Abstract
Objective
The objectives of this study were to determine whether job strain is more strongly associated with higher ambulatory blood pressure (ABP) among blue-collar workers compared to white-collar workers; to examine whether this pattern generalizes across working and nonworking days and across sex; and to examine whether this pattern is accounted for by psychosocial factors or health behaviors during daily life.
Methods
480 healthy workers (mean age = 43; 53% female)in the Adult Health and Behavior Project – Phase 2 (AHAB-II)completed ABP monitoring during 3 working days and 1 nonworking day. Job strain was operationalized as high psychological demand (> sample median) combined with low decision latitude (< sample median) (Karasek model; Job Content Questionnaire).
Results
Covariate-adjusted multilevel random coefficients regressions demonstrated that associations between job strain and systolic and diastolic ABP were stronger among blue-collar workers compared to white-collar workers (b = 6.53, F(1, 464)= 3.89, p = .049 and b = 5.25, F(1, 464)= 6.09, p = .014, respectively). This pattern did not vary by sex but diastolic ABP findings were stronger when participants were at work. The stronger association between job strain and ABP among blue-collar workers was not accounted for by education, momentary physical activity or substance use, but was partially accounted for by covariation between higher hostility and blue-collar status.
Conclusions
Job strain is associated with ABP among blue-collar workers. These results extend previous findings to a mixed-sex sample and nonworking days and provide, for the first time, comprehensive exploration of several behavioral and psychosocial explanations for this finding.
Keywords: occupational stress, socioeconomic status, cardiovascular, ambulatory blood pressure, reserve capacity, job strain
Introduction
Research suggests that occupational characteristics contribute to adverse health outcomes, including cardiovascular disease (CVD) (1). “Job strain” is an occupational exposure characterized by high psychological demands and low decision latitude or control over work activities (2). The job strain model predicts that high psychological demands at the workplace, whether subjective or objective, may contribute to disease risk, while having control over one's schedule and one's work may mitigate the pathogenic effects of psychological demands (3). Constructive debate continues regarding standardizing the measurement of the job strain construct and conceptualization of the mechanisms by which it influences health (4). Despite these complexities, meta-analyses have found consistent associations between job strain and CVD (5). Case-control and cohort studies demonstrate that the association between job strain and CVD morbidity and mortality may be strongest among blue-collar workers (6-8). Evidence is consistent with the possibility that disproportionate cardiovascular impacts of job strain among blue-collar workers may even manifest in elevated blood pressure, a CVD risk factor, but this warrants further investigation (9).
Existing studies on the association between job strain and blood pressure are not entirely consistent, with some finding a stronger association between job strain and blood pressure among blue-collar workers (10, 11); others indicating that the association between job strain and blood pressure is stronger among low occupational status workers only if they are male and only with respect to meeting hypertension criteria (12); and one finding that the association between job strain and blood pressure is not significantly stronger amongst blue-collar workers (13). Inconsistent findings may be due to differences in sample characteristics, measurement or formulation of job strain, blood pressure assessment methodology, and adjustment for important covariates, such as physical activity.
The most recent evidence that job strain disproportionately affects the blood pressure of lower occupational status workers is a study of working women, which found that job demand was directly associated with systolic ambulatory blood pressure (ABP) and job control inversely associated with systolic ABP only among blue-collar workers (but not others) (11). Although the job strain components were examined separately in this study rather than as a job strain variable due to power constraints, the pattern of findings suggests that the effect of job strain (the combination of high demand and low control) on ABP is strongest among blue-collar workers. One limitation of this study (11) and others in this area (10,13) is that ABP measures were collected only on workdays. No study has examined whether the differential association of job strain and ABP by occupation status is seen to the same extent on nonworking days. Demonstrating this pattern on a nonworking day would indicate that the differential ABP influence of job strain among blue-collar workers is chronic, and not just acutely experienced in the workplace context. Further, although this most recent study (11) included data on location (e.g., work, home) during the workday, the authors reported insufficient power to examine whether the stronger associations between job characteristics and workday ABP among blue-collar workers generalized across workday ABPs recorded in work and home settings. Although it also improved on previous studies in men with methodology that allowed adjustments for physical activity and substance use at the time of ABP, adjustments for “momentary” cigarette smoking were not made. Adjustments for momentary behaviors (cigarette use, physical activity, and substance use) and overall biobehavioral patterns (body mass index (BMI), general smoking status, and typical drinking habits) are important given that occupational status and job strain are associated with these momentary behaviors and biobehavioral patterns (4, 5, 14, 15, 16), all of which are major risk factors for momentary elevations in blood pressure during daily life (17) and chronic blood pressure elevation (18). It is noteworthy, for example, that our research team typically utilizes momentary assessments of posture, physical activity, and substance use as time-varying covariates, and have found each to be significantly associated with acute fluctuations in cardiovascular activity (17).
Further, no prior research comprehensively examined whether individual-level socioeconomic and psychosocial factors play a role in the stronger relationship between job strain and ABP among blue-collar workers. Prior studies tested the moderating effects of education and income on job strain in models separate from occupation or did not consider education or income. Given differences in education and income across occupations, it is important to determine whether the occupation-job strain interaction reflects differences in occupational characteristics or differences in access to social capital as a function of education or income. Moreover, studies examining the combined effects of occupation and job strain typically do not examine the roles of personality and psychosocial characteristics not tied to the work environment in accounting for observed effects (5). Only one study examined the role of a personality factor, i.e., Type A behavior, but did not find it to be an explanatory factor (13).
The reserve capacity model (RCM) (19-20) identifies a series of biopsychosocial pathways (e.g., higher negative emotions and cognitions and/or reduced positive resources such as optimism and social support) by which lower socioeconomic status (SES) may contribute to negative health outcomes. Given that blue-collar occupational status is one manifestation of lower SES and concomitant with other manifestations of lower SES such as lower education, the RCM model is applicable for understanding the psychosocial conditions of blue-collar workers. Informed by this model, we examined whether the differential association between job strain and ABP among blue-collar workers compared to white-collar workers may be attributed to differences in negative emotions or psychosocial resources available to cope with job strain.
In addition, with one exception (12), all studies in this area focused on sex-restricted samples. Existing findings cannot address whether the interaction between occupational status and job strain differs by sex.
The aims of the current study were to examine differential associations between job strain and ABP by occupation, and to explore some of the possible mechanisms accounting for these effects, including health behaviors and educational and psychosocial resources. In addition, our design allowed us to extend effects observed in previous studies across sex (men and women) and across context (working vs. nonworking days and settings).
Method
Participants
Participants were drawn from the Adult Health and Behavior Project – Phase 2 (AHAB-II), a comprehensive study of psychosocial factors, behavioral and biological risk factors, and subclinical CVD. AHAB-II was approved by the University of Pittsburgh Institutional Review Board. AHAB-II participants were recruited from the community primarily through mass mailings of recruitment letters to individuals selected from voter registration lists and other public domain lists. Participants who responded to the recruitment letter were screened for eligibility.
To be eligible to participate in AHAB-II, individuals had to be between the ages of 30 and 54 years and employed at least 25 hours per week outside of the home. Individuals were excluded from participation if they (a) had a history of CVD, schizophrenia or bipolar disorder, chronic hepatitis, renal failure, major neurological disorder, chronic lung disease, or stage 2 hypertension (blood pressure ≥ 160/100 mm Hg); (b)consumed > 35 alcoholic drinks per week; (c)used fish-oil supplements (because of requirements for another sub-study); (d) were prescribed insulin or glucocorticoid, anti-arrhythmic, antihypertension, psychotropic, lipid-lowering, or weight-loss medications; (e) had less than 8th grade reading skills; or (f) were shift workers. Pregnant women were also excluded. As the protocol included magnetic resonance imaging, remaining exclusion criteria were claustrophobia; presence of medical devices, implants, or other metal objects in or on the body that could not be removed; tattooed eyeliners; or a very large body habitus.
Participants received compensation up to $410, depending on extent of participation in visits as well as compliance with the protocol. A community sample of 494 men and women completed the ambulatory protocol between March 2008 and October 2011. Due to missing data, study analyses were run on a subset of 480 participants (see Statistical Analyses section).
Procedure
Participants completed IRB-approved informed consent forms when enrolled in AHAB-II and completed six laboratory visits at the University of Pittsburgh in approximately 4 to 8 weeks. The current study uses data obtained during Visits 1-3. Specifically, during Visit 1, participants completed a structured interview regarding demographic, occupational, and health behavior characteristics. Between Visits 2 and 3, participants completed a 4-day ABP monitoring protocol during waking hours on three working days and one nonworking day. While wearing the ABP monitor, participants completed self-report ecological momentary assessments (EMAs) immediately following each ABP measure to permit examination of time-varying covariates of ABP, such as physical activity and substance use. During Visit 3, participants completed questionnaires assessing job strain and other psychosocial variables.
Measures
Demographics
Participants self-reported age, race/ethnicity, sex, and years of schooling (i.e., education).
Occupational status
Participants self-reported job title, industry, responsibilities, and relevant credentials (e.g., degrees or licenses) during a structured interview. This information was used by trained research staff to classify participants into 4-level Standard Occupation Classification (SOC) codes (21) based on primary job title. In the rare case when the appropriate SOC code was unclear, code assignments were verified by consensus within the research team. SOC codes were aggregated into three broad occupation groups for the purpose of analysis: blue-collar, sales and administrative support, and white-collar. This grouping is a higher-level aggregation of the standard 6 group aggregation recommended by the Standard Occupational Classification Policy Committee (21) and parallels the 3 occupational classes used in other studies (8). Individuals with SOC codes within the 31-0000 through 39-0000 levels (service), 45-0000 level (agricultural), 47-0000 level (construction), 49-0000 level (installation, maintenance, and repair), 51-0000 level (production), and 53-0000 level (transportation and material moving) were considered blue-collar. Individuals with SOC codes within the 41-0000 level (sales) and 43-0000 level (administrative support) were considered to be in sales or administrative support positions. Individuals with SOC codes within the 11-0000 level (managerial), 13-0000 level (business operations), and 15-0000 through 29-0000 levels (professional) were considered white-collar.
Job strain
Job strain was assessed using the Job Content Questionnaire (JCQ) (22). The JCQ subscales used in assessing job strain are the psychological demands (5 items), skill discretion (6 items), and decision authority (3 items) subscales. The psychological demand subscale assesses workload and intensity (“My job requires working very fast”), the skill discretion subscale assesses degree of creative challenge (“My job requires a high level of skill”), and the decision authority subscale assesses authority over daily tasks (“My job allows me to make a lot of decisions on my own”). Psychological demand was calculated as a weighted sum of the five psychological demand items and had an internal reliability of 0.72 (Cronbach's alpha). Decision latitude, representing a global measure of job control, was computed from the weighted sum of the skill discretion and decision authority subscales and had internal reliability of .84 (Cronbach's alpha). Adequate 3-year test-retest reliabilities of .64 have been reported for these subscales (23). Consistent with one traditional approach (24, 25), participants above the sample median score of 32 on the psychological demand subscale and below the sample median score of 38 on the decision latitude subscale were categorized as experiencing job strain. All other participants were categorized as not experiencing job strain. We focused on examining job strain (dichotomous measure) rather than the interaction of job demand and job control (cross-product score) for several reasons. A meta-analysis and individual studies found that, compared to job demand or control alone, the job strain dichotomous measure is a more powerful indicator of risk for high ABP when combined with low SES (13, 26). Further, the job strain operationalization and demand-control interaction are conceptually and empirically different (27). The interaction is not of theoretical interest here, only the specific combination of high demand and low control, i.e., job strain. The demand-control interaction determines whether these factors modify each other, but without a particular focus on those who perceive themselves as involved in high demand, low control work. When the cross-product term is used, statistical tests do not distinguish between those with high demand, low control jobs and those with low control, high demand jobs because they have similar cross-product term scores. Nonetheless, for the purposes of comparison, we conducted supplemental analyses examining the associations of continuous job demands, job control, and their interaction with ABP (see Statistical Analyses section).
Psychosocial variables
Per the RCM, positive psychosocial resource indicators were optimism (Life Orientation Test-Revised) (28), social support (Interpersonal Support Evaluation List) (29), job social support (22), and social network size (Social Network Index) (30). Indicators of negative emotions and cognitions were hostility (Buss-Perry Aggression Questionnaire) (31), depressive symptomatology (Beck Depression Inventory) (32), and negative affect (Positive and Negative Affect Schedule-Expanded) (33).
ABP
ABP was assessed using a 4-day protocol (3 working days and 1 nonworking day). Participants wore the oscillometric Oscar 2™ ABP monitor (SunTech Medical®, Inc., North Carolina) for two 2-day monitoring periods, usually one period at the beginning of the work week and one at the end of the work week (including a weekend day) with at least one non-monitoring day in between. On each monitoring day, the cuff worn on the upper arm inflated every hour during waking hours and the monitor recorded blood pressure. Telephone calls were made to participants before and during monitoring periods to remind them of upcoming monitoring responsibilities and determine if participants had questions or technical difficulties. The Oscar 2™ has been validated to the standards of several international protocols (34, 35).
ABP covariates
After each hourly ABP cuff inflation, participants completed a brief electronic diary entry on a handheld personal digital assistant (Palm Z22). Participants reported their location (home, work, vehicle, etc.), posture (on feet, sitting, or lying down), temperature comfort (comfortable, too cold, or too hot), and speaking status (yes or no) at the time of ABP assessment; physical activity during the 10 minutes before ABP assessment (limited, light, moderate, or heavy); and consumption of a meal, snack, alcoholic drink, caffeine, or drug in the hour before ABP assessment (yes or no for each). Additionally, each time participants smoked a cigarette, they reported this activity in a separate electronic diary form on the same device, which was used to calculate the number of cigarettes smoked each hour.
Between-subjects covariates
Body mass index (BMI) was calculated based on height and weight measured in the clinic (kg/m2). Participants self-reported smoking status (non-smoker, ex-smoker, current smoker, and other tobacco user) and number of alcoholic drinks in the month prior to data collection.
Statistical Analyses
For the purpose of analyses, race/ethnicity was recoded into two dummy variables (whites vs. others, blacks vs. others). Male sex was coded as 1 and female sex as 0. Occupational status was recoded into two dummy variables (blue-collar status vs. others, sales-administrative support status vs. others). Several time-varying variables were also recoded into dummy variables: location was recoded as being at work (vs. at any other location), posture as standing vs. others and sitting vs. others, temperature comfort as too cold vs. others and too hot vs. others, and physical activity as light activity vs. others, moderate activity vs. others, and heavy activity vs. others.
Preliminary analyses
Occupational differences in demographics, BMI, health behaviors, job strain, and ABP were examined using ANOVA and chi square analyses. ABP covariates were assessed for inclusion in primary systolic and diastolic ABP analyses using multilevel random coefficients regressions applied to all assessment points (PROC MIXED, SAS 9.3).
Primary analyses
Primary ABP analyses were conducted using multilevel random coefficients regression analyses (PROC MIXED, SAS 9.3). All ABP covariates that were associated with systolic and/or diastolic ABP (ps < .100) in preliminary analyses were included in the corresponding primary ABP analyses as covariates. Age, sex, white race, black race, years of education, BMI, smoking status, and number of alcoholic drinks in the past month were also treated as covariates. Because of a priori hypotheses that the association between job strain and ABP would be stronger among blue-collar as compared to white-collar workers, ABP analyses included dummy variables for blue-collar status and sales-administrative support status (thus, white-collar status as the reference group). Each of these occupation dummy variables (white-collar as the reference), job strain, and the multiplicative interaction term between them were entered as between-subjects effects in analyses for systolic and diastolic ABP. Each primary analysis was repeated three times, once with each of the following variables entered into three-way interactions with each occupation dummy variable and job strain: workday, location, and sex. Appropriate lower order two-way interactions were included in each analysis.
Twelve participants were missing Visit 3 job strain data. Two participants were missing smoking status data (one of which was also missing BMI data). Final primary ABP analyses included 480 participants with complete data.
For comparison purposes, we also conducted supplemental analyses to examine the associations of continuous job demands, job control, and their interaction with ABP using the same covariates mentioned above and to examine whether occupational status further moderated this interaction.
Secondary psychosocial analyses
Occupational differences in psychosocial factors (psychosocial resources and negative emotions and cognitions) were examined using ANOVAs and Kruskal-Wallis tests (nonparametric one-way analyses of variance). Psychosocial factors that differed by occupation were included in subsequent analyses. Multilevel random coefficients regression analyses were used to test the interaction of each resource factor with job strain (e.g., optimism*job strain) to test the hypothesis that positive resources buffer the effects of job strain on ABP. Separate multilevel random coefficients regression analyses were used to test the interaction of each negative emotion and cognition factor with job strain (e.g., hostility*job strain) to test the hypothesis that negative emotions or cognitions exacerbate the effects of job strain on ABP. Psychosocial-factor-by-job-strain interaction terms that were significant were entered in the model along with occupation-by-job-strain interactions to determine whether the psychosocial factor in question might account for or explain the effects of occupational status. The sample sizes for some secondary psychosocial analyses were lower than that for primary analyses and varied depending on missing data on respective psychosocial variables (Ns from 468-480).
Results
Mean age of participants in the analytic sample (N = 480) was 42.8 years and mean years of education was 16.9. Approximately 52.7% of participants were female and 17.1% were African American. The analytic sample included 326 white-collar workers, 93 sales-administrative support workers, and 61 blue-collar workers. See Table 1 for results of tests for occupational differences in demographics, BMI, health behaviors, job strain, and ABP. Twenty-three percent of the sample experienced job strain.
Table 1. Demographic and Clinical Characteristics of the Analytic Sample by Occupation (N = 480).
| White-Collar (n = 326) | Sales / Administrative Support (n = 93) | Blue-Collar (n = 61) | χ2 | |
|---|---|---|---|---|
| Characteristic | ||||
|
| ||||
| Mean (SD) | ||||
|
| ||||
| Mean age (SD) | 42.2 (7.4) | 44.1 (7.0) | 43.8 (7.1) | 5.6 |
| Mean years of education (SD) | 17.8 (2.7)a,b | 15.2 (2.3)a | 14.5 (1.8)b | 128.0**** |
| Mean BMI (SD) | 26.4 (4.9)a | 28.6 (6.0)a | 28.1 (5.7) | 12.5** |
| Mean drinks per month (SD) | 10.9 (14.5) | 11.0 (21.6) | 14.9 (24.5) | 2.3 |
| Mean systolic ABP (SD) | 133.0 (11.9)a | 134.8 (11.8) | 136.7 (10.1)a | 7.2* |
| Mean diastolic ABP (SD) | 80.4 (7.3)a | 81.2 (7.6) | 82.8 (6.7)a | 6.3* |
|
| ||||
| % (n) | ||||
|
| ||||
| % Female (n) | 50.9 (166)a | 66.7 (62)a,b | 41.0 (25)b | 11.1** |
| % AfricanAmerican (n) | 10.7 (35)a,b | 26.9 (25)b | 36.1 (22)a | 31.1**** |
| % current smokers (n) | 9.5 (31)a | 12.9 (12)b | 34.4 (21)a,b | 34.5**** |
| % job strain (n) | 16.9 (55)a,b | 36.6 (34)b | 36.1 (22)a | 22.4**** |
Note. For omnibus tests,
p < .050,
p < .010,
p < .001,
p < .0001.
For Bonferroni-corrected pairwise comparisons, groups that share superscripts are significantly different from each other at p < .050.
A total of 25,545 valid ABP assessments (an average of 53 ABP assessments per participant) were obtained, 9400 of which were completed at work. The following time-varying covariates were associated with systolic and/or diastolic ABP (ps< .100) in preliminary analyses and included in corresponding primary ABP analyses as covariates: type of day (workday vs. non-workday), location (at work vs. not at work), posture, physical activity, temperature, speaking, alcohol consumption, caffeine consumption, drug consumption, meal consumption, snack consumption, and number of cigarettes smoked in the past hour.
Primary Results: Differential Association between Job Strain and ABP among Blue-Collar versus White-Collar Workers
Systolic ABP final analysis
Covariates
Significant between-subjects covariates associated with systolic ABP (ps< .050) were sex (b = 6.76), white race (b = -8.72), BMI (b = .46), and drinks per month (b = .10). Years of education was not associated with systolic ABP (p = .50). Many of the time-varying covariates were significantly associated with systolic ABP (ps < .050), with ABP being higher during workdays and moments at work and during moments of greater physical activity, standing or sitting (vs lying down), cigarette smoking, caffeine or meal consumption, no drug consumption, temperature discomfort, and speaking1.
Interaction between occupational status and job strain
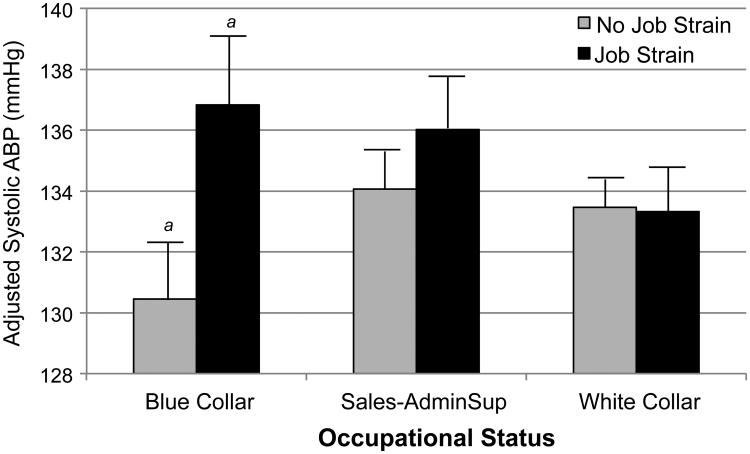
The interaction between blue-collar status (vs. white-collar) and job strain on systolic ABP was significant, b = 6.53, F(1, 464)= 3.89, p = .049, indicating that the association between job strain and systolic ABP was stronger among blue-collar workers compared to white-collar workers (Table 2). For blue-collar workers, the difference in mean systolic ABP between those with job strain and those without was 6.4 mm Hg (p = .010, with those having job strain exhibiting higher systolic ABP); this difference was .2 mmHg and non-significant among white-collar workers. The interaction between sales-administrative support status (vs. white-collar) and job strain was not significant, F(1, 464)= .57, p = .45. These results did not vary by sex, type of day, or location. See Figure 1 for illustration of systolic ABP differences by occupation and job strain.
Table 2. Multilevel Regression - Adjusted Effects of Job Strain on ABP by Occupation.
| ba | SE | F | |
|---|---|---|---|
| Systolic ABP | |||
| Job strain | -.15 | 1.60 | .01 |
| Blue-collar (vs. white-collar) | -3.02 | 1.96 | 2.39 |
| Sales-admin.sup (vs. white-collar) | .59 | 1.63 | .13 |
| Job strain × blue-collar (vs. white-collar) | 6.53 | 3.31 | 3.89* |
| Job strain × sales-admin.sup (vs. white-collar) | 2.12 | 2.80 | .57 |
| Diastolic ABP | |||
| Job strain | -1.31 | 1.03 | 1.60 |
| Blue-collar (vs. white-collar) | -1.94 | 1.26 | 2.37 |
| Sales-admin.sup (vs. white-collar) | -.17 | 1.05 | .02 |
| Job strain × blue-collar (vs. white-collar) | 5.25 | 2.13 | 6.09* |
| Job strain × sales-admin.sup (vs. white-collar) | 2.06 | 1.80 | 1.29 |
Adjusted for age, sex, race, education, BMI, smoking status, number of drinks in the past month, and ABP covariates.
p < .050.
Figure 1.
Systolic ABP by occupation type and job strain adjusted for age, sex, race, education, BMI, smoking status, number of drinks in the past month, and ABP covariates. Bars represent standard error. a denotes groups that are significantly different from each other at the p < .050 level.
Diastolic ABP final analysis
Covariates
Significant between-subjects covariates associated with diastolic ABP (ps< .050) were age (b = .10), sex (b = 2.76), BMI (b = .26), and drinks per month (b = .07). Years of education was not associated with diastolic ABP (p = .66). Many of the time-varying covariates were significantly associated with diastolic ABP (ps < .050), with ABP being higher during workdays and moments of greater physical activity, standing or sitting (vs lying down), not speaking, cigarette smoking, caffeine consumption, no snack consumption, and feeling too cold2.
Interaction between occupational status and job strain
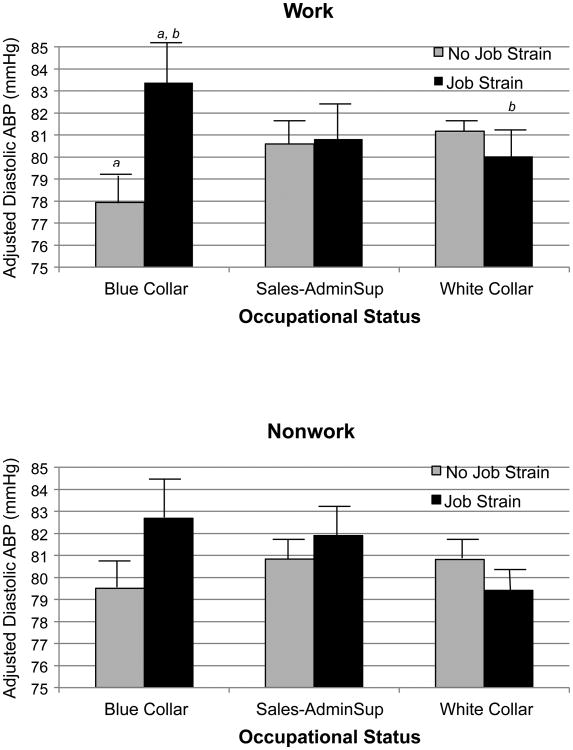
The interaction between blue-collar status (vs. white-collar) and job strain was significant, b = 5.25, F(1, 464)= 6.09, p = .014, indicating that the association between job strain and diastolic ABP was stronger among blue-collar workers as compared to white-collar workers. For blue-collar workers, the difference in mean diastolic ABP between those with job strain and those without was 4.0 mmHg (with those having job strain having higher diastolic ABP); this difference was 1.3 mmHg and non-significant among white-collar workers. These results did not vary by sex or type of day but were stronger when participants were at work (location*blue-collar status*job strain interaction: F(1, 25000) = 5.04, p = .025). Although job strain was significantly associated with diastolic ABP among blue-collar workers regardless of location (work: b = 5.77, F(1, 50)= 13.97, p < .001; non-work: b = 3.48, F(1, 50)= 4.70, p = .035), the adjusted mean DBP difference due to job strain was 5.8 mmHg for work time and 3.5 mmHg for non-work time. The interaction between sales-administrative support status (vs. white-collar) and job strain was not significant, F(1, 464)= 1.29, p = .26. These results did not vary by sex, type of day, or location. See Figure 2 for illustrations of diastolic ABP differences by occupation and job strain during work and nonwork time. Note that the pattern is strongest when participants were at work. Although blue-collar workers without job strain had lower work-time ABP than white-collar workers without job strain, this difference was not significant. Blue-collar workers with job strain had significantly higher work-time diastolic ABP than white-collar workers with job strain (p= .043) and blue-collar workers without job strain (p< .001), which supports the hypothesis that the combination of blue-collar occupational status and job strain is associated with the highest risk for elevated ABP.
Figure 2.
Diastolic ABP by occupation type and job strain during work time and nonwork time adjusted for age, sex, race, education, BMI, smoking status, number of drinks in the past month, and ABP covariates. Bars represent standard error. a denotes groups that are significantly different from each other at the p <.010 level. b denotes groups that are significantly different from each other at the p < .050 level.
Results of analyses using continuous job demand and job control scores did not parallel our job strain findings (Table S1, Suppplemental Digital Content 1).
Secondary Results: The Role ofPsychosocial Differences
Of the occupational categories, blue-collar workers had the lowest levels of optimism, job social support, and social network size and the highest levels of hostility. None of the interactions between optimism, job social support, or social network size, on the one hand, and job strain, on the other, was associated with ABP (results available upon request). Hostility interacted with job strain to predict both systolic ABP (b = .38, F(1, 455) = 4.10, p = .044) and diastolic ABP (b = .24, F(1, 455) = 3.90, p = .049), such that those with job strain and high hostility had the highest ABP. In systolic ABP analyses with both the blue-collar status-by-job strain interaction and hostility-by-job strain interaction included, the interaction between blue-collar status (vs. white-collar) and job strain was no longer significant, F(1, 451) = 2.82, p = .094, and the hostility-by-job strain interaction approached significance, F(1, 451) = 3.11, p = .079. Diastolic ABP analyses demonstrated that the blue-collar status-by-job strain interaction was robust to the inclusion of the hostility-by-job strain interaction.3
Discussion
Findings of the current study suggest that low occupational status workers are disproportionately exposed to job strain and disproportionately vulnerable to its effects on ABP. This study is the first to demonstrate this pattern on a nonworking day as well and included the most comprehensive examination of time-varying covariates and psychosocial factors as confounders of these associations. Diastolic ABP measured at work most strongly captured the effects of job strain among blue-collar workers, a pattern that is congruent with job strain being a workplace-specific exposure. However, this relationship was also observed among high strain blue-collar workers while not at work and on nonworking days, suggesting a chronic influence of job strain on cardiovascular health. It is noteworthy that this finding is robust to adjustment for health status (e.g., BMI); health behaviors (e.g., smoking status, monthly alcohol consumption); “momentary” factors (e.g., cigarette smoking, alcohol consumption, physical activity); and another indicator of SES (i.e., education). The benefit of using a healthy sample is the reduction of potential confounding effects of disease and medications on ABP. Hypertensive individuals were excluded from study participation, restricting the ABP range observed. It is possible that associations would be stronger in the general working population without this exclusion. Even in this healthy sample, though, blue-collar workers had significantly higher mean ABP than white-collar workers.
Our primary findings are plausible within a psychophysiological context. It is possible that the overall stress burden experienced by workers in blue-collar occupations may be associated with long-term alterations in sympathoadrenal arousal and vascular adaptations (i.e., vascular hypertrophy). For example, experimental studies suggest that low occupational status workers have slower blood pressure recovery after stress (36). Our finding that job strain is associated with the ABP of blue-collar workers even while outside the work environment seem to demonstrate chronic rather than transient ABP elevations due to work stress. This finding contributes to the theoretical understanding of the nature of the influence of job strain.
We explored the possibility that the apparent differential sensitivity of blue-collar workers to job strain may be attributed to psychosocial characteristics and not just blue-collar status per se. Consistent with the RCM model, blue-collar workers were burdened not only with greater job strain but also with other psychosocial challenges, i.e., lower optimism, job social support, and social network size, and higher hostility. Of these factors, only hostility exacerbated the association between job strain and ABP in that job strain had a stronger positive association with ABP among those with high hostility levels. Given that, for systolic ABP, the blue-collar status-by-job strain interaction was not robust to accounting for the hostility-by-job strain interaction, it is possible that the role of hostility in exacerbating the impact of job strain may have partially accounted for the stronger positive association between job strain and systolic ABP among blue-collar workers (as compared to white-collar workers). Socioeconomic conditions of relative deprivation among blue-collar workers may elicit cynicism, undermine trust, increase suspicion in interactions with others, and increase negative emotions such as hostility. This social vulnerability, when combined with environmental triggers such as job strain, may have downstream consequences for health. Research has demonstrated that individuals with higher hostility levels tend to perceive more hassles and interpersonal stressors and show exaggerated cardiovascular reactivity to these stressors and to job demands (37-41). Nevertheless, present results regarding the role of hostility should be interpreted with caution given that we conducted several analyses to explore psychosocial factors and only hostility was found to be promising. Future research should develop a priori hypotheses regarding the role of hostility in the influence of job strain on blue-collar workers' health. The current study contributes to our understanding of some of the mechanisms by which lower occupational status may increase susceptibility to the effects of job strain on health.
There may be other explanations for the differential effects of job strain across occupational status. Unmeasured factors, such as early life adversity or cumulative stress, may sensitize these workers to the effects of job strain. For example, one longitudinal study found that early life adversity was prospectively associated with a stronger positive association between job strain and allostatic load as an adult (42). It is also possible that job strain perceptions are qualitatively different in different work environments, e.g., a highly demanding blue-collar work environment may be demanding in a different way from a highly demanding white-collar work environment, and it may be that the demands of a white-collar work environment are less toxic for health. For example, white-collar workers (but not blue-collar workers) may experience less negative emotion when they have a higher workload (i.e., more demands) (43). Further, there is suggestive evidence that blue-collar workers and white-collar workers differ in how highly their self-reports of demand and control correlate with expert ratings of demand and control in their jobs (44), so future studies may benefit from including expert ratings to determine whether current findings hold.
The finding that sex did not moderate the interaction between occupational status and job strain in accounting for ABP may seem counterintuitive given complex sex patterns in cardiovascular outcomes (45) but a recent meta-analysis found that there were no sex differences in the impact of job strain on CHD (5). Further, previous studies demonstrated that occupational status and job strain (or demand and control) interact in predicting ABP in female (11) and male samples (10). Although one previous study, using sex-stratified analyses, found that the occupational status-job strain interaction had a slightly weaker association with ABP among females as compared to males (12), that study did not statistically examine the three-way interaction between sex, occupational status, and job strain, as we did in the current study. Although interesting, the lack of sex difference in our findings should be interpreted with caution given the modest number of female blue-collar workers in the sample.
The current study is not without limitations. One limitation is that the sample included only 61 blue-collar workers. Nevertheless, mean ABP and interaction estimates within the blue-collar-job strain groups had comparable standard errors to other groups, indicating that estimates in these groups are not less precise than those from other groups despite being based on fewer participants. We had a substantial number of ABP observations per participant, which increases reliability of the estimates. Another limitation is that participants did not wear ABP monitors while asleep. Sleep ABP is associated with long-term cardiovascular outcomes (46). Studies have found job strain to be associated with nighttime ABP (47), but have not examined whether this association varies by occupational status. Another limitation is the cross-sectional nature of the study. The only longitudinal study examining this occupation-by-job stress interaction included two time points, 3 years apart (10). Additional longitudinal studies with multiple time points and longer time courses are needed to examine whether cumulative effects of job strain on ABP vary by occupation. These studies would allow for dynamic exploration of psychosocial mechanisms and causal attribution. A fourth limitation is insufficient power to examine whether the occupation-by-job strain interaction differed by race. In final adjusted models, whites had significantly lower systolic ABP than non-whites. These residual racial disparities are noteworthy. Race and SES effects are difficult to disentangle, so future studies should recruit more ethnically diverse samples stratified by SES to permit such analyses.
Despite limitations, this study contributes to the literature in several ways. First, it statistically examined moderation of the occupation-job strain interaction by several daily life descriptors (e.g., work vs. non-worktime). To this effect, it demonstrated that blue-collar workers are more vulnerable to the effects of job strain on ABP even on non-work days but that the associations are stronger during work-time. Second, our mixed-sex sample allowed for more systematic examination of the associations across sex. Third, our findings showed that disproportional vulnerability to job stress amongst blue-collar workers is independent of educational, behavioral, and “momentary” differences but partially confounded with differences in hostility levels. Future research should document longitudinal effects of job strain exposures, as well as further explore the mechanisms by which occupational status increases vulnerability to job strain, including but not limited to hostility.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Source of Funding: This research was supported by National Institutes of Health Grants P01 HL040962 awarded to Drs. Manuck, Kamarck, and Muldoon and T32 HL007560 (fellowship) awarded to Dr. Joseph.
Glossary
- AHAB-II
Adult Health and Behavior Project – Phase 2
- ABP
ambulatory blood pressure
- BMI
body mass index
- CVD
cardiovascular disease
- EMA
ecological momentary assessment
- JCQ
Job Content Questionnaire
- MIL
maximum inflation level
- mmHg
millimeters of mercury
- RCM
reserve capacity model
- SES
socioeconomic status
- SOC
Standard Occupation Classification
Footnotes
Detailed results are available upon request.
Detailed results are available upon request.
Results did not differ when we re-ran all analyses using an objective measure of momentary physical activity rather than self-reported momentary physical activity. The momentary objective measure used was the average level of metabolic expenditure in the 15 minutes prior to ABP measurements based on Sensewear actigraphy data. Eight participants were missing this data so were not included in this analysis.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Nataria T. Joseph, Social Sciences Division, Pepperdine University.
Matthew F. Muldoon, Heart and Vascular Institute, Department of Medicine, University of Pittsburgh School of Medicine.
Stephen B. Manuck, Department of Psychology, University of Pittsburgh.
Karen A. Matthews, Departments of Psychiatry, Psychology, and Epidemiology, University of Pittsburgh.
Leslie A. MacDonald, National Institute for Occupational Safety and Health.
James Grosch, National Institute for Occupational Safety and Health.
Thomas W. Kamarck, Departments of Psychology and Psychiatry, University of Pittsburgh.
References
- 1.Brand JE, Warren JR, Carayon P, Hoonakker P. Do job characteristics mediate the relationship between SES and health? Evidence from sibling models. Soc Sci Res. 2007;36(1):222–53. [Google Scholar]
- 2.Karasek RA, Theorell T. Healthy work : stress, productivity, and the reconstruction of working life. New York: Basic Books; 1990. [Google Scholar]
- 3.Karasek R, Baker D, Marxer F, Ahlbom A, Theorell T. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health. 1981;71(7):694–705. doi: 10.2105/ajph.71.7.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith PM, LaMontagne AD. What is needed to make research on the psychosocial work environment and health more meaningful? Reflections and missed opportunities in IPD debates. Scand J Work Environ Health. 2015;41(6):594–596. doi: 10.5271/sjweh.3519. [DOI] [PubMed] [Google Scholar]
- 5.Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep. 2015;17:74–82. doi: 10.1007/s11886-015-0630-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson JV, Hall EM, Theorell T. Combined effects of job strain and social isolation on cardiovascular disease morbidity and mortality in a random sample of the Swedish male working population. Scand J Work Environ Health. 1989;15(4):271–9. doi: 10.5271/sjweh.1852. [DOI] [PubMed] [Google Scholar]
- 7.Hallqvist J, Diderichsen F, Theorell T, Reuterwall C, Ahlbom A. Is the effect of job strain on myocardial infarction risk due to interaction between high psychological demands and low decision latitude? Results from Stockholm Heart Epidemiology Program (SHEEP) Soc Sci Med. 1998;46(11):1405–15. doi: 10.1016/s0277-9536(97)10084-3. [DOI] [PubMed] [Google Scholar]
- 8.Ferrario MM, Veronesi G, Chambless LE, Sega R, Fornari C, Bonzini M, Cesana G. The contribution of major risk factors and job strain to occupational class differences in coronary heart disease incidence: the MONICA Brianza and PAMELA population-based cohorts. Occup Environ Med. 2011;68(10):717–22. doi: 10.1136/oem.2010.060822. [DOI] [PubMed] [Google Scholar]
- 9.Landsbergis P, Dobson M, Koutsouras G, Schnall P. Job strain and ambulatory blood pressure: a meta-analysis and systematic review. Am J Public Health. 2013;103(3):e61–71. doi: 10.2105/AJPH.2012.301153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landsbergis PA, Schnall PL, Warren K, Pickering TG, Schwartz JE. The effect of job strain on ambulatory blood pressure in men: does it vary by socioeconomic status? Ann N Y Acad Sci. 1999;896(1):414–6. doi: 10.1111/j.1749-6632.1999.tb08157.x. [DOI] [PubMed] [Google Scholar]
- 11.Gallo LC, Bogart LM, Vranceanu AM, Walt LC. Job characteristics, occupational status, and ambulatory cardiovascular activity in women. Ann Behav Med. 2004;28(1):62–73. doi: 10.1207/s15324796abm2801_8. [DOI] [PubMed] [Google Scholar]
- 12.Tsutsumi A, Kayaba K, Tsutsumi K, Igarashi M. Association between job strain and prevalence of hypertension: a cross sectional analysis in a Japanese working population with a wide range of occupations: the Jichi Medical School cohort study. Occup Environ Med. 2001;58(6):367–73. doi: 10.1136/oem.58.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landsbergis PA, Schnall PL, Pickering TG, Warren K, Schwartz JE. Lower socioeconomic status among men in relation to the association between job strain and blood pressure. Scand J Work Environ Health. 2003;29(3):206–15. doi: 10.5271/sjweh.723. [DOI] [PubMed] [Google Scholar]
- 14.Nyberg ST, Heikkilä K, Fransson EI, Alfredsson L, De Bacquer D, Bjorner JB, Bonenfant S, Borritz M, Burr H, Casini A, Clays E, Dragano N, Erbel R, Geusken GA, Goldberg M, Hooftman WE, Houtman IL, Jöckel K, Kittel F, Knutsson A, Koskenvuo M, Leineweber C, Lunau T, Madsen EH, Hanson LLM, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Rugulies R, Siegrist J, Suominen S, Vahtera J, Virtanen M, Westerholm PJM, Westerlund H, Zins M, Ferrie JE, Theorell T, Steptoe A, Hamer M, Singh-Manoux A, Batty GD, Kivimäki M for the IPD-Work Consortium. Job strain in relation to bodymass index: pooled analysis of 160 000 adults from 13 cohort studies. J Intern Med. 2012;272:65–73. doi: 10.1111/j.1365-2796.2011.02482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kivimäki M, Lawlor DA, Smith GD, Kouvonen A, Virtanen M, Elovainio M, Vahtera J. Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart disease: the Finnish Public Sector Study. Am J Public Health. 2007;97(5):874–879. doi: 10.2105/AJPH.2005.078691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nyberg ST, Fransson EI, Heikkilä K, Alfredsson L, Casini A, Clays E, De Bacquer D, Dragano N, Erbel R, Ferrie JE, Hamer M, Jöckel K, Kittel F, Knutsson A, Ladwig K, Lunau T, Marmot MG, Nordin M, Rugulies R, Siegrist J, Steptoe A, Westerholm PJM, Westerlund H, Theorell T, Brunner EJ, Singh-Manoux A, Batty GD, Kivimäki M for the IPD-Work Consortium. Job strain and cardiovascular disease risk factors: Meta-analysis of individual-participant data from 47,000 men and women. PLoS ONE. 8(6):e67323. doi: 10.1371/journal.pone.0067323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kamarck TW, Janicki DL, Shiffman S, Polka DE, Muldoon MF, Liebenauera LL, Schwartz JE. Psychosocial demands and ambulatory blood pressure: a field assessment approach. Physiol Behav. 2002;77:699–704. doi: 10.1016/s0031-9384(02)00921-6. [DOI] [PubMed] [Google Scholar]
- 18.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302(4):401–411.19. doi: 10.1001/jama.2009.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129(1):10. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 19.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129(1):10. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 20.Gallo LC, de los Monteros KE, Shivpuri S. Socioeconomic status and health: what is the role of reserve capacity? Curr Dir Psychol Sci. 2009;18(5):269–274. doi: 10.1111/j.1467-8721.2009.01650.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Bureau of Labor Statistics. Standard occupational classification and coding structure. 2010 Retrieved from http://www.bls.gov/soc/soc_2010_class_and_coding_structure.pdf.
- 22.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–55. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 23.Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG. A longitudinal study of job strain and ambulatory blood pressure: results from a three-year follow-up. Psychosom Med. 1998;60(6):697–706. doi: 10.1097/00006842-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Schnall PL, Pieper C, Schwartz JE, Karasek RA, Schlussel Y, Devereux RB, Ganau A, Alderman M, Warren K, Pickering TG. The relationship between “job strain”, workplace diastolic blood pressure, and left ventricular mass index. Results of a case-control study. J Am Med Assoc. 1990;263(14):1929–35. [PubMed] [Google Scholar]
- 25.Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG. Relation between job strain, alcohol, and ambulatory blood pressure. Hypertension. 1992;19:488–94. doi: 10.1161/01.hyp.19.5.488. [DOI] [PubMed] [Google Scholar]
- 26.Kivimaki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, Clays E, De Bacquer D, Dragano N, Ferrie JE, Geuskens GA, Goldberg M, Hamer M, Hooftman WE, Houtman IL, Joensuu M, Jokela M, Kittel F, Knutsson A, Koskenvuo M, Koskinen A, Kouvonen A, Kumari M, Madsen IEH, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Rugulies R, Salo P, Siegrist J, Singh-Manoux A, Suominen SB, Väänänen A, Vahtera J, Virtanen M, Westerholm PJM, Westerlund H, Zins M, Steptoe A, Theorell T for the IPD-Work Consortium. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491–7. doi: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bobko P. A solution to some dilemmas when testing hypotheses about ordinal interactions. J Appl Psychol. 1986;71(2):323. [Google Scholar]
- 28.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A re-evaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–78. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13:99–125. [Google Scholar]
- 30.Cohen S. Social supports and physical health. In: Greene A, Cummings M, Karraker K, editors. editors Life-Span Developmental Psychology: Perspectives on Stress and Coping. Hillsdale, NJ: Erlbaum Associates; 1991. [Google Scholar]
- 31.Buss AH, Perry M. The aggression questionnaire. J Pers Soc Psychol. 1992;63(3):452–9. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- 32.Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 33.Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule - Expanded Form. 1999 [Google Scholar]
- 34.Goodwin J, Bilous M, Winship S, Finn P, Jones SC. Validation of the Oscar 2 oscillometric 24-h ambulatory blood pressure monitor according to the British Hypertension Society protocol. Blood Press Monit. 2007;12(2):113–7. doi: 10.1097/MBP.0b013e3280acab1b. [DOI] [PubMed] [Google Scholar]
- 35.Jones SC, Bilous M, Winship S, Finn P, Goodwin J. Validation of the OSCAR 2 oscillometric 24-hour ambulatory blood pressure monitor according to the International Protocol for the validation of blood pressure measuring devices. Blood Press Monit. 2004;9(4):219–23. doi: 10.1097/00126097-200408000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Steptoe A, Feldman PJ, Kunz S, Owen N, Willemsen G, Marmot M. Stress responsivity and socioeconomic status. A mechanism for increased cardiovascular disease risk? Eur Heart J. 2002;23(22):1757–63. doi: 10.1053/euhj.2001.3233. [DOI] [PubMed] [Google Scholar]
- 37.Benotsch EG, Christensen AJ, McKelvey L. Hostility, social support, and ambulatory cardiovascular activity. J Behav Med. 1997;20(2):163–76. doi: 10.1023/a:1025530711432. [DOI] [PubMed] [Google Scholar]
- 38.Smith TW, Gallo LC. Hostility and cardiovascular reactivity during marital interaction. Psychosom Med. 1999;61(4):436–45. doi: 10.1097/00006842-199907000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Miller SB, Dolgoy L, Friese M, Sita A. Dimensions of hostility and cardiovascular response to interpersonal stress. J Psychosom Res. 1996;41(1):81–95. doi: 10.1016/0022-3999(96)00090-6. [DOI] [PubMed] [Google Scholar]
- 40.Burns JW, Katkin ES. Psychological, situational, and gender predictors of cardiovascular reactivity to stress: a multivariate approach. J Behav Med. 1993;16(5):445–65. doi: 10.1007/BF00844816. [DOI] [PubMed] [Google Scholar]
- 41.Burns JW, Hutt J, Weidner G. Effects of demand and decision latitude on cardiovascular reactivity among coronary-prone women and men. Behav Med. 1993;19(3):122–8. doi: 10.1080/08964289.1993.9935181. [DOI] [PubMed] [Google Scholar]
- 42.Westerlund H, Gustafsson PE, Theorell T, Janlert U, Hammarström A. Social adversity in adolescence increases the physiological vulnerability to job strain in adulthood: a prospective population-based study. PLoS ONE. 2012;7(4):e35967. doi: 10.1371/journal.pone.0035967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Axelrod WL, Gavin JF. Stress and strain in blue-collar and white-collar management staff. J Vocat Behav. 1980;17(1):41–9. [Google Scholar]
- 44.Theorell T, Hasselhorn HM. On cross-sectional questionnaire studies of relationships between psychosocial conditions at work and health—are they reliable? Int Arch Occup Environ Health. 2005;78(7):517–22. doi: 10.1007/s00420-005-0618-6. [DOI] [PubMed] [Google Scholar]
- 45.Kannel WB. The Framingham Study: historical insight on the impact of cardiovascular risk factors in men versus women. J Gend Specif Med. 2002;5(2):27–37. [PubMed] [Google Scholar]
- 46.Hermida RC, Ayala DE, Mojón A, Fernández JR. Blunted sleep-time relative blood pressure decline increases cardiovascular risk independent of blood pressure level—The “Normotensive Non-dipper” paradox. Chronobiol Int. 2013;30(1–2):87–98. doi: 10.3109/07420528.2012.701127. [DOI] [PubMed] [Google Scholar]
- 47.Clays E, Leynen F, De Bacquer D, Kornitzer M, Kittel F, Karasek R, De Backer G. High job strain and ambulatory blood pressure in middle-aged men and women from the Belgian Job Stress Study. Occup Environ Med. 2007;49(4):360–367. doi: 10.1097/JOM.0b013e31803b94e2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.