Abstract
Objectives:
We assess the association between marital quality and both the risk of developing diabetes and the management of diabetes after its onset in later life.
Method:
We use data from the first two waves of the National Social Life, Health, and Aging Project to estimate regression models with lagged dependent variables. The sample includes 1,228 married respondents, among whom 389 were diabetic. Those with either a reported diagnosis or with HbA1c ≥ 6.5% are identified diabetic. We categorize diabetic respondents into three groups: controlled, undiagnosed, and uncontrolled diabetes. We conduct factor analysis to construct positive and negative marital quality scales.
Results:
For women, an increase in positive marital quality between Waves 1 and 2 is related to a lower risk of being diabetic at Wave 2, net of diabetes status at Wave 1; surprisingly, for men, an increase in negative marital quality between Waves 1 and 2 is related to both a lower risk of being diabetic at Wave 2 and a higher chance of controlling diabetes at Wave 2 after its onset.
Discussion:
Our results challenge the traditional assumption that negative marital quality is always detrimental to health and encourage family scholars to distinguish different sources and types of negative marital quality.
Keywords: Diabetes, Disease management, Gender, Marital quality, Marriage
Diabetes is the fastest growing chronic condition in the United States. According to the U.S. Centers for Disease Control (CDC), 25.8 million Americans—8.3% of the population—had diabetes in 2010 (CDC, 2011); these figures rose rapidly to 29.1 million and 9.3% in 2012 (CDC, 2014). The consequences of diabetes are clearly recognized and include serious complications and premature death (CDC, 2014). In the United States, diabetes remains the seventh leading cause of death (CDC, 2014). Because diabetes can be controlled, the risk of complications lowered, and the onset of disease delayed, identifying risk factors is extremely important in designing effective prevention strategies and management programs. Yet previous research on diabetes has mostly focused on proximate behavioral risk factors, such as diet and exercise, ignoring upstream causes of social factors that lead to the development of the disease. In this study, we assess marital quality as one of the social factors that may shape both the risk and management of diabetes. Diabetes risk refers to the presence of any physiological or functional state that is a step on the way to diabetes, and diabetes management refers to a systematic process of diagnosis, monitoring, and control of diabetes after the onset of the disease.
Marriage is a unique type of social relationship in which spouses share space and resources, make investments together, and influence each other’s health behaviors (Umberson, 1992; Waite & Gallagher, 2000). Marital quality—spouses’ subjective appraisal of the marital relationship, including satisfaction, happiness, strain, and conflict—has a profound influence on each partner’s life context and thus on his or her health (Carr, Cornman, & Freedman, 2016; Umberson, Williams, Powers, Liu, & Needham, 2006). Marital quality influences how people manage their health and is especially important for diseases and conditions that rely on self-management. Diabetes is one such disease; it requires a day-to-day self-care regimen (Trief et al., 2006). Support from a good-quality marriage or conflict from a poor-quality marriage may promote or disrupt adherence to diabetes care regimens (Trief et al., 2006).
To date, empirical evidence of marital quality’s effect on diabetes is limited and primarily based on cross-sectional studies and clinical or community samples (Robles & Kiecolt-Glaser, 2003). Moreover, although gender differences have been a central focus of research on health links to marriage, empirical evidence is quite mixed. Some studies suggest a stronger effect of marital quality on health for women, some report stronger effects on men, and still other studies find no significant gender differences (Kiecolt-Glaser & Newton, 2001; Whisman, Li, Sbarra, & Raison, 2014). To fill these research gaps, we analyze data from the first two waves of the National Social Life, Health, and Aging Project (NSHAP) to address two major research questions: (1) How is marital quality related to diabetes risk and management over time among older adults? and (2) Do those patterns vary by gender?
Marital Quality and Diabetes Risk
Scholars have long recognized that married people have better health and live longer than unmarried people (Liu, 2012; Waite & Gallagher, 2000; Zhang & Hayward, 2006). Recent research suggests that marital quality is more significant than marital status per se in shaping health (Liu & Waite, 2014; Umberson, Williams, Powers, Liu, & Needham, 2006). Two of the primary theories to explain the links between marriage and health are the social control model and the stress model. The social control perspective on marriage suggests that spouses may regulate each other’s health behaviors (such as encouraging the spouse to quit smoking, reduce drinking, do exercise, or eat healthier food), comprising a source of social control that presumably promotes healthier behaviors and thus better health (Tucker & Anders, 2001; Umberson, 1992). The social control process is more likely to happen in the desired direction within a supportive rather than a strained relationship (Kotwal, Lauderdale, Waite, & Dale, 2016). In fact, marital stress may increase unhealthy behaviors either by undermining individuals’ self-control or via reducing the spouse’s behavior regulation (Kiecolt-Glaser & Newton, 2001; Umberson, 1992). Engaging in such unhealthy behaviors, such as overeating, adopting a sedentary lifestyle, smoking, or drinking alcohol, may contribute to diabetes exacerbation and complications (Marshall & Flyvbjerg, 2006).
Moreover, according to the stress model, the marital relationship is a key dimension of adulthood life that may affect health by modifying stress exposure (Robles & Kiecolt-Glaser, 2003). For example, ongoing marital conflict may expose spouses to chronic stress and lead to psychological distress that may increase the risk of chronic inflammation and in turn poor physical health (Umberson et al., 2006). Marital stress may also directly trigger the “fight-or-flight” process, in which the sympathetic nervous system induces the release of stress hormones (e.g., catecholamines and cortisol) and evokes physiological responses that increase the metabolization of glucose (Kiecolt-Glaser & Newton, 2001; Taylor et al., 2000). Consistent high blood glucose levels, along with inadequate levels of insulin or insulin resistance, increase the risk of developing diabetes (American Diabetes Association, 2010). In contrast, involvement in a happy marriage presumably provides social support and a safe haven that may reduce exposure to stress, aid in recovery from stress, and promote a healthy lifestyle, all of which may enhance both emotional and physical health (Carr et al., 2016; Waite & Gallagher, 2000).
Empirical studies have examined how marital quality relates to certain risk factors for diabetes, such as inflammation or metabolic syndrome (Whisman, Uebelacker, & Settles, 2010). Yet little research examines the effect of social factors on the onset of diabetes. One of the very few national studies of diabetes prevalence in a population-based sample finds that men who reported more positive marital exchanges were less likely to have diabetes, whereas men who reported more negative marital exchanges were more likely to have diabetes; no relationship appeared for women (Whisman et al., 2014). Because this study used cross-sectional data to examine marital exchanges among those with and without diabetes, it provides no information on the effect of marital quality on the development of diabetes. The associations may reflect responses to the disease rather than causes of it. Taken together, previous literature leads us to expect that:
Hypothesis 1: Those with higher levels of negative marital quality will show greater risk of incident diabetes than those with lower levels of negative marital quality, and those with higher levels of positive marital quality will show lower risk of incident diabetes than those with lower levels of positive marital quality.
Marital Quality and Diabetes Diagnosis and Management
Diagnosis of diabetes depends on access to medical care, whereas management of the disease largely depends on a daily regimen of self-care (Trief et al., 2006). Diabetes diagnosis is the first step of the disease management process. Early detection of diabetes prompts timely treatment and can delay onset of neurological and vascular damage that can result from uncontrolled spikes and falls in blood glucose (Marshall & Flyvbjerg, 2006). Because most symptoms of diabetes are mild and may go unnoticed, diagnosis depends heavily on regular medical examinations (Marshall & Flyvbjerg, 2006). According to the social control perspective on marriage, a supportive spouse, especially the wife, may take a primary role in reminding the partner to have regular medical checkups that generally include screening for diabetes (Kotwal et al., 2016). A supportive marriage may also facilitate the treatment of diabetes once diagnosed. Diabetes regulation and treatment includes medication, diet, glucose level monitoring, and lifestyle habits (Lutfey & Freese, 2005). Support from a spouse may indirectly promote adherence to a diabetes care regimen through spouses’ control of health behaviors (e.g., taking medicine and quitting alcohol) that increase the chances of controlling blood glucose levels (Trief, Ploutz-Snyder, Britton, & Weinstock, 2004). A happy marriage may also directly promote self-regulation: it may motivate a diabetes patient to comply with doctor’s recommendations and maintain a healthy diet and regular exercise routine (Trief et al., 2004), all of which promote blood glucose control. In contrast, marital stress may disrupt adherence to a diabetes management regimen, either by affecting patients’ own behavior and decision making or by reducing spouses’ involvement in patients’ disease management (August, Rook, Franks, & Parris Stephens, 2013). Moreover, the stress model suggests that marital stress may directly stimulate the release of stress hormones that causes blood sugar to rise and makes the disease control process harder, whereas a happy marriage may reduce the patient’s exposure to stress and thus improve the efficiency of the disease control efforts.
No nationally representative, population-based studies have assessed the relationship between marital quality and diabetes diagnosis and management, but a few clinical studies provide evidence that supports our reasoning (Robles & Kiecolt-Glaser, 2003; Trief, Himes, Orendorff, & Weinstock, 2001; Trief, Wade, Britton, & Weinstock, 2002; Trief et al., 2006). For example, Trief and colleagues (2001) analyzed 78 diabetic patients aged 18–55 years and found that those with better marital quality were more content with the process of adjusting to the disease and experienced less stress from diabetes than those with worse marital quality. A similar study by Trief and colleagues (2002) followed up with 61 diabetic respondents 2 years later and found that better marital quality predicted more satisfaction with diabetes management and greater diabetes-related quality of life. Another study of 134 elderly diabetic patients showed that greater marital stress was related to worse control of blood glucose levels (Trief et al., 2006). These clinical studies generally conclude that marital quality is directly correlated with diabetes management and that diabetics who have better marital adjustment and higher levels of intimacy adapt better to the disease and experience less distress from management regimens (Trief et al., 2001; Trief et al., 2002). Taken together, we expect that:
Hypothesis 2: Those with higher levels of negative marital quality will be less likely to be diagnosed with diabetes after its onset and also less likely to control it than those with lower levels of negative marital quality, and those with higher levels of positive marital quality will be more likely to be diagnosed with diabetes after its onset and also more likely to control it than those with lower levels of positive marital quality.
Gender Differences
On average, men receive more health-promotion benefits (e.g., emotional support and regulation of health behaviors) from their marriages than do women, and women’s health seems to be more vulnerable to marital stress than men’s (Kiecolt-Glaser & Newton, 2001; Liu & Waite, 2014). Women’s metabolic systems also appear to be more responsive to marital strain than men’s (Kiecolt-Glaser & Newton, 2001). Because women are generally more sensitive than men are to the quality of a relationship, women in strained marriages have a greater incidence of depression (Kiecolt-Glaser & Newton, 2001) that increases the risk of diabetes (Carnethon, Kinder, Fair, Stafford, & Fortmann, 2003). A handful of clinical studies confirm this view and conclude that marital conflict tends to evoke greater and more persistent physiological changes (e.g., increases in glucose levels) in women than in men (Kiecolt-Glaser & Newton, 2001). However, a more recent population-based national study finds that marital quality relates to men’s risk of diabetes but not women’s (Whisman et al., 2014). This mixed evidence reflects gender differences in the physiological mechanisms and health outcomes the studies measured as well as different samples and research designs. To the extent that women appear both physiologically and psychologically more reactive to marital stress than men (Donoho, Crimmins, & Seeman, 2013), we expect that:
Hypothesis 3: The associations between marital quality and diabetes risk and management will be stronger for women than for men.
Additional Sociodemographic Covariates
In addition to health behaviors (indicated by the social control model) and psychological distress (indicated by the stress model), both marital quality and diabetes are associated with other sociodemographic characteristics. The risk of diabetes increases with age (American Diabetes Association, 2010), and it also becomes more difficult to control this disease at older ages (CDC, 2011; Trief et al., 2006). Previous studies also suggest that marital quality tends to decline with age (Umberson et al., 2005). Diabetes is more prevalent among blacks and people with lower socioeconomic status (e.g., lower education and lower family income) than among whites and people with higher socioeconomic status (CDC, 2014; Lutfey & Freese, 2005). Marital quality is also lower among the former groups than the latter (Umberson et al., 2005).
Data
We use the first two waves of data from the NSHAP that was conducted by National Opinion Research Center (NORC) at the University of Chicago. A nationally representative probability sample of community-dwelling individuals aged 57–85 years was selected across the United States and screened in 2004. African Americans, Latinos, men, and those 75–84 years old were over sampled. We use the survey data analysis commands in Stata to weight all analyses and adjust them for clustering and stratification resulting from the complex sampling design (StataCorp, 2012).
The first wave of the NSHAP included a sample of 3,005 adults aged 57–85 years who were interviewed in 2005 or 2006 (Waite, Laumann, Levinson, Lindau, & O’Muircheartaigh, 2014). Both in-home interviews and lab tests and assays were conducted. Wave 2 consisted of 2,261 Wave 1 respondents who were reinterviewed in 2010 or 2011 (Waite, Cagney, et al., 2014). We restrict our analysis to the 1,250 respondents who remained married and who were interviewed in both waves. Results (data not shown but available upon request) suggest that in comparison with those who were interviewed in both waves, those who were lost to follow-up between waves are more likely to be diabetic, older, with lower levels of education and family income. This suggests that our sample may have excluded respondents who are relatively more disadvantaged—indicating a potentially more conservative finding. We further delete cases with missing values (n = 22) on key variables, including Wave 1 marital quality and Wave 2 diabetes. We draw two subsamples to analyze diabetes risk and management respectively. To analyze diabetes risk, we use the total sample of 1,228 respondents who were married and interviewed in both waves (with and without diabetes at baseline). To analyze diabetes management, we further restrict the sample to the 389 respondents who were diabetic at Wave 2.
Measures
Diabetes Risk and Management
To measure diabetes, we combine the biological and self-reported measures. The NSHAP directly measured glycosylated hemoglobin, or HbA1c, a biological marker that is useful in diagnosing and treating diabetes (Gomero, McDade, Williams, & Lindau, 2008). During the home interviews, blood was collected via a single finger-stick using a retractable tip, single-use disposable lancet, and then applied to filter paper for transport and storage. Gomero et al. (2008) describe the procedures of NSHAP HbA1c measurement in detail. Following the recommendations of the American Diabetes Association (2010), we identify respondents as having diabetes when their HbA1c is ≥6.5%. Additional analyses (results not shown) using a different cutoff point of HbA1c at 5.7%—usually used for identifying prediabetes (American Diabetes Association, 2010)—showed similar results. In addition, respondents were asked whether they had ever been told by a medical doctor that they had diabetes or high blood sugar. Based on responses to this question, along with the measures of HbA1c, we created two variables to measure diabetes risk and diabetes management separately.
We measure diabetes risk as a dichotomous outcome with the value of 1 indicating respondents who either reported a diagnosis of diabetes or showed an HbA1c ≥6.5%; we assigned the value of 0 to all others. Among those who have diabetes, we further measure diabetes management with three categories: (1) normal blood sugar reading but diagnosed with diabetes (referred as “controlled” diabetic group), (2) high blood sugar reading but no diagnosis of diabetes (referred as “undiagnosed” diabetic group), and (3) high blood sugar reading and diagnosed diabetes (referred as “uncontrolled” diabetic group). The controlled diabetic group is the reference group in the analysis of diabetes management.
Marital Quality
Marital quality consists of both positive and negative dimensions that are not opposite ends of a single dimension but distinct constructs. A marriage may be high, for example, on both positive and negative dimensions (Umberson et al., 2006). We follow previous studies (e.g., Galinsky & Waite, 2014; Liu & Waite, 2014; Warner & Adams, 2016) to calculate marital quality scales using the NSHAP data. These scales are composed of 8 items that we recoded to obtain consistent response categories across all items. First, respondents were asked how close they felt their relationship with the spouse was (Item 1). Responses range from 1 (not very close or somewhat close) to 3 (extremely close). Respondents were also asked how happy they were in their marriage (Item 2: 1 [very unhappy] to 7 [very happy]) and how emotionally satisfied they felt with their marriage (Item 3: 0 [not at all] to 4 [extremely]). Because Items 2 and 3 were highly skewed, we collapsed the categories. For relationship happiness, we collapsed the values to: 1 = Unhappy (1, 2, 3, 4), 2 = Happy (5, 6), and 3 = Very Happy (7). For emotional satisfaction, we collapsed the values to 1 = Not Satisfied (0, 1, 2), 2 = Satisfied (3), and 3 = Very Satisfied (4).
Additionally, respondents were asked the extent to which they preferred to spend their free time doing things with their spouse (Item 4). Responses included (1) mostly together, (2) some together and some apart, and (3) mostly apart. We reverse coded this item so that higher values indicate better marital quality. Finally, respondents were asked four questions about their spouse: how often they could open up to the spouse if they needed to talk about their worries (Item 5), how often they could rely on the spouse for help if they had a problem (Item 6), how often the spouse made too many demands on them (Item 7), and how often the spouse criticized them (Item 8). Responses to each question (Items 5–8) are 1 (never, hardly ever, or rarely), 2 (some of the time), and 3 (often).
Results from exploratory factor analyses suggest that these 8 items form two different dimensions that we refer to as positive and negative marital quality. We create two factor scores for positive and negative marital quality based on the iterated principle factor method and an oblique rotation. Table 1 shows the factor loadings of each item. The validity and reliability of these marital quality measures are well justified in previous studies (e.g., Galinsky & Waite, 2014; Liu & Waite, 2014; Warner & Adams, 2016).
Table 1.
Factor Loadings for Marital Quality
| Wave 1 | Wave 2 | |||
|---|---|---|---|---|
| PMQ | NMQ | PMQ | NMQ | |
| How close do you feel is your relationship with spouse? | 0.58 | −0.11 | 0.65 | 0.01 |
| How would you describe your marriage in terms of happiness? | 0.57 | −0.15 | 0.61 | −0.09 |
| How emotionally satisfying do you find your relationship with spouse? | 0.63 | −0.08 | 0.55 | −0.07 |
| Do you and spouse spend free time together or apart? | 0.38 | −0.02 | 0.45 | 0.06 |
| How often can you open up to spouse? | 0.60 | 0.08 | 0.62 | −0.02 |
| How often can you rely on spouse? | 0.61 | 0.09 | 0.52 | 0.01 |
| How often does spouse make too many demands on you? | −0.01 | 0.64 | 0.08 | 0.76 |
| How often does spouse criticize you? | 0.03 | 0.71 | −0.13 | 0.51 |
Note: PMQ = positive marital quality; NMQ = negative marital quality. Boldface numbers indicate factor loadings above the 0.35 cutoff point.
Other Covariates
We include three types of covariates (all measured at Wave 1) that relate to both marital quality and diabetes: sociodemographic covariates, psychological distress, and health behavior-related covariates.
Sociodemographic Covariates
We stratify all analyses by gender. We create three age categories: 57–64 (reference), 65–74, and 75–85. Race ethnicity includes non-Hispanic white (reference), non-Hispanic black, Hispanic, and other. We divide education into four categories: no diploma (reference), high school graduate, some college, and college graduate. We derive family income from a question that asked respondents to compare their family income level to that of other American families. Responses include below average (reference), average, and above average. We create a “missing” indicator category for about 15% of the analytic sample without valid values on family income.
Psychological distress
We control for depression, which is measured by a sum of an 11-question subset of the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977). Respondents were asked how often in the past week they experienced any of the following: (1) I did not feel like eating; (2) I felt depressed; (3) I felt that everything I did was an effort; (4) My sleep was restless; (5) I was happy; (6) I felt lonely; (7) People were unfriendly; (8) I enjoyed life; (9) I felt sad; (10) I felt that people disliked me; and (11) I could not get going. Response categories ranged from rarely or none of the time (0) to most of the time (3). We recode these items such that higher values indicate higher levels of depression.
Health Behavior-Related Covariates
Because respondents may take medications for diabetes, we include an indicator for taking any diabetes medications (1 = Yes, 0 = No). We also control indicators for currently smoke (1 = Yes, 0 = No), currently drink alcohol (1 = Yes, 0 = No), physical exercise (1 = vigorous physical activity or exercise three times or more per week, 0 = others), and body mass index (BMI). Although BMI is not a direct measure for health behaviors, it is closely related to eating behaviors. We use measured height and weight to calculate BMI and group results into four categories: normal or underweight (BMI <25), overweight (25 ≥ BMI < 30), obese (30 ≥ BMI < 40), and morbidly obese (BMI ≥40) (WHO Expert Committee, 1995). Missing values on BMI (about 4%) were imputed with the mean. Excluding these cases and including them as a separate category led to similar results.
Analytic Approach
We use lagged dependent variables to analyze the incidence of diabetes between two waves. Specifically, we use Wave 1 marital quality and change in marital quality between Waves 1 and 2 to predict Wave 2 diabetes, controlling for Wave 1 diabetes and all other covariates. We estimate binary logistic regression models to assess diabetes risk and multinomial logistic regression models to assess diabetes management as predicted by marital quality. Because our preliminary analysis revealed similar results (data not shown) when our models included positive and negative marital quality simultaneously and separately, we report only the final models that include both measures of marital quality simultaneously.
We estimate a sequence of models. We start by examining the general relationship between marital quality and diabetes risk and management controlling for sociodemographic covariates only. Next, we add measures of health behaviors and psychological distress separately. This allows us to test the idea that health behaviors and psychological distress may mediate the relationship between marital quality and diabetes. Since preliminary results (available upon request) showed no evidence of mediation, we report only the final full model, in which all covariates are controlled—including sociodemographic, health behavior-related covariates, and psychological distress. We note that our ability to test those potential mediation mechanisms is limited as our measures of health behaviors are not extensive and we do not have direct measures of social control. We stratify all analyses by gender and use t tests to assess the statistical significance of the gender differences. Results from t tests (data not shown) suggest that gender differences in all key findings are statistically significant.
Correction for Sample Selection Bias
We restrict our analyses to respondents who were married at both waves, so the samples select those with relatively good marital quality; marriages of poor quality are more likely to have ended. Moreover, sample attrition between waves—due to mortality, poor health, refusal, or inability to locate the respondent—is not random. Therefore, we apply Heckman’s (1979) approach to adjust sample selection biases due to marriage and mortality selections (see Liu, 2012 and Liu and Waite, 2014, for similar applications). This approach entails using logistic regression to model the probability that a respondent would die between Waves 1 and 2 and the probability that a respondent would be married at both waves, conditional on a set of predictors measured at Wave 1. Then for individuals who did not die and who were married at both waves, we modeled diabetes as a function of a set of independent variables, including the estimated probabilities of dying and of being married at both waves. By using this Heckman-type correction, we have adjusted our estimates of diabetes risk and management for factors that may affect that risk as well as for the tendency to die and the tendency to remain married.
Results
Table 2 shows the weighted descriptive statistics of all analyzed variables for the subsamples of diabetes risks (N = 1,228) and diabetes management (N = 389). From Table 2, we can see that 18.55% of respondents were diabetic at Wave 1 and that this proportion rises rapidly to 29.57% at Wave 2. There are only modest changes in marital quality over time.
Table 2.
Weighted Descriptive Statistics
| Diabetes Risk (N = 1,228) | Diabetes Management (N = 389) | ||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Min | Max | Marital Quality | Mean (SD) | Min | Max | |
| Marital Quality | |||||||
| Positive marital quality W1 | 0.05 (0.86) | −3.75 | 0.95 | Positive marital quality W1 | 0.06 (0.79) | −3.52 | 0.95 |
| Negative marital quality W1 | −0.05 (0.79) | −0.96 | 2.56 | Negative marital quality W1 | −0.03 (0.76) | −0.94 | 2.39 |
| Positive marital quality W2 | 0.06 (0.83) | −3.56 | 0.96 | Positive marital quality W2 | 0.01 (0.86) | −3.56 | 0.95 |
| Negative marital quality W2 | −0.04 (0.77) | −0.81 | 2.60 | Negative marital quality W2 | −0.04 (0.76) | −0.81 | 2.60 |
| Diabetes | Percent/mean (SD) | Diabetes | Percent/mean (SD) | ||||
| Diabetes risk W1 | Diabetes management W1 | ||||||
| Nondiabetic | 81.45 | Controlled diabetes | 12.63 | ||||
| Diabetic | 18.55 | Undiagnosed diabetes | 5.20 | ||||
| Uncontrolled diabetes | 20.72 | ||||||
| Nondiabetic or missing | 61.44 | ||||||
| Diabetes risk W2 | Diabetes management W2 | ||||||
| Nondiabetic | 70.43 | Controlled diabetes | 34.28 | ||||
| Diabetic | 29.57 | Undiagnosed diabetes | 34.41 | ||||
| Uncontrolled diabetes | 31.31 | ||||||
| Covariates W1 | Covariates W1 | ||||||
| Gender | Gender | ||||||
| Female | 37.87 | Female | 33.35 | ||||
| Male | 62.13 | Male | 66.65 | ||||
| Age groups | Age groups | ||||||
| 57–64 | 54.05 | 57–64 | 54.86 | ||||
| 65–74 | 31.61 | 65–74 | 29.26 | ||||
| 75–85 | 14.34 | 75–85 | 15.89 | ||||
| Race ethnicity | Race ethnicity | ||||||
| Non-Hispanic white | 84.33 | Non-Hispanic white | 79.62 | ||||
| Non-Hispanic black | 6.24 | Non-Hispanic black | 10.33 | ||||
| Hispanic | 6.98 | Hispanic | 7.25 | ||||
| Others | 2.45 | Others | 2.79 | ||||
| Education | Education | ||||||
| No diploma | 12.25 | No diploma | 13.81 | ||||
| High school graduate | 23.35 | High school graduate | 24.21 | ||||
| Some college | 32.53 | Some college | 30.31 | ||||
| College graduate | 31.87 | College graduate | 31.68 | ||||
| Relative family income | Relative family income | ||||||
| Below average | 16.72 | Below average | 16.95 | ||||
| Average | 35.47 | Average | 32.63 | ||||
| Above average | 33.06 | Above average | 30.71 | ||||
| Missing | 14.75 | Missing | 19.71 | ||||
| Smoke | Smoke | ||||||
| No | 86.46 | No | 88.64 | ||||
| Yes | 13.54 | Yes | 11.36 | ||||
| Drink | Drink | ||||||
| No | 34.00 | No | 43.27 | ||||
| Yes | 66.00 | Yes | 56.73 | ||||
| BMI | BMI | ||||||
| Normal or underweight | 21.55 | Normal or underweight | 13.86 | ||||
| Overweight | 41.93 | Overweight | 36.57 | ||||
| Obesity | 32.94 | Obesity | 44.65 | ||||
| Morbidly obese | 3.58 | Morbidly obese | 4.93 | ||||
| Physical activity | Physical activity | ||||||
| <3 times per week | 32.59 | <3 times per week | 43.19 | ||||
| ≥3 times per week | 67.41 | ≥3 times per week | 56.81 | ||||
| Medications | Medications | ||||||
| Does not take diabetes medications | 86.43 | Does not take diabetes medications | 58.16 | ||||
| Takes diabetes medications | 12.78 | Takes diabetes medications | 40.57 | ||||
| Missing | 0.79 | Missing | 1.27 | ||||
| Psychological distress | 4.28 (4.33) | Psychological distress | 4.91 (4.70) | ||||
| Probability of death between W1 and W2 | 0.09 (0.08) | Probability of death between W1 and W2 | 0.10 (0.08) | ||||
| Probability of staying married in both waves | 0.56 (0.21) | Probability of staying married in both waves | 0.55 (0.20) | ||||
Note: BMI = body mass index; W1 = Wave 1; W2 = Wave 2.
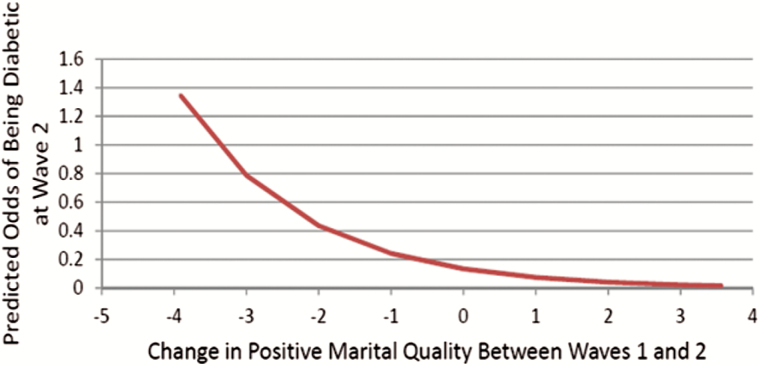
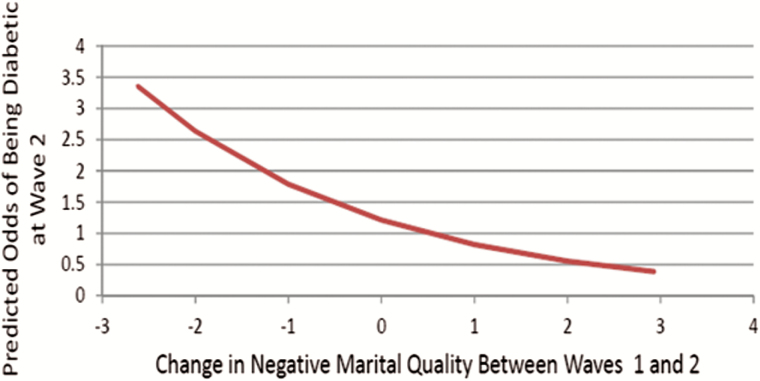
Table 3 shows estimated regression coefficients from binary logistic regression models for diabetes risk predicted by marital quality for the total sample and by gender. To facilitate interpretation, we use exponentiation to derive the odds ratios. Results from Table 3 suggest that after Wave 1 diabetes status and all other covariates are controlled, increases in both positive and negative marital quality between Wave 1 and Wave 2 are significantly associated with lower odds of having diabetes at Wave 2 for the total sample. Yet the results of our gender analysis (Table 3, also presented in Figures 1 and 2) reveal that the relationship between positive marital quality and diabetes risk is only present for women, while the relationship between negative marital quality and diabetes risk is only present for men. Specifically, when we hold constant Wave 1 diabetes status and all other covariates, for women (shown in Figure 1), every one unit increase of positive marital quality between Waves 1 and 2 decreases the odds of being diabetic at Wave 2 by 45% (i.e., 1 − exp (−0.59)), whereas, surprisingly, for men (shown in Figure 2), every one unit of increase in negative marital quality between Waves 1 and 2 decreases the odds of being diabetic at Wave 2 by 32% (i.e., 1 − exp(−0.39)).
Table 3.
Estimated Regression Coefficients From Binary Logistic Regression Models for Marital Quality to Predict Diabetes Risk
| Total Sample | Women | Men | |
|---|---|---|---|
| W1 PMQ | 0.04 (0.17) | −0.18 (0.19) | 0.12 (0.22) |
| Change PMQ W2-W1 | −0.30* (0.12) | −0.59* (0.26) | −0.11 (0.19) |
| W1 NMQ | −0.14 (0.23) | −0.53 (0.34) | −0.03 (0.25) |
| Change NMQ W2-W1 | −0.41** (0.14) | −0.47 (0.27) | −0.39* (0.16) |
| Constant | −1.35 (0.80) | −2.01 (1.21) | 0.19 (1.14) |
| N = 1,228 | N = 474 | N = 754 |
Note: PMQ = positive marital quality; NMQ = negative marital quality; W1 = Wave 1; W2 = Wave 2. Standard errors in parentheses. All models control for age, race, education, income, diabetes status at W1, probability of death between W1 and W2, probability of remaining married in both waves, smoking, drinking, BMI, physical activity level, taking diabetes medications, and psychological distress.
***p < .001. **p < .01. *p < .05.
Figure 1.
Diabetes risk and positive marital quality for women.
Figure 2.
Diabetes risk and negative marital quality for men.
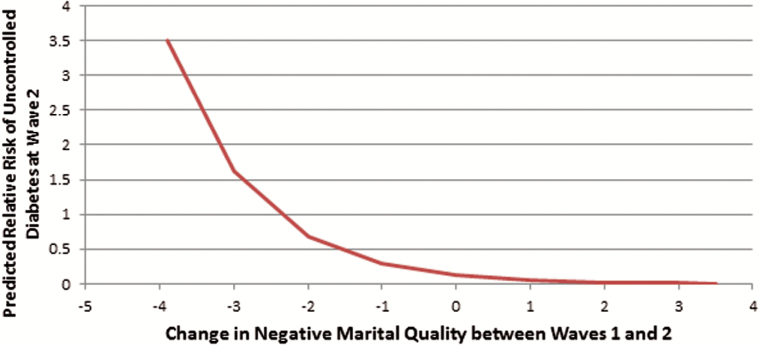
Table 4 shows the results for diabetes management. The relative risk ratios can be derived by using exponentiation of the reported coefficients. These results suggest that after Wave 1 diabetes management and all other covariates are controlled, an increase in negative marital quality between Waves 1 and 2 is significantly associated with lower risks of uncontrolled diabetes at Wave 2, but only for men. Specifically, when we hold constant Wave 1 diabetes management status and all other covariates, every one unit of increase in negative marital quality between Waves 1 and 2 decreases the relative risk of uncontrolled diabetes at Wave 2 by about 58% (i.e., 1 − exp(−0.86)) for men. This result for men is illustrated in Figure 3.
Table 4.
Estimated Regression Coefficients From Multinomial Logistic Regression Models for Marital Quality to Predict Diabetes Management
| Total Sample | Women | Men | ||||
|---|---|---|---|---|---|---|
| Undiagnosed vs. Controlled | Uncontrolled vs. Controlled | Undiagnosed vs. Controlled | Uncontrolled vs. Controlled | Undiagnosed vs. Controlled | Uncontrolled vs. Controlled | |
| W1 PMQ | −0.31 (0.26) | 0.01 (0.28) | −0.42 (0.44) | 0.04 (0.44) | −0.06 (0.53) | −0.02 (0.45) |
| Change PMQ W2-W1 | −0.23 (0.28) | −0.12 (0.26) | 0.28 (0.47) | 0.89 (0.45) | −0.44 (0.41) | −0.30 (0.33) |
| W1 NMQ | −0.33 (0.32) | −0.52 (0.38) | −0.34 (0.52) | −0.21 (0.64) | 0.05 (0.43) | −0.66 (0.59) |
| Change NMQ W2-W1 | 0.05 (0.29) | −0.57* (0.26) | 0.67 (0.53) | 0.50 (0.49) | −0.05 (0.46) | −0.86** (0.29) |
| Constant | −14.68*** (1.04) | −3.38* (1.42) | −18.68*** (3.19) | −3.92 (2.45) | −14.97*** (1.76) | −2.10 (1.91) |
| N = 389 | N = 136 | N = 253 | ||||
Note: PMQ = positive marital quality; NMQ = negative marital quality; W1 = Wave 1; W2 = Wave 2. Standard errors in parentheses. All models control for age, race, education, income, diabetes status at W1, probability of death between W1 and W2, probability of remaining married in both waves, smoking, drinking, BMI, physical activity level, taking diabetes medications, and psychological distress.
***p < .001. **p < .01. *p < .05.
Figure 3.
Diabetes management and negative marital quality for men.
Discussion and Conclusion
Although family and health scholars have long argued that marriage may promote health (Waite & Gallagher, 2000), this protective effect is highly contingent upon the quality of marriage (Liu & Waite, 2014; Umberson et al., 2006). This study highlights the importance of marital quality for the development and management of diabetes in later life. We provide nationally representative, population-based, longitudinal evidence of this relationship, and we give particular attention to gender variation. Based on previous clinical evidence, we hypothesized that those with higher levels of negative marital quality would subsequently experience both greater diabetes risk and worse diabetes management than those with lower levels of negative marital quality, and those with higher levels of positive marital quality would subsequently experience lower diabetes risk and better diabetes management than those with lower levels of positive marital quality (Hypotheses 1 and 2). Our results provide mixed evidence for these hypotheses depending to a large extent on gender (Hypothesis 3).
For women, we find that an increase in positive marital quality may reduce the risk of subsequent diabetes over time. This finding contrasts with a recent national study’s finding that more positive marital exchanges are related to decreased diabetes prevalence for men but not for women (Whisman et al., 2014). That study analyzed a cross-sectional sample, whereas our study used a longitudinal design. Moreover, our finding accords with previous clinical evidence suggesting that marital quality affects women’s health more than men’s (Kiecolt-Glaser & Newton, 2001). Women may be more sensitive than men to the quality of a relationship and thus more likely to experience a health boost from a good-quality relationship (Liu, Waite, Shen, & Wang, in press). Scholars often contend that poor marital quality and marital loss are especially detrimental to women’s health (Liu & Waite, 2014; Zhang & Hayward, 2006). Our results show the positive side, suggesting that good marital quality may promote women’s metabolic health. Future studies should examine the specific social, psychological, behavioral, and biological mechanisms through which positive marital quality promotes women’s metabolic health.
Our most surprising finding is that, for men, an increase in negative marital quality may decrease the risk of developing diabetes and increase the chances of managing diabetes after its onset. It is likely that those men who experienced an increase in negative marital quality are more likely to be self-regulated or self-centered than other men that may promote their health—suggesting a selection process. Another possibility is that our measure of negative marital quality does not reflect intense conflict in the relationship but is based on reports that the spouse often “criticizes” or “makes too many demands.” These may reflect the wife’s efforts to regulate the husband’s health behaviors that would explain this finding. Indeed, we note that this gender finding is consistent with the long-standing literature on gender differences in social control of health behaviors. A social control perspective suggests that spouses control each other’s health habits, and such social control attempts are more common among women than men (Tucker & Anders, 2001; Umberson, 1992). Wives are more likely than husbands to regulate a spouse’s health behaviors, perhaps especially if the husband is diabetic and/or in poor health. Both the development and treatment of diabetes are highly affected by lifestyle. Diabetes requires day-to-day (and even more frequent) monitoring that the wives could nudge the husband to do. Such efforts may improve the spouse’s health outcomes but at the same time can be very annoying and can provoke behavioral resistance, hostility, and emotional distress for the spouse—suggesting a “dual effects” process of spouse control (Tucker & Anders, 2001). This “dual effects” process may increase the conflict and marital strain over time between spouses but at the same time decrease the chance of developing diabetes and promote the husband’s success in controlling his diabetes. Indeed, our finding is in line with a couple of recent studies that also find marital strain may be protective for certain health outcomes (e.g., cognitive decline; Xu, Thomas, & Umberson, 2016), whereas marital support may not be, especially for men (Carr et al., 2016).
Moreover, although the spouse’s control of health behavior has long been posited to promote the partner’s health (Tucker & Anders, 2001; Umberson, 1992), recent empirical studies find that spouses’ pressure is actually associated with increases in patients’ diabetes-specific distress and decreases in dietary adherence and thus poor health outcomes (Stephens et al., 2013). Some scholars argue that the consequences of social control on the target of the control attempts depends on individual life context that determines the target’s affective responses to the social control attempts: people experiencing a more positive affective response to the spouse’s control are more likely to engage in desired behaviors (Tucker & Anders, 2001). Although we cannot directly test this hypothesis, our additional analyses (data not shown) that includes the interaction of positive and negative marital quality suggest that an increase in negative marital quality decreases diabetes risk over time only when the levels of positive marital quality are high. Future research should consider different life contexts of negative marital quality for men as well as specific mechanisms through which such contexts affect people’s response to their spouse’s control attempt and thus may lead to different health outcomes.
This study is limited in several ways. First, it is based on two waves of longitudinal data. Although we attempt to tease out some selectivity issues and causal relationships, we are limited by sample size, especially for diabetes management when looking at men and women separately. We work from the social control and the stress perspectives to consider how marital quality may affect later diabetes development and management, but it is also likely that diabetes status affects later change of marital quality—suggesting a potential reversal causality. To better understand these selection and causation processes, future studies should employ longitudinal data with larger sample sizes and more follow-up waves. The NSHAP is currently collecting its third wave of data that will provide opportunities to further untangle causality. Second, our samples are restricted to respondents who survived and were married in both waves. Therefore, our conclusions may only apply to a selected population of older adults; our conclusions are more relevant to older adults who are not in very poor health, are less likely to die, and are more likely to stay married. This study is, however, based on a random sample from that segment of the population. Moreover, we are not able to distinguish Type 1 and Type 2 diabetes due to data limitations, but the development of these two types of diabetes may be different in response to marital quality. Since 95% of adult diabetes are Type 2 (CDC, 2014), our results apply primarily to this group. Finally, various social, biological, psychological, and behavioral mechanisms underlie the link between marital quality and diabetes. Future studies should seek to identify the precise mechanisms and processes through which marital quality and diabetes affect each other and address how those mechanisms and processes vary by gender.
Despite its limitations, our study makes significant contributions to the literature on marital quality and health. We use a nationally representative, longitudinal data set to build on clinical evidence of the importance of marital quality for metabolic health. More importantly, our results add to the mixed evidence on gender differences in the links between marital quality and health in later life. Although growing evidence suggests that women’s health is especially vulnerable to poor marital quality and marital loss (Liu & Waite, 2014), our results reveal an optimistic finding: positive marital quality benefits women’s metabolic health in later life. Since diabetes is the fastest growing chronic condition in the United States, implementation of public policies and programs designed to promote marital quality should also reduce the risk of diabetes and promote health and longevity, especially for women at old ages. Surprisingly, we find that, for older men, negative marital quality may slow the development of diabetes and promote successful treatment after its onset. These results challenge the traditional assumption that negative marital quality is always detrimental to health and encourage family scholars to further distinguish different sources and types of negative marital quality.
Funding
This research was supported by the National Institute on Aging K01 Award K01AG043417 to H. Liu, the MERIT Award R37AG030481 to L. Waite, and by grants R01 AG043538, R01 AG033903, and P30 AG012857 from the National Institute on Aging as well as R03 HD078754 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of Behavioral and Social Sciences Research.
Acknowledgments
H. Liu planned the study, developed the framework, supervised and participated in the data analysis, and wrote the initial paper. L. Waite helped with conceptualization and participated in writing and revision of the paper. S. Shen conducted the data analysis and helped with literature review. An earlier draft of this paper is presented at the 2015 annual meeting of the Population Association of America, San Diego, California.
References
- American Diabetes Association. (2010). Diagnosis and classification of diabetes mellitus. Diabetes Care, 33(Suppl 1), S62–S69. doi:10.2337/dc11-s062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- August K. J. Rook K. S. Franks M. M., & Parris Stephens M. A (2013). Spouses’ involvement in their partners’ diabetes management: Associations with spouse stress and perceived marital quality. Journal of Family Psychology, 27, 712–721. doi:10.1037/a0034181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnethon M. R. Kinder L. S. Fair J. M. Stafford R. S., & Fortmann S. P (2003). Symptoms of depression as a risk factor for incident diabetes: Findings from the National Health and Nutrition Examination Epidemiologic Follow-up Study, 1971–1992. American Journal of Epidemiology, 158, 416–423. doi:10.1093/aje/kwg172 [DOI] [PubMed] [Google Scholar]
- Carr D. Cornman J. C., & Freedman V. A (2016). Marital quality and negative experienced well-being: An assessment of actor and partner effects among older married persons. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 71, 177–187. doi:10.1093/geronb/gbv073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2011). National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2014). National diabetes statistics report: Estimates of diabetes and its burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Donoho C. J. Crimmins E. M., & Seeman T. E (2013). Marital quality, gender, and markers of inflammation in the MIDUS Cohort. Journal of Marriage and the Family, 75, 127–141. doi:10.1111/j.1741-3737.2012.01023.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galinsky A. M., & Waite L. J (2014). Sexual activity and psychological health as mediators of the relationship between physical health and marital quality. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 69, 482–492. doi:10.1093/geronb/gbt165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomero A. McDade T. Williams S., & Lindau S. T (2008). Dried blood spot measurement of glycosylated hemoglobin (HbA1c) in wave 1 of the National Social Life Health & Aging Project (NSHAP). Chicago, IL: NORC and the University of Chicago. [Google Scholar]
- Heckman J. J. (1979). Sample selection bias as a specification error. Econometrica, 47, 153. doi:10.2307/1912352 [Google Scholar]
- Kiecolt-Glaser J. K., & Newton T. L (2001). Marriage and health: His and hers. Psychological Bulletin, 127, 472–503. doi:10.1037/0033-2909.127.4.472 [DOI] [PubMed] [Google Scholar]
- Kotwal A. A. Lauderdale D. S. Waite L. J., & Dale W (2016). Differences between husbands and wives in colonoscopy use: Results from a national sample of married couples. Preventive Medicine, 88, 46–52. doi:10.1016/j.ypmed.2016.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H. (2012). Marital dissolution and self-rated health: age trajectories and birth cohort variations. Social Science & Medicine (1982), 74, 1107–1116. doi:10.1016/j.socscimed.2011.11.037 [DOI] [PubMed] [Google Scholar]
- Liu H., & Waite L (2014). Bad marriage, broken heart? Age and gender differences in the link between marital quality and cardiovascular risks among older adults. Journal of Health and Social Behavior, 55, 403–423. doi:10.1177/0022146514556893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H. Waite L. J. Shen S., & Wang D (in press). Is sex good for your health? A national study on partnered sexuality and cardiovascular risk among older men and women. Journal of Health and Social Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutfey K., & Freese J (2005). Toward some fundamentals of fundamental causality: Socioeconomic status and health in the routine clinic visit for diabetes. American Journal of Sociology, 110, 1326–1372. doi:10.1086/428914 [Google Scholar]
- Marshall S. M., & Flyvbjerg A (2006). Clinical review: Prevention and early detection of vascular complications of diabetes. British Medical Journal, 333, 475–480. doi:10.1136/bmj.38922.650521.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Robles T. F., & Kiecolt-Glaser J. K (2003). The physiology of marriage: Pathways to health. Physiology & Behavior, 79, 409–416. doi:10.1016/s0031-9384(03)00160-4 [DOI] [PubMed] [Google Scholar]
- StataCorp LP (2012). Stata 10 User’s Guide. College Station, TX: Author. [Google Scholar]
- Stephens M. A. P. Franks M. M. Rook K. S. Iida M. Hemphill R. C., & Salem J. K (2013). Spouses’ attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes. Health Psychology, 32, 1029–1037. doi:10.1037/a0030018 [DOI] [PubMed] [Google Scholar]
- Taylor S. E. Klein L. C. Lewis B. P. Gruenewald T. L. Gurung R. A. R., & Updegraff J. A (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107, 411–429. doi:10.1037/0033-295x.107.3.411 [DOI] [PubMed] [Google Scholar]
- Trief P. M. Himes C. L. Orendorff R., & Weinstock R. S (2001). The marital relationship and psychosocial adaptation and glycemic control of individuals with diabetes. Diabetes Care, 24, 1384–1389. doi:10.2337/diacare.24.8.1384 [DOI] [PubMed] [Google Scholar]
- Trief P. M. Wade M. J. Britton K. D., & Weinstock R. S (2002). A prospective analysis of marital relationship factors and quality of life in diabetes. Diabetes Care, 25, 1154–1158. doi:10.2337/diacare.25.7.1154 [DOI] [PubMed] [Google Scholar]
- Trief P. M. Morin P. C. Izquierdo R. Teresi J. Starren J. Shea S., & Weinstock R. S (2006). Marital quality and diabetes outcomes: The IDEATel project. Families, Systems, & Health, 24, 318–331. doi:10.1037/1091-7527.24.3.318 [Google Scholar]
- Trief P. M. Ploutz-Snyder R. Britton K. D., & Weinstock R. S (2004). The relationship between marital quality and adherence to the diabetes care regimen. Annals of Behavioral Medicine, 27, 148–154. doi:10.1207/s15324796abm2703_2 [DOI] [PubMed] [Google Scholar]
- Tucker J. S., & Anders S. L (2001). Social control of health behaviors in marriage. Journal of Applied Social Psychology, 31, 467–485. doi:10.1111/j.1559–1816.2001.tb02051.x [Google Scholar]
- Umberson D. (1992). Gender, marital status, and the social control of health behavior. Social Science and Medicine, 34, 907–917. doi:10.1016/0277-9536(92)90259-s [DOI] [PubMed] [Google Scholar]
- Umberson D. Williams K. Powers D. A. Chen M. D., & Campbell A. M (2005). As good as it gets? A life course perspective on marital quality. Social Forces, 84, 493–511. doi:10.1353/sof.2005.0131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D. Williams K. Powers D. A. Liu H., & Needham B (2006). You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior, 47, 1–16. doi:10.1177/002214650604700101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite L. J. Laumann E. O. Levinson W. Lindau S. T., & O’Muircheartaigh C. A (2014). National Social Life, Health, and Aging Project (NSHAP): Wave 1. ICPSR20541-v6. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]. [Google Scholar]
- Waite L. J. Cagney K. Dale W. Huang E. Laumann E. O. McClintock M. O’Muircheartaigh C. A. Schumm L. P., & Cornwell B (2014). National Social Life, Health, and Aging Project (NSHAP): Wave 2 and Partner Data Collection. ICPSR34921-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]. [Google Scholar]
- Waite L. J., & Gallagher M (2000). The case for marriage: Why married people are happier, healthier, and better off financially. New York, NY: Doubleday. [Google Scholar]
- Warner D. F., & Adams S. A (2016). Physical disability and changes in loneliness among married older adults: The role of changing social relations. Society & Mental Health. Advance online publication. doi:10.1177/2156869315616257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman M. A. Li A. Sbarra D. A., & Raison C. L (2014). Marital quality and diabetes: Results from the Health and Retirement Study. Health Psychology, 33, 832–840. doi:10.1037/hea0000064 [DOI] [PubMed] [Google Scholar]
- Whisman M. A. Uebelacker L. A., & Settles T. D (2010). Marital distress and the metabolic syndrome: Linking social functioning with physical health. Journal of Family Psychology, 24, 367–370. doi:10.1037/a0019547 [DOI] [PubMed] [Google Scholar]
- WHO Expert Committee. (1995). Physical status: The use and interpretation of anthropometry. WHO Technicoal Report Series 854. Geneva, Switzerland: World Health Organization. [PubMed] [Google Scholar]
- Xu M. Thomas P. A., & Umberson D (2016). Marital quality and cognitive limitations in late life. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 71, 165–176. doi:10.1093/geronb/gbv014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., & Hayward M. D (2006). Gender, the marital life course, and cardiovascular disease in late midlife. Journal of Marriage and Family, 68, 639–657. doi:10.1111/ j.1741-3737.2006.00280.x [Google Scholar]