and MCM2-positive cells (mean 21.2% [range: 16%-25%]) than Ki67-positive cells (mean: 2.3%: [range 0%-7%, P < .01]). This indicates that these markers identified a greater proportion of tumor cells than Ki67 per se.
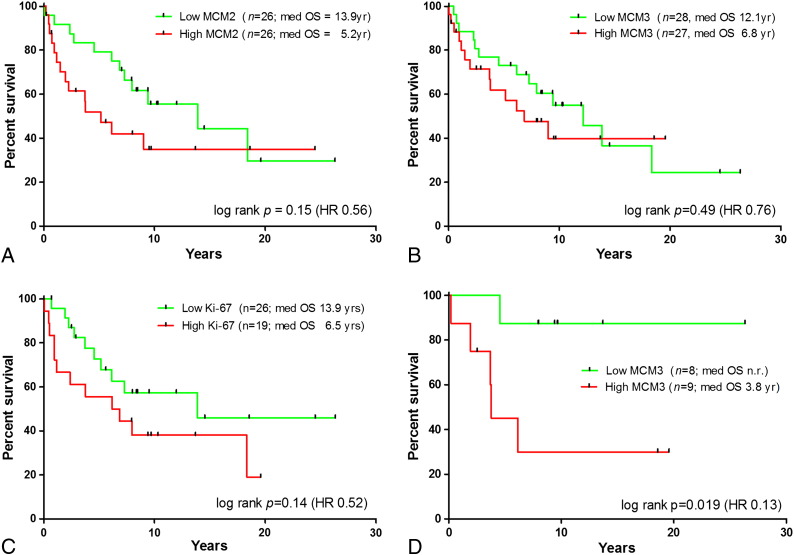
Thereafter, we examined whether MCM2 and 3 protein expression was prognostic for survival in these lesions. Groups were prospectively divided as below or above the median to represent low or high expression of each protein. As demonstrated in Figure 3, the differences in median OS between low- and high-expression groups were large for both MCM2 (8.7-year difference) and MCM3 (5.3-year difference). The log-rank statistic, however, did not reach significance (MCM2, hazard ratio [HR] 0.56, P = .15, Figure 3A; MCM3, HR 0.76, P = .49, Figure 3B). Like MCMs, Ki67 also did not significantly prognosticate survival in this cohort (HR 0.52, P = .14).
Figure 3.
Survival curves for AQUA analysis of MCM2 and MCM3 in SI-NENs.
Low expressions of MCM2 (A) and MCM3 (B) were both associated with notably longer OS. Using a combination of proliferative markers, patients with low–proliferation score tumors (0-1; n = 21) had prolonged survival (median OS 12 years) compared to those with high–proliferation scores tumors (2-3; n = 24) (median OS years 6.5) (C, P = .06, HR 0.46). A high MCM3 expression was correlated with worst prognosis, whereas after more than 25-years of follow-up, the median OS of patients with low MCM3 expression was not reached in the subset of tumors that were only Ki67% positive (D, P = .019, HR 0.13).
To further examine a prognostic role for Ki67 and MCM2/3 in SI NENs, we combined the results of Ki67 with MCM2 and 3 to generate a proliferative marker score based on the number of elevated markers in each tumor. In this algorithm, e.g., a tumor with high levels of 2-3 markers but low levels of 0-1 markers would score “2-3” out of a maximum of 3. Individuals with tumors with low proliferation scores (0-1; n = 21) had prolonged survival (median OS 11.98 years) compared to those with tumors exhibiting high proliferative scores (2-3; n = 23; median OS 6.15 years) (log-rank P = .06) (Figure 3C).
In the examination of the 25 tumors with detectable Ki67%, a high MCM3 expression was associated with a worse prognosis (OS 3.8 years), whereas after more than 25 years of follow-up, the median OS of patients with low MCM3 expression was not reached (Figure 3D, P = .0019, HR 0.13).
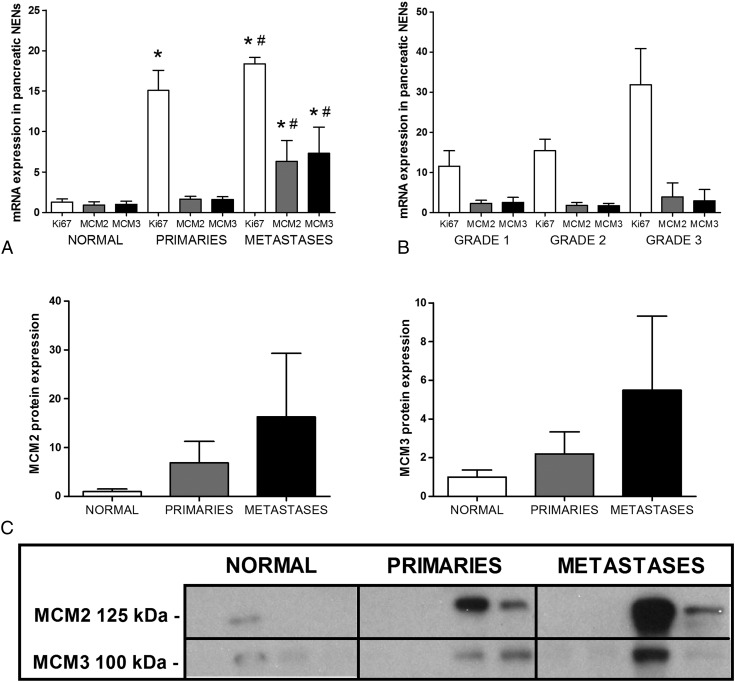
MCM2 and MCM3 in Normal Pancreas and Pancreatic NENs (Set 3)
As comparators, we examined MCM expression in pancreatic NENs which generally exhibit a higher proliferative rate and are known to be more aggressive [1]. Elevated mRNA expression of MCM2 and MCM3 was identified in metastases compared to primaries or normal pancreas, respectively (Figure 4A, Kruskal-Wallis P < .0001, post hoc P < .05). Similar elevations of Ki67 mRNA was noted in metastases (Figure 4A, post hoc P < .05). Ki67 and MCM expression correlated with tumor size (Ki67% r = 0.39, P < .05; Ki67 mRNA r = 0.41, P < .05; MCM2 r = 0.52, P < .01; and MCM3 r = 0.55, P < .01) but not with lymph node status or angioinvasion (data not shown). MCM expression was not related to grade (Figure 4B). Although MCM2 and MCM3 proteins were elevated in tumors, the differences were not significant (Figure 4C).
Figure 4.
mRNA and protein expression of MCM2 and MCM3 in normal pancreas and pancreatic NENs (primaries and metastases).
(A) MCM2 and MCM3 mRNAs were elevated in metastases in comparison to normal pancreas and to primaries, whereas Ki67 was elevated in metastases compared to normal pancreas (Kruskal-Wallis P < 0.0001, *P < .05 versus normal, #P < .05 versus primaries). (B) Ki67 and MCM mRNA expression as a function of grade identified no significant differences in pancreatic NENs. (C) Using Western blot, an elevation of MCM protein expression in pNEN metastases was confirmed (Kruskal-Wallis, MCM2: P = .24, MCM3: P = .44). Mean ± SD.
Discussion
We examined MCM2 and MCM3 expression in neuroendocrine cells from the small intestine and pancreas and then evaluated their potential role as proliferative and prognostic markers. This was undertaken as the Ki67 index has limitations as a proliferative marker in low proliferating tumors, particularly in those derived from the small intestine [4], [34].
Normal small intestinal neuroendocrine cells seldom exhibited either MCM2 or MCM3 positivity, confirming that few cells are replication licensed; the majority are terminally differentiated. In addition, we could not identify MCM2 or 3 in a small intestinal transcriptome library [35]; expression of mRNA was undetectable by quantitative PCR in five of six small intestinal enterochromaffin cell preparations (data not shown). SI-NENs are largely homogeneous and exhibit a low proliferation (they are predominantly grade NET G1) [36]. Despite this, MCM3 protein expression was higher in tumors compared to normal small intestine mucosa (Figure 1B, e.g., MCM3: P = .06) identifying that tumor cells are replication licensed. Although small intestinal mucosa may not be the perfect control tissue due to low numbers of neuroendocrine cells (1%-2% of mucosa), the observation that expression is increased in NENs compared to a tissue resource that has a high turnover confirms our hypothesis that MCM expression in NENs is of biological relevance. The elevation in tumors is not likely to be due to changes in copy number (Figure 2D). The significance of CNV noted is uncertain, with possible explanations including chromosomal instability [37] (albeit less commonly seen than in most cancer types) or tumor-specific changes in the reference gene. It does, however, raise the possibility of an oncogenic effect targeting MCM2/3 which specifically contributes to tumorigenesis in SI-NENs.
Ki67 is currently the proliferation marker of choice for GEP-NENs, and its expression at a protein level (IHC: Ki67 index or Ki67%) is used to grade these lesions [6]. We contrasted MCM2 and MCM3 expression with Ki67 in SI-NENs. MCM2 mRNA expression was correlated with Ki67 staining, Ki67 mRNA expression, and grade. Interestingly, significantly more small intestinal tumor cells were immunostained with MCM2 and 3 antibodies than Ki67, indicating that measurement of these proteins may identify more cells, particularly those that are replication licensed. This is of importance for these lesions because discrimination with Ki67 is difficult when neoplasms have “low” proliferative rates (G1 SI-NETs: <2%). This also suggests that these tumors are not quiescent but do have the potential to grow and can enter the cell cycle and progress to active proliferation [38].
To explore the clinical relevance of these observations, we evaluated the relationship between MCM protein expression and OS using an AQUA-based immunohistochemistry protocol [27], [31]. In this analysis, in an independent set of SI-NENs, Ki67 expression when measured by AQUA staining was not prognostic of survival (HR 0.52; P = .14). However, the median survival of SI-NENs with elevated MCM2 was 5.2 years compared to 13.9 years in tumors with low levels of MCM2 (HR 0.56). The prognostic ability of Ki67 and MCMs was amplified when they were included in an algorithm. Tumors with elevated expression of the majority of markers (2-3 markers) had poor survival (median OS 6.1 years) compared to tumors with elevated expression in a minority of markers (0-1 markers: median OS 12 years). MCM3 itself was not prognostic as a single marker, but in patients with tumors with detectable Ki67, MCM3 staining was prognostic for survival (P = .019, HR 0.13).
When considered together, the correlation between MCM expression and Ki67 expression confirms that MCMs are a proliferative marker in GEP-NENs, and the survival analysis identifies that they measure a similar phenomenon. It is evident that elevations in multiple markers (MCM2/3 and Ki67) are consistent with a poorer prognosis and highlights the importance of identifying all cells that may be proliferating or have the potential (are replication licensed) for entering the proliferative cycle.
In pancreatic NENs, MCM expression was generally higher in metastases than in primaries and higher in primaries than in normal pancreas. Such a spectrum has been previously identified in the adenoma-dysplasia-carcinoma sequence in the transitions to adrenocortical carcinoma [20], prostate carcinoma [39], [40], colorectal carcinoma [41], melanoma [42], anal carcinoma [43], and thyroid malignancies [21]. This continuum in pancreatic NENs recapitulates the variability in proliferation in these tumors (pNENs range across grades NET G1, NET G2, NEC) [44]. Because MCM expression behaves similar to Ki67 in pNENs but do not correlate with grade, MCMs does not appear to add to Ki67 in these more aggressive neoplasms.
Conclusion
MCM2 and MCM3 are proliferative markers in GEP-NENs, and MCM protein expression is elevated in SI NENs relative both to normal mucosa, a proliferating, MCM-positive control, as well as to normal cells (little to no expression). In addition, an MCM “proliferative index” is prognostic of survival. Augmentation of Ki67 with a marker that measures replication licensing and is expressed in a larger proportion of cells could improve prognostic reliability. Furthermore, evaluation of the mechanisms that govern MCM2/3 regulation may provide insight into the regulation of SI-NEN proliferation and metastases.
Acknowledgements
S. S. was supported by the Deutsche Forschungsgemeinschaft: SCHI 1177/1-1. B. L. was partially supported by the Murray Jackson Clinical Fellowship from the Genesis Oncology Trust Auckland, New Zealand. Professor Sir Nicholas Wright (Centre for Tumor Biology, Barts Cancer Institute, Barts, and the London School of Medicine and Dentistry, Queen Mary University of London, UK) for initially suggesting examining MCMs in neuroendocrine tumors and for discussion regarding these proliferation-associated proteins. The authors have nothing to disclose.
Footnotes
S. S. was supported by the Deutsche Forschungsgemeinschaft: SCHI 1177/1-1. B. L. was partially supported by the Murray Jackson Clinical Fellowship from the Genesis Oncology Trust Auckland, New Zealand.
Contributor Information
Simon Schimmack, Email: simon.schimmack@med.uni-heidelberg.de.
Ben Lawrence, Email: b.lawrence@auckland.ac.nz.
Barton Kenney, Email: barton.kenney@yale.edu.
Hubertus Schmitz-Winnenthal, Email: winnenthal@gmail.com.
Irvin M. Modlin, Email: imodlin@optonline.net.
Mark Kidd, Email: mkidd01@snet.net.
References
- 1.Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin N Am. 2011;40(1):1–18. doi: 10.1016/j.ecl.2010.12.005. vii. [DOI] [PubMed] [Google Scholar]
- 2.Bosman F, Carneiro F, Hruban RH, Theise ND, editors. Classification of Tumours of the Digestive System. World Health Organization; International Agency for Research on Cancer; Lyon: 2010. [Google Scholar]
- 3.Fischer L, Bergmann F, Schimmack S, Hinz U, Priess S, Muller-Stich BP, Werner J, Hackert T, Buchler MW. Outcome of surgery for pancreatic neuroendocrine neoplasms. Br J Surg. 2014;101(11):1405–1412. doi: 10.1002/bjs.9603. [DOI] [PubMed] [Google Scholar]
- 4.Panzuto F, Nasoni S, Falconi M, Corleto VD, Capurso G, Cassetta S, Di Fonzo M, Tornatore V, Milione M, Angeletti S. Prognostic factors and survival in endocrine tumor patients: comparison between gastrointestinal and pancreatic localization. Endocr Relat Cancer. 2005;12(4):1083–1092. doi: 10.1677/erc.1.01017. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed A, Turner G, King B, Jones L, Culliford D, McCance D, Ardill J, Johnston BT, Poston G, Rees M. Midgut neuroendocrine tumours with liver metastases: results of the UKINETS study. Endocr Relat Cancer. 2009;16(3):885–894. doi: 10.1677/ERC-09-0042. [DOI] [PubMed] [Google Scholar]
- 6.Panzuto F, Campana D, Fazio N, Brizzi MP, Boninsegna L, Nori F, Di Meglio G, Capurso G, Scarpa A, Dogliotti L. Risk factors for disease progression in advanced jejunoileal neuroendocrine tumors. Neuroendocrinology. 2012;96(1):32–40. doi: 10.1159/000334038. [DOI] [PubMed] [Google Scholar]
- 7.Jann H, Roll S, Couvelard A, Hentic O, Pavel M, Muller-Nordhorn J, Koch M, Rocken C, Rindi G, Ruszniewski P. Neuroendocrine tumors of midgut and hindgut origin: tumor-node-metastasis classification determines clinical outcome. Cancer. 2011;117(15):3332–3341. doi: 10.1002/cncr.25855. [DOI] [PubMed] [Google Scholar]
- 8.Tang LH, Gonen M, Hedvat C, Modlin IM, Klimstra DS. Objective quantification of the Ki67 proliferative index in neuroendocrine tumors of the gastroenteropancreatic system: a comparison of digital image analysis with manual methods. Am J Surg Pathol. 2012;36(12):1761–1770. doi: 10.1097/PAS.0b013e318263207c. [DOI] [PubMed] [Google Scholar]
- 9.Bailis JM, Forsburg SL. MCM proteins: DNA damage, mutagenesis and repair. Curr Opin Genet Dev. 2004;14(1):17–21. doi: 10.1016/j.gde.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Giaginis C, Vgenopoulou S, Vielh P, Theocharis S. MCM proteins as diagnostic and prognostic tumor markers in the clinical setting. Histol Histopathol. 2010;25(3):351–370. doi: 10.14670/HH-25.351. [DOI] [PubMed] [Google Scholar]
- 11.Tachibana KE, Gonzalez MA, Coleman N. Cell-cycle-dependent regulation of DNA replication and its relevance to cancer pathology. J Pathol. 2005;205(2):123–129. doi: 10.1002/path.1708. [DOI] [PubMed] [Google Scholar]
- 12.MacCallum DE, Hall PA. The location of pKi67 in the outer dense fibrillary compartment of the nucleolus points to a role in ribosome biogenesis during the cell division cycle. J Pathol. 2000;190(5):537–544. doi: 10.1002/(SICI)1096-9896(200004)190:5<537::AID-PATH577>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 13.Joshi S, Watkins J, Gazinska P, Brown JP, Gillett CE, Grigoriadis A, Pinder SE. Digital imaging in the immunohistochemical evaluation of the proliferation markers Ki67, MCM2 and Geminin, in early breast cancer, and their putative prognostic value. BMC Cancer. 2015;15:546. doi: 10.1186/s12885-015-1531-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nowinska K, Chmielewska M, Piotrowska A, Pula B, Pastuszewski W, Krecicki T, Podhorska-Okolow M, Zabel M, Dziegiel P. Correlation between levels of expression of minichromosome maintenance proteins, Ki-67 proliferation antigen and metallothionein I/II in laryngeal squamous cell cancer. Int J Oncol. 2016;48(2):635–645. doi: 10.3892/ijo.2015.3273. [DOI] [PubMed] [Google Scholar]
- 15.Guzinska-Ustymowicz K, Pryczynicz A, Kemona A, Czyzewska J. Correlation between proliferation markers: PCNA, Ki-67, MCM-2 and antiapoptotic protein Bcl-2 in colorectal cancer. Anticancer Res. 2009;29(8):3049–3052. [PubMed] [Google Scholar]
- 16.Nishihara K, Shomori K, Fujioka S, Tokuyasu N, Inaba A, Osaki M, Ogawa T, Ito H. Minichromosome maintenance protein 7 in colorectal cancer: implication of prognostic significance. Int J Oncol. 2008;33(2):245–251. [PubMed] [Google Scholar]
- 17.Giaginis C, Georgiadou M, Dimakopoulou K, Tsourouflis G, Gatzidou E, Kouraklis G, Theocharis S. Clinical significance of MCM-2 and MCM-5 expression in colon cancer: association with clinicopathological parameters and tumor proliferative capacity. Dig Dis Sci. 2009;54(2):282–291. doi: 10.1007/s10620-008-0305-z. [DOI] [PubMed] [Google Scholar]
- 18.Fujioka S, Shomori K, Nishihara K, Yamaga K, Nosaka K, Araki K, Haruki T, Taniguchi Y, Nakamura H, Ito H. Expression of minichromosome maintenance 7 (MCM7) in small lung adenocarcinomas (pT1): Prognostic implication. Lung Cancer. 2009;65(2):223–229. doi: 10.1016/j.lungcan.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Kato H, Miyazaki T, Fukai Y, Nakajima M, Sohda M, Takita J, Masuda N, Fukuchi M, Manda R, Ojima H. A new proliferation marker, minichromosome maintenance protein 2, is associated with tumor aggressiveness in esophageal squamous cell carcinoma. J Surg Oncol. 2003;84(1):24–30. doi: 10.1002/jso.10287. [DOI] [PubMed] [Google Scholar]
- 20.Szajerka A, Dziegiel P, Szajerka T, Zabel M, Winowski J, Grzebieniak Z. Immunohistochemical evaluation of metallothionein, Mcm-2 and Ki-67 antigen expression in tumors of the adrenal cortex. Anticancer Res. 2008;28(5B):2959–2965. [PubMed] [Google Scholar]
- 21.Mehrotra P, Gonzalez MA, Johnson SJ, Coleman N, Wilson JA, Davies BR, Lennard TW. Mcm-2 and Ki-67 have limited potential in preoperative diagnosis of thyroid malignancy. Laryngoscope. 2006;116(8):1434–1438. doi: 10.1097/01.mlg.0000225931.59644.93. [DOI] [PubMed] [Google Scholar]
- 22.Gambichler T, Shtern M, Rotterdam S, Bechara FG, Stucker M, Altmeyer P, Kreuter A. Minichromosome maintenance proteins are useful adjuncts to differentiate between benign and malignant melanocytic skin lesions. J Am Acad Dermatol. 2009;60(5):808–813. doi: 10.1016/j.jaad.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 23.Kobierzycki C, Pula B, Skiba M, Jablonska K, Latkowski K, Zabel M, Nowak-Markwitz E, Spaczynski M, Kedzia W, Podhorska-Okolow M. Comparison of minichromosome maintenance proteins (MCM-3, MCM-7) and metallothioneins (MT-I/II, MT-III) expression in relation to clinicopathological data in ovarian cancer. Anticancer Res. 2013;33(12):5375–5383. [PubMed] [Google Scholar]
- 24.Rodins K, Cheale M, Coleman N, Fox SB. Minichromosome maintenance protein 2 expression in normal kidney and renal cell carcinomas: relationship to tumor dormancy and potential clinical utility. Clin Cancer Res. 2002;8(4):1075–1081. [PubMed] [Google Scholar]
- 25.Jankowska-Konsur A, Kobierzycki C, Reich A, Grzegrzolka J, Maj J, Dziegiel P. Expression of MCM-3 and MCM-7 in Primary Cutaneous T-cell Lymphomas. Anticancer Res. 2015;35(11):6017–6026. [PubMed] [Google Scholar]
- 26.Grande E, Capdevila J, Barriuso J, Anton-Aparicio L, Castellano D. Gastroenteropancreatic neuroendocrine tumor cancer stem cells: do they exist? Cancer Metastasis Rev. 2011;22:22. doi: 10.1007/s10555-011-9328-6. [DOI] [PubMed] [Google Scholar]
- 27.Kidd M, Modlin IM, Mane SM, Camp RL, Shapiro MD. Q RT-PCR detection of chromogranin A: a new standard in the identification of neuroendocrine tumor disease. Ann Surg. 2006;243(2):273–280. doi: 10.1097/01.sla.0000197734.28551.0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Camp RL, Chung GG, Rimm DL. Automated subcellular localization and quantification of protein expression in tissue microarrays. Nat Med. 2002;8(11):1323–1327. doi: 10.1038/nm791. [Epub 2002 Oct 1321] [DOI] [PubMed] [Google Scholar]
- 29.Schimmack S, Lawrence B, Svejda B, Alaimo D, Schmitz-Winnenthal H, Fischer L, Buchler MW, Kidd M, Modlin I. The clinical implications and biologic relevance of neurofilament expression in gastroenteropancreatic neuroendocrine neoplasms. Cancer. 2012;118(10):2763–2775. doi: 10.1002/cncr.26592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kidd M, Nadler B, Mane S, Eick G, Malfertheiner M, Champaneria M, Pfragner R, Modlin I. GeneChip, geNorm, and gastrointestinal tumors: novel reference genes for real-time PCR. Physiol Genomics. 2007;30(3):363–370. doi: 10.1152/physiolgenomics.00251.2006. [DOI] [PubMed] [Google Scholar]
- 31.Kidd M, Eick G, Shapiro MD, Camp RL, Mane SM, Modlin IM. Microsatellite instability and gene mutations in transforming growth factor-beta type II receptor are absent in small bowel carcinoid tumors. Cancer. 2005;103(2):229–236. doi: 10.1002/cncr.20750. [DOI] [PubMed] [Google Scholar]
- 32.Kidd M, Modlin IM, Mane SM, Camp RL, Eick G, Latich I. The role of genetic markers--NAP1L1, MAGE-D2, and MTA1--in defining small-intestinal carcinoid neoplasia. Ann Surg Oncol. 2006;13(2):253–262. doi: 10.1245/ASO.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 33.Potten CS, Gandara R, Mahida YR, Loeffler M, Wright NA. The stem cells of small intestinal crypts: where are they? Cell Prolif. 2009;42(6):731–750. doi: 10.1111/j.1365-2184.2009.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Eeden S, Quaedvlieg PF, Taal BG, Offerhaus GJ, Lamers CB, Van Velthuysen ML. Classification of low-grade neuroendocrine tumors of midgut and unknown origin. Hum Pathol. 2002;33(11):1126–1132. doi: 10.1053/hupa.2002.129204. [DOI] [PubMed] [Google Scholar]
- 35.Modlin IM, Kidd M, Pfragner R, Eick GN, Champaneria MC. The functional characterization of normal and neoplastic human enterochromaffin cells. J Clin Endocrinol Metab. 2006;91(6):2340–2348. doi: 10.1210/jc.2006-0110. [DOI] [PubMed] [Google Scholar]
- 36.Pape UF, Perren A, Niederle B, Gross D, Gress T, Costa F, Arnold R, Denecke T, Plockinger U, Salazar R. ENETS Consensus Guidelines for the Management of Patients with Neuroendocrine Neoplasms from the Jejuno-Ileum and the Appendix Including Goblet Cell Carcinomas. Neuroendocrinology. 2012;95(2):135–156. doi: 10.1159/000335629. [DOI] [PubMed] [Google Scholar]
- 37.Zikusoka MN, Kidd M, Eick G, Latich I, Modlin IM. The molecular genetics of gastroenteropancreatic neuroendocrine tumors. Cancer. 2005;104(11):2292–2309. doi: 10.1002/cncr.21451. [DOI] [PubMed] [Google Scholar]
- 38.Shetty A, Loddo M, Fanshawe T, Prevost AT, Sainsbury R, Williams GH, Stoeber K. DNA replication licensing and cell cycle kinetics of normal and neoplastic breast. Br J Cancer. 2005;93(11):1295–1300. doi: 10.1038/sj.bjc.6602829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ananthanarayanan V, Deaton RJ, Yang XJ, Pins MR, Gann PH. Alteration of proliferation and apoptotic markers in normal and premalignant tissue associated with prostate cancer. BMC Cancer. 2006;6:73. doi: 10.1186/1471-2407-6-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Padmanabhan V, Callas P, Philips G, Trainer TD, Beatty BG. DNA replication regulation protein Mcm7 as a marker of proliferation in prostate cancer. J Clin Pathol. 2004;57(10):1057–1062. doi: 10.1136/jcp.2004.016436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott IS, Morris LS, Bird K, Davies RJ, Vowler SL, Rushbrook SM, Marshall AE, Laskey RA, Miller R, Arends MJ. A novel immunohistochemical method to estimate cell-cycle phase distribution in archival tissue: implications for the prediction of outcome in colorectal cancer. J Pathol. 2003;201(2):187–197. doi: 10.1002/path.1444. [DOI] [PubMed] [Google Scholar]
- 42.Boyd AS, Shakhtour B, Shyr Y. Minichromosome maintenance protein expression in benign nevi, dysplastic nevi, melanoma, and cutaneous melanoma metastases. J Am Acad Dermatol. 2008;58(5):750–754. doi: 10.1016/j.jaad.2007.12.026. [DOI] [PubMed] [Google Scholar]
- 43.Scarpini C, White V, Muralidhar B, Patterson A, Hickey N, Singh N, Mullerat J, Winslet M, Davies RJ, Phillips ML. Improved screening for anal neoplasia by immunocytochemical detection of minichromosome maintenance proteins. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2008;17(10):2855–2864. doi: 10.1158/1055-9965.EPI-08-0288. [DOI] [PubMed] [Google Scholar]
- 44.Yachida S, Vakiani E, White CM, Zhong Y, Saunders T, Morgan R, de Wilde RF, Maitra A, Hicks J, Demarzo AM. Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol. 2012;36(2):173–184. doi: 10.1097/PAS.0b013e3182417d36. [DOI] [PMC free article] [PubMed] [Google Scholar]