Abstract
Objective
Studies have revealed a phenomenon called skin-deep resilience, which develops in upwardly mobile African-American youth. They perform well in school, maintain good mental health, and avoid legal problems. Despite outward indications of success, they also show evidence of worse health in biomarker studies. Here we extend this research, asking whether it manifests in differential susceptibility to upper respiratory infection, and if it emerges in European-Americans as well.
Methods
The sample included 514 adults in good health, as judged by physician examination and laboratory testing. Subjects completed questionnaires about lifecourse socioeconomic conditions, conscientiousness, psychosocial adjustment, and lifestyle factors. They were subsequently inoculated with a rhinovirus that causes upper respiratory infection, and monitored in quarantine for 5 days the development of illness.
Results
Consistent with past work, African-Americans from disadvantaged backgrounds displayed indications of skin-deep resilience. To the extent these subjects were high in conscientiousness, they fared better across multiple domains of psychosocial functioning, as reflected in educational attainment, symptoms of depression, and close relationship quality (p values .01–.04). But analyses of these subjects’ susceptibility to infection revealed the opposite pattern; higher conscientiousness was associated with a greater likelihood of becoming ill following inoculation (p value = .03). In European-Americans, there was no evidence of skin-deep resilience; conscientiousness was associated with better psychosocial outcomes, but not infection risk.
Conclusions
These observations suggest that resilience may be a double-edged sword for African-Americans from disadvantaged backgrounds. The same characteristics associated with academic success and psychological adjustment forecast increased vulnerability to health problems.
Keywords: resilience, socioeconomic status, upward mobility, respiratory infection
There are pronounced racial disparities in health in the United States. While the magnitude of these disparities has declined in recent decades, Black Americans continue to have worse health and shorter lives compared with White Americans (Bleich, Jarlenski, Bell, & LaVeist, 2012; Williams, 2012). These trends are evident across the lifespan and apparent in multiple, though not all, categories of disease and disability (National Center for Health Statistics, 2012). Recent vital statistics show that Blacks live, on average, 3.8 (females) to 5.4 (males) fewer years than Whites (Harper, MacLehose, & Kaufman, 2014). One surprising feature of this life-expectancy gap is that its size increases with educational attainment. For example, Blacks without a high-school diploma live 3.1 fewer years than Whites with a comparable education. But the gap between Blacks and Whites with a college degree is 4.2 years (Braveman, Cubbin, Egerter, Williams, & Pamuk, 2010).
Based on these observations, researchers have suggested that upward mobility has diminishing returns for the health of Black Americans (Farmer & Ferraro, 2005). The factors that underlie this phenomenon are not yet clear. However, theorists have emphasized distinctive stressors that upwardly mobile Blacks may confront – including devaluation, workplace alienation, stereotype threat, outright discrimination, and cultural discontinuity (Geronimus, 1992; Hardaway & McLoyd, 2009; James, 1994; Johnson, Richeson, & Finkel, 2011). Research also highlights the behavioral and biological costs of coping strategies that individuals from disadvantaged social groups may deploy to regulate their emotions, keep pursuing goals, and maintain a positive identity in the face of these stressors (James, Strogatz, Wing, & Ramsey, 1987; Jackson, Knight, & Rafferty, 2010; Jackson, Redline, Kawachi, Williams, & Hu, 2013; Major, Mendes, & Dovidio, 2013; Sellers, Neighbors, Zhang, & Jackson, 2012; Zapolski, Pedersen, McCarthy, & Smith, 2014). Consistent with these observations, our group followed Black youth from the rural South across adolescence, and identified an upwardly mobile subgroup. Although these youths were raised in neighborhoods with concentrated poverty, they had graduated from high school and were enrolled in colleges and universities. Relative to other subjects, they had lower rates of cigarette, alcohol, and marijuana use. Despite their academic success and healthy lifestyles, these youths showed high cardiometabolic risk relative to other subjects, as reflected in a composite indicator of adiposity, blood pressure, and stress hormones (Chen, Miller, Brody, & Lei, 2015). These findings are part of broader phenomenon that we call “skin-deep resilience,” wherein outward indicators of achievement and competence co-occur with worse health in upwardly mobile youth.
The same general pattern has emerged in other analyses. For example, in two distinct samples of rural Black youth, we observed that higher self control forecasted better psychosocial outcomes years later, as reflected in lower levels of depressive symptoms, drug use, and aggressive behavior (Brody et al., 2013; Miller, Yu, Chen, & Brody, 2015). But in both cases self control related to indicators of physical health in the opposite direction. In other words, to the extent that youth had more self control, they subsequently displayed worse cardiometabolic risk profiles and faster epigenetic aging of immune cells (Brody et al., 2013; Miller et al., 2015). Importantly, this pattern of diverging outcomes was only evident among the sample’s most disadvantaged youth. For Black youth whose families enjoyed better socioeconomic conditions, self control presaged better outcomes across domains, as would be expected from the broader resilience literature (Blair & Raver, 2012; Luthar, 2006; Masten, 2001).
This collection of findings on skin-deep resilience raises several questions. First, because all of the results are from studies of Black youth from the rural South, it remains unclear whether the pattern is unique to this population, or represents a more general phenomenon that is evident across demographic and geographical lines. Second, all of the extant studies have used biomarkers to index physical health. While useful indicators of risk, biomarkers are not reflections of actual disease or disability. Studies are therefore needed to ascertain whether skin-deep resilience is associated with disparities in health that are clinically meaningful. Finally, more needs to be learned about the mechanisms through which skin-deep resilience arises. What behavioral and biological processes does upward mobility set into motion for highly disadvantaged youth, and how might they affect health?
To address these questions, we conducted secondary analyses of datasets from the Common Cold Project. In these studies, healthy adults completed extensive psychosocial and biological assessments, and were then inoculated with viruses known to cause upper respiratory infection (URI). They were subsequently monitored in quarantine for the emergence of signs and symptoms of illness. Using these datasets, we asked whether the pattern of skin-deep resilience observed in previous research would extend to Whites and Blacks from urban areas, and to the more clinically meaningful outcome of URI susceptibility.
We also explored potential behavioral and biological mechanisms. Although there are many possible origins of skin-deep resilience, we focus here on the hypothesis that achieving upwardly mobility is an intensely demanding process for disadvantaged youth. Simply put, they have more obstacles to overcome than privileged youth, and must do so with fewer resources and less support from their families, schools, and communities (Duncan & Murnane, 2011). These demands may explain why youth with skin-deep resilience display relatively high levels of cortisol in everyday life (Brody et al., 2013; Chen et al., 2015), a pattern that is associated with URI risk (Janicki-Deverts, Cohen, Turner, & Doyle, 2016). To cope with heavy demands on their time, upwardly mobile individuals also may neglect sleep. Indeed, a recent study found that African-American professionals are 30–50% more likely to have short sleep than European-Americans in the same occupation (Jackson et al., 2013). Brief sleep durations are associated with higher URI risks (Cohen, Doyle, Alper, Janicki-Deverts, & Turner, 2009; Prather, Janicki-Deverts, Hall, & Cohen, 2015). Finally, it is possible that individuals cope with the challenges of upward mobility through mood- repairing behaviors such as cigarette smoking and alcohol consumption. At first blush this hypothesis may seem unlikely, because past work finds that youth who display skin-deep resilience use fewer substances (Chen et al., 2015). But this pattern might change during the transition into adulthood. For instance, among African-Americans, rates of heavy substance use are low during childhood and adolescence, but climb steadily in the mid-20s relative to other racial/ethnic groups (Watt, 2008). Heavy consumption of cigarettes and alcohol increases URI susceptibility (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997; Cohen, Tyrrell, Russell, Jarvis, & Smith, 1993).
METHODS
The Common Cold Project is a publicly available archive (www.commoncoldproject.com) which contains five distinct studies addressing the role of psychosocial factors in URI susceptibility. Our analyses used data from two studies that included measures of childhood socioeconomic conditions: Pittsburgh Cold Study 2 (PCS2; conducted from 1997–2001; Cohen, Doyle, Turner, Alper, & Skoner, 2004) and Pittsburgh Cold Study 3 (PCS3; conducted from 2007–2011; Cohen et al., 2013a). In both studies, the sample was primarily comprised of subjects who self-identified as White (n = 226 and n = 142 with complete data in PCS2 and PCS3, respectively). A smaller proportion self-identified as Black (n = 99 in PCS2; n = 57 in PCS3), and a handful of subjects as another racial/ethnic background (n = 9 in PCS2; n = 13 in PCS3). In light of these demographics, and the significant power demands associated with the binary outcome variable of URI diagnosis, we decided to aggregate the datasets and to perform race-stratified analyses, testing hypotheses separately in Blacks and Whites, and omitting other racial/ethnic groups.
Sample
Both studies recruited subjects from the Pittsburgh, PA metropolitan area. To be included, subjects had to be 18–55 years old, fluent in English, and judged to be in good health. Before viral challenge, candidates had a physical examination with a study physician, who gathered medical history and ordered laboratory tests. Exclusion criteria included current pregnancy, history of chronic medical or psychiatric illness, most standing medication regimens, treatment with steroids or immune-modulating agent in the previous three months, a history of nasal or otologic surgery, and abnormal findings on complete blood count, urinalysis, or blood chemistry. Candidates also were excluded if they displayed URI symptoms during the first 24 hours of quarantine, i.e., prior to administration of the virus. Other trial-specific exclusion criteria are described in the original publications (Cohen et al., 2013a; Cohen et al., 2004). Both protocols were approved by Institutional Review Boards at Carnegie Mellon University and the University of Pittsburgh. All subjects provided written informed consent, and received an honorarium ($800 in PCS2, $1000 in PCS3).
Procedure
Candidates who passed the medical screening returned to the clinic within six weeks. During that session, subjects completed questionnaires about socioeconomic status, life stress and mood states, personality, and lifestyle, which are described below. On two subsequent days, they collected saliva at home multiple times daily for analysis of cortisol. Blood was collected to evaluate history of exposure to the challenge viruses by serology; in PCS2 this occurred 7–8 weeks prior to quarantine and in PCS3 3–5 days prior to quarantine. Within six weeks of saliva collection, subjects entered quarantine at a local hotel. On Day 0 (prior to viral challenge), they completed additional questionnaires, underwent a nasal examination, and collected more salivary cortisol samples. At the end of that day, subjects were inoculated with nasal drops that contained 100–300 tissue culture infective doses (50%) of a respiratory virus known to cause URI. PCS2 used two different viruses to evaluate the generalizability of effects - rhinovirus 39 (RV39; n = 228) and rhinovirus 23 (RV23; n = 106). In PCS3 only RV39 was used. Subjects remained in quarantine for 5 additional days. Each day they reported on cold symptoms, underwent objective assessments of mucus production and nasal congestion (mucuciliary clearance), and provided nasal lavage samples to measure viral shedding. Roughly 28 days later, subjects returned for another blood collection, used to verify infection by serology. The investigators were blinded to all psychological and biological measures.
Predictors
In previous work, skin-deep resilience has manifest as a crossover interaction between childhood SES and self control (Brody et al., 2013; Miller et al., 2015). Among highly disadvantaged youth, higher self control presaged worse health, whereas the opposite pattern was observed among more privileged youth. Here, we adopted a similar approach to the extent that was possible. Drawing on past work (Cohen et al., 2013b; Cohen et al., 2004; Miller & Chen, 2007) childhood SES was indexed through parental home ownership. Subjects were asked to report, for each year of childhood (ages 1–18), whether their parents owned the principal family residence. These data were used to compute a summary variable reflecting years of home ownership, which ranged from 0–18. The reliability and validity of this metric has been established in previous research (Cohen et al., 2013b; Cohen et al., 2004; Miller & Chen, 2007), which demonstrates that parental home ownership can be recalled accurately, and predicts a variety of outcomes related to physical health.
Unfortunately, none of the studies in the archive contained measures of self control. However, they did contain assessments of conscientiousness, a broad personality trait that encompasses self control, as well as other facets like industriousness and responsibility. Indeed, conscientiousness is defined as “individual differences in the propensity to be self controlled, responsible to others, hardworking, orderly, and rule abiding” (Roberts, Lejuez, Krueger, Richards, & Hill, 2014). To determine whether this conceptual overlap was also evident empirically, we analyzed a publicly available dataset consisting of 15,139 adults who completed a personality instrument (Roberts, Chernyshenko, Stark, & Goldberg, 2005) as part of the 2008 and 2010 waves of the Health and Retirement Study (Roberts, Smith, Jackson, & Edmonds, 2009). In this dataset, self control correlated strongly with overall conscientiousness, r = .62, which is consistent with the relationships observed in other large cohorts (Roberts et al., 2005; Tangney, Baumeister, & Boone, 2004). Accordingly, we adopted conscientiousness as a proxy for self control here. In PCS2, conscientiousness was measured on two occasions before quarantine, spaced apart by approximately 8 weeks, using items from Goldberg’s questionnaire (Goldberg, 1992). On a 5-point scale, subjects indicated how well each of 8 adjectives described them, e.g., “organized” and “thorough.” At both administrations, the scale was internally consistent (Cronbach’s alpha’s > .77), and subjects’ responses were stable across time (Spearman correlation = .75). Accordingly, we averaged responses across administrations. In PCS3, conscientiousness was measured with the International Personality Item Pool (Goldberg et al., 2006). On a 5-point scale, subjects indicated how accurately each of 10 statements described them, e.g., “Am always prepared” and “Like order.” The scale was internally consistent (Cronbach’s alpha’s = .83). To ensure that conscientiousness values from PCS2 and PCS3 were on the same metric, we standardized scores to a mean of 0 and standard deviation of 1. Past research indicates that conscientiousness scores from the two scales are highly related, with correlations ranging from.71 to .90 (Saucier & Goldberg, 2002).
Psychosocial Outcomes
As noted, skin-deep resilience entails outward indications of competence and achievement, coupled with worse health status. Using data from the Common Cold Project, we explored three indicators of competence and achievement, each representing a distinct domain of psychosocial functioning. They included years of education completed, symptoms of depression, and close relationship quality. Across both studies, subjects reported the total years of formal schooling they had completed. Symptoms of depression were assessed using the Trait Adjective Questionnaire (Cohen, Alper, Doyle, Treanor, & Turner, 2006; Usala & Hertzog, 1989;). On a five-point scale, subjects indicated how accurately three mood-related adjectives described how they generally or typically felt. The adjectives were sad, unhappy, and depressed (Cronbach’s α = .84). The quality of subjects’ close relationships was assessed using the Positive Relations with Others dimension, taken from Ryff’s Scales of Psychological Well-Being (Ryff, 1989). On a 6-point scale, respondents indicated how much they agreed with 9 statements, e.g., “People would describe me as a giving person, willing to share my time with others,” and “I know that I can trust my friends, and they know they can trust me.” Across studies, internal consistency was high, with Cronbach’s α = 0.76.
URI Diagnosis
The primary health outcome in our analyses was whether subjects developed a clinically verified URI. To receive a URI diagnosis, subjects had to display evidence of both infection (viral replication) and illness (signs and symptoms). Infection was coded as present if (a) the challenge virus was isolated in nasal secretions collected on any of the five post-inoculation days, or (b) subjects displayed a 4-fold increase in serum antibody to the challenge virus from baseline to 28 days post-quarantine. (In PCS2, baseline was 60 days before inoculation; whereas the interval for PCS3 ranged from 3–5 days.) The illness criterion was based on objective indicators of illness response after viral exposure – the amount of mucus produced and mucociliary clearance function. Mucus weights were determined by collecting used tissues in sealed plastic bags during quarantine, weighing them and then subtracting the weights of unused tissues and bags. After correcting for mucus weight at baseline, the post-inoculation weights were summed across the five days to create a adjusted total mucus score. Nasal mucociliary clearance function refers to the effectiveness of nasal cilia in clearing mucus from the nasal passage toward the throat. Clearance function was assessed as the time required for a dye administered into the nose to reach the throat. Each daily time was adjusted for baseline and the adjusted average time in minutes was calculated across the post-inoculation days of the trial. To meet illness criteria, subjects had to display a total adjusted mucus weight > 10 grams or an adjusted average mucociliary nasal clearance time > 7 minutes (Cohen et al., 1997).
Controls
The statistical models predicting URI susceptibility included four control variables that could provide alternative explanations for any observed associations. They were subject age and sex, plus challenge virus (RV23 vs. RV39) and pretrial serostatus (positive vs. negative). The latter variable reflects subjects’ history of exposure to the challenge virus. The immune system develops memories of previous infections by producing virus-specific antibodies, which can linger in blood for years. By measuring these antibodies before inoculation, we were able to categorize subjects as positive (titer > 4) vs. negative for previous exposure. Additional details of these procedures can be found in earlier publications (Cohen et al., 2013a; Cohen et al., 2004). In supplementary models, we also introduced covariates reflecting study (PCS2 vs. PCS3) and season of exposure (dummy variables representing fall, winter, spring, or summer). However, these covariates did not predict URI, or affect other results, so we omitted them from the final models to minimize risks of overfitting (Babyak, 2004). In psychosocial outcomes, we included age and sex as covariates, but omitted challenge virus and pretrial serostatus, as they are not plausible alternative explanations.
Mediators
We evaluated three mediators that could plausibly explain disparities in URI susceptibility. Sleep problems were assessed using the Pittsburgh Sleep Quality Instrument (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989), an extensively validated questionnaire, which yields estimates of typical nightly sleep duration and efficiency. Duration is computed as time in bed, minus latency to sleep and length of awakenings. Efficiency reflects the proportion of time in bed actually spent sleeping (sleep duration / time in bed). We considered the role of two unhealthy behaviors, cigarette smoking and heavy alcohol consumption, using self-report measures validated in our past work (Cohen et al., 1993). Smoking was represented as the number of cigarettes used in a typical day. Alcohol use was indexed as the number of drinks in a typical week, with a drink considered a beer, glass of wine, or shot of spirits. Because this variable had a strong right skew, we transformed it into a 3-category ordinal variable reflecting lower, medium, and higher consumption (0, 1–10, and 10 or more weekly drinks).
Diurnal patterns of cortisol secretion were assessed by having subjects collect saliva for three days. (The initial two days were at home, between screening and quarantine. The third was the initial/baseline day of quarantine.) In PCS2, 11 samples were collected on home days, and 14 samples during quarantine. In PCS3, the parallel numbers were 7 and 8. To render the assessments comparable, we focused on samples that were relatively similar across studies. At home, the common samples were collected at 1, 2, 4, 6–7, 8–9, 11–12, and 14 hours after waking. In quarantine, the common samples were collected at waking, 1 hour later, and 10am, 12pm, 1pm, and 3pm. Saliva was collected using salivettes (Sarstedt, Rommelsdorft, Germany), and subjects were instructed to abstain from eating food and brushing teeth for one hour prior to collection, and smoking for 30 minutes. Cortisol was measured via fluorescence immunoassay, with cortisol-biotin conjugate as a tracer (Polk, Cohen, Doyle, Skoner, & Kirschbaum, 2005). The average intra- and inter-assay coefficients of variation were less than 12%. Aggregating across each day’s values, we calculated a ground-referenced area-under-the-curve statistic, which reflects the total volume of diurnal cortisol secretion over the monitoring period (Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003).
Missing Data
The PCS2 and PCS3 datasets were almost fully complete. Of the 524 Black and White participants who underwent viral challenge, just 10 had missing data on the primary independent variables of early disadvantage and adult conscientiousness. Thus, the final analytic sample for primary analyses was 514 (364 Whites and 150 Blacks). In mediation analyses, there were an additional 14 cases of missing data for cortisol secretion and 3 cases for sleep duration. Given the nearly complete datasets, we did not impute missing values.
RESULTS
Table 1 displays sample characteristics. The subjects were primarily young adults, with a broad range of socioeconomic backgrounds and psychosocial characteristics. Because of the strict inclusion criteria, they were in good overall health, though a sizeable minority were smokers and/or overweight. Slightly more than a quarter developed a URI following viral inoculation.
Table 1.
Description of sample.
| Black Subjects | (n=150) | White Subjects | (n=364) | |
|---|---|---|---|---|
| Average / Percent | Standard Deviation | Average / Percent | Standard Deviation | |
| Age, years | 31.82 | 9.95 | 28.48 | 10.83 |
| Gender, % female | 48.00 | - | 49.18 | - |
| Education, years | 13.09 | 1.63 | 13.77 | 1.83 |
| Received rhinovirus 39, % | 76.00 | - | 81.86 | - |
| Pre-challenge seronegative, % | 52.67 | - | 67.31 | - |
| Time owned home ages 1–18, years | 7.75 | 7.53 | 13.44 | 6.25 |
| Never owned home ages 1–18, % | 36.00 | - | 10.98 | - |
| Conscientiousness, SD units | 0.16 | 0.94 | −0.05 | 1.01 |
| Body mass index, m/kg2 | 28.58 | 7.10 | 26.01 | 5.42 |
| Smoker (≥10 cigarettes/day), % | 13.1 | - | 15.9 | - |
| Alcoholic drinks, per week | 4.02 | 7.89 | 6.24 | 12.02 |
| Depressive symptoms, 0–12 | 0.83 | 1.64 | 1.51 | 1.89 |
| Close relationship quality, 9–54 | 40.56 | 6.77 | 41.84 | 6.94 |
| Developed URI after challenge, % | 26.67 | - | 27.47 | - |
Psychosocial Outcomes
Our first wave of analyses explored psychosocial outcomes. After stratifying the sample into White and Black subjects, we estimated a series of regression equations where outcomes were predicted from three sequentially entered blocks of variables: (1) the covariates age and sex, (2) the main effects of early disadvantage and adult conscientiousness, and (3) a product term representing the interaction of the latter two variables. The outcome variables were years of education, depressed mood, and close relationship quality.
Table 2 summarizes the results. A few themes are evident. First, there were generally main effects of conscientiousness (p’s from .001 to .04). Among Black subjects, conscientiousness was associated with more years of education, less depressed mood, and better close relationships. Among Whites, it was associated with less depressed mood and better close relationships. Second, across groups, a main effect of early disadvantage was evident for educational attainment (p’s < .005), but not for depressed mood or relationship quality (p’s ranged from .12 to .71). Third, none of the interaction terms that crossed early disadvantage with adult conscientiousness were significant (p’s from .09 to .65). Because some participants were aged 18–22 and may have still been in school, we redid education analyses using a developmentally normative outcome at 18 years, receipt of a high-school diploma. The results were the same; those Black subjects who completed high school reported higher levels of conscientiousness and less early disadvantage (p’s < .01).
Table 2.
Results of regression analyses predicting psychosocial outcomes.
| Black Subjects |
(n = 150) | White Subjects |
(n=364) | |||
|---|---|---|---|---|---|---|
| B (SE) | β | p | B (SE) | β | p | |
| Years of Education | ||||||
| Time owned home | .48 (.16) | .31 | .005 | .59 (.12) | .33 | <.001 |
| Conscientiousness | .48 (.18) | .27 | .01 | .17 (.11) | .09 | .13 |
| Time Owned Home × Conscientiousness | −.12 (.17) | −.07 | .47 | .18 (.11) | .11 | .09 |
| Depressive Symptoms | ||||||
| Time owned home | −.18 (.14) | −.11 | .19 | .04 (.10) | .02 | .71 |
| Conscientiousness | −.30 (.15) | −.18 | .04 | −.37 (.10) | −.20 | <.001 |
| Time Owned Home × Conscientiousness | −.07 (.15) | −.04 | .65 | .08 (.10) | .04 | .39 |
| Positive Relationships | ||||||
| Time owned home | .63 (.56) | .09 | .26 | .55 (.35) | .08 | .12 |
| Conscientiousness | 1.27 (.60) | .18 | .04 | 1.55 (.35) | .23 | <.001 |
| Time Owned Home × Conscientiousness | −.57 (.60) | −.08 | .34 | −.46 (.34) | −.07 | .18 |
Notes. The covariates age and sex also were included in these models. Due to space constraints, we omit those results here, but they are available upon request.
URI Diagnosis
Our second wave of analyses explored URI risk. In racial-group stratified binary logistic regressions, we predicted diagnosis from three sequentially entered blocks of variables: (1) the covariates age, sex, challenge virus, and pretrial serostatus, (2) main effects of early disadvantage and adult conscientiousness, and (3) a product representing the interaction of the latter variables.
Tables 3 and 4 present results of these analyses. Among White subjects, higher age, inoculation with RV39, and negative serostatus were associated with greater odds of developing a URI. As previously reported in these samples (Cohen et al., 2013b; Cohen et al., 2004), so was early socioeconomic disadvantage, as indexed by fewer years of family home ownership. Conscientiousness was not associated with URI, and the interaction term was non-significant.
Table 3.
Results of logistic regression in White subjects (n=364), predicting odds of developing clinically verified URI.
| B | SE B | p | Exp (B) | 95% CI Exp (B) | |
|---|---|---|---|---|---|
| Constant | −2.12 | .40 | < .001 | 0.12 | |
| Age | 0.33 | .12 | .006 | 1.38 | 1.10, 1.75 |
| Female gender | −0.10 | .25 | .70 | 0.91 | 0.56, 1.47 |
| Received rhinovirus 39 | 0.75 | .37 | .04 | 2.11 | 1.03, 4.32 |
| Seronegative to challenge virus | 0.85 | .29 | .003 | 2.35 | 1.33, 4.15 |
| Time owned home ages 1–18 | −0.33 | .12 | .006 | 0.72 | 0.57, 0.91 |
| Conscientiousness | 0.07 | .12 | .59 | 1.07 | 0.84, 1.36 |
| Time Owned Home × Conscientiousness | 0.15 | .12 | .19 | 1.17 | 0.93, 1.46 |
Notes. Age, time owned home, and conscientiousness are continuous predictors. The other predictors are categorical, and coded such that referents are male gender, challenged with rhinovirus 23, and seropositive to challenge virus (antibody titer of 4 or greater before challenge).
Table 4.
Results of logistic regression in Black subjects (n=150), predicting odds of developing clinically verified URI.
| B | SE B | p | Exp (B) | 95% CI Exp (B) | |
|---|---|---|---|---|---|
| Constant | −2.09 | .57 | < .001 | 0.12 | |
| Age | 0.07 | .21 | .74 | 1.07 | 0.71, 1.62 |
| Female gender | −0.20 | .40 | .62 | 0.82 | 0.37, 1.80 |
| Received rhinovirus 39 | 0.52 | .52 | .32 | 1.69 | 0.60, 4.71 |
| Seronegative to challenge virus | 1.07 | .43 | .01 | 2.90 | 1.25, 6.72 |
| Time owned home, ages 1–18 | −0.26 | .21 | .21 | 0.77 | 0.51, 1.16 |
| Conscientiousness | 0.10 | .22 | .66 | 1.10 | 0.72, 1.70 |
| Time Owned Home × Conscientiousness | −0.48 | .23 | .04 | 0.62 | 0.39, 0.98 |
Notes. Age, time owned home, and conscientiousness are continuous predictors. The other predictors are categorical, and coded such that referents are male gender, challenged with rhinovirus 23, and seropositive to challenge virus (antibody titer of 4 or greater before challenge).
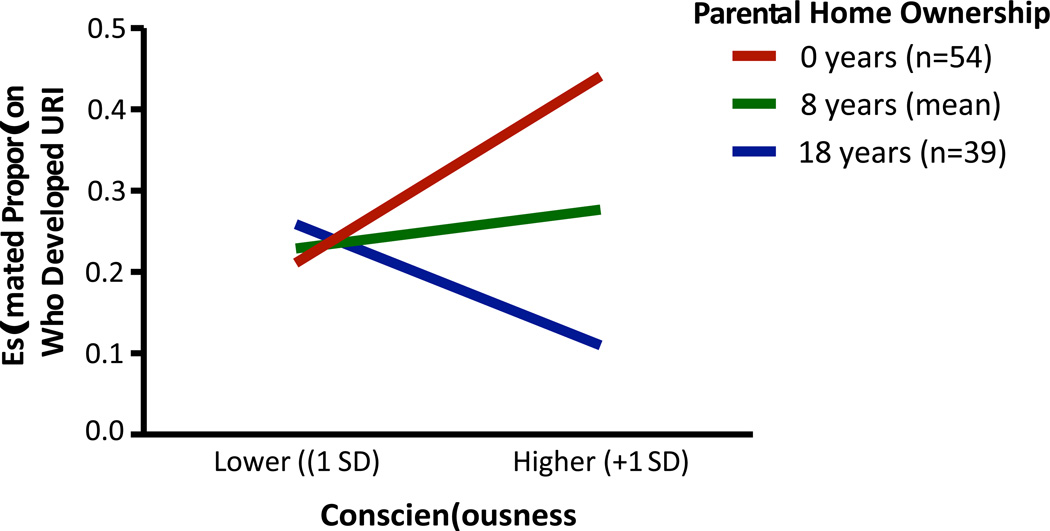
Among Black subjects, negative serostatus was associated with greater odds of URI. None of the remaining covariates significantly predicted risk, and neither did the main effects of early disadvantage and adult conscientiousness. However, the interaction between the latter variables was significant. To clarify the nature of this interaction, we followed standard procedures (Cohen, Cohen, West, & Aiken, 2003), plotting estimated cold risk as a function of lower and higher levels of conscientiousness (−1 and +1 SD from sample average), at three representative levels of early disadvantage. They corresponded to subjects whose parents never owned the family home (0 years; n = 54, 36%), the sample average of 8 years, and subjects whose parents owned continuously through childhood (18 years; n = 39; 26%). As Figure 1 shows, the interaction was a crossover. For subjects from the sample’s most disadvantaged families – i.e., those whose families never owned a home – higher conscientiousness was associated with greater odds of URI diagnosis. This association went in the opposite direction for subjects raised in the sample’s most privileged families; for them higher conscientiousness covaried with greater protection from URI. At the sample’s average level of early disadvantage, the slope for conscientiousness was relatively flat.
Figure 1.
URI risks as a function of early disadvantage and adult conscientiousness among Black subjects.
To evaluate the sensitivity of these results, we re-estimated the logistic regression model using a four-level categorical variable to represent early disadvantage. The groups were comprised of subjects who reported 0 (n=54), 1–9 (n=36), 10–17 (n=21), or 18 (n=39) years of familial home ownership during childhood. As Table S1 shows, the results were identical to those above, with a significant interaction (Wald = 8.07, p = .04). Table S1 also provides a rough estimate of the size of the effect, by contrasting groups of Black subjects with the lowest and highest levels of early disadvantage. The value of the odds ratio suggests for every 1 standard deviation increase in conscientiousness, the latter group has 4.38 times greater odds of URI relative to the former group.
Candidate Mediators
In the last wave of analyses, we examined three explanations for the interaction seen among Black subjects - sleep duration, unhealthy behavior, and cortisol secretion. Following Hayes (2013), we estimated a series of Model 8 equations using the PROCESS macro. These analyses examine whether the strength of an indirect pathway connecting a predictor (adult conscientiousness) and outcome (URI susceptibility) varies across levels of a moderator (early disadvantage). The critical parameter is an index of moderated mediation (Hayes, 2015), whose confidence intervals PROCESS generates in 1000 bootstrapped samples. We tested each candidate mediator in a separate model, and restricted analyses to Black subjects, in whom the interaction was observed. However, none of the models yielded evidence in support of a moderated mediation scenario; in all instances the confidence intervals around the index included 0. (For sleep: index = −.01, SE = .04, CI = −.13, .03; for smoking: index = .01, SE = .03, CI = −.04, .08; for alcohol: index = .02, SE = .04, CI =−.03, .13; for cortisol: index = −.02, SE = .04, CI = −.14, .02).1 As a secondary approach, we also used linear regression to examine whether the candidate mediators patterned in a similar manner to URI risk; i.e., the disadvantage × conscientiousness interaction that defines skin-deep resilience. However, no such interactions were evident among Black subjects (p’s ranged from .18 to .58).
DISCUSSION
Consistent with previous research (Brody et al., 2013; Chen et al., 2015; Miller et al., 2015), we observed a pattern indicative of skin-deep resilience among Black subjects from the sample’s most disadvantaged backgrounds. To the degree they endorsed higher levels of conscientiousness, these subjects fared better across multiple domains of psychosocial functioning, as reflected in educational attainment, symptoms of depression, and close relationships. But the opposite pattern emerged in analyses of health - among these subjects, higher conscientiousness was associated with greater odds of URI diagnosis. These findings extend previous research in several regards. The first is geographic; the results indicate that skin-deep resilience is evident among Black adults (from highly disadvantaged backgrounds) who reside in a large metropolitan area in the Northern United States. Thus, the phenomenon is not restricted to rural Southern youth. The present findings also help clarify the clinical relevance of this phenomenon. Previous research on skin-deep resilience has used biomarkers as proxies for health; the results here suggest that it is associated with disparities in health that are likely to be clinically and economically meaningful. Each year, an estimated 500 million Americans develop viral respiratory tract infections (excluding influenza). The direct costs of treating these illnesses is roughly 17 billion dollars annually, and the indirect costs to families and the economy through lost productivity are even more substantial. Indeed, these illnesses account for roughly 70 millions days of missed work and 189 million days of school each year in the United States (Fendrick, Monto, Nightengale, & Sarnes, 2003).
We also sought to identify pathways through which skin-deep resilience arises, but these analyses did not provide evidence supporting a mediational role for sleep duration, unhealthy behaviors, or cortisol secretion. There are several plausible explanations for these null findings. With only 150 African-American subjects, we are likely to be underpowered for mediation analyses, particularly if there are multiple pathways involved, each accounting for a small portion of the phenomenon. It is also possible that other unmeasured mediators are at work. As a result of the study’s design - subjects were inoculated with fixed doses of specific viruses in a quarantined setting - we are confident that differential exposure is not the key mechanism. Instead, the findings probably reflect disparities in host resistance, which could stem from a plethora of neuroendocrine, virologic, and/or immunologic mechanisms. For instance, skin-deep resilience is associated with greater outflow from the sympathetic nervous system, as reflected in overnight catecholamines (Brody et al., 2013; Chen et al., 2015). Sustained exposure to high doses of these hormones can facilitate replication of some viral species (Lyte, 1993; Sloan et al., 2007). Another factor likely to be important in URI susceptibility is the local inflammatory response. Following infection, airway epithelia and responding leukocytes express cytokines, histamines, leukotrienes, and other mediators, whose actions bring about illness symptoms (Doyle, Skoner, & Gentile, 2005). Consistent with this reasoning, one study observed that the relationship between chronic stress and influenza symptoms was mediated through increased expression of interleukin-6 in nasal secretions (Cohen, Doyle, & Skoner, 1999). Accordingly, future research should examine the roles of sympathetic activity, leukocyte anti-viral functions, and local inflammation in this phenomenon.
Another priority for subsequent research is to clarify the psychological mechanisms that give rise to skin-deep resilience. Doing so may shed light on why this phenomenon occurs among the most disadvantaged Black Americans, but not other demographic groups. Indeed, we observed that in Black subjects from more privileged backgrounds, higher conscientiousness was associated with better psychosocial outcomes and lower URI susceptibility. This convergence of outcomes is consistent with patterns observed in the broader literature, where conscientiousness is known to presage favorable outcomes across multiple life domains (Roberts, Kuncel, Shiner, Caspi, & Goldberg, 2007; Shanahan, Hill, Roberts, Eccles, & Friedman, 2014). Although most of these studies consider SES, they usually evaluate it as an alternative explanation, not as an effect-modifier of conscientiousness. The findings observed here join previous research (Brody et al., 2013; Miller et al., 2015) in suggesting demographic variations in how conscientiousness – and related constructs like self control – forecast health outcomes. As we show here, these variations are most evident at the intersection of two disadvantaged identities, Black race and early poverty.
Why skin-deep resilience arises solely at this particular demographic intersection remains unclear. It may be a consequence of devaluation and alienation in the workplace, or cultural discontinuity. The prevalence and poignancy of these stressors is likely to be disproportionately high among upwardly mobile Black Americans. Also of potential importance in this population is the relative scarcity of family wealth, which can help offspring achieve and maintain financial security, e.g., by subsidizing costs of higher education, contributing to down-payments on a home, cushioning against future incomes shocks. Upwardly mobile individuals whose families lack wealth may also assume financial responsibility for less fortunate relatives, compounding these economic challenges. With that said, none of these hypotheses explains the absence of skin-deep resilience in White subjects from highly disadvantaged backgrounds. It may be that for Blacks, the normative challenges associated with mobility are compounded by experiences like stereotype threat and racial discrimination, which have biological consequences of relevance for health (Brody, Miller, Yu, Beach, & Chen, 2016; Geronimus, 1992; Sellers et al., 2012; Myers, 2009; Lewis, Aiello, Leurgans, Kelly, & Barnes, 2010). Another possibility is that home ownership confers fewer psychosocial and socioeconomic benefits for Black Americans, who even at middle and higher income levels tend to live in neighborhoods with disproportionately high rates of poverty, violence, and pollution (Hardaway & McLoyd, 2009).
The results of these analyses should be considered in light of several limitations. First, the indicators of skin-deep resilience were not optimally measured. Early disadvantage was assessed retrospectively with a single measure of home ownership, and conscientiousness was used a proxy for self control. Although a prospective study originating in childhood would have been optimal, the most plausible consequence of these weaknesses would be to introduce random error and diminish statistical power. The significant results in Black subjects indicate these were not salient problems here; moreover, our previous studies of skin-deep resilience have been multiwave analyses of youth, tracing the developmental course of this phenomenon (Brody et al., 2013; Miller et al., 2015; Chen et al., 2015). Second, because of the demographic composition of samples in the Cold Archive, we were unable to consider these relationships among Latinos, Asians, and other minority communities. Future research should address this question in cohort studies with large, more diverse, samples. Finally, we considered a limited panel of potential mediators, focusing on variables available in both PCS2 and PCS3. As outlined above, there are multiple avenues of mediational research to explore in the future, ranging from economic to psychological to biological. Despite these limitations, these analyses substantially extend our knowledge of skin-deep resilience, clarifying the population in which it arises and documenting its association with URI susceptibility. More broadly, the findings reinforce the notion that resilience is a domain-specific phenomenon (Masten & Narayan, 2012), and that outward indications of overcoming hardship are not necessarily reflective of the biological consequences of having done so (Jackson et al., 2010).
Supplementary Material
Acknowledgments
The studies described herein were supported by grants MH50429 and AI066367 to SC, from the National Institutes of Health (NIH). These projects received clinical and regulatory support via NIH grants RR00056, RR024153, and TR0005, awarded to the University of Pittsburgh. Development of the Common Cold Archive was supported by NIH grant AT006694 to SC.
Footnotes
None of the authors has a conflict of interest to declare related to this paper.
Based on suggestions from reviewers, we also considered perceived stress, social support, educational attainment, subjective SES, physical inactivity, and body mass as mediators, using the same analytic strategy. However, no evidence to support a role for these constructs emerged.
REFERENCES
- Babyak MA. What you see may not be what you get: A brief, nontechnical introduction to overfitting in regression-type models. Psychosomatic Medicine. 2004;66(3):411–421. doi: 10.1097/01.psy.0000127692.23278.a9. [DOI] [PubMed] [Google Scholar]
- Blair C, Raver CC. Child development in the context of adversity: Experiential canalization of brain and behavior. American Psychologist. 2012;67(4):309–318. doi: 10.1037/a0027493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich SN, Jarlenski MP, Bell CN, LaVeist TA. Health inequalities: Trends, progress, and policy. Annual Review of Public Health. 2012;33:7–40. doi: 10.1146/annurev-publhealth-031811-124658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health. 2010;100(Suppl 1):S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Miller GE, Yu T, Beach SR, Chen E. Supportive family environments ameliorate the link between racial discrimination and epigenetic aging: A Replication across two longitudinal cohorts. Psychological Science. 2016 doi: 10.1177/0956797615626703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen E, Miller GE, Kogan SM, Beach SR. Is resilience only skin deep?: Rural African Americans’ socioeconomic status-related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychological Science. 2013;24(7):1285–1293. doi: 10.1177/0956797612471954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Chen E, Miller GE, Brody GH, Lei MK. Neighborhood poverty, college attendance, and diverging profiles of substance use and allostatic load in rural African American youth. Clinical Psychological Science. 2015;3:675–685. doi: 10.1177/2167702614546639. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Alper CM, Doyle WJ, Treanor JJ, Turner RB. Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza a virus. Psychosomatic Medicine. 2006;68(6):809–815. doi: 10.1097/01.psy.0000245867.92364.3c. [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Turner RB, Casselbrant ML, Li-Korotky HS, Epel ES, Doyle WJ. Association between telomere length and experimentally induced upper respiratory viral infection in healthy adults. JAMA. 2013a;309(7):699–705. doi: 10.1001/jama.2013.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Turner RB, Marsland AL, Casselbrant ML, Li-Korotky HS, Doyle WJ. Childhood socioeconomic status, telomere length, and susceptibility to upper respiratory infection. Brain, Behavior, and Immunity. 2013b;34:31–38. doi: 10.1016/j.bbi.2013.06.009. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Third. Malwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB. Sleep habits and susceptibility to the common cold. Archives of Internal Medicine. 2009;169:62–67. doi: 10.1001/archinternmed.2008.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP. Psychological stress, cytokine production, and severity of upper respiratory illness. Psychosomatic Medicine. 1999;61:175–180. doi: 10.1097/00006842-199903000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. Journal of the American Medical Association. 1997;277:1940–1944. [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Childhood socioeconomic status and host resistance to infectious illness in adulthood. Psychosomatic Medicine. 2004;66(1534–7796):553–558. doi: 10.1097/01.psy.0000126200.05189.d3. [DOI] [PubMed] [Google Scholar]
- Cohen S, Tyrrell DA, Russell MA, Jarvis MJ, Smith AP. Smoking, alcohol consumption, and susceptibility to the common cold. American Journal of Public Health. 1993;83(9):1277–1283. doi: 10.2105/ajph.83.9.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle WJ, Skoner DP, Gentile D. Nasal cytokines as mediators of illness during the common cold. Current Allergy and Asthma Reports. 2005;5(3):173–181. doi: 10.1007/s11882-005-0034-8. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Murnane J, editors. Whither Opportunity? Rising Inequality, Schools, and Children’s Life Chances. New York: Russell Sage Foundation; 2011. [Google Scholar]
- Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Social Science and Medicine. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non-influenza-related viral respiratory tract infection in the United States. Archives of Internal Medicine. 2003;163(4):487–494. doi: 10.1001/archinte.163.4.487. [DOI] [PubMed] [Google Scholar]
- Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethnicity and Disease. 1992;2(3):207–221. [PubMed] [Google Scholar]
- Goldberg LR. The development of markers for the Big 5 factor structure. Psychological Assessment. 1992;4:26–42. [Google Scholar]
- Goldberg LR, Johnson JA, Eber HW, Hogan R, Ashton MC, Cloninger CR, Gough HC. The International Personality Item Pool and the future of public-domain personality measures. Journal of Research in Personality. 2006;40:84–96. [Google Scholar]
- Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: how race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. Journal of Youth and Adolescence. 2009;38(2):242–256. doi: 10.1007/s10964-008-9354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S, MacLehose RF, Kaufman JS. Trends in the black-white life expectancy gap among US states, 1990–2009. Health Affairs. 2014;33(8):1375–1382. doi: 10.1377/hlthaff.2013.1273. [DOI] [PubMed] [Google Scholar]
- Hayes AF. An index and test of linear moderated mediation. Multivariate Behavioral Research. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis. New York: The Guilford Press; 2013. [Google Scholar]
- Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. Racial disparities in short sleep duration by occupation and industry. American Journal of Epidemiology. 2013;178(9):1442–1451. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SA. John Henryism and the health of African-Americans. Cultural and Medical Psychiatry. 1994;18(2):163–182. doi: 10.1007/BF01379448. [DOI] [PubMed] [Google Scholar]
- James SA, Strogatz DS, Wing SB, Ramsey DL. Socioeconomic status, John Henryism, and hypertension in blacks and whites. American Journal of Epidemiology. 1987;126(4):664–673. doi: 10.1093/oxfordjournals.aje.a114706. [DOI] [PubMed] [Google Scholar]
- Janicki-Deverts D, Cohen S, Turner RB, Doyle WJ. Basal salivary cortisol secretion and susceptibility to upper respiratory infection. Brain, Behavior, and Immunity. 2016;53:255–261. doi: 10.1016/j.bbi.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SE, Richeson JA, Finkel EJ. Middle class and marginal? Socioeconomic status, stigma, and self-regulation at an elite university. Journal of Personality and Social Psychology. 2011;100(5):838–852. doi: 10.1037/a0021956. doi: [DOI] [PubMed] [Google Scholar]
- Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Behavior, and Immunity. 2010;24(3):438–443. doi: 10.1016/j.bbi.2009.11.011. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, 2nd ed., Vol. 3. Risk, Disorder, and Adaptation. New York: John Wiley & Sons; 2006. pp. 739–795. [Google Scholar]
- Lyte M. The role of microbial endocrinology in infectious disease. Journal of Endocrinology. 1993;137:343–345. doi: 10.1677/joe.0.1370343. [DOI] [PubMed] [Google Scholar]
- Major B, Mendes WB, Dovidio JF. Intergroup relations and health disparities: A social psychological perspective. Health Psychology. 2013;32(5):514–524. doi: 10.1037/a0030358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS. Ordinary magic. Resilience processes in development. American Psychologist. 2001;56(3):227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- Masten AS, Narayan AJ. Child development in the context of disaster, war, and terrorism: pathways of risk and resilience. Annual Review of Psychology. 2012;63:227–257. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E. Unfavorable socioeconomic conditions in early life presage expression of proinflammatory phenotype in adolescence. Psychosomatic Medicine. 2007;69(5):402–409. doi: 10.1097/PSY.0b013e318068fcf9. [DOI] [PubMed] [Google Scholar]
- Miller GE, Yu T, Chen E, Brody GH. Self control forecasts better psychosocial outcomes but faster epigenetic aging in low-SES youth. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(33):10325–10330. doi: 10.1073/pnas.1505063112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers HF. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. Journal of Behavioral Medicine. 2009;32(1):9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- National Center for Statistics. Health, United States 2011: With special feature on socioeconomic status and health. Hyateesville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- Polk DE, Cohen S, Doyle WJ, Skoner DP, Kirschbaum C. State and trait affect as predictors of salivary cortisol in healthy adults. Psychoneuroendocrinology. 2005;30(3):261–272. doi: 10.1016/j.psyneuen.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38(9):1353–1359. doi: 10.5665/sleep.4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28(7):916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Chernyshenko OS, Stark S, Goldberg L. The structure of conscientiousness: An empirical investigation based on seven major personality questionnaires. Personnel Psychology. 2005;58:103–139. [Google Scholar]
- Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The Power of Personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science. 2007;2(4):313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Lejuez C, Krueger RF, Richards JM, Hill PL. What is conscientiousness and how can it be assessed. Developmental Psychology. 2014;50(5):1315–1330. doi: 10.1037/a0031109. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Smith J, Jackson JJ, Edmonds G. Compensatory conscientiousness and health in older couples. Psychological Science. 2009;20(5):553–559. doi: 10.1111/j.1467-9280.2009.02339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychlogy. 1989;57:1069–1081. [Google Scholar]
- Saucier G, Goldberg LR. Assessing the Big Five: Applications of 10 psychometric criteria to the development of marker scales. In: D RB, P M, editors. Big Five Assessment. Boston: Hogrefe & Hube; 2002. pp. 29–58. [Google Scholar]
- Sellers SL, Neighbors HW, Zhang R, Jackson JS. The impact of goal-striving stress on physical health of White Americans, African Americans, and Caribbean blacks. Ethnicity and Disease. 2012;22(1):21–28. [PubMed] [Google Scholar]
- Shanahan MJ, Hill PL, Roberts BW, Eccles J, Friedman HS. Conscientiousness, health, and aging: the life course of personality model. Developmental Psychology. 2014;50(5):1407–1425. doi: 10.1037/a0031130. [DOI] [PubMed] [Google Scholar]
- Sloan EK, Capitanio JP, Tarara RP, Mendoza SP, Mason WA, Cole SW. Social stress enhances sympathetic innervation of primate lymph nodes: Mechanisms and implications for viral pathogenesis. Journal of Neuroscience. 2007;27(33):8857–8865. doi: 10.1523/JNEUROSCI.1247-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality. 2004;72(2):271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Usala PD, Hertzog C. Measurement of affective states in adults: Evaluation of an adjective rating scale instrument. Research on Aging. 1989;11:403–426. doi: 10.1177/0164027589114001. [DOI] [PubMed] [Google Scholar]
- Watt TT. The race/ethnic age crossover effect in drug use and heavy drinking. Journal of Ethnicity and Substance Abuse. 2008;7(1):93–114. doi: 10.1080/15332640802083303. [DOI] [PubMed] [Google Scholar]
- Williams DR. Miles to go before we sleep: racial inequities in health. Journal of Health and Social Behavior. 2012;53(3):279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski TC, Pedersen SL, McCarthy DM, Smith GT. Less drinking, yet more problems: understanding African American drinking and related problems. Psychological Bulletin. 2014;140(1):188–223. doi: 10.1037/a0032113. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.